Abstract
Background
Intermittent fasting (IF) during the month of Ramadan is part of the religious rituals of Muslims. The effect of intermittent fasting on disease activity in inflammatory bowel diseases (IBD) is still unknown. This is the first study to assess the effect of IF during Ramadan on inflammatory markers in patients diagnosed with IBD. The effects on clinical disease activity, quality of life, and levels of depression were also assessed.
Methods
Patients diagnosed with ulcerative colitis (UC) or Crohn’s disease (CD) who intended to observe Ramadan fasting were recruited. The following were assessed immediately before and at the end of Ramadan: Serum CRP and stool calprotectin, partial Mayo score, Harvey Bradshaw index (HBI), Simple IBD questionnaire (SIBDQ), and Hamilton depression scale questionnaire.
Results
80 patients diagnosed with IBD were recruited (60 UC, 20 CD). Serum CRP and stool calprotectin did not show a significant change before vs after fasting (median CRP 0.53 vs 0.50, P value = 0.27, Calprotectin 163 vs 218 respectively, P value = 0.62). The partial Mayo score showed a significant rise after fasting (median 1 before vs 1 after fasting, mean: 1.79 vs 2.33 respectively, P value = 0.02). Harvey-Bradshaw index did not show a significant change after fasting (median 4 vs 5, P value = 0.4). Multiple linear regression revealed that older age and a higher baseline calprotectin were associated with a higher change in Mayo score after fasting (P value = 0.02 and P value = 0.01, respectively). No significant change was detected in SIBDQ or Hamilton depression scale scores.
Conclusions
In patients diagnosed with UC, IF during Ramadan was associated with worsening of clinical parameters, the effect was more pronounced in older patients and those with higher baseline calprotectin levels. However, IF during Ramadan was not associated with an adverse effect on objective inflammatory markers (CRP and calprotectin).
Similar content being viewed by others
Introduction
Ramadan is the ninth month of the lunar calendar and is considered a Holy month in the beliefs of about 2 billion Muslims all over the world. Fasting throughout the daytime during the month of Ramadan is considered one of the pillars of Islam, and except for pregnant women, the sick, and the elderly, all adult Muslims are expected to fast every day throughout this month. Fasting during Ramadan is one of the intermittent fasting (IF) regimens that mimics several protocols used frequently for weight loss and other health benefits, especially the time-restricted eating (TRE) [1,2,3] Ramadan intermittent fasting (RIF) entails a complete abstinence from food and liquids from dawn to sunset. Counselling patients with IBD on whether fasting will benefit or harm their bowel condition remains difficult due to the lack of studies on this issue.
The term IF encompasses several regimens of fasting such as alternate day fasting and fast-mimicking diet, yet most commonly it refers to time-restricted eating which usually lasts between 12 to 16 h daily [2]. Intermittent fasting has become a point of interest for researchers as beneficial effects on health have been demonstrated [3,4,5]. On the other hand, some studies have warned of possible deleterious effects of IF on some health conditions [6, 7]. The ability of IF to reduce systemic inflammation has been of particular interest, when considering RIF in particular, basic research has shown mostly a positive impact on inflammatory and oxidative stress markers, many of which are involved in the pathogenesis of IBD such as IL-1, TNF-alpha, IL-1 beta, and C-reactive protein (CRP) [8, 9]. Clinical studies on RIF in autoimmune disorders such as rheumatoid arthritis (RA) and psoriasis have shown improved activity indices and a reduction in inflammatory markers in both diseases after a period of RIF [10, 11]. Whether this effect will be replicated in inflammatory bowel diseases is still unknown. Only the clinical effect of RIF on patients diagnosed with IBD has been reported in 2 studies; one reported no clinical deterioration while the other reported some improvement in clinical parameters [12, 13]. Two studies are currently underway to assess fasting-mimicking diet and intermittent reduced-calories diet as therapeutic tools in IBD [14, 15].
To our knowledge, no study to date has assessed the effects of RIF on inflammatory markers in IBDs. In this study, we assessed the impact of RIF on serum CRP and faecal calprotectin (fCal), as well as disease activity indices, quality of life, and depression scales in patients diagnosed with IBD.
