Abstract
Background and aim
In China, hepatorenal syndrome is a serious complication in the decompensated stage of hepatitis B cirrhosis, which requires early clinical intervention, so the early diagnosis of hepatorenal syndrome is crucial. This study establishes a new predictive model based on serum biomarkers for the early diagnosis of hepatorenal syndrome.
Methods
Patients with decompensated hepatitis B cirrhosis who met the inclusion and exclusion criteria were retrospectively enrolled. Patients were randomly assigned to the training dataset and validation dataset at a 7:3 ratio. Univariate and multivariate logistic regression analyses were used to screen the risk factors for hepatorenal syndrome. The identified risk factors were used to establish and verify a model.
Results
This study included 255 patients with decompensated hepatitis B cirrhosis, including 184 in the training group and 71 in the validation group. The multivariate logistic regression model was established in the training group and verified in the validation group. Logistic regression showed that hemoglobin (OR 0.938, 95% CI 0.908–0.969), total bilirubin (OR 1.014, 95% CI 1.008–1.021) and creatinine (OR 1.079, 95% CI 1.043–1.117) were independent risk factors for hepatorenal syndrome (P < 0.05). These were used to establish the model. In the training group and the validation group, the area under the ROC curve of the nomogram for the diagnosis of hepatorenal syndrome was 0.968 and 0.980, respectively.
Conclusion
The three serum biomarkers, including hemoglobin, total bilirubin and creatinine, can be used as independent early predictors of hepatorenal syndrome in patients with decompensated hepatitis B cirrhosis.
Similar content being viewed by others
Introduction
Hepatorenal syndrome (HRS) is a form of renal insufficiency and is one of the most common severe complications in the late stage of decompensated cirrhosis; it presents as decreased renal blood flow and a decreased glomerular filtration rate (GFR), without significant changes in renal histology [1]. In the past, HRS was considered to be a functional kidney injury, but with the development of pathophysiology, it is now believed that as a functional kidney injury, HRS will also progress to a structural kidney injury. In 2015, the International Ascites Club (IAC) proposed a new definition of acute kidney injury with cirrhosis in terms of the progression of HRS [2], and in 2019, the IAC proposed a new perspective based on the results of relevant clinical studies in recent years [3]. HRS is called hepatorenal syndrome-nonacute kidney injury (HRS-NAKI). Hepatorenal syndrome-acute kidney disease (HRS-AKD) and hepatorenal syndrome-chronic kidney disease (HRS-CKD) are subtypes of HRS-NAKI.
The pathogenesis of HRS is complex and involves many factors. First, portal hypertension dilates visceral blood vessels, leading to renal vasoconstriction, which leads to a decrease in the GFR [4]. Second, the increase in circulating inflammatory mediators [5], bacterial infection [5], cardiac dysfunction [6], and impaired renal tubule function [7] are also important mechanisms of HRS. HRS mostly manifests as acute renal failure in patients with severe liver disease such as cirrhosis, and it is also the main cause of death in advanced cirrhosis patients [8, 9]. The median survival time is 2 weeks to 2 months [10, 11]. Treatment of hepatorenal syndrome should be started as soon as possible after diagnosis. Liver transplantation is the best treatment for hepatorenal syndrome [12]. Drug therapy and renal replacement therapy are usually used as transitional treatments before liver transplantation. Among them, albumin combined with terisopressin is the current preferred drug treatment for hepatorenal syndrome [3, 13, 14]. At present, research on HRS mainly focuses on diagnosis and treatment, and studies on the prediction of HRS are limited, especially the prediction model. At the same time, China is a country with a high prevalence of hepatitis B [15], long-term HBV infection will damage the liver, resulting in a higher incidence rate of Compensated cirrhosis with hepatitis B, which further leads to a higher incidence of HRS in patients with compensated hepatitis B. Therefore, it is important to develop a predictive model for HRS in decompensated hepatitis B cirrhosis and timely intervention.
In this study, we aimed to construct a new model for the early prediction of HRS occurrence by retrospectively studying patients with decompensated hepatitis B cirrhosis from July 2018 to June 2021.
