Abstract
Background
Magnetic resonance imaging (MRI) has excellent accuracy in diagnosing preoperative lesions before anal fistula surgery. However, MRI is not good in identifying early recurrent lesions and effective methods for quantitative assessment of fistula healing are still warranted. This retrospective study aimed to develop and validate a specific MRI-based nomogram model to predict fistula healing during the early postoperative period.
Methods
Patients with complex cryptoglandular anal fistulas who underwent surgery between January 2017 and October 2020 were included in this study. MRI features and clinical parameters were analyzed using univariate and multivariate logistic regression analysis. A nomogram for predicting fistula healing was constructed and validated.
Results
In total, 200 patients were included, of whom 186 (93%) were male, with a median age of 36 (18–65) years. Of the fistulas, 58.5% were classified as transsphincteric and 19.5% as suprasphincteric. The data were randomly divided into the training cohort and testing cohort at a ratio of 7:3. Logistic analysis revealed that CNR, ADC, alcohol intake history, and suprasphincteric fistula were significantly correlated with fistula healing. These four predictors were used to construct a predictive nomogram model in the training cohort. AUC was 0.880 and 0.847 for the training and testing cohorts, respectively. Moreover, the decision and calibration curves showed high coherence between the predicted and actual probabilities of fistula healing.
Conclusions
We developed a predictive model and constructed a nomogram to predict fistula healing during the early postoperative period. This model showed good performance and may be clinically utilized for the management of anal fistulas.
Similar content being viewed by others
Background
Anal fistulas have a mean incidence of 8.6 cases per 100,000 of the population [1], with the surgical approach depending on the classification [2]. Magnetic resonance imaging (MRI) has been shown to be extremely accurate in identifying the perianal fistula anatomy, the presence and location of an internal opening, and the structural relationship between the fistula tract(s) and the main sphincter complex [3, 4]. The degree of accuracy has been improved by a range of techniques that routinely include T1- and T2-weighted imaging, and fat suppression sequences. Such examinations can qualitatively discriminate between the signal characteristics of active sepsis and those of fibrotic tissues. Consequently, the value of preoperative MRI in influencing the course of subsequent surgery has been well-documented, greatly reducing the likelihood of recurrence [5]. In addition to its crucial role in preoperative evaluation, MRI is highly accurate in identifying and diagnosing postoperative complications like abscess formation or tracts which were missed intraoperatively. After surgery, fistulas may recur even in apparently clinically healed tracts, where MRI can clearly detect recurrent or recrudescent abscess, even with external opening or openings have closed [6].
However, this MR-centered approach must consider the fact that in the immediate and early postoperative periods (before 12 weeks), an active fistula without abscess may be difficult to differentiate from healing granulation tissue. Both can initially appear hyperintense on T2W and STIR sequencing [6]. This adds many difficulties to clinical decisions regarding whether a relapse or a normal healing process occurs.
Two recent advances in MRI are diffusion-weighted imaging (DWI) and dynamic contrast-enhanced (DCE) sequences. These techniques provide an objective measure of diffusion and perfusion parameters associated with fistula activity [7]. Reflecting the limited diffusion of water molecules, DWI has a specific advantage in helps discriminate between an abscess and inflammatory mass [8]. In contrast, DCE-MRI permits the semiquantitative represent the signal intensity of the tissue [9], where in a previous study the absolute amounts of the time-intensity curves shape types correlate with the perianal disease activity index [10]. For most complex anal fistulas, improper management of the tracts and internal opening is one of the most common causes of fistula recurrence. As a result, early postoperative MRI evaluation helps to identify the presence of recurrence so that corrective measures can be promptly taken. Therefore, we aimed to assess the application of DWI and DCE in determining whether a relapse or normal healing process occurs at an early stage after fistula surgery. To our knowledge, many studies have used MRI parameters to build a nomogram model to predict the regression of patients with tumor [11,12,13]. Similar to these studies, the aim of our study was to explore and validate a specific MRI-based nomogram model to predict fistula healing during the early postoperative period. We suggest that this model would assist surgeons and patients in a shared decision-making process.