Methods
This was a prospective observational cohort study during the lunar month of Ramadan 2021 (1442 Hijri year). The study was performed at 2 tertiary referral centres for IBD in Egypt: The integrated clinical and research centre for intestinal disorders, Cairo University, and the Inflammatory bowel diseases clinic, endemic medicine department, Ain Shams University. All patients who were independently willing to fast during the month of Ramadan this year were assessed for eligibility. Inclusion criteria included: Age ≥ 18 years of age and less than 70 years, on the same drug regimen for the past 12 weeks at least with no plan to change drug regimen within the coming month and known adherence to medications. Exclusion criteria included: any change in medications dosage or type during the previous 12 weeks, history of perforation of the bowel or megacolon, active infection, presence of other systemic diseases (such as diabetes, cardiovascular diseases, or any other disorder that may be aggravated by fasting), elevated serum creatinine above normal, elevated transaminases > 2 × ULN and known alcohol or drug abuse. Patients on immunomodulators, biological therapies, or corticosteroids were not excluded from the study (unless a change in dose within the following month is anticipated).
During the month before Ramadan, all eligible patients from our IBD registries were contacted. No instruction or recommendation to fast was given to any patient. However, patients were advised not to fast if they had experienced previous harmful effects from fasting or if they had any other comorbidities that could be exacerbated by fasting (e.g., uncontrolled diabetes). Ethical committee approval was obtained in both centers (approval numbers: N-27–2021, R 93/2021). After a written informed consent, assessments were done twice at the following time points: the first, during the week immediately before Ramadan, the second, during the last 3 days of Ramadan or 3 days immediately after Ramadan.
Assessments included: inflammatory markers (CRP, fCal), clinical disease activity (partial Mayo score for patients with UC and Harvey Bradshaw index (HBI) for patients with CD), quality of life (short inflammatory bowel disease questionnaire, SIBDQ), and depression levels (Hamilton depression rating scale) [16,17,18,19].
Fasting details
Fasting for Muslims during the month of Ramadan entails complete abstinence from food and liquids intake, smoking, and sexual activities from dawn to sunset. In Egypt, this year at the start of Ramadan sunrise was at 3:59 while the sunset was at 18:23, i.e., a duration of just more than 14 h of complete fasting, by the end of Ramadan this reached 15 h of fasting a day due to the lengthening of daytime. At night, between sunset and dawn, there is no restriction to any type of the usual Halal food or liquids intake.
Assessment of disease activity
Quantitative fCal levels were assessed by ELISA technique (ORG 580 kit, Orgentec diagnostika GmbH). CRP level assessment was done using nephelometry methodology (mispa-i2, Agappe Diagnostics GmbH). Blood sampling included a 5 cc whole blood sample taken in the morning after an 8 h fast, samples taken during Ramadan were shifted to noon only if a late sohour meal was taken and thus ensure an 8 h fast. Clinical disease activity was assessed by either the HBI in cases of CD or the partial Mayo score in cases of UC.
Quality of life and depression questionnaires
The SIBDQ consists of ten questions from the Inflammatory Bowel Disease Questionnaire (IBDQ) that record disease-specific quality-of-life on bowel-, systemic-, emotional- and social subscales [19]. An overall score can be calculated and ranges from 10 to 70. This self-administered questionnaire was translated according to Behling and Law's technique [20]. We appointed three translators with excellent proficiency in both Arabic and English languages. The first translator translated the original version into Arabic. The second translator back-translated the translated version into English. The third translator compared the original and back-translated versions and prepared the final draft with minor modifications to adjust to Egyptian patients. The assessment of depression was performed by the Hamilton depression score, this has already been translated and validated in Arabic [21].
Statistical analysis
Wilcoxon Signed Ranks test was used to compare different parameters before and after Ramadan fasting, change in different scores and lab investigations (CRP and fCal) was calculated by subtracting the value before fasting from the value after fasting, then multiple linear regression analysis was done to measure the independent effect of different parameters on these changes. Analysis of data was done using SPSS program version 25. Quantitative variables were presented as median and Interquartile range (IQR). Qualitative variables were presented as count and percentage. P value < 0.05 was considered statistically significant.