Materials and methods
Patients
This was a single-center, retrospective study. This study recruited patients with decompensated hepatitis B cirrhosis who were hospitalized in Zhejiang Provincial People’s Hospital (Hangzhou, China) between July 2018 and June 2021. Inclusion criteria: (1) patients with Decompensated cirrhosis with or without HRS according to the diagnostic criteria; (2) 18–90 years of age; and (3) Compliance with HRS diagnostic criteria. Exclusion criteria: (1) Patients infected with hepatitis A, C, D, or E virus; (2) Infection with human immunodeficiency virus (HIV); (3) Non-HBV with autoimmune hepatitis (AIH), primary biliary cholangitis (PBC), primary sclerosing cholangitis (PSC), hereditary metabolic liver disease, drug-induced liver injury (DILI) or alcoholic liver disease; (5) Hepatocellular carcinoma; or (6) Incomplete clinical data. The study was approved by the Ethics Committee of Zhejiang Provincial People’s Hospital and conformed to the ethical guidelines of the Helsinki Declaration. Researchers only analyzed anonymous data, so they gave up informed consent.
Laboratory tests, clinical diagnosis and definitions
The baseline variables of patients, including age, sex, and clinical data, were collected. All included patients were subject to routine laboratory tests at admission, including routine blood tests, liver function, renal function, electrolytes, blood lipids, coagulation function, the use of diuretics, esophageal-gastro varices bleeding (EGVB) and bacterial infection. The routine blood examination indexes were white blood cells, neutrophil/lymphocyte ratio and platelets; the liver function indexes were albumin, globulin, alanine aminotransferase, aspartate aminotransferase, and total bilirubin; the renal function indexes were urea and creatinine; the electrolyte index was serum sodium concentration; and the coagulation function indexes were prothrombin time, international standardized ratio and activated partial thromboplastin time. The diagnosis of hepatitis B cirrhosis meet the following criteria (1) and (2) or (1) and (3) [16, 17]: (1) currently HBsAg positive, or HBsAg negative, anti-HBc positive, with a clear history of chronic HBV infection (previous HBsAg positive > 6 months), and excluding other causes; (2) patients whose liver biopsy pathology confirmed liver cirrhosis; and (3) two or more of the following five items were met, except for noncirrhotic portal hypertension: (1) imaging examination showed signs of cirrhosis and/or portal hypertension; (2) endoscopic examination showed esophageal and gastric varices; (3) liver hardness value was consistent with liver cirrhosis; (4) serum biochemical examination showed a decrease in albumin level; and (5) blood routine examination showed platelet count < 100 × 109/L. Decompensated liver cirrhosis: Patients with liver cirrhosis are diagnosed with decompensated liver cirrhosis if they have serious complications such as ascites, gastroesophageal variceal bleeding or hepatic encephalopathy [18]. Its liver function mostly belongs to Child‒Pugh B or C grade. HRS diagnostic criteria: (1) Cirrhosis with ascites; (2) Comply with the diagnostic criteria of liver cirrhosis acute kidney injury (AKI). (3) 48 h of continuous discontinuation of diuretics and albumin (1 g kg−1 d−1) volume expansion therapy was ineffective; (4) No shock; (5) Not taking drugs that can damage the kidney (such as nonsteroidal anti-inflammatory drugs, aminoglycoside antibiotics, iodine contrast agents, etc.) (6) There were no obvious clinical signs of structural renal injury, namely, no proteinuria, no microhaematuria, and no abnormalities in renal imaging, but renal tubule and renal interstitial lesions were not completely excluded. Among them, protein excretion in urine > 500 mg/d, microscopic examination of micro hematuria finger urine sediment per high vision red blood cells < 50 [3].
