Abstract
Background
This study will focus on exploring the clinical characteristics of rectal cancer (RC) patients with Second Primary Malignancies (SPMs) and constructing a prognostic nomogram to provide clinical treatment decisions.
Methods
We determined the association between risk factors and overall survival (OS) while establishing a nomogram to forecast the further OS status of these patients via Cox regression analysis. Finally, we evaluated the performance of the prognostic nomogram to predict further OS status.
Results
Nine parameters were identified to establish the prognostic nomogram in this study, and, the C-index of the training set and validation set was 0.691 (95%CI, 0.662–0.720) and 0.731 (95%CI, 0.676–0.786), respectively. The calibration curve showed a high agreement between the predicted and actual results, and the receiver operating characteristic (ROC) curves verified the superiority of our model for clinical usefulness. In addition, the nomogram classification could more precisely differentiate risk subgroups and improved the discrimination of SPMs’ prognosis.
Conclusions
We systematically explored the clinical characteristics of SPMs after RC and constructed a satisfactory nomogram.
Similar content being viewed by others
Introduction
Rectal cancer represents the eighth most frequent diagnosed malignancy and the tenth most common reason for cancer-related deaths globally in 2018, [1] with approximately 732,210 new cases and 339,022 fatalities in 2020 [2, 3]. Nowadays, due to the progress of early diagnosis, comprehensive treatment, and advances in cancer detection, the OS of RC patients has greatly improved [4]. For early-treated rectal cancer, the 5-year OS rate among patients could even reach 90% [5, 6]. However, second primary malignancies are threatening the lives of RC patients who underwent long-term survival [7]. Recently, A growing number of studies have been carried out to investigate the risk factors for the development of SPMs in specific tumors, such as lung cancer [8], prostate cancer [9], breast cancer [10], stomach cancer [11], and so on. The prevalence of SPMs in RC survivors has been reported in earlier studies is 4-8% higher than in the normal population [12]. Factors thought to be influencing this higher rate have been explored in several studies, related to the patient’s genetic factors, lifestyle, environmental risk factors, and cancer therapy [13,14,15].
Nomogram have been identified as a simpler and more sophisticated clinical prediction tool for predicting individualized OS based on clinical characteristics and risk factors [16,17,18]. We discover that it is extremely important to understand the incidence and prognosis of SPM patients for treatment providers and RC patients. Therefore, this study will concentrate on the risk factors for SPMs and will develop a nomogram to forecast the 1-, 3-, and 5-year OS of SPMs after RC.
Materials and methods
Data source
Methods Data were obtained from SEER Research Plus Date,18 Registries, Nov 2020 Sub(2000–2018) in the Surveillance, Epidemiology, and End Results (SEER) database(http:/ /seer.cancer.gov)using SEER* Stat version 8.4.0. Clinicopathological information was gathered including age, race, gender, SPMs site, tumor size, histological type of SPMs and RC, TNM stage, clinical stage, surgical history of SPMs and RC, chemotherapy, radiotherapy, marital status, follow-up time, latency between RC and SPMs, respectively.
Definition of SPMs
SPMs was defined as metachronous invasive solid cancer developing ≥ 6 months after initial primary cancer (IPC), under criteria of Warren and Gates as modified by the National Cancer Institute [19]. The SEER database listed the pathologic subtypes of IPC and SPMs. To better distinguish SPMs from primary and metastatic tumors, we defined SPMs as second malignancy and histological different from IPC with an incubation period of not less than 6 months. Likewise, SEER database provided key clinical information on “malignant tumors for patient” and the “sequence number” of the multiple primary malignancies. It could be used to identify patients with SPM and index the sequence of multiple malignancies.
Patient selection
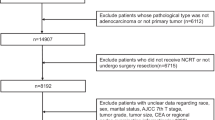
The clinicopathological information of a total of 4374 patients with rectal cancer was obtained from the SEER database. The following were the inclusion criteria: (1) Diagnosed age was between 20 and 80 years. (2) Rectal cancer was discovered in patients between January 2004 and December 2013, and the follow-up period was at least 5 years; (3) Detailed survival data and follow-up information on patients should be provided. The following were the exclusion criteria: (1) Patients without pathological confirmation of the diagnosis; (2) Patients who only provided death certificate records or autopsy records; (3) Latency periods of fewer than 6 months between IPC and SPMs. Next, we screened for the same histological type as rectal cancer (N = 2536), wherein 1838 patients were still diagnosed with SPMs. Patients with unclear clinical data were excluded, including the patients who have no TNM stage (N = 403), unknown lymph node removed (LNR) and marital status (N = 639), and unknown clinical stage of RC (N = 55). Finally, the prognostic nomogram was created using the risk factors that were identified, which were integrated from the detailed clinical data of 741 SPM patients with rectal cancer. Then, the data of 741 patients were randomly split into a training set (N = 585) and a verification set (N = 156) at a ratio of 7:2. Meanwhile, the training and validation set were used for external and internal validation, respectively. The precise details of SPMs screening were shown in Fig. 1.