Sample size: To our knowledge, this was the first study to assess the effect of intermittent/Ramadan fasting on inflammatory markers in inflammatory bowel diseases. In this respect, this is considered a pilot study, and thus no power-based sample size estimate was possible or appropriate. We chose to include all our clinic patients meeting the inclusion criteria with a minimum of 50 subjects for our primary outcome measure: CRP and fCal levels (according to the estimate by Sim and Lewis, the minimum recommended number of subjects for a pilot clinical study is 50) [22].
Results
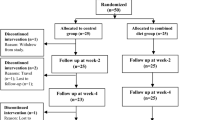
Out of 88 eligible patients contacted, 80 patients (91%) were intending to fast during Ramadan and were included: 60 UC and 20 CD, median age 32 years (range 18–64 years), 41 males & 39 females (Table 1). Forty patients (50%) were on biologics (33 Infliximab, 4 adalimumab, 2 ustekinumab, 1 vedolizumab), 57 (71%) were on immunomodulators (55 azathioprine, 1 mycophenolate mofetil, 1 methotrexate), 51 (64%) on oral mesalamine and 15 (19%) were on low-dose oral steroids (< 10 mg prednisolone). The median partial Mayo score was 1 (range 0–6), median HBI was 5 (range 0–15). During the study, one patient had an iatrogenic perforation during a routine screening colonoscopy and was thus excluded from the study. Two UC patients stopped fasting due to deterioration of their condition after 20 and 22 days, their assessments were performed at the time of stopping and were not excluded. Both patients had resolution of their symptoms by oral prednisolone 20 mg. No other patient required dose adjustment or change in medication during the study period. No hospitalizations or ER visits were recorded during the study period.
Serum CRP did not show a significant change before vs after fasting (median 0.53 vs. 0.50 mg/dl respectively, P value = 0.27) (Table 2). fCal did not differ significantly before vs after fasting (median 163 vs. 218 mcg/g respectively, P value = 0.62). In UC patients, the median partial Mayo score showed a statistically significant rise after fasting (1 before vs. 1 after, P value = 0.02, mean: 1.79 vs 2.33 respectively), while in CD patients the median HBI did not differ significantly before vs. after fasting (4 vs. 5 respectively, P value = 0.41). SIBDQ score showed no significant difference before vs after fasting (median 43 vs. 40 respectively, p P value = 0.12). Hamilton depression scale score was also similar before and after fasting (median 18 v. 18 respectively, P value = 0.81) as shown in Table 2.
A subgroup analysis was performed to assess factors associated with the significant rise in partial Mayo score (Table 3). The following groups showed a significant association with worsening partial Mayo score after fasting: older patients, males, those with a lower baseline Mayo score, and those with higher baseline fCal levels (Table 3). However, multiple linear regression analysis revealed that only higher age and higher baseline fCal were significantly associated with a rise in partial Mayo score after fasting (P value = 0.02 and P value = 0.01, respectively) (Table 4).
Discussion
IBD was typically considered a “Western” disease, seldom being encountered in Eastern countries with a higher Muslim population. The situation is changing, however, with more and more eastern, Muslim predominant countries showing a rising prevalence of IBD over the last 2 decades [23]. This translated to a pressing need to know and inform these patients whether fasting during the month of Ramadan could benefit or harm their condition.