Methods
Study population
This retrospective study was approved by Ethical Committee of the Sixth Affiliated Hospital of Sun Yat-Sen University (no. 2020ZSLYEC-199). The study database initially included data pertaining to 2,840 consecutive patients who were under the care of the Coloproctology Section of the Sixth Affiliated Hospital of Sun Yat-Sen University between January 2017 and October 2020. Based on the data presented in Fig. 1, it is evident that only approximately 22.5% of the reviewed patients had complete preoperative and postoperative MRI data. After the exclusion process, a total of 200 cases were ultimately included, all of which had complex cryptoglandular anal fistulas managed with a two-stage procedure and assessed using pre- and postoperative MRI examinations, enabling the use of their MRI data to develop a model for predicting fistula healing. Regarding the purposes of definition and analysis, complex cryptoglandular anal fistulas included high transsphincteric fistulas that exceeded one-third of the coronal length of the anal sphincter complex. They also included horseshoe anal fistula, supra- and extrasphincteric fistulas, fistula with lateral extensions, multiple tracts, and any case of translevator extension(s). The exclusion criteria were as follows: Patients aged < 18 or > 65 years, simple or no branch fistula, fistulas associated with inflammatory bowel disease (IBD), underlying gastrointestinal cancer, known pulmonary tuberculosis, fistula surgery combined with another operation, HIV-AIDS, type 2 diabetes or hypertension and no DCE or DWI sequence. The details are shown in Fig. 1.
Clinical data collection
All patients in this study underwent preoperative MRI to assess the fistula anatomy. The patients included in this study were diagnosed with complex anal fistulas and underwent a two-stage surgical approach. In the first-staged surgery, a modified Henley procedure was performed with focus on curetting the branch tract(s) outside the EAS and placing a loose seton around the sphincters. Approximately one and half months later, the branch tracts were healed/nearly healed and another MRI examination was performed to identify whether the tract(s) outside the EAS healed. If the wound outside the EAS healed, the patients underwent a delayed second-stage procedure consisting of seton removal and fistulotomy. For a minority of patients, in outpatient practice a loose seton is tightened until falling out on its own.
Patient demographic data collected included age, sex, body mass index (BMI), fistula classification, alcohol intake history, smoking history and previous anal surgery history. Fistula healing was defined as complete epithelialization of the external opening without discharge [14, 15]. Alcohol intake was defined as current or prior habitual consumption (one to two times/week) of any amount or type of alcohol and then divided into two variables (drinking and no drinking) [16, 17]. Smoking was defined as self-reported smoking (smoking ≥ 5 cigarettes per day for > 6 months) [18].
Quantitative MRI analysis
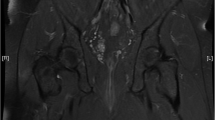
The MRI scans were evaluated by two doctors with extensive experience who were leading in interpreting pelvic MRIs. Consensus findings were recorded by a senior radiologist who were blinded to the clinical history and reference standard of the outcomes. We used T2-weighted and fat suppression sequences to reveal the anatomic structures of the anal region and fistula. For DWI, we delineated the region of interest (ROI) for the lesion area (b = 1200 s/mm2). They then located this region on an apparent diffusion coefficient (ADC) map. ADC values were calculated automatically on a dedicated workstation, as shown in Fig. 2 with measurements repeated thrice to obtain an average recording. Regarding DCE sequences, the contrast-to-noise ratio (CNR) in the Ax-LAVA Flex + C series was also measured thrice, and the average value was calculated as follows:
a. The fistula tracks visible on the preoperative DCE images, SIlesion, SItissue, and SDbackground are measured. b. In preoperative DWI in the axial plane (b = 1200), the fistula tracks have a high signal intensity. c. A ROI is manually positioned on the diffusion MR image and copied on the ADC map. d. The same level to measure the SIlesion, SItissue, and SDbackground on postoperative DCE images. e. Postoperative DWI (same level) in the axial plane (b = 1200), showing healed fistula tracks. f. A ROI is manually positioned on the diffusion MR image and copied on the ADC map. DWI, diffusion-weighted images; ROI, region of interest; MR, magnetic resonance; ADC, apparent diffusion coefficient; DCE, dynamic contrast-enhanced; SI, signal intensity
In this fomula, SIlesion represents the fistula signal intensity (SI), whereas SInormal tissue represents the SI of normal muscles around the fistulas. SDbackground reflects the standard deviation of background signal [19].
