Abstract
Objective
This study aimed to compare the prognostic value of rectal cancer by comparing different lymph node staging systems, and a nomogram was constructed based on superior lymph node staging.
Methods
Overall, 8700 patients with rectal cancer was obtained from the Surveillance, Epidemiology, and End Results (SEER) database between 2010 and 2015. The area under the curve (AUC), the C index, and the Akaike informativeness criteria (AIC) were used to examine the predict ability of various lymph node staging methods. Prognostic indicators were assessed using univariate and multivariate COX regression, and further correlation nomograms were created after the data were randomly split into training and validation cohorts. To evaluate the effectiveness of the model, the C index, calibration curves, decision curves (DCA), and receiver operating characteristic curve (ROC) were used. We ran Kaplan-Meier survival analyses to look for variations in risk classification.
Results
While compared to the N-stage positive lymph node ratio (LNR), the log odds ratio of positive lymph nodes (LODDS) had the highest predictive effectiveness. Multifactorial COX regression analyses were used to create nomograms for overall survival (OS) and cancer-specific survival (CSS). The C indices of OS and CSS for this model were considerably higher than those for TNM staging in the training cohort. The created nomograms demonstrated good efficacy based on ROC, rectification, and decision curves. Kaplan-Meier survival analysis revealed notable variations in patient survival across various patient strata.
Conclusions
Compared to AJCC staging, the LODDS-based nomograms have a more accurate predictive effectiveness in predicting OS and CSS in patients with rectal cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rectal cancer makes up around 40% of colorectal cancer cases, which is a frequent malignant tumor of the digestive tract that ranks second in death and the third in incidence among all malignant tumors [1]. The prognosis of patients with rectal cancer and the necessity for adjuvant therapy are significantly influenced by the existence of lymph node metastases [2,3,4]. Currently, The American Joint Committee on Cancer (AJCC) staging system is primarily used to stage lymph nodes; however, the anatomy of the pathologist, the technique of the surgeon, tumor heterogeneity, and adjuvant treatments (chemotherapy and radiation) all have an impact on the lymph nodes, which in turn affects the patient’s tumor staging and causes the phenomenon of staging migration [5, 6], and thus affects the treatment and prognosis of patients.
The lymph node ratio (LNR) and the log odds ratio of positive lymph nodes (LODDS) have been shown in multiple studies to have significant prognostic value in various tumors [7,8,9,10,11] and can partially offset the lack of lymph node count, which can alleviate the under or overstatement of the conventional N staging, which is based on the number of a single positive lymph node, and achieve accurate staging and improved clinical outcome for patients with rectal cancer [12]. There are stringent restrictions on the pathology and pathological staging of the patients included in the existing research based on LNR or LODDS, and these studies are not generally applicable. A specific assessment of the various risk stratifications for adjuvant therapy is also lacking, and the usefulness of the lymph node staging threshold still needs to be determined.
Nomograms are now commonly used to assess the prognosis of tumors. They do this by thoroughly evaluating each patient’s various prognostic variables and risk factors, providing individualized prognostic analysis for each patient, improving prediction accuracy, and yielding numerous advantages over traditional TNM staging [13, 14]. Numerous prognostic research on rectal cancer makes use of it.
The majority of the predictive nomograms now in use for rectal cancer have not been further examined for adjuvant therapy and have not been able to overcome the impact of other factors on lymph node detection. We looked into the long-term prognostic effectiveness of the three distinct lymph node stratification techniques for OS and CSS in patients. The most vital predicted efficacy criteria were used in developing the nomograms. A nomogram was used to determine each patient’s risk scores, and reliable risk score stratification of rectal cancer patients was used to perform prognostic analyses. Lastly, we discuss the advantages of radiation and chemotherapy for patients in various risk categories. This research aims to maximize the therapeutic benefit for patients by developing individualized treatment programs, accurately predicting long-term survival, and conducting a thorough investigation of various risk variables.
Methods
Inclusion of Patients
The data in this study were based on the SEER database, which included 8700 patients who were pathologically diagnosed with rectal cancer (209) or rectosigmoid junction cancer (199) according to the International Classification of Diseases of Oncology, Third Edition (ICD-O-3) from 2010 to 2015, and excluded patients who had incomplete basic clinical information due to the following reasons: TNM staging or AJCC staging was missing or unknown; the number of detected lymph nodes or positive lymph node counts were missing or unknown; survival information was missing; and tumor size was unknown. Based on the abovementioned criteria, 8700 patients were selected in this study. Subsequently, they were randomly divided into a training and validation cohorts with a ratio of 7:3. COX regression analysis was used to screen for significant risk factors so that line plots predicting 1-year, 3-year, and 5-year OS and CSS could be created.