The results of numerous preclinical studies favour the idea that fasting may be able to shift the immune environment from pro- to anti-inflammatory and thus have a beneficial role in autoimmune disorders [24]. An important concept in favour of the anti-inflammatory effect of fasting is the shift in immune cell behaviour according to nutrient availability and abundance [25,26,27]. The mechanistic target of rapamycin (mTOR) for example, an intracellular energy sensor, increases TH1 and TH17 differentiation in the case of an abundance of calories, whilst decreased activation (with caloric restriction) leads to Treg cell differentiation, potentially creating a more anti-inflammatory environment [28]. In multiple sclerosis, 3-day fasting-mimicking diet in mice was found to induce apoptosis of autoimmune Th1 and Th17 cells and enhanced the expansion of the Treg cell population [29]. Intestinal dysbiosis in IBD is characterized by low microbial diversity, decreased Bifidobacterium spp, Lactobacillus spp, and Faecalibacterium prausnitzii, and increased pathobionts such as invasive E. coli and C.diff resulting in decreased butyrate production [30,31,32,33,34,35]. Butyrate has powerful anti-inflammatory properties promoting Treg cell proliferation and improving intestinal barrier function [25]. Fasting has been found to increase Faecalibacterium prausnitzii and Akkermansia mucinophilia, both have been deemed to characterize an anti-inflammatory intestinal environment [24]. Despite the results of these studies favouring the effect of fasting in IBD, immune suppression as a result of prolonged fasting may in theory depress the protective response to pathogens, some which could potentially be implicated in the augmentation of inflammation in IBD. Clinical studies have shown a positive effect of fasting on body weight and adiposity, cardiovascular health, asthma, liver enzymes, and multiple sclerosis [8, 36,37,38,39,40,41,42]. The benefit of fasting in autoimmune disorders such as RA and psoriasis has been demonstrated in clinical controlled trials, sparking enthusiasm on whether these results will be mirrored in other autoimmune disorders such as IBD [10, 11]. Interestingly, a study has shown that RIF in obese individuals (not diagnosed with IBD) decreased proinflammatory adipokines such as TNF-α and IL6 (known to have a role in IBD), and promoted anti-inflammatory IL10 known to have a protective role in the intestinal mucosa [8]. However, a recent study on fasting in hospitalized patients with IBD (a form of fasting quite different from RIF) has shown no benefit compared to enteral nutrition [43].
Our results showed a statistically significant rise in partial Mayo score after fasting throughout the month of Ramadan. Calprotectin also showed a rise yet it did not demonstrate a statistical significance, nevertheless, this rise is supportive of the finding that the Mayo score did rise after fasting. Two UC patients had to stop fasting due to the deterioration of their condition while fasting. To our knowledge, two previous studies assessed the effect of RIF on patients with IBD, they did not assess CRP or calprotectin [12, 13]. One of the studies showed a reduction in UC activity index after fasting, however, in this study only 5 patients fasted throughout the month, a number too small to draw any solid conclusion [12]. The other study by Elmountassir et al. conducted on 100 CD patients concluded that fasting was well tolerated by 94% of patients, but no assessment of disease activity indices was performed [13]. Our results are also in contradiction to what was previously reported in rheumatologic diseases such as RA and psoriasis, where some studies have shown an improvement in activity indices as well as a reduction in CRP [10, 11]. One pilot study in systemic lupus erythematosus (SLE), however, showed no effect on disease activity but a significant rise in Anti-dsDNA [44]. IBD shares similar pathophysiological sequences with several other autoimmune disorders and thus treatment is usually very similar. Major differences, however, do exist and can reflect greatly on the clinical management of such patients, e.g. anti-IL17 medications used to treat RA have a deleterious effect on disease activity in IBD [45]. In addition, the fact that IBD is predominantly a pathology of the intestines, makes it vulnerable to different effects of fasting other than those to which rheumatological disorders are exposed. Therefore, it remains plausible that the effects of fasting could be conflicting between IBD and other autoimmune disorders.
It has to be taken into account that RIF includes other factors that could influence disease activity. The timing of oral medications is changed during Ramadan due to the inability to take any medications during the daytime. Many patients who usually take medications twice a day are forced to take them either once a day or with a much smaller interval in between, this may affect compliance to taking the medications with several doses possibly being missed altogether. Sleeping patterns are also usually changed during the month of Ramadan with a possible effect on circadian rhythm [46,47,48,49]. Circadian cycle proteins and hormones have a direct effect on the inflammatory response and have shown pro- or anti-inflammatory effects in animal models of autoimmune diseases [49]. These peculiarities of Ramadan fasting mean that it remains important not to apply our results to all types of intermittent fasting.