Statistical analysis
Continuous data are presented as medians and ranges, while categorical variables are expressed as numbers and percentages (%). The Mann-Whitney U test was used to compare continuous data, and the Chi-square or Fisher’s exact test was used where appropriate for comparisons between categorical variables. Receiver operating characteristic (ROC) analysis was performed to define the optimal cut-off values for ADC and CNR by calculating the area under the curve (AUC), other indicators include sensitivity and specificity. Risk factors for fistula healing were assessed using univariate analysis, and significant variables (P < 0.1) were incorporated into a multivariate logistic regression analysis. Factors with prognostic significance in the multivariate logistic regression analysis were used to build a fistula-healing model. A nomogram was used to visualize the model. Prediction models were developed with a random sample of 70% of the cohort as the training cohort, and then validated with the remaining 30% of the cohort as the validation cohort. Decision curve analysis and calibration curves were used to evaluate the model’s predictive performance. Statistical analyses were performed using R software version 4.1.0. P values < 0.05 were considered significant.
Results
Clinical characteristics and basic MRI features of the patients
The baseline clinical characteristics of the patients are summarized in Table 1. A total of 200 patients were included in the study, of whom 186 (93%) were male. The median age and BMI were 36 years (range: 18–65 years) and 23.8 kg/m2 (16.9–35.9 kg/m2), respectively. A total of 92 (46%) patients had a smoking history and 28 (14%) had a history of alcohol intake. Seventy one (35.5%) and 109 (54.5%) patients had recurrent and horseshoe fistulas, respectively. In total, there was a 19.5% incidence of suprasphincteric fistula in this cohort.The median time from preoperative MRI examination to the first stage surgery were 3 days (range: 0–39 days). The median time from the first stage surgery to postoperative MRI examination were 62 days (range: 26–179 days). The median postoperative CNR values of healed fistulas were lower than those measured in non-healed cases (36.6 versus 99.9; P < 0.01). The median postoperative ADC values of healed fistulas were higher than those measured in non-healed cases (1.35 × 10− 3 mm2/s versus 1.28 × 10− 3 mm2/s; P < 0.05). In total, there were no significant differences between the two groups except for alcohol intake history, postoperative CNR value and postoperative ADC value.
Predictors for fistula healing in the training cohort
The data were randomly divided into the training and testing cohort at a ratio of 7:3. The characteristics of the patients in the training and testing cohort are displayed in Table 2. To explore the cut-off value of the CNR and ADC, we performed ROC analysis in the training cohort. Based upon the ROC analysis, the optimal CNR cut-off for healing fistula was 63.51 with an AUC of 0.854. This provided a sensitivity of 83.8% and a specificity of 78.9%. Additionally, an optimal ADC cut-off value for a healing fistula, which was 1.34 × 10− 3 mm2/s with an AUC of 0.612, provided a sensitivity of 68.9%, specificity of 57.7% (Fig. 3a). Given the performance characteristics of the CNR, we demonstrated its ability to predict early fistula healing using ROC analysis. The AUC value was 0.837 in the 60-day period and 0.868 in the 90-day period by ROC analysis. In the 60 days therapeutic range, a CNR cut-off of 65.83 yielded a sensitivity of 77.8%, specificity of 81.1%. In addition, in the 90 days therapeutic range, a CNR cut-off of 65.33 resulted in a sensitivity of 85.0%, specificity of 79.0% (Fig. 3b).
Subsequently, logistic regression was performed in the training cohort to develop the predictive model. Data regarding sex, age, alcohol intake history, smoking history, BMI, recurrent fistula, horseshoe fistula, fistula classification (Intersphincteric fistula, transsphincteric fistula, suprasphincteric fistula and extrasphincteric fistula), CNR value, and ADC value were considered potential prognostic factors affecting fistula healing and were included in the univariate analysis. The results suggested that alcohol intake history (P = 0.07), suprasphincteric fistula (P = 0.08), CNR value (P < 0.01), and ADC value (P < 0.01) were potential independent factors for fistula healing. These factors were then fitted in the multivariate analysis, which showed that no alcohol intake history (odds ratio [OR] = 4.46, 95% confidence interval [CI]: 1.16–17.17, P = 0.03), suprasphincteric fistula (OR = 0.17, 95% CI: 0.04–0.78, P = 0.02), CNR value (OR = 0.04, 95% CI: 0.01–0.1, P < 0. 01) and ADC value (OR = 2.78, 95% CI: 1.12–6.89, P = 0.03) were significantly correlated with fistula healing (Table 3).