Statistical analysis
To investigated the relationship between clinicopathological variables and OS of SPMs, univariate and multivariate Cox regression analyses were performed to specify the risk factors. Next, significantly different risk factors were used to build a nomogram that accurately forecast the 1-, 3- and 5-year survival rates of SPM patients. To verified the performance of the nomogram we constructed, the C-index was used to assess the accuracy of the prediction results. Next, the calibration curve was created to evaluate the consistency between predicted and actual results while bootstrapping with 1000 resamples was used to assess discrimination and calibration. Then, survival predictions for 1-, 3-and 5-year were estimated using the ROC curve. In addition, the nutrition risk index (NRI) and integrated discrimination improvement (IDI) were used to evaluate the degree the of accuracy between the nomogram and the conventional AJCC staging system, And the clinical usefulness and benefits of the nomogram were estimated by the decision curve analysis (DCA) plots.
In this study, R software (version 4.1.2) and SPSS 25.0 were both used for all statistical analysis. All tests were two-way and P < 0.05 was considered statistically significant.
Results
Characteristics of patients
A total of 51,611 patients diagnosed with rectal cancer during 2004–2013 was obtained from the SEER database, of which 4,374 patients were diagnosed with cancer more than 6 months after the initial diagnosis of RC. To rule out caused recurrence and metastasis of RC, the patient’s data with the same histological type as RC was ruled out. Ultimately, a total of 1838 (3.56%) patients diagnosed with SPMs were identified. The results showed that the median interval between RC and SPMs diagnosis was 36 months and the median age at SPMs diagnosis was 67.5 years. By using original data obtained from the SEER database, 741 cases of SPMs were found. After removing those with unclear clinical information, more than 1% of the patients’ SPM sites and histological types were listed (Fig. 2), suggesting that the three most common sites for SPMs were the Lung and Bronchus (18.35%), Urinary Bladder (15.11%), and Breast (11.20%) (Table 1) (Table S1). The three most prevalent histological types for SPMs were Squamous Cell Neoplasms (21.32%), Adenomas and Adenocarcinomas (18.76%), Transitional Cell Papillomas and Carcinomas (15.11%) (Table 1) (Table S2).
Final enrollment for further analysis included 741 patients in total, both the training set (N = 585) and the validation set (N = 156) were randomly divided from the 741 patients. Meanwhile, there was no significant difference in clinical information by using the χ2 test (P > 0.05), including the site of SPMs, histology of SPMs, age, race, TNM stage, treatment information, tumor size, and grade of SPMs (Table 2). The training set was used to build the nomogram and verify the model internally, while the validation set was utilized for external validation.
Prognostic factors selection and nomogram construction
Univariate and multivariate Cox regression analysis was applied to reveal OS-related factors in SPMs. The results (Table 3) show that the OS of SPMs was a significantly higher risk with age, TNM stage, stage M of RC, SPMs surgical history, SPMs tumor size (P < 0.001) and site(P = 0.009), while the OS of SPMs was a significantly lower risk with chemotherapy and radiotherapy(P<0.001). Multivariate Cox regression analysis revealed that age, stage-M, stage-M of RC, and SPMs surgical history(P<0.001), stage-T(P = 0.003), and stage-N(P = 0.012) were independent predictive variables for SPMs survival. According to the results of univariate and multivariate Cox regression analysis, 9 parameters including the site, age, stage TNM, stage M of RC, SPMs surgical history, SPMs radiotherapy records, SPMs chemotherapy records, and SPMs tumor size were used to establish a nomogram for predicting 1-, 3-, and 5-year OS (Fig. 3). To use the nomogram more conveniently, each of these characteristics was allocated a particular point on the scale. A total point was received for the individual patients, followed by a summary of the points from each parameter. Then, the probability of OS occurrence after 1, 3, and 5 years was predicted by transferring the entire score to the nomogram’s total score table. As an example, the total point of all variables for an SPM patient diagnosed with 60 years in urinary bladder site of 5 cm Tumor size, T2N2M0, M0 of RC, having SPMs Surgery record and Radiation record, but no chemotherapy record was 135, which corresponded to 1-,3-, and 5- year OS rates of about 88.3%,62.5%, and 50.1%, respectively.