Our study did not show a statistically recognizable effect on inflammatory markers (CRP and stool calprotectin), despite the numbers showing a trend for a rise. It can be argued that a larger sample size is required to demonstrate this difference. A systematic review assessing the effect of RIF on inflammatory markers in healthy adults concluded that minimal reductions in Il-1 and CRP and small reductions in Il-6 and TNF-α were noted after RIF [50]. Whether these small reductions are related only to the weight loss achieved by RIF is yet to be concluded [50]. The largest meta-analysis to date on the effects of intermittent fasting (other than RIF) on inflammatory markers (in non-IBD patients) has shown a reduction in CRP after fasting, predominantly in obese individuals and importantly, those who follow intermittent fasting for more than 8 weeks, a condition not met in the one-month Ramadan fasting [51]. Notably, this large study also demonstrated no effect on IL-6 and TNF-α, pivotal cytokines in the pathogenesis of IBD [52]. These facts could partially explain why RIF did not demonstrate an improvement in inflammatory markers in IBD patients.
Our multiple logistic regression revealed that older patients and those with higher baseline fCal are more prone to deterioration in their partial Mayo score. A higher baseline fCal is known to be associated with a higher risk of clinical relapse in asymptomatic IBD patients [53]. It is thus rational that those with a higher baseline fCal will be the most prone to clinical deterioration when an inciting factor (fasting) is present. Older patients are more prone to negative effects of fasting such as dehydration and hypoglycaemia, the symptoms of which might raise the “physician global assessment” part of the partial Mayo score [54]. Elderly patients also more commonly have comorbidities and have polypharmacy problems that are compounded during the month of Ramadan. Whether age independently is a factor associated with disease relapse during fasting requires larger studies for confirmation, but for now, it seems sensible to inform elderly patients with UC about the possible deleterious effects of fasting and keep those who do fast on a strict follow-up.
The SIBDQ score showed no significant change after fasting. This could lead to the conclusion that if fasting is associated with a negative effect on IBD, then it does not seem to be significant enough to affect the quality of life of patients related to the disease, this needs to be confirmed however by a study with a larger number of patients. SIBDQ also assesses symptoms within the previous 2 weeks, it might thus be less sensitive to changes that occur within a short period such as a month, in comparison to Mayo score which assesses symptoms in the previous 3 days. We assessed the Hamilton depression scale before and after fasting to negate any possibility that any change in activity indices would be secondary to a change in mood and psychiatric status of the patients. Our results show no significant change in the depression index after fasting. Several other studies on healthy volunteers and different medical conditions have shown contradicting results on the effect of fasting on depression and mood disorders [55,56,57].
Our study has some notable limitations; first, the lack of a control group where IBD patients would not fast during Ramadan would provide more concrete evidence for our results. Second, a few variables that hypothetically could affect results were not assessed, such as sleep patterns and compliance with medications. The type of diet is also a potential confounder as types of foods may change during Ramadan, especially with an increase in high-calorie foods or overeating, this should be assessed in future studies by a food diary [59, 60]. Third, assessments of disease activity using ultrasound and/or endoscopy were not performed, these could have added confidence to the results. It remains difficult however to get patients to do a colonoscopy twice within one month, it is also difficult logistically for an endoscopy unit to get a large number of patients to have a colonoscopy within one week from the end of Ramadan.
In conclusion, IF for 14 to 15 h during the month of Ramadan did not seem to significantly affect CRP and fCal levels in patients diagnosed with IBD. However, in UC patients, especially older ones, and those with a higher baseline fCal, RIF was associated with a deterioration in their clinical activity indices. Larger studies are required to confirm our initial findings, but for now, it seems prudent to counsel patients diagnosed with IBD that intermittent (Ramadan) fasting is allowed but with caution and vigilance, especially in older UC patients and those with a baseline calprotectin above normal.
Availability of data and materials
All data generated or analysed during this study are included in this published article. Availability and implementation VCFvariance.pl is a Perl script available at https://github.com/kfletcher88/VCFvariance.
References
Ismail S, Manaf RA, Mahmud A. Comparison of time-restricted feeding and Islamic fasting: a scoping review. East Mediterr Health J. 2019;25(4):239–45.
Patterson R, Sears D. Metabolic Effects of Intermittent Fasting. Annu Rev Nutr. 2017;37(1):371–93.
de Cabo R, Mattson MP. Effects of intermittent fasting on health, aging, and disease. N Engl J Med. 2019;381:2541–51.
Anton SD, Moehl K, Donahoo WT, et al. Flipping the metabolic switch: understanding and applying the health benefits of fasting. Obesity. 2018;26:254–68.