Statistical analysis
SPSS software (version 26.0, SPSS Inc., IBM, Chicago, IL, USA) was used for statistical analysis of the data. Quantitative variables are expressed as the mean ± standard deviation (SD) or median (25th percentile; 75th percentile) and were compared by independent t test or a nonparametric test (Mann–Whitney). Categorical variables are expressed as numbers (percentages) and were compared by the chi-square test. P < 0.05 was considered statistically significant. The variables that met the criteria in univariate analysis were introduced into multivariate stepwise logistic regression to construct a prediction model in the training set. Both univariate analysis and multivariate analysis showed that P < 0.05 was significantly different. The accuracy of the model for the diagnosis of HRS was evaluated by the area under the ROC curve (AUC). Welch-corrected t-test was used to analyze the model values of the HRS group and the non-HRS group in the training set, the validation set and the whole population. P < 0.05 indicated that the difference was statistically significant.
Results
General characteristics
From July 2018 to June 2021, 438 patients with decompensated cirrhosis, including 325 patients with hepatitis B, were diagnosed in the Department of Infection, Zhejiang Provincial People’s Hospital. Fifty-three patients with malignant liver tumors were excluded from our study. Seventeen patients were excluded due to incomplete clinical data, which resulted in 255 patients being enrolled (Fig. 1). Among all patients, 46 patients had hepatitis B cirrhosis complicated with HRS, and 209 patients did not have HRS. The baseline characteristics are shown in Table 1. The average time from admission to HRS diagnosis in all patients with hepatitis B cirrhosis complicated with HRS was 4.4 days; the longest time was 30 days, and the shortest time was 2 days. A total of 255 patients were randomly divided into a training group and a validation group at a ratio of 7:3. The training group had 184 patients with decompensated hepatitis B cirrhosis, of whom 35 had HRS. There were 71 patients with decompensated hepatitis B cirrhosis in the validation group, including 11 patients with HRS. The baseline characteristics of all enrolled patients are listed in Table 2. There was no significant difference in the parameters between the training set and the validation set (P > 0.05).
Predictors of HRS and formulation of the model
The results of univariate logistic regression analysis with HRS as the dependent variable showed that WBC, NLR, Hb, GLB, TB, BUN, serum creatinine, Na+, PT, APTT and infection might be influencing factors of HRS in patients with decompensated hepatitis B cirrhosis (P < 0.05) in the training set (Table 3). The independent variables with statistically significant differences (P < 0.05) in univariate logistic regression were included in the multivariate logistic regression (stepwise forward/maximum likelihood ratio method). The results suggested that Hb, TB and serum creatinine were independent risk factors for HRS in patients with decompensated hepatitis B cirrhosis (P < 0.05). The corresponding predictive model was constructed (Table 4). The model formula was as follows (hemoglobin is in g/L, total bilirubin is in µmol/L, and creatinine is in µmol/L):
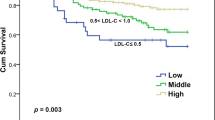
In the training group (t = 10.350, P < 0.0001), the validation group (t = 8.213, P < 0.0001) and the total group (t = 11.830, P < 0.0001), the model score of the HRS group was significantly higher than that of the non-HRS group (Fig. 2A–C).
ROC curves of model values and early diagnosis models in patients with decompensated hepatitis B cirrhosis in the HRS group and the non-HRS group. A In the training set, the model value of the HRS group was significantly higher than that of the non-HRS group (t = 10.350, P < 0.0001). B In the validation set, the model value of the HRS group was significantly higher than that of the non-HRS group (t = 8.213, P < 0.0001). C In all patients, the model value in the HRS group was significantly higher than that in the non-HRS group (t = 11.830, P < 0.0001). D The ROC curve [area under the ROC curve (AUC)] of the model in the training set was 0.968. E ROC curve of the model in the validation set (AUC 0.980). F ROC curve of the model in all patients (AUC 0.969)
Figure 2D shows the ROC curve of the model for the early prediction of HRS in decompensated hepatitis B cirrhosis patients, with an AUC of 0.968 [standard error (SE) 0.011, 95% confidence interval (CI) 0.946–0.989]. The ROC curve of the model for the validation set is shown in Fig. 2E, and its AUC was 0.980 [standard error (SE) 0.014, 95% 0.951–1.000]. The ROC curve of the model for all patients is shown in Fig. 2F, with an AUC of 0.969 (SE 0.009, 95% CI 0.951–0.987).