Variable Selection
Variables for the analysis conducted in this study included age, sex, histological grading, AJCC stage (7th), T stage, N stage, M stage, chemotherapy, radiotherapy, marital status, regional lymph nodes examined, regional lymph node positivity, survival status, months of survival, cause-specific death status, LNR, and LODDS. The formula for calculating LNR and LODDS based on the number of regional lymph nodes examined and the number of regional lymph node positives is as follows: LNR = regional lymph node positives / regional lymph nodes examined; LODDS = LOG (number of regional lymph node positives + 0.5 / number of regional lymph nodes examined − regional lymph node positives + 0.5). The optimum critical values of LNR and LODDS were calculated using X-tile software based on the principle of maximum rank square value and minimum p value. LNR was divided into three groups: LNR1 (0–0.048), LNR2 (0.049–0.278), and LNR3 (0.280–1). LODDS was divided into three groups: LODDS1 (− 2.25–1.301), LODDS2 (− 1.300–0.355), and LODDS3 (− 0.350–1.886).
Statistical Analysis
The R software (version 4.22, https://www.r-project.org/) was used for all statistical analyses. All tests were two-sided, and p ≤ 0.05 was deemed statistically significant. Continuous data were expressed as mean ± standard deviation and median (range) and compared using the t tests or nonparametric tests. Categorical data were expressed as frequency (percentage) and compared with the chi-squared or Fisher’s exact tests. The N stage, LNR, and LODDS prediction performance for OS and CSS were compared using the C index, Akaike information criterion (AIC), and area under the receiver operating characteristic curve (AUC). The validity of N staging, LNR, and LODDS for prognostic classification of patients with rectal cancer was evaluated using Kaplan-Meier curves. Multivariate Cox analysis was used to identify independent risk factors for rectal cancer, and univariate Cox regression analysis was used to screen for prognosis-related risk factors. Hazard ratio (HR) with their 95% confidence intervals (CIs) were calculated. Recess cancer patients’ nomograms were created using the multifactorial analysis results to forecast OS and CSS at 1, 3, and 5 years. The C index, AUC, AIC, calibration curves, and DCA analysis were utilized to validate the nomograms’ predictive performance. The net benefit of the predictive models for OS, CSS, and other domains was compared with the AJCC staging system at various times. X-tile software performed risk stratification into three stages (NSL, NSM, and NSH). Kaplan-Meier analysis was then utilized to examine the variations in survival at each stage and further analyze the effects of the various risk stratifications on chemotherapy and radiation therapy.
Results
Patient Clinical Information
A total of 8700 rectal cancer patients were included in this study and were randomly assigned into training and validation cohorts with a ratio of 7:3. Specific clinical information and pathological characteristics are shown in Table 1.
Comparison of Predictive Efficacy of Different Lymph Node Analyses
Among the cohort of all patients, we firstly conducted a univariate COX regression analysis to evaluate the impact of various lymph node staging on overall prognosis. The findings indicated that N staging, LNR, and LODDS were significantly associated with (p < 0.001) patients with rectal cancer (Table 2). In addition, the three lymph node staging methods exhibited high predictive efficiency among different risk strata, as demonstrated by the Kaplan-Meier survival analysis (Fig. 1). The results show that LODDS staging has the highest AUC and C index values and the lowest AIC value (Table 3). This suggests that LODDS is more reliable than N staging and LNR in predicting the long-term survival outcome and has the best efficacy in predicting OS and CSS in patients with rectal cancer.