Harvie MN, Pegington M, Mattson MP, et al. The effects of intermittent or continuous energy restriction on weight loss and metabolic disease risk markers: a randomized trial in young overweight women. Int J Obes (Lond). 2011;35:714–27.
Nakamura Y, Walker BR, Ikuta T. Systematic review and meta-analysis reveals acutely elevated plasma cortisol following fasting but not less severe calorie restriction. Stress. 2015;19:1–21.
Kahraman S, Dogan A. Ventricular arrhythmia linked to long intermittent fasting. J Electrocardiol. 2020;58:125–7.
Faris MAE, Madkour MI, Obaideen AK, et al. Effect of Ramadan diurnal fasting on visceral adiposity and serum adipokines in overweight and obese individuals. Diabetes Res Clin Pract. 2019;153:166–75.
Faris MA, Kacimi S, Al-Kurd RA, et al. Intermittent fasting during Ramadan attenuates proinflammatory cytokines and immune cells in healthy subjects. Nutr Res. 2012;32:947–55.
Adawi M, Damiani G, Bragazzi N, et al. The impact of intermittent fasting (Ramadan fasting) on psoriatic arthritis disease activity, enthesitis, and dactylitis: a multicentre study. Nutrients. 2019;11(3):601.
Ben Nessib D, Maatallah K, Ferjani H, et al. Impact of Ramadan diurnal intermittent fasting on rheumatic diseases. Clin Rheumatol. 2020;39:2433–40.
Tavakkoli H, Haghdani S, Emami M, et al. Ramadan fasting and inflammatory bowel disease. Indian J Gastroenterol. 2008;27:239–41.
El Mountassir M, Benelbarhdadi I, Borahma M, et al. Impact of Ramadan on Crohn’s disease. Gastroenterol Hepatol Endosc. 2021;6:1–2.
Effects of an intermittent reduced calorie diet on Crohn's disease. ClinicalTrials.gov identifier: NCT04147585. Accessed 20 March 2022. https://clinicaltrials.gov/ct2/show/NCT04147585.
The Influence of a Fasting Mimicking Diet on Ulcerative Colitis. ClinicalTrials.gov Identifier: NCT03615690. Accessed 20 Mar 2022. https://clinicaltrials.gov/ct2/show/NCT03615690.
Lewis J, Chuai S, Nessel H, et al. Use of the noninvasive components of the Mayo score to assess clinical response in ulcerative colitis. Inflamm Bowel Dis. 2008;14:1660–6.
Harvey R, Bradshaw J. A simple index of Crohn’s-disease activity. Lancet. 1980;1(8167):514.
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62.
Jowett SL, Seal CJ, Barton JR, et al. The short inflammatory bowel disease questionnaire is reliable and responsive to clinically important change in ulcerative colitis. Am J Gastroenterol. 2001;96:2921–8.
Behling O, Law KS. Translating Questionnaires and Other Research Instruments: Problems and solutions. SAGE Publications Inc, Thousand Oaks. 2000. https://doi.org/10.4135/9781412986373.
Obeid S, Abi Elias Hallit C, Haddad C. Validation of the Hamilton Depression Rating Scale (HDRS) and sociodemographic factors associated with Lebanese depressed patients. Encephale. 2018;44:397–402.
Sim J, Lewis M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J Clin Epidemiol. 2012;65:301–8.
GBD 2017 Inflammatory Bowel Disease Collaborators. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol 2020;5:17–30.
Remely M, Hippe B, Geretschlaeger I, et al. Increased gut microbiota diversity and abundance of Faecalibacterium prausnitzii and Akkermansia after fasting: a pilot study. Wien Klin Wochenschr. 2015;127:394–8.
Celiberto LS, Graef FA, Healey GR, et al. Inflammatory bowel disease and immunonutrition: novel therapeutic approaches through modulation of diet and the gut microbiome. Immunology. 2018;155:36–52.
O’Neill LAJ, Kishton RJ, Rathmell J. A guide to immunometabolism for immunologists. Nat Rev Immunol. 2016;16:553–65.
Buck MD, Sowell RT, Kaech SM, Pearce EL. Metabolic instruction of immunity. Cell. 2017;169:570–86.