Based on ROC analysis, the best cutoff value of the model was calculated. When the high cutoff value (> 0.146) is selected to determine which patients have HRS, symptomatic treatment is needed. A lower cutoff value (< 0.146) was used to determine whether patients without HRS could be followed up regularly. The sensitivity, specificity, positive predictive value and negative predictive value of the model were calculated (Table 5). In the training group, when the critical value of the model was 0.146, 22 patients (62.9%) were recommended to start symptomatic treatment, and 13 patients were regularly followed up.
The model performed well on the training set and verification set, with AUCs of 0.968 and 0.980, respectively. A total of 46 patients with decompensated hepatitis B cirrhosis were complicated with HRS in the entire population, of whom 30 (65.2%) could be treated early according to the critical value.
To facilitate clinical application, this study provided a visualization of the prediction model and established the nomogram (Fig. 3A), which can more intuitively express the relationship between the three variables in the prediction model. The calibration curves of the training and validation groups are shown in Fig. 3B, C, and the predicted risk and the actual risk are in good agreement. Additionally, to evaluate the clinical effectiveness of the model, this study drew a decision curve (Fig. 3D, E). The analysis showed that the scoring prediction model had obvious net benefits, suggesting that the prediction model had high clinical application value and met the actual needs of clinical decision-making. Since the AUC of the model in the training group was relatively high and the calibration curve and the decision curve were good, the collinearity of the prediction indexes of the training group was judged. The variance inflation factors (VIFs) of the predictive factors (Hb, TB and serum creatinine) were all less than 5, indicating no collinearity.
Nomo map based on the training group, calibration curve and decision curve based on the validation set. A Displaying the model with visual charts is more suitable for clinical application. B, C Validation of the nomogram prediction accuracy by building calibration curves using validation sets. D, E The decision curve of the validation set shows that the prediction model has obvious net benefits, indicating that the model has high clinical application value
Discussion
The prevalence of hepatitis B virus is a major public health problem not only in China but also worldwide. For patients with decompensated cirrhosis, hepatorenal syndrome is one of the serious complications. Therefore, early prediction and diagnosis of HRS can reduce the incidence [19] and severity [20] of HRS by allowing for early control and prevention of infection, correction of anemia, avoidance of nephrotoxic drugs, and maintenance of blood volume balance.
HRS is a serious complication of renal function damage without obvious organic disease in the kidney that may occur in patients with advanced severe liver disease, and the incidence rate of HRS in patients with cirrhosis is about 19.2%. In this study, we tried to establish a diagnostic model to predict HRS by retrospective analysis of clinical data of HRS patients. It should be pointed out that the laboratory indicators included in this study are all indicators that must be tested on admission, so some unconventional indicators related to renal injury are not included, such as Urine electronics and urine β 2-MG concentrations. Janicko et al. included urine sodium in a study on predictors of alcohol-related cirrhosis with hepatorenal syndrome, but the difference was not statistically significant [21]. At the same time, urinary sodium was not used as a routine test indicator at admission, so we did not include urinary electrolytes in the study of prediction indicators.
In addition, some biomarkers whose predictive value for HRS has not been clearly defined are also excluded from the model established in this study, such as serum cystatin C (CysC) [22, 23], urine neutrophil gelatinase-associated lipocalin (NGAL) [24], serum interleukin-18 (IL-18) [25, 26], serum N-acetyl-β-D glucosaminidase (NAG) [23], urinary kidney injury molecule-1 (KIM-1) [27] and liver-type fatty acid binding protein (LFABP) [28], have been proposed for the detection of HRS [29]. Although these markers have been shown to increase in HRS in patients with cirrhosis [27, 30, 31], the predictive value of these markers for HRS has not been well studied in decompensated cirrhosis patients with normal serum creatinine levels [19]. Therefore, we performed a retrospective study in patients with decompensated hepatitis B cirrhosis with normal serum creatinine levels to study the predictive model for the early prediction of HRS development.