Kaplan-Meier analysis of overall survival (OS) and cancer-specific survival (CSS) of rectal cancer patients based on different lymph node staging modalities OS: a Kaplan-Meier curves based on N staging; b Kaplan-Meier curves based on LNR staging; and c Kaplan-Meier curves based on LODDS staging. CSS: d Kaplan-Meier curves based on N staging; e Kaplan-Meier curves based on LNR staging; and f Kaplan-Meier curves based on LODDS staging
Univariate and Multivariate COX Regression Analyses of Prognostic Factors
Univariate Cox regression analysis revealed that age, gender, histological stage, T stage, M stage, radiotherapy, chemotherapy, tumor size, marital status, and LODDS as risk factors for OS and CSS. Multifactorial analysis was performed, showing age, gender, histological staging, T staging, M staging, chemotherapy, tumor size, marital status, and LODDS as independent risk factors for OS (p < 0.05) (Table 4). There was a statistically significant difference (p < 0.05) in CSS concerning age, gender, histological staging, T staging, M staging, chemotherapy, marital status, and LODDS (Table 5).
Construction and Validation of the OS and CSS Nomograms
Based on the results of the above analysis, we selected 9 variables, including LODDS (age, gender, histological grading, T staging, M staging, tumor size, chemotherapy, LODDS, marital status) to construct OS and CSS prognostic nomograms for rectal cancer patients (Fig. 2). The patient’s OS and CSS were predicted by aggregating the relative risk scores of the patient’s risk variables to get a final total risk score. The calibration curves were close to the standard curves in both the training and validation cohorts, indicating that the column plot had exceptional predictive accuracy in predicting 1-, 3-, and 5-year OS and CSS (Figs. 3 and 4).
Prognosis of Patients with Rectal Cancer by the Nomograms Versus Conventional AJCC Staging
The C indices of the LODDS-based nomograms for OS and CSS for the training and validation cohorts, respectively (OS training cohort 0.716, validation cohort 0.726; CSS training cohort 0.755, validation cohort 0.757) were significantly higher than those for the traditional AJCC staging (OS training cohort 0.624, validation cohort 0.629; CSS training cohort 0.679, validation cohort 0.678). Meanwhile, the nomograms of AIC (OS training cohort 36,625, validation cohort 14,441; CSS training cohort 25,666, validation cohort 9877) were lower than the AJCC staging (OS training cohort 37,390, validation cohort 14,797 CSS; training cohort 26,278, validation cohort 10,121) (Table 6). The ROC curves also showed good discriminatory ability and predictive accuracy (Figs. 5 and 6). The DCA curves showed that the nomograms constructed based on the LODDS would achieve a more significant net gain than traditional AJCC staging, which is more favorable to the clinical benefit of rectal cancer patients (Figs. 7 and 8).
Survival Curves and Adjuvant Treatment Effects Based on the Nomograms Risk Scores
We calculated the total risk scores for OS and CSS for each patient based on the nomograms using R language calculations, respectively, and risk-stratified them using the X-tile software into a high-risk group (NSH, OS 242.01 < NSH < 411.19; CSS 208.43 < NSH < 348.49), an intermediate risk group (NSM, OS 160.25 < NSM < 241.87, CSS 141.05 < NSM < 208.38), and low-risk group (NSL, OS NSL < 160.19, CSS NSL < 141.04), and then, Kaplan-Meier analyses were carried out on them. Based on our risk score stratification, the results showed that OS or CSS had good differentiation between high-risk, moderate-risk, and low-risk insurance groups (Fig. 9). We then further explored the impact of chemotherapy on patient survival according to different risk stratifications. In the high-risk group, chemotherapy showed a significant advantage in improving patients’ CSS and OS survival, and the intermediate-risk group showed a similar trend, but the results were not statistically significant. In the low-risk group, however, chemotherapy demonstrated deleterious effects on OS and CSS (Supplementary Fig. 1). Similar results to chemotherapy were demonstrated at the radiotherapy level, with a significant benefit at the radiotherapy level in the high-risk group. However, a similar trend towards benefit was demonstrated in the intermediate-risk group and a trend towards detriment to radiotherapy in the low-risk group. However, no statistically reliable results were obtained in either group (Supplementary Fig. 2).