Ma L, Dong W, Wang R, et al. Effect of caloric restriction on the SIRT1/mTOR signaling pathways in senile mice. Brain Res Bull. 2015;116:67–72.
Choi IY, Piccio L, Childress P, et al. A diet mimicking fasting promotes regeneration and reduces autoimmunity and multiple sclerosis symptoms. Cell Rep. 2016;15:2136–46.
Andoh A, Kuzuoka H, Tsujikawa T, Nakamura S, Hirai F, Suzuki Y, et al. Multicenter analysis of fecal microbiota profiles in Japanese patients with Crohn’s disease. J Gastroenterol. 2012;47:1298–307.
Ott SJ, Musfeldt M, Wenderoth DF, et al. Reduction in diversity of the colonic mucosa associated bacterial microflora in patients with active inflammatory bowel disease. Gut. 2004;53:685–93.
Sokol H, Seksik P, Furet JP, Firmesse O, Nion-Larmurier I, Beaugerie L, et al. Low counts of Faecalibacterium prausnitzii in colitis microbiota. Inflamm Bowel Dis. 2009;15:1183–9.
Sokol H, Lepage P, Seksik P, et al. Temperature gradient gel electrophoresis of fecal 16S rRNA reveals active Escherichia coli in the microbiota of patients with ulcerative colitis. J Clin Microbiol. 2006;44:3172–7.
Rodemann JF, Dubberke ER, Reske KA, et al. Incidence of Clostridium difficile infection in inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007;5:339–44.
Huda-Faujan N, Abdulamir AS, Fatimah AB, et al. The impact of the level of the intestinal short chain fatty acids in inflammatory bowel disease patients versus healthy subjects. Open Biochem J. 2010;4:53–8.
Fontana L, Partridge L. Promoting health and longevity through diet: from model organisms to humans. Cell. 2015;26(161):106–18.
Most J, Gilmore LA, Smith SR, Han H, Ravussin E, Redman LM. Significant improvement in cardiometabolic health in healthy nonobese individuals during caloric restriction-induced weight loss and weight loss maintenance. Am J Physiol Endocrinol Metab. 2018;314:E396–405.
Fernando HA, Zibellini J, Harris RA, et al. Effect of Ramadan fasting on weight and body composition in healthy non-athlete adults: a systematic review and meta-analysis. Nutrients. 2019;24(11):478.
Jahrami HA, Alsibai J, Clark CCT, et al. A systematic review, meta-analysis, and meta-regression of the impact of diurnal intermittent fasting during Ramadan on body weight in healthy subjects aged 16 years and above. Eur J Nutr. 2020;59:2291–316.
Jahrami HA, Faris ME, Janahi A, et al. Does four-week consecutive, dawn-to-sunset intermittent fasting during Ramadan affect cardiometabolic risk factors in healthy adults? A systematic review, meta-analysis, and meta-regression. Nutr Metab Cardiovasc Dis. 2021;31:2273–301.
Faris AE, Jahrami HA, Alsibai J, et al. Impact of Ramadan diurnal intermittent fasting on the metabolic syndrome components in healthy, non-athletic Muslim people aged over 15 years: a systematic review and meta-analysis. Br J Nutr. 2020;14(123):1–22.
Faris M, Jahrami H, Abdelrahim D, Bragazzi N, et al. The effects of Ramadan intermittent fasting on liver function in healthy adults: A systematic review, meta-analysis, and meta-regression. Diabetes Res Clin Pract. 2021;178: 108951.
Park Y, Park Y, Park S, Kim T, et al. Is fasting beneficial for hospitalized patients with inflammatory bowel diseases? Intest Res. 2020;18:85–95.
Goharifar H, Faezi S, Paragomi P, et al. The effect of Ramadan fasting on quiescent systemic lupus erythematosus (SLE) patients’ disease activity, health quality of life and lipid profile: a pilot study. Rheumatol Int. 2015;35:1409–14.
Darch KM, Holland TL, Spelman LJ. Secukinumab-Induced inflammatory bowel disease in a patient treated for chronic plaque psoriasis and psoriatic arthritis: a case report and review of the role of novel biologic agents targeting the p19 subunit of IL-23. Case Rep Med. 2020;2020:9404505.