In this study, we constructed a noninvasive model of early HRS in patients with decompensated hepatitis B cirrhosis and a specific algorithm (Fig. 4). The model was constructed with three independent predictors: Hb, TB and scr. The method successfully predicted the diagnosis of 22 training set patients (63%), 5 validation set patients (45%) and 27 full-cohort patients (59%). Therefore, it can predict concurrent HRS in advance, allowing for earlier symptomatic treatment and improving prognosis. Alessandria C et al. also established a model to predict HRS, that is, the diagnostic value of the model of end-stage liver disease (MELD) score Compared with the prediction model of Alessandria C et al., the AUC value of the prediction model established in this study is higher (0.968 vs. 0.896), but the prediction model in this study relies on serum creatinine, while the model of Alessandria C et al. does not rely on serum creatinine.
The following might explain the clinical significance and predictive value of Hb, TB and Cr for the early prediction of HRS. First, anemia is common in patients with advanced liver disease. When the MELD score increases, hemoglobin levels decrease [29]. Anemia can reduce the oxygen supply of the kidney and may lead to microcirculation renal hypoxia or injury, which can cause early renal tubular injury [32, 33], and renal ischemia is the most common cause of HRS. Studies have found that anemia can aggravate HRS in patients with liver cirrhosis [34]. In patients with end-stage renal disease, there was a strong positive correlation between anemia and the risk of adverse prognosis [35]. In this study, we found that Hb was one of the influencing factors for the early prediction of concurrent HRS, which was similar to the above research results.
Second, total bilirubin is divided into direct bilirubin and indirect bilirubin. Most human bilirubin comes from hemoglobin released from aging red blood cells. Indirect bilirubin is transported to the liver through blood and generates direct bilirubin through the action of hepatocytes. The occurrence of liver diseases will affect this process. Serum total bilirubin is an index reflecting the reserve function of the liver. The worse the reserve function of the liver, the more likely patients are to have HRS. Therefore, patients with liver cirrhosis who have obvious liver function damage should be aware of the potential occurrence of HRS. Studies have found that serum total bilirubin concentration may be a new risk factor for chronic kidney disease [36], and serum bilirubin concentration is positively correlated with renal dysfunction [37, 38]. Therefore, we assessed the association between TB and HRS risk and found that TB was one of the factors that could predict concurrent HRS early.
Finally, most guidelines define HRS based on serum creatinine. Adding serum creatinine to the MELD score can reflect the prognostic impact of renal function, predict the likelihood of death within 3 months and rank American patients for organ transplants [39, 40]. In this study, it was found that serum creatinine was one of the influencing factors for the early prediction of concurrent HRS. These results are similar to previous research results [41].
Our prediction model has unique characteristics. It uses only conventional serum markers, which are inexpensive and easy to obtain. Therefore, it would be useful in most medical institutions. At the same time, the diagnostic efficiency (AUC = 0.968) was better than that of the MELD score (AUC = 0.896) [10]. Although the MELD score can effectively evaluate the severity of advanced liver diseases and liver graft allocation [42], it has not been used for the early prediction of HRS.
This study also has several limitations. First, the sample size is relatively small. Before its clinical application, large cohort studies should be conducted. Second, the model was built in a training group, and another group in the same center was randomly selected for validation. Third, serum-specific test indicators can improve the effectiveness of the model. Nonetheless, we believe that external validation of multicenter studies can enhance the effectiveness of the model. However, our main goal is to build a noninvasive model for use in most medical facilities. Many hospitals have no access to data on special test indexes in serum, which limits clinical application.