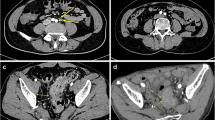
Kaplan-Meier survival analyses based on the nomograms’ hazard scores for nomogram high-scoring group (NSH), nomogram medium-scoring group (NSM), and nomogram low-scoring group (NSL). a Kaplan-Meier curves in the OS training set. b Kaplan-Meier curves in the CSS training set. c Kaplan-Meier curves in the OS validation set. d Kaplan-Meier curves in the CSS validation set
Discussion
Lymph node status is an essential factor affecting local recurrence and overall survival in patients with rectal cancer [15]. Treatment options regarding rectal cancer are increasingly converging towards surgery combined with radiotherapy and chemotherapy [16, 17], and the pathological staging of lymph nodes is closely related to adjuvant treatment options. Currently, AJCC staging is widely used to evaluate the pathological staging of lymph nodes. However, this criterion is affected by various factors such as surgical approach, pathological assessment, adjuvant therapy, and BMI of the patient, compromising the precision of staging the pathology [6, 18]. In recent years, the emergence of LNR and LODDS has been recognized as a better alternative to traditional N staging. It is not limited by the number of lymph nodes detected, reducing staging migration [19, 20]. Several studies have confirmed that LODDS is an independent prognostic factor for different types of cancers and has a more accurate predictive efficacy than traditional AJCC staging and LNR [21,22,23].
Through univariate COX regression analysis, we can see that the N, LNR, and LODDS stages are all potential prognostic factors for patients with rectal cancer. The Kaplan-Meier survival curves also revealed that the three staging schemes were able to stratify the patients’ prognostic status and that the LODDS staging had the highest C index, AUC value, and lowest AIC value when compared to the N staging and LNR staging, indicating that it was the most effective at predicting the prognosis of patients with rectal cancer. In univariate and multivariate COX regression analysis of prognostic factors in the patient population, the other risk factors affecting the prognosis of patients with rectal cancer include age, gender, histological grading, T staging, M staging, chemotherapy, tumor size, LODDS, and marital status. Based on our constructed nomograms, the predictive efficacy of 1-, 3-, and 5-year OS and CSS for rectal cancer patients was significantly higher than that of AJCC staging. It was more pronounced in the training cohorts and validation cohorts of CSS. The correction curves likewise showed good agreement with the actual observations. Guo et al. explored that LODDS had predicted CSS in T1 stage rectal cancer [24], showing satisfactory results, and within T1 stage, LODDS can be further stratified for more accurate survival prediction and identification of high-risk patients. However, its applicability in other stages has to be confirmed. Christina et al. predicted survival in patients with stage III rectal cancer [5]. However, the sample size of this study was too small, except for staging limitations, and there was a higher likelihood of class II error. The present study has no strict limitations on pathological staging, has good applicability, and included 8700 patients with rectal cancer, making it a reliable study. It is worth mentioning that tumor size did not show statistically significant in the CSS cohort. The reason may be attributed to unclear patient information in some of the SEER databases and other reasons for the impact of patient death on survival status. However, studies have shown that tumor size is closely associated with long-term survival in colorectal cancer, with a prognostic value of clinical importance no less than that of the T staging [25,26,27]. Therefore, we have included it in the CSS the nomograms.
Currently, adjuvant treatment options for rectal cancer remain controversial [28], with some articles reporting no significant improvement in survival benefits with adjuvant chemotherapy in older patients with stage II and III rectal cancer [29,30,31], and an increase in chemotherapeutic complications as well as toxic effects [32, 33]. Therefore, identifying the population that will benefit from adjuvant therapy is crucial. Until now, no studies have been found to explore the correlation between LODDS and adjuvant therapy for rectal cancer. We scored the included patients’ basic clinical information and pathological characteristics using a nomogram. We used X-tile software to categorize the patients in the training cohort into three groups based on their nomogram scores: a nomogram high-scoring group, a nomogram medium-scoring group, and a nomogram low-scoring group. Regarding chemotherapy, the high-scoring group showed a significant survival benefit, with a statistically significant difference (p < 0.05).
On the contrary, the low-scoring group demonstrated a detrimental trend. A beneficial trend was also demonstrated in the nomogram medium-scoring group. However, statistical significance has yet to be reached in the validation group, and it is reasonable to infer that it is related to insufficient sample size in the training cohort. In radiotherapy, similar to chemotherapy, only the nomogram high-scoring group showed improved survival outcomes, with the nomogram medium-scoring group and the nomogram low-scoring group showing detrimental trends. These results suggest our nomograms, which are essential for the treatment of rectal cancer patients. There are some limitations of this study; firstly, the cohort lacked an external validation cohort to confirm further the model’s predictive ability for OS and CSS. Secondly, the clinical data included in this study inevitably suffered from retrospective bias, with some patients needing more clinical information, resulting in their non-inclusion in the study cohort. Future large-scale prospective clinical data are needed to confirm the reliability of the findings of this study.