Performance and validation of the nomogram
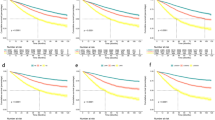
To assessed the discriminative potential of the constructed nomogram in this study, C-index in the training set 0.691 (95% CI, 0.662–0.720) and validation set 0.731 (95% CI, 0.676–0.786) was calculated, indicating that the nomogram has moderate accuracy. To assessed the correctness of our model, calibration plots were utilized to verify the consistency of our prediction and actual outcomes. The 1-, 3-, and 5-year 0 S calibration curves fit well with the 45° diagonal, indicating an excellent performance of the nomogram (Fig. 4). Meanwhile, the time-dependent ROC curves at 1-,3-and 5-year illustrated that the nomogram was more accurate in predicting OS prognosis in the training set 0.79 (95%,0.73–0.85),0.74 (95, 0.69–0.78) and 0.74 (95%,0.69–0.78), and validation set 0.72 (95%CI,0.58–0.85),0.72 (95%CI,0.64–0.80), and 0.70 (95%,0.62–0.79) (Fig. 5), respectively.
As shown in Fig. 6, DCA curves showed that the nomogram could more accurately forecast the likelihood of OS occurring after 1, 3, and 5 years, which, in both groups, may offer greater net clinical advantages than the AJCC stage model. Furthermore, we utilized the NRI and IDI to compare the accuracy of the nomogram with the usual AJCC staging system (Table 4). In the training set, the NRI for 1-3- and 5-year OS were 0.247(95%CI 0.022–0.503), 0.445(95%CI 0.363–0.689) and 0.445(95%CI 0.363–0.689), while the NRI for 1-3- and 5-year OS were 0.247(95%, CI 0.024–0.506), 0.445(95%, CI 0.299–0.682) and 0.075(95%CI 0.400–0.720) in the validation set. Additionally, the INI for 1-3- and 5-year OS were 0.030(P<0.001),0.072(P<0.001), and 0.080(P<0.001) in the training set, and 0.068(P<0.001),0.131(P<0.001) and 0.141(P<0.001) in the validation set. The NRI and IDI results demonstrated that the accuracy of the nomogram to predict OS is much superior than the usual AJCC staging system.
Finally, a risk score for each patient was calculated by nomogram with an establishment of risk stratification (Fig. 7). In both the training (Fig. 7A) and validation (Fig. 7B) sets, the Kaplan-Meier survival curves displayed remarkable statistical difference between high and low-risk individuals (p<0.001).
Discussion
As the incidence of SPMs increased significantly, recent developments in SPMs had heightened the need for research on the monitoring, prognosis, and treatment decisions for clinical and public health [20, 21]. To investigated the prognosis of SPMs following RC, 9 parameters including the site, age, stage TNM, stage M of RC, SPMs surgical history, radiotherapy records, chemotherapy records, and tumor size were analyzed, which were applied to create a new nomogram that forecasts the survival rate of SPM patients. Taken together, our research showed that nomograph is superior to the AJCC staging system in predicting the probability of OS after 1 year, 3 years, and 5 years in the training set and validation set.
In reviewing the literature, Du et al. [22] reported that the three most prevalent sites of SPMs were neoplasms of colorectum (SIR 1.59, 95%CI 1.38–1.83), corpus uteri (SIR 2.11, 95%CI 1.62–2.76), and small intestine (SIR 4.00, 95%CI 2.91–5.49) in recently mete-analysis. Xu et al. [23] showed that Patients with RC were more likely to develop malignant tumors in the thyroid, uterine body, colon, rectum, lung/ bronchus. The same as our research results showed that the three most popular sites for SPMs were the Lung and Bronchus (18.35%), Urinary Bladder (15.11%), and Breast (11.20%). Therefore, it is of great significance to regular and long-term monitoring of the Lung and Bronchus, Urinary Bladder, and Rectum, which was necessary for RC patients at high risk.