Conclusion
This study showed that Hb, TB and Cr were independent risk factors for hepatorenal syndrome in patients with decompensated hepatitis B cirrhosis. A simple, rapid, personalized and accurate diagnostic method for HRS is provided by the line chart established by serological indicators and is worthy of application in clinical trials. However, despite the innovativeness of this study, we still need to conduct multicenter and large-sample studies to confirm our findings and develop more effective methods for the early diagnosis of hepatorenal syndrome using line maps.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- OR:
-
Odds ratio
- 95% CI:
-
95% Confidence interval
- ROC:
-
Receiver operator curve
- AUC:
-
Area under the ROC curve
- HRS:
-
Hepatorenal syndrome
- GFR:
-
Glomerular filtration rate
- IAC:
-
International Ascites Club
- HBV:
-
Hepatitis B virus
- SE:
-
Standard error
- MELD:
-
Model of end-stage liver disease
- WBC:
-
White blood cell count
- NLR:
-
Neutrophil to lymphocyte ratio
- Hb:
-
Hemoglobin
- PLT:
-
Platelet count
- ALB:
-
Albumin
- GLB:
-
Globulin
- ALT:
-
Alanine transaminase
- AST:
-
Aspartate transaminase
- TB:
-
Total bilirubin
- BUN:
-
Blood urea nitrogen
- Cr:
-
Creatinine
- Na+:
-
Serum sodium ion concentration
- PT:
-
Prothrombin time
- INR:
-
International normalized ratio
- APTT:
-
Activated partial thromboplastin time
- EGVB:
-
Esophageal-gastro varices bleeding
References
Mindikoglu AL, Pappas SC. New developments in hepatorenal syndrome. Clin Gastroenterol Hepatol. 2018;16(2):162-77.e161.
Angeli P, Gines P, Wong F, Bernardi M, Boyer TD, Gerbes A, Moreau R, Jalan R, Sarin SK, Piano S, et al. Diagnosis and management of acute kidney injury in patients with cirrhosis: revised consensus recommendations of the International Club of Ascites. Gut. 2015;64(4):531–7.
Angeli P, Garcia-Tsao G, Nadim MK, Parikh CR. News in pathophysiology, definition and classification of hepatorenal syndrome: a step beyond the International Club of Ascites (ICA) consensus document. J Hepatol. 2019;71(4):811–22.
Ginès P, Schrier RW. Renal failure in cirrhosis. N Engl J Med. 2009;361(13):1279–90.
Solé C, Solà E, Huelin P, Carol M, Moreira R, Cereijo U, Mas JM, Graupera I, Pose E, Napoleone L, et al. Characterization of inflammatory response in hepatorenal syndrome: relationship with kidney outcome and survival. Liver Int. 2019;39(7):1246–55.
Krag A, Bendtsen F, Henriksen JH, Møller S. Low cardiac output predicts development of hepatorenal syndrome and survival in patients with cirrhosis and ascites. Gut. 2010;59(1):105–10.
Trawalé JM, Paradis V, Rautou PE, Francoz C, Escolano S, Sallée M, Durand F, Valla D, Lebrec D, Moreau R. The spectrum of renal lesions in patients with cirrhosis: a clinicopathological study. Liver Int. 2010;30(5):725–32.
Moreau R. Acute-on-chronic liver failure: a new syndrome in cirrhosis. Clin Mol Hepatol. 2016;22(1):1–6.
Bucsics T, Mandorfer M, Schwabl P, Bota S, Sieghart W, Ferlitsch A, Trauner M, Peck-Radosavljevic M, Reiberger T. Impact of acute kidney injury on prognosis of patients with liver cirrhosis and ascites: a retrospective cohort study. J Gastroenterol Hepatol. 2015;30(11):1657–65.
Alessandria C, Ozdogan O, Guevara M, Restuccia T, Jiménez W, Arroyo V, Rodés J, Ginès P. MELD score and clinical type predict prognosis in hepatorenal syndrome: relevance to liver transplantation. Hepatology (Baltimore MD). 2005;41(6):1282–9.
Cárdenas A. Hepatorenal syndrome: a dreaded complication of end-stage liver disease. Am J Gastroenterol. 2005;100(2):460–7.
Boyer TD, Sanyal AJ, Garcia-Tsao G, Regenstein F, Rossaro L, Appenrodt B, Gülberg V, Sigal S, Bexon AS, Teuber P. Impact of liver transplantation on the survival of patients treated for hepatorenal syndrome type 1. Liver Transplant. 2011;17(11):1328–32.