Nomogram construction
Based on the results of multivariate analysis four independent prognostic factors (alcohol intake history, suprasphincter fistula, CNR value and ADC value) were incorporated to establish a predictive model for fistula healing (Fig. 4). This model was visualized using a nomogram, the usage of which was illustrated with an assumptive patient after surgery for an anal fistula, who did not have a history of alcohol intake, CNR value ≤ 63.51, ADC value > 1.34 × 10− 3 mm2/s and was a suprasphincteric fistula. The number of points for history of alcohol intake, CNR value, ADC value and suprasphincteric fistula was 47, 100, 31, and 0, respectively. A total of 178 points were added to this patient, which represented an approximately 75% chance of the fistula healing.
The nomogram to predict fistula healing by four independent prognostic factors. (To use the nomogram, an individual patient’s value is located on each variable axis, and a line is drawn upward to determine the number of points received for each variable value. The sum of these numbers is located on the Total Points axis, and a line is drawn downward to the healing axes to determine the likelihood of healing.)
Performance of the nomogram in the training and testing cohorts
Figure 5 showed the AUC value of the models in the training and testing cohorts. The AUC value was 0.880 and 0.847 in the training and testing cohorts. Figure 6 showed the calibration and decision curves of the nomogram model for the training and testing cohorts. The calibration curve showed a good correction effect in both cohorts. The decision curve showed that the nomogram may be a useful model for clinical use.
Discussion
To the best of our knowledge, this is the first study to use a nomogram model to predict early postoperative fistula healing. Our findings demonstrate the significant influence of factors such as CNR value, ADC value, alcohol intake history, and suprasphincter fistula on the healing process. After developing and validating the nomogram model in both the training and testing cohorts, we observed strong predictive capability. Thus, we believe that this innovative model has great potential for clinical applications and can provide valuable insights.
MRI has become the technique of choice for imaging anal fistulas because of its ability to identify tracts, define complex anatomies, and detect abscesses [20, 21]. However, most studies have focused primarily on the utility of preoperative MRI in the assessment of anal fistulas. Recently, in a study conducted by Garg, postoperative MRI was used to evaluate the long-term healing and complications of complex fistulas, demonstrating its high accuracy in assessing healing and post-surgical complications [6]. However, MRI performed shortly after surgery may not adequately distinguish between the postoperative inflammatory granulation and persistent fistula activity. In such cases, both the clinical conditions may appear hyperintense on T2W or STIR sequencing, potentially directing to misleading results. While the traditional approach to assessing MRI examinations for anal fistulas involves qualitative interpretation of signal characteristics, emerging techniques allow for the objective measurement of quantitative parameters that may be indicative of fistula activity [7]. A previous study evaluated the ability of DWI MRI to detect active inflammatory diseases through the measurement of ADC values in the fistula tract. The ADC value reflects the extent of water molecule diffusion through tissues [22]. Boruah et al [23] found that DWI with mean ADC calculation had a good performance in differentiating active from the inactive fistulas. Yoshizako et al [24] also proposed that ADC value of DWI is a feasible method for evaluating perianal fistula activity. Our results are consistent with these findings, suggesting that ADC value of healing group is higher than non-healing, and ADC parameter is a significant factor with anal fistula healing by univariate and multivariate logistic regression analysis.
Recently, several studies have evaluated fistula activity using DCE-MRI, with a particular focus on assessing activity in Crohn’s fistulas [9, 10]. LeFrançois et al. [7] combined DWI and DCE-MRI to differentiate active and inactive anal fistulas. Their findings showed that the transient enhancement observed in DCE-MRI measurements improved the assessment of anal fistula activity, suggesting the potential advantages of incorporating DCE sequences for evaluating anal fistula activity. CNR is defined as the ratio of the absolute value of the signal difference between two tissues to the background noise. This represents the relative difference in signal intensity between the two tissues. Previous studies have shown that DCE-CNR values can be used to effectively classify different tissue classes [25]. Generally, the factors that influence CNR are the inherent differences between tissues and the imaging technology used. In this study, cases were selected based on the same sequence and scanning parameters using DCE sequence for measurements across different cases. Consequently, the differences in the CNR values of the actual measured images primarily reflect the inherent differences between tissues. Active fistulas, characterized by pus and granulation tissue, exhibit high signal intensity on the DCE sequence because of the abundant blood vessels in the granulation tissue. This leads to a higher signal intensity compared with the surrounding muscle tissue, resulting in a higher CNR value. Our results showed that the CNR value of the DCE sequence had sufficient sensitivity and high specificity for assessing early-stage fistula healing.