Among the 9 parameters included in our nomogram, Age was recognized important risk contributor for SPM patients [24, 25]. Liu et al. [26] reported that Age (50–59:HR 0.958, 95%CI 0.842 − 0.091; 60–100:HR 1.557, 95%1.370–1.747; 18–49 as a reference) by multivariate analysis were all correlated with OS (P<0.001). Similarly, Li et al. [27] noted that Age (≥ 73:HR 1.482,95%CI 1.048–2.152; <73 as a reference) by multivariate analysis were all correlated with OS(P = 0.045). After dividing age into four age groups to better explore the relationship between age and overall survival, the results indicate that Age (60–69:HR1.422,95%CI1.074-1.883;70–79:HR 1.713,95%1.297–2.263; ≥80:HR 2.801,95%11.763–4.450; <60 as a reference) by multivariate analysis were all correlated with OS (P < 0.001). The degradation of the physical state, terrible treatment sensitivity, and the worsening cancer stage in elderly patients may all be contributing factors to these results.
Likewise, multivariate analysis in our study revealed that N stage (N1:HR 0.926, 95%CI 0.660–1.299; N2:1.534 95%CI 1.071–2.197;N3:HR 2.011,95%CI 0.923–4.380; N0 as a reference) for SPM patients had statistically significant OS rates(P = 0.012). This is consistent with those the findings of previous work that the N stage was one of the most significant contributions to OS [28, 29]. This view is supported by Park et al. [30] who reported that patients had higher pathological N stage (N1:HR 1.182,95%CI 1.191–1.845, P<0.001; N2:2.344 95%CI 1.779–3.289, P<0.001; N0 as a reference) significantly associated with OS, suggesting that surveillance was more frequent. As noted by Song et al [31], the N stage was considered as a potential predictor by LASSO, whose classification contributes most to the prognosis of survival in the nomogram they constructed.
Nomogram as a suitable scoring tool for clinical research, it could integrate the effects of various prognostic factors and present the results intuitively. Compared with the current AJCC sixth edition, the nomogram we created demonstrates a noticeably stronger capacity for risk stratification of RC SPM patients. Meanwhile, it is straightforward to gather nine prognostic factors on SPM patients, match that data with the nomogram we created, and calculate the corresponding scores. We could convenient to obtain the 1-, 3-, and 5-year OS by adding and matching the nomogram. The nomogram could help patients’ contributions to information on survival, clinical decision-making guidance, and treatment allocation. For those patients at high risk, they need active therapeutic and close monitoring to improve their overall survival.
Several questions still remain unanswered at present. First, although this study is a retrospective study and strictly complies with the inclusion and exclusion criteria, potential selection bias may have occurred. Secondly, Due to the lack of data relating to chemotherapy protocols and dose, it is not possible to evaluate the effects of different protocols and dose on the onset of secondary cancer. Finally, although our predictive model performs well through internal validation, additional external validation with other populations is still required.
Conclusions
In summary, this study was conducted to describe the clinical characteristics of SPMs in RC survivors and 9 clinical parameters are chosen to create a nomogram to forecast the 1-, 3-, and 5-year OS of SPM patients. It was also shown that the model prediction for OS in SPM patients was superior to the SEER historic stage with RC. Taken together, our findings might provide clinical prognostic guidelines for SPM patients, whose actual efficiency should be further improved through larger research further.
Data Availability
Original data are available from the corresponding author(extract the data in the SEER database: (http://seer.cancer.gov).
Abbreviations
- RC:
-
Rectal Cancer
- OS:
-
Overall Survival
- ROC:
-
Receiver Operating Characteristic
- IPC:
-
Initial Primary Cancer
- LNR:
-
Lymph Node Removed
- NRI:
-
Nutrition Risk Index
- IDI:
-
Integrated Discrimination Improvement
- DCA:
-
Decision Curve Analysis
- SEER:
-
Surveillance, Epidemiology, and End Results
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66(4):683–91. https://doi.org/10.1136/gutjnl-2015-310912.
Biju K, Zhang GQ, Stem M, Sahyoun R, Safar B, Atallah C, et al. Impact of treatment coordination on overall survival in rectal Cancer. Clin Colorectal Cancer. 2021;20(3):187–96. https://doi.org/10.1016/j.clcc.2021.01.002.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1). https://doi.org/10.3322/caac.21590.