Sanyal AJ, Boyer TD, Frederick RT, Wong F, Rossaro L, Araya V, Vargas HE, Reddy KR, Pappas SC, Teuber P, et al. Reversal of hepatorenal syndrome type 1 with terlipressin plus albumin vs. placebo plus albumin in a pooled analysis of the OT-0401 and REVERSE randomised clinical studies. Aliment Pharmacol Ther. 2017;45(11):1390–402.
Arroyo V, Terra C, Ginès P. Advances in the pathogenesis and treatment of type-1 and type-2 hepatorenal syndrome. J Hepatol. 2007;46(5):935–46.
Yuen MF, Yuan HJ, Wong DK, Yuen JC, Wong WM, Chan AO, Wong BC, Lai KC, Lai CL. Prognostic determinants for chronic hepatitis B in Asians: therapeutic implications. Gut. 2005;54(11):1610–4.
Wu X, Zhou J, Xie W, Ding H, Ou X, Chen G, Ma A, Xu X, Ma H, Xu Y, et al. Entecavir monotherapy versus de novo combination of lamivudine and adefovir for compensated hepatitis B virus-related cirrhosis: a real-world prospective multicenter cohort study. Infect Drug Resist. 2019;12:745–57.
Suk KT, Baik SK, Yoon JH, Cheong JY, Paik YH, Lee CH, Kim YS, Lee JW, Kim DJ, Cho SW, et al. Revision and update on clinical practice guideline for liver cirrhosis. Korean J Hepatol. 2012;18(1):1–21.
D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44(1):217–31.
Gifford FJ, Morling JR, Fallowfield JA. Systematic review with meta-analysis: vasoactive drugs for the treatment of hepatorenal syndrome type 1. Aliment Pharmacol Ther. 2017;45(5):593–603.
Hung TH, Lay CJ, Tseng CW, Tsai CC, Tsai CC. The effect of renal function impairment on the mortality of cirrhotic patients: a nationwide population-based 3-year follow-up study. PLoS ONE. 2016;11(9):e0162987.
Janicko M, Veseliny E, Senajova G, Jarcuska P. Predictors of hepatorenal syndrome in alcoholic liver cirrhosis. Biomed Pap Med Fac Univ Palacky Olomouc Czech. 2015;159(4):661–5.
Sharawey MA, Shawky EM, Ali LH, Mohammed AA, Hassan HA, Fouad YM. Cystatin C: a predictor of hepatorenal syndrome in patients with liver cirrhosis. Hep Int. 2011;5(4):927–33.
Kim TH, Lee HA, Seo YS, Lee YR, Yim SY, Lee YS, Suh SJ, Jung YK, Kim JH, An H, et al. Assessment and prediction of acute kidney injury in patients with decompensated cirrhosis with serum cystatin C and urine N-acetyl-β-D-glucosaminidase. J Gastroenterol Hepatol. 2019;34(1):234–40.
Barreto R, Elia C, Solà E, Moreira R, Ariza X, Rodríguez E, Graupera I, Alfaro I, Morales-Ruiz M, Poch E, et al. Urinary neutrophil gelatinase-associated lipocalin predicts kidney outcome and death in patients with cirrhosis and bacterial infections. J Hepatol. 2014;61(1):35–42.
Parikh CR, Mishra J, Thiessen-Philbrook H, Dursun B, Ma Q, Kelly C, Dent C, Devarajan P, Edelstein CL. Urinary IL-18 is an early predictive biomarker of acute kidney injury after cardiac surgery. Kidney Int. 2006;70(1):199–203.
Parikh CR, Jani A, Mishra J, Ma Q, Kelly C, Barasch J, Edelstein CL, Devarajan P. Urine NGAL and IL-18 are predictive biomarkers for delayed graft function following kidney transplantation. Am J Transplant. 2006;6(7):1639–45.
Belcher JM, Sanyal AJ, Peixoto AJ, Perazella MA, Lim J, Thiessen-Philbrook H, Ansari N, Coca SG, Garcia-Tsao G, Parikh CR. Kidney biomarkers and differential diagnosis of patients with cirrhosis and acute kidney injury. Hepatology (Baltimore MD). 2014;60(2):622–32.