In addition, it is necessary to understand why postoperative MRI examination is required in patients with anal fistulas. In the present study, almost 54.5% of the patients had horseshoe fistulas and 35.5% of the cohort had recurrent fistulas. For these patients, MR imaging can help doctors and patients understand whether the fistula surgery succeed. Occasionally, although the lesion was adequately treated in the first-stage procedure, after a period of seton treatment, there were cases of poor drainage or even non-healing of the fistula branches or around the posterior portion of the seton. In this circumstance, the second-stage procedure not only needs to incise the position of the seton, but also needs to drainage these places to allow them to heal better.
In our study, we observed significant associations between alcohol intake history, and fistula healing. Alcohol consumption can negatively impact wound healing by affecting both the quality and speed of the healing process [26, 27]. A systematic review has reported an increased risk of postoperative complications, including wound complications, in patients with a history of preoperative alcohol consumption [28]. This could be attributed to the potential reduction in the vascular endothelial growth factor caused by alcohol, which led to a decrease in the formation of new blood vessels.
The main risk factors affecting fistula healing are the type of fistula, number of fistula tracts, and height or location of the internal opening. Previous studies have also reported a higher risk of complications and recurrence of complex fistulas, especially suprasphincteric and extrasphincteric fistulas [29, 30]. Consistent with these reports our results revealed a significant association between suprasphincteric fistulas and failure of healing. A suprasphincteric fistula can be seen as an indication of increased complexity of the fistula [31].
This study has several limitations. First, our study was retrospective and conducted at a single center, which means that it was limited in terms of methodology. To overcome this limitation, a multicenter study should be performed to assess the intra- and inter-observer agreement of measurable MRI parameters and to determine the sensitivity and specificity of different MR technologies in diagnosing fistula healing. Second, the retrospective nature of the study limited the ability to establish a definitive relationship between the amount of alcohol intake and anal fistula healing. Future prospective studies with more comprehensive assessments of alcohol intake as an ordinal variable may provide a more accurate understanding of the association between alcohol intake and fistula healing. Finally, the relatively small sample size may have affected the accuracy of the model used. Therefore, it is important to conduct larger studies to improve the validity and generalizability of our findings.
Conclusions
We developed a prognostic model and nomogram for predicting fistula healing and achieved good discrimination calibration. This may allow for the prediction of fistula healing in the early postoperative period and could help in the clinical management of anal fistulas.
Data availability
All analysed data are included in this published article. The original data are available upon reasonable request from the corresponding author.
Abbreviations
- BMI:
-
body mass index
- CI:
-
confidence interval
- ROC:
-
receiver operating characteristic
- AUC:
-
area under the curve
- ADC:
-
apparent diffusion coefficient
- STIR:
-
short tau inversion recovery
- DWI:
-
diffusion-weighted imaging
- DCE:
-
dynamic contrast-enhanced
- IBD:
-
inflammatory bowel disease
- EAS:
-
external anal sphincter
- ROI:
-
region of interest
- CNR:
-
contrast-to-noise ratio
- MRI:
-
magnetic resonance imaging
- OR:
-
odds ratio
- SI:
-
signal intensity
- LAVA:
-
liver acquisition with volume acceleration
References
Sainio P. Fistula-in-ano in a defined population. Incidence and epidemiological aspects. Ann Chir Gynaecol. 1984;73(4):219–24.
Limura E, Giordano P. Modern management of anal fistula. World J Gastroenterol. 2015;21(1):12–20.
Vo D, Phan C, Nguyen L, Le H, Nguyen T, Pham H. The role of magnetic resonance imaging in the preoperative evaluation of anal fistulas. Sci Rep. 2019;9(1):17947.