Conclusion
This study is based on the population to develop the LODDS-based nomograms, which were confirmed to have superior predictive ability by analysis. And LODDS is a more reliable prognostic predictor than conventional TNM staging and LNR. The nomogram-based prognostic classification is valuable for identifying high-risk populations that may benefit from adjuvant treatment. In summary, these nomograms can be a reliable prognostic predictor for rectal cancer patients and can help guide patient treatment.
Data Availability
No datasets were generated or analysed during the current study.
References
Sung H, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
Resch A, Langner C. Lymph node staging in colorectal cancer: old controversies and recent advances. World J Gastroenterol. 2013;19(46):8515–26. https://doi.org/10.3748/wjg.v19.i46.8515.
Horne J, et al. Lymph node revealing solutions in colorectal cancer: should they be used routinely? J Clin Pathol. 2014;67(5):383–8. https://doi.org/10.1136/jclinpath-2013-202146.
Betge J, et al. Lymph node retrieval in colorectal cancer: determining factors and prognostic significance. Int J Colorectal Dis. 2017;32(7):991–8. https://doi.org/10.1007/s00384-017-2778-8.
Lee CW, et al. The log odds of positive lymph nodes stratifies and predicts survival of high-risk individuals among stage III rectal cancer patients. Oncologist. 2016;21(4):425–32. https://doi.org/10.1634/theoncologist.2015-0441.
McDonald JR, et al. Lymph node harvest in colon and rectal cancer: current considerations. World J Gastrointest Surg. 2012;4(1):9–19. https://doi.org/10.4240/wjgs.v4.i1.9.
Yang XL, et al. Comparison of different lymph node staging schemes for predicting survival outcomes in node-positive endometrioid endometrial cancer patients. Front Med (Lausanne). 2021;8(2296–858X (Print)):688535. https://doi.org/10.3389/fmed.2021.688535.
Zhang X, et al. Development and validation of a new lymph node ratio-based staging system for ampullary carcinoma after curative pancreaticoduodenectomy. Front Oncol. 2021;11(2234–943X (Print)):811595.https://doi.org/10.3389/fonc.2021.811595.
Yu Y, et al. Prognostic value of log odds of positive lymph nodes in node-positive lung squamous cell carcinoma patients after surgery: a SEER population-based study. Transl Lung Cancer Res. 2020;9(4):1285–301. https://doi.org/10.21037/tlcr-20-193.
Jin ML, et al. Modified lymph node ratio improves the prognostic predictive ability for breast cancer patients compared with other lymph node staging systems. Breast. 2020;49(1):93–100. https://doi.org/10.1016/j.breast.2019.11.003.
Sun Y, et al. Development and validation of nomograms for predicting overall survival and cancer-specific survival in elderly patients with locally advanced gastric cancer: a population-based study. BMC Gastroenterol. 2023;23(1):117. https://doi.org/10.1186/s12876-023-02749-9.
Zhang CH, et al. The prognostic impact of the metastatic lymph nodes ratio in colorectal cancer. Front Oncol. 2018;8(2234–943X (Print)):628. https://doi.org/10.3389/fonc.2018.00628.
Balachandran VP, et al. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16(4):e173-80. https://doi.org/10.1016/S1470-2045(14)71116-7.
Grimes DA. The nomogram epidemic: resurgence of a medical relic. Ann Intern Med. 2008;149(4):273–5. https://doi.org/10.7326/0003-4819-149-4-200808190-00010.
Zhuang Z, et al. Magnetic resonance imaging evaluation of the accuracy of various lymph node staging criteria in rectal cancer: a systematic review and meta-analysis. Front Oncol. 2021;11(2234–943X (Print)):709070.https://doi.org/10.3389/fonc.2021.709070.
Benson AB, et al. Rectal Cancer, Version 2.2022, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2022;20(10):1139–67. https://doi.org/10.6004/jnccn.2022.0051.
Hagerty BL, et al. Age determines adjuvant chemotherapy use in resected stage II colon cancer. Dis Colon Rectum. 2022;65(10):1206–14. https://doi.org/10.1097/DCR.0000000000002074.
Gorog D, et al. Influence of obesity on lymph node recovery from rectal resection specimens. Pathol Oncol Res. 2003;9(3):180–3. https://doi.org/10.1007/BF03033734.