Wen Y, Parikh CR. Current concepts and advances in biomarkers of acute kidney injury. Crit Rev Clin Lab Sci. 2021;58(5):354–68.
Yap DY, Seto WK, Fung J, Chok SH, Chan SC, Chan GC, Yuen MF, Chan TM. Serum and urinary biomarkers that predict hepatorenal syndrome in patients with advanced cirrhosis. Dig Liver Dis. 2017;49(2):202–6.
Bagshaw SM, Bellomo R. Cystatin C in acute kidney injury. Curr Opin Crit Care. 2010;16(6):533–9.
Liangos O, Perianayagam MC, Vaidya VS, Han WK, Wald R, Tighiouart H, MacKinnon RW, Li L, Balakrishnan VS, Pereira BJ, et al. Urinary N-acetyl-beta-(D)-glucosaminidase activity and kidney injury molecule-1 level are associated with adverse outcomes in acute renal failure. J Am Soc Nephrol. 2007;18(3):904–12.
Güngör G, Akyıldız M, Keskin M, Solak Y, Gaipov A, Bıyık M, Çifçi S, Ataseven H, Polat H, Demir A. Is there any potential or additive effect of anemia on hepatorenal syndrome? Turk J Gastroenterol. 2016;27(3):273–8.
Legrand M, Mik EG, Johannes T, Payen D, Ince C. Renal hypoxia and dysoxia after reperfusion of the ischemic kidney. Mol Med (Cambridge Mass). 2008;14(7–8):502–16.
Bizid S, Yacoub H, Mohamed G, Ben Slimane B, Boughoula K, Ben Abdallah H, Bouali R, Abedelli N. Does anemia have a potential effect on type 2 hepatorenal syndrome? Can J Gastroenterol Hepatol. 2020;2020:1134744.
Schmid H, Schiffl H. Erythropoiesis stimulating agents and anaemia of end-stage renal disease. Cardiovasc Hematol Agents Med Chem. 2010;8(3):164–72.
Tanaka M, Fukui M, Okada H, Senmaru T, Asano M, Akabame S, Yamazaki M, Tomiyasu K, Oda Y, Hasegawa G, et al. Low serum bilirubin concentration is a predictor of chronic kidney disease. Atherosclerosis. 2014;234(2):421–5.
Perlstein TS, Pande RL, Beckman JA, Creager MA. Serum total bilirubin level and prevalent lower-extremity peripheral arterial disease: National Health and Nutrition Examination Survey (NHANES) 1999 to 2004. Arterioscler Thromb Vasc Biol. 2008;28(1):166–72.
Adin CA, Croker BP, Agarwal A. Protective effects of exogenous bilirubin on ischemia-reperfusion injury in the isolated, perfused rat kidney. Am J Physiol Ren Physiol. 2005;288(4):F778–84.
Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, Kremers W, Lake J, Howard T, Merion RM, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124(1):91–6.
Freeman RB. MELD: the holy grail of organ allocation? J Hepatol. 2005;42(1):16–20.
Janičko M, Veselíny E, Abraldes JG, Jarčuška P. Serum sodium identifies patients with cirrhosis at high risk of hepatorenal syndrome. Z Gastroenterol. 2013;51(7):628–34.
Angeli P, Gines P. Hepatorenal syndrome, MELD score and liver transplantation: an evolving issue with relevant implications for clinical practice. J Hepatol. 2012;57(5):1135–40.
Acknowledgements
Not applicable.
Funding
There is no financial support for this article.
Author information
Authors and Affiliations
Contributions
HYP designed the study. SHW and ZWZ wrote the main manuscript text. CAX, HZC, WYR and XDY collected the data and reviewed the manuscript. QQY and WZ analyzed the data. All authors approved the final version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of Zhejiang Provincial People’s Hospital and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, S., Zhou, Z., Xu, C. et al. Establishment and evaluation of an early prediction model of hepatorenal syndrome in patients with decompensated hepatitis B cirrhosis. BMC Gastroenterol 23, 1 (2023). https://doi.org/10.1186/s12876-022-02618-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-022-02618-x