Holzer B, Rosen HR, Urban M, Anzbock W, Schiessel R, Hruby W. Magnetic resonance imaging of perianal fistulas: predictive value for Parks classification and identification of the internal opening. Colorectal Dis. 2000;2(6):340–5.
Halligan S. Magnetic resonance imaging of Fistula-In-Ano. Magn Reson Imaging Clin N Am. 2020;28(1):141–51.
Garg P. Comparison of preoperative and postoperative MRI after Fistula-in-ano surgery: Lessons Learnt from an audit of 1323 MRI at a single centre. World J Surg. 2019;43(6):1612–22.
Lefrancois P, Zummo-Soucy M, Olivie D, Billiard JS, Gilbert G, Garel J, Visee E, Manchec P, Tang A. Diagnostic performance of intravoxel incoherent motion diffusion-weighted imaging and dynamic contrast-enhanced MRI for assessment of anal fistula activity. PLoS ONE. 2018;13(1):e0191822.
Dohan A, Eveno C, Oprea R, Pautrat K, Place V, Pocard M, Hoeffel C, Boudiaf M, Soyer P. Diffusion-weighted MR imaging for the diagnosis of abscess complicating fistula-in-ano: preliminary experience. Eur Radiol. 2014;24(11):2906–15.
Ziech ML, Lavini C, Bipat S, Ponsioen CY, Spijkerboer AM, Stokkers PC, Nederveen AJ, Stoker J. Dynamic contrast-enhanced MRI in determining disease activity in perianal fistulizing Crohn disease: a pilot study. AJR Am J Roentgenol. 2013;200(2):W170–177.
Horsthuis K, Lavini C, Bipat S, Stokkers PC, Stoker J. Perianal Crohn disease: evaluation of dynamic contrast-enhanced MR imaging as an indicator of disease activity. Radiology. 2009;251(2):380–7.
Qian W, Li Z, Chen W, Yin H, Zhang J, Xu J, Hu C. RESOLVE-DWI-based deep learning nomogram for prediction of normal-sized lymph node metastasis in cervical cancer: a preliminary study. BMC Med Imaging. 2022;22(1):221.
Liu X, Tian J, Wu J, Zhang Y, Wang X, Zhang X, Wang X. Utility of diffusion weighted imaging-based radiomics nomogram to predict pelvic lymph nodes metastasis in prostate cancer. BMC Med Imaging. 2022;22(1):190.
Li S, Yu X, Shi R, Zhu B, Zhang R, Kang B, Liu F, Zhang S, Wang X. MRI-based radiomics nomogram for differentiation of solitary metastasis and solitary primary tumor in the spine. BMC Med Imaging. 2023;23(1):29.
Alvandipour M, Ala S, Tavakoli H, Yazdani Charati J, Shiva A. Ef fi cacy of 10% sucralfate ointment after anal fistulotomy: a prospective, double-blind, randomized, placebo-controlled trial. Int J Surg. 2016;36(Pt A):13–7.
Garg P, Kaur B, Menon GR. Transanal opening of the intersphincteric space: a novel sphincter-sparing procedure to treat 325 high complex anal fistulas with long-term follow-up. Colorectal Dis. 2021;23(5):1213–24.
Stuart KV, Madjedi K, Luben RN, Chua SYL, Warwick AN, Chia M, Pasquale LR, Wiggs JL, Kang JH, Hysi PG, et al. Alcohol, intraocular pressure, and Open-Angle Glaucoma: a systematic review and Meta-analysis. Ophthalmology. 2022;129(6):637–52.
Polsky S, Akturk HK. Alcohol consumption, diabetes risk, and Cardiovascular Disease within diabetes. Curr Diab Rep. 2017;17(12):136.
Purani H, Friedrichsen S, Allen AM. Sleep quality in cigarette smokers: Associations with smoking-related outcomes and exercise. Addict Behav. 2019;90:71–6.
Biswas J, Nelson CB, Runge VM, Wintersperger BJ, Baumann SS, Jackson CB, Patel T. Brain tumor enhancement in magnetic resonance imaging: comparison of signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) at 1.5 versus 3 tesla. Invest Radiol. 2005;40(12):792–7.