BaHammam AS, Almeneessier AS. Recent evidence on the impact of ramadan diurnal intermittent fasting, mealtime, and circadian rhythm on cardiometabolic risk: a review. Front Nutr. 2020;11(7):28.
Faris MAE, Jahrami HA, Alhayki FA, et al. Effect of diurnal fasting on sleep during Ramadan: a systematic review and meta-analysis. Sleep Breath. 2020;24:771–82.
Al-Rawi N, Madkour M, Jahrami H, et al. Effect of diurnal intermittent fasting during Ramadan on ghrelin, leptin, melatonin, and cortisol levels among overweight and obese subjects: a prospective observational study. PLoS ONE. 2020;26(15): e0237922.
Torres-Ruiz M, Sulli A, Cutolo M, et al. Air travel, circadian rhythms/hormones, and autoimmunity. Clin Rev Allerg Immunol. 2017;53:117–25.
Faris MAE, Jahrami A, Obaideen A, et al. Impact of diurnal intermittent fasting during Ramadan on inflammatory and oxidative stress markers in healthy people: Systematic review and meta-analysis. J Nutr Intermed Metab. 2019;15:18–26.
Wang X, Yang Q, Liao Q, et al. Effects of intermittent fasting diets on plasma concentrations of inflammatory biomarkers: a systematic review and meta-analysis of randomized controlled trials. Nutrition. 2020;79–80:110974.
Atreya R, Neurath M. Involvement of IL-6 in the pathogenesis of inflammatory bowel disease and colon cancer. Clin Rev Allergy Immunol. 2005;28:187–96.
Bjarnason I. The use of fecal calprotectin in inflammatory bowel disease. Gastroenterol Hepatol. 2017;13:53–6.
Hassanein M, Hussein Z, Shaltout I, et al. The DAR 2020 Global survey: Ramadan fasting during COVID 19 pandemic and the impact of older age on fasting among adults with Type 2 diabetes. Diabetes Res Clin Pract. 2021;173: 108674.
Heun R. A systematic review on the effect of Ramadan on mental health: minor effects and no harm in general, but increased risk of relapse in schizophrenia and bipolar disorder. Global Psych. 2018;1(1):7–16.
Akgul S, Derman O, Kanbur NA. Fasting during Ramadan: a religious factor as a possible trigger or exacerbator for eating disorders in adolescents. Int J Eat Disord. 2014;47:905–10.
Daradkeh TK. Parasuicide during Ramadan in Jordan. Acta Psychiatr Scand. 1992;86:253–4.
Eddahby S, Kadri N. Moussaoui D Fasting during Ramadan isassociated with a higher recurrence rate in patients with bipolar disorder. World Psychiatry. 2014;13:97.
Chicco F, Magrì S, Cingolani A, et al. Multidimensional impact of Mediterranean diet on IBD patients. Inflamm Bowel Dis. 2021;1(27):1–9.
Chiba M, Nakane K, Komatsu M. Westernized diet is the most ubiquitous environmental factor in inflammatory bowel disease. Perm J. 2019;23:18–107.
Acknowledgements
The authors would like to express their gratitude to professor M. Serafy for his input and guidance in the manuscript.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study's conception and design. Material preparation, data collection, and analysis were performed by [MN, AB, AF, RL, HB, ME, SK, MS, WE, MS, AB, ID, HS]. The first draft of the manuscript was written by [MN, HS] and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by Kasralainy Research Ethics Committee (N-27-2021) and Ain Shams University Research ethics committee (R93/2021).
Consent for publication
The manuscript does not contain any person’s data in any form.
Informed consent
Informed consent was obtained from all subjects and/or their legal guardian(s). All experiments were performed in accordance with relevant guidelines and regulations. All methods were carried out in accordance with relevant guidelines and regulations.
Competing interests
All authors declare the absence of any financial or personal relationships with other people or organizations that could inappropriately influence and bias the work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Negm, M., Bahaa, A., Farrag, A. et al. Effect of Ramadan intermittent fasting on inflammatory markers, disease severity, depression, and quality of life in patients with inflammatory bowel diseases: A prospective cohort study. BMC Gastroenterol 22, 203 (2022). https://doi.org/10.1186/s12876-022-02272-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-022-02272-3