Cronin KA, Lake AJ, Scott S, Sherman RL, Noone A-M, Howlader N, et al. Annual Report to the Nation on the Status of Cancer, part I: national cancer statistics. Cancer. 2018;124(13):2785–800. https://doi.org/10.1002/cncr.31551.
Xu J, Huang C, Wu Z, Xu H, Li J, Chen Y, et al. Risk prediction of second primary malignancies in primary early-stage ovarian Cancer survivors: a SEER-Based National Population-Based Cohort Study. Front Oncol. 2022;12:875489. https://doi.org/10.3389/fonc.2022.875489.
Hong J, Wei R, Nie C, Leonteva A, Han X, Du X, et al. The risk and prognosis of secondary primary malignancy in lung cancer: a population-based study. Future Oncol. 2021;17(33):4497–509. https://doi.org/10.2217/fon-2021-0045.
Liu Y, Zhang P, Zhang Y, Zheng L, Xu W, Hou D, et al. Clinical characteristics and overall survival nomogram of second primary malignancies after prostate cancer, a SEER population-based study. Sci Rep. 2021;11(1):1293. https://doi.org/10.1038/s41598-020-80534-4.
Li Z, Wang K, Shi Y, Zhang X, Wen J. Incidence of second primary malignancy after breast cancer and related risk factors-Is breast-conserving surgery safe? A nested case-control study. Int J Cancer. 2020;146(2):352–62. https://doi.org/10.1002/ijc.32259.
Shah BK, Khanal A, Hewett Y. Second primary malignancies in adults with gastric Cancer - A US Population-Based study. Front Oncol. 2016;6:82. https://doi.org/10.3389/fonc.2016.00082.
Lee Y-T, Liu C-J, Hu Y-W, Teng C-J, Tzeng C-H, Yeh C-M, et al. Incidence of second primary malignancies following colorectal Cancer: a distinct pattern of occurrence between Colon and rectal cancers and Association of Co-Morbidity with Second Primary Malignancies in a Population-Based cohort of 98,876 patients in Taiwan. Med (Baltim). 2015;94(26):e1079. https://doi.org/10.1097/MD.0000000000001079.
Wood ME, Vogel V, Ng A, Foxhall L, Goodwin P, Travis LB. Second malignant neoplasms: assessment and strategies for risk reduction. J Clin Oncol. 2012;30(30):3734–45. https://doi.org/10.1200/JCO.2012.41.8681.
Andrieu N, Launoy G, Guillois R, Ory-Paoletti C, Gignoux M. Estimation of the familial relative risk of cancer by site from a french population based family study on colorectal cancer (CCREF study). Gut. 2004;53(9):1322–8.
Dixon LB, Balder HF, Virtanen MJ, Rashidkhani B, Männistö S, Krogh V, et al. Dietary patterns associated with colon and rectal cancer: results from the dietary patterns and Cancer (DIETSCAN) Project. Am J Clin Nutr. 2004;80(4):1003–11.
Balachandran VP, Gonen M, Smith JJ, DeMatteo RP. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16(4):e173–e80. https://doi.org/10.1016/S1470-2045(14)71116-7.
Nieder C, Mehta MP, Geinitz H, Grosu AL. Prognostic and predictive factors in patients with brain metastases from solid tumors: a review of published nomograms. Crit Rev Oncol Hematol. 2018;126:13–8. https://doi.org/10.1016/j.critrevonc.2018.03.018.
Liang W, Zhang L, Jiang G, Wang Q, Liu L, Liu D, et al. Development and validation of a nomogram for predicting survival in patients with resected non-small-cell lung cancer. J Clin Oncol. 2015;33(8):861–9. https://doi.org/10.1200/JCO.2014.56.6661.
Swaroop VS, Winawer SJ, Kurtz RC, Lipkin M. Multiple primary malignant tumors. Gastroenterology. 1987;93(4):779–83.
Joelsson J, Wästerlid T, Rosenquist R, Jakobsen LH, El-Galaly TC, Smedby KE, et al. Incidence and time trends of second primary malignancies after non-hodgkin lymphoma: a swedish population-based study. Blood Adv. 2022;6(8):2657–66. https://doi.org/10.1182/bloodadvances.2021006369.