Joyce M, Veniero JC, Kiran RP. Magnetic resonance imaging in the management of anal fistula and anorectal sepsis. Clin Colon Rectal Surg. 2008;21(3):213–9.
Halligan S, Stoker J. Imaging of fistula in ano. Radiology. 2006;239(1):18–33.
Li XR, Cheng LQ, Liu M, Zhang YJ, Wang JD, Zhang AL, Song X, Li J, Zheng YQ, Liu L. DW-MRI ADC values can predict treatment response in patients with locally advanced breast cancer undergoing neoadjuvant chemotherapy. Med Oncol. 2012;29(2):425–31.
Boruah DK, Hazarika K, Ahmed H, Borah KK, Borah S, Malakar S, Hajoari N. Role of diffusion-weighted imaging in the evaluation of Perianal Fistulae. Indian J Radiol Imaging. 2021;31(1):91–101.
Yoshizako T, Wada A, Takahara T, Kwee TC, Nakamura M, Uchida K, Hara S, Luijten PR, Kitagaki H. Diffusion-weighted MRI for evaluating perianal fistula activity: feasibility study. Eur J Radiol. 2012;81(9):2049–53.
Goldenberg JM, Berthusen AJ, Cardenas-Rodriguez J, Pagel MD. Differentiation of Myositis-Induced Models of bacterial infection and inflammation with T(2)-Weighted, CEST, and DCE-MRI. Tomography. 2019;5(3):283–91.
Napavichayanun S, Aramwit P. Effect of animal products and extracts on wound healing promotion in topical applications: a review. J Biomater Sci Polym Ed. 2017;28(8):703–29.
Avishai E, Yeghiazaryan K, Golubnitschaja O. Impaired wound healing: facts and hypotheses for multi-professional considerations in predictive, preventive and personalised medicine. EPMA J. 2017;8(1):23–33.
Eliasen M, Gronkjaer M, Skov-Ettrup LS, Mikkelsen SS, Becker U, Tolstrup JS, Flensborg-Madsen T. Preoperative alcohol consumption and postoperative complications: a systematic review and meta-analysis. Ann Surg. 2013;258(6):930–42.
Garcia-Aguilar J, Belmonte C, Wong WD, Goldberg SM, Madoff RD. Anal fistula surgery. Factors associated with recurrence and incontinence. Dis Colon Rectum. 1996;39(7):723–9.
Jordan J, Roig JV, Garcia-Armengol J, Garcia-Granero E, Solana A, Lledo S. Risk factors for recurrence and incontinence after anal fistula surgery. Colorectal Dis. 2010;12(3):254–60.
Boenicke L, Karsten E, Zirngibl H, Ambe P. Advancement Flap for treatment of Complex Cryptoglandular Anal Fistula: prediction of Therapy Success or failure using anamnestic and clinical parameters. World J Surg. 2017;41(9):2395–400.
Acknowledgements
Not applicable.
Funding
This research was sponsored by the Science and Technology Program of Guangzhou, China (No. 202002020081), Natural Science Foundation of Guangdong Province of China (No. 2020A1515011254), National Natural Science Foundation of China (No. 81973847), and National Natural Science Foundation of China (No. 82174369).
Author information
Authors and Affiliations
Contributions
Hong-Cheng Lin and Wen-Ru Li were the principal investigators responsible for the study plan. Hao Xu, Guo-Zhong Xiao, Yi-Hui. Zheng, Yuan-Ji. Fu, Sheng-Lan Zhong, and Dong-Lin Ren drafted the manuscript. Hong-Cheng Lin finalized the manuscript. All the authors have read and approved the final version of this manuscript. Given their contributions to this paper, Hao Xu and Guo-Zhong Xiao may be considered the first co-authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study complied with the standards of the Declaration of Helsinki and the current ethical guidelines. The requirement for informed consent was waived, and approval was granted by the Ethical Committee of the Sixth Affiliated Hospital of Sun Yat-Sen University.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, H., Xiao, GZ., Zheng, YH. et al. A magnetic resonance imaging-based decision-making tool for predicting complex anal fistulas healing in the early postoperative period. BMC Gastroenterol 23, 372 (2023). https://doi.org/10.1186/s12876-023-02963-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-023-02963-5