Wang J, et al. Lymph node ratio: role in the staging of node-positive colon cancer. Ann Surg Oncol. 2008;15(6):1600–8. https://doi.org/10.1245/s10434-007-9716-x.
Marchet A, Mocellin S, Ambrosi A, et al. The ratio between metastatic and examined lymph nodes (N ratio) is an independent prognostic factor in gastric cancer regardless of the type of lymphadenectomy: results from an Italian multicentric study in 1853 patients. Ann Surg. 2007;245(4):543–52. https://doi.org/10.1097/01.sla.0000250423.43436.e1.
Jin W, et al. Prognostic value of log odds of positive lymph nodes in patients with resectable oral squamous cell carcinoma. Oral Oncol. 2020;108(1879–0593 (Electronic)):104709.https://doi.org/10.1016/j.oraloncology.2020.104709.
Li S, Wang Y, Hu X. Prognostic nomogram based on the lymph node metastasis indicators for patients with bladder cancer: a SEER population-based study and external validation. Cancer Med. 2023;12(6):6853–66. https://doi.org/10.1002/cam4.5475.
Liang Z, et al. Log odds of positive lymph nodes show better predictive performance on the prognosis of early-onset colorectal cancer. Int J Colorectal Dis. 2023;38(1):192. https://doi.org/10.1007/s00384-023-04490-x.
Guo Z, et al. A nomogram based on the log odds of positive lymph nodes for predicting the prognosis of T1 stage rectal cancer. Am J Cancer Res. 2023;13(4):1498–508.
Saha S, et al. Tumor size predicts long-term survival in colon cancer: an analysis of the National Cancer Data Base. Am J Surg. 2015;209(3):570–4. https://doi.org/10.1016/j.amjsurg.2014.12.008.
Dai W, et al. The critical role of tumor size in predicting prognosis for T1 colon cancer. Oncologist. 2020;25(3):244–51. https://doi.org/10.1634/theoncologist.2019-0469.
Alese OB, et al. Predictive and prognostic effects of primary tumor size on colorectal cancer survival. Front Oncol. 2021;11(2234–943X (Print)):728076.https://doi.org/10.3389/fonc.2021.728076.
Hu X, et al. Adjuvant chemotherapy seemed not to have survival benefit in rectal cancer patients with ypTis-2N0 after preoperative radiotherapy and surgery from a population-based propensity score analysis. Oncologist. 2019;24(6):803–11. https://doi.org/10.1634/theoncologist.2017-0600.
Lee Y, et al. Effect of adjuvant chemotherapy on elderly stage II high-risk colorectal cancer patients. Ann Coloproctol. 2021;37(5):298–305. https://doi.org/10.3393/ac.2020.00829.0118.
Shiraishi T, et al. Differences in prognosis and underuse of adjuvant chemotherapy between elderly and non-elderly patients in stage III colorectal cancer. Ann Gastroenterol Surg. 2023;7(1):91–101. https://doi.org/10.1002/ags3.12604.
Lee KY, et al. Adjuvant chemotherapy does not provide survival benefits to elderly patients with stage II colon cancer. Sci Rep. 2019;9(1):11846. https://doi.org/10.1038/s41598-019-48197-y.
Andre T, et al. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol. 2009;27(19):3109–16. https://doi.org/10.1200/JCO.2008.20.6771.
Tong L, et al. Effects of newly developed chemotherapy regimens, comorbidities, chemotherapy-related toxicities on the changing patterns of the leading causes of death in elderly patients with colorectal cancer. Ann Oncol. 2014;25(6):1234–42. https://doi.org/10.1093/annonc/mdu131.
Author information
Authors and Affiliations
Contributions
All authors contributed to the research design. Study design: Jian Li and Peng Xu, statistical analysis: Jian Li. and Yu Zhou Yang, manuscript writing: Jian Li and Yu Zhou Yang, study guidance and supervision: Peng Xu and Cheng Zhang; all authors participated in writing and approved the submission of the manuscript for publication.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent for Publication
All authors consent to the publication of this study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, J., Yang, Y.z., Xu, P. et al. A Prognostic Model Based on the Log Odds Ratio of Positive Lymph Nodes Predicts Prognosis of Patients with Rectal Cancer. J Gastrointest Canc (2024). https://doi.org/10.1007/s12029-024-01046-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s12029-024-01046-2