Li JL, Li H, Wu Q, Zhou H, Li Y, Li YH, et al. Analysis of prognosis and treatment decisions for patients with second primary lung cancer following esophageal cancer. Front Oncol. 2022;12:777934. https://doi.org/10.3389/fonc.2022.777934.
Du S, Li Y, Sun H, Deng G, Tang S, Zeng F, et al. The risk of developing second primary malignancies among colorectal cancer patients. Aging. 2022;14(16):6756–79. https://doi.org/10.18632/aging.204250.
Guan X, Jin Y, Chen Y, Jiang Z, Liu Z, Zhao Z, et al. The incidence characteristics of second primary malignancy after diagnosis of primary Colon and rectal Cancer: a Population based study. PLoS ONE. 2015;10(11):e0143067. https://doi.org/10.1371/journal.pone.0143067.
Valentini V, van Stiphout RG, Lammering G, Gambacorta MA, Barba MC, Bebenek M, et al. Nomograms for predicting local recurrence, distant metastases, and overall survival for patients with locally advanced rectal cancer on the basis of european randomized clinical trials. J Clin Oncol. 2011;29(23):3163–72. https://doi.org/10.1200/jco.2010.33.1595.
Li Y, Liu D, Zhao L, Güngör C, Song X, Wang D, et al. Accurate nomograms with excellent clinical value for locally advanced rectal cancer. Ann Transl Med. 2021;9(4):296. https://doi.org/10.21037/atm-20-4144.
Liu LL, Sun JD, Xiang ZL. A nomogram to predict the prognosis of patients with unresected rectal adenocarcinoma undergoing chemoradiotherapy: a population-based study. J Cancer. 2021;12(16):4745–61. https://doi.org/10.7150/jca.61642.
Li R, Zhang C, Du K, Dan H, Ding R, Cai Z, et al. Analysis of prognostic factors of rectal Cancer and construction of a Prognostic Prediction Model based on bayesian network. Front Public Health. 2022;10:842970. https://doi.org/10.3389/fpubh.2022.842970.
van Gijn W, van Stiphout R, van de Velde CJH, Valentini V, Lammering G, Gambacorta MA, et al. Nomograms to predict survival and the risk for developing local or distant recurrence in patients with rectal cancer treated with optional short-term radiotherapy. Ann Oncol. 2015;26(5):928–35. https://doi.org/10.1093/annonc/mdv023.
Li M, Zhu YZ, Zhang YC, Yue YF, Yu HP, Song B. Radiomics of rectal cancer for predicting distant metastasis and overall survival. World J Gastroenterol. 2020;26(33):5008–21. https://doi.org/10.3748/wjg.v26.i33.5008.
Park MY, Park IJ, Ryu HS, Jung J, Kim MS, Lim SB, et al. Optimal postoperative surveillance strategies for colorectal Cancer: a retrospective observational study. Cancers (Basel). 2021;13(14). https://doi.org/10.3390/cancers13143502.
Song J, Chen Z, Huang D, Wu Y, Lin Z, Chi P, et al. Nomogram Predicting overall survival of Resected locally advanced rectal Cancer patients with Neoadjuvant Chemoradiotherapy. Cancer Manag Res. 2020;12:7375–82. https://doi.org/10.2147/cmar.S255981.
Acknowledgements
We thank the people involved in running the SEER database within the Division of Cancer Control and Population Sciences at the US National Cancer Institute (Bethesda, MD, USA).
Funding
This research was supported by grants from the National Natural Science Foundation of China (82002790, 81902391). This research was also supported by grants from the Foundation of Changzhou Sci&Tech Program (CJ20190097) and the Young Talent Development Plan of Changzhou Health Commission (CZQM2020064).
Author information
Authors and Affiliations
Contributions
YCS and ZDZ: data acquisition and processing, and manuscript drafting. NY: contributed to revising the manuscript. YWJ and JWZ: technique assistance, and data curation. YF: data statistical analysis and critical revision of the manuscript. WHS: research design, results interpretation, and critical revision of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
SEER database belongs to public databases. The patients involved in the database have obtained ethical approval. Users can download relevant data for free for research and publish relevant articles. Our study is based on open source data, so there are no ethical issues.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, YC., Zhao, ZD., Yao, N. et al. Risk prediction of second primary malignancies in patients after rectal cancer: analysis based on SEER Program. BMC Gastroenterol 23, 354 (2023). https://doi.org/10.1186/s12876-023-02974-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-023-02974-2