Abstract
Background
Dyspepsia is a common complaint in upper gastrointestinal disorders. It is described as predominant epigastric pain lasting for at least one month. Globally, peptic ulcer disease occurs in 3.5–32% of patients with dyspepsia. Helicobacter pylori (H. pylori) infection and non-steroidal anti-inflammatory drugs/aspirin use are the widely known risk factors for peptic ulcer disease. There was no recent document on H. pylori infection rate among patients with peptic ulcer disease in Ethiopia. This study aimed to determine magnitude and associated factors of peptic ulcer disease among dyspeptic patients in Northwest Ethiopia.
Methods
An institutional-based cross sectional study was conducted at the University of Gondar hospital, Northwest Ethiopia. A convenience sampling method was used to recruit 218 study subjects. A pre-designed semi-structured questionnaire was used to extract clinical information. Olympus flexible fiber-optic endoscope (Olympus, GIF-E 600, Olympus Corp., Hamburg, Germany) was used to confirm the presence of peptic ulcer disease. Diagnosis of active H. pylori infection was made using the fecal H. pylori Antigen 25 T Card Test (Anamol Lab., Pvt. Ltd., Palghar, India). The Data were entered into EPI Info version 4.6.0.2, and then exported to SPSS version 20 for analysis. Explanatory variables associated with peptic ulcer disease were analyzed by applying logistic regression model. P value < 0.05 was used to declare significant association.
Result
A total of 218 dyspeptic patients who underwent upper gastrointestinal endoscopic evaluations were included in the study. The mean (+ SD) age of patients was 42 ± 16.4 years. Forty nine percent (95% CI 42.4–56.2) of dyspeptic patients had active H. pylori infection. Peptic ulcer disease was diagnosed in 35% (95% CI 31.4–39.2) of patients with dyspepsia. H. pylori infection (AOR = 6.298, 95% CI 2.965–13.378, P value < 0.001) and NSAIDs/ASA use (AOR = 6.252, 95% CI 2.925–13.362, P value < 0.001) were identified as risk factors for peptic ulcer disease.
Conclusion
Medical treatment of peptic ulcer disease should target treatment of H. pylori infection and cautious use of non-steroidal anti-inflammatory drugs/aspirin.
Similar content being viewed by others
Background
Dyspepsia is a common complaint in upper gastrointestinal disorders. It is described as predominant epigastric pain lasting for at least one month [1, 2]. It can manifest as postprandial fullness, early satiety, or epigastric burning or pain. Globally, dyspepsia occurs in 10–20% of adults, and accounts for 3% of medical office visits. Dyspepsia has an impact on the quality of life of patients and the expenses to the health care service [1, 2]. According to previous studies, peptic ulcer disease (PUD) occurred in 2.4–3.5% of the Western populace, 12–15% of Asian inhabitants, and 24–28% of sub-Saharan African dwellers [3,4,5,6,7,8]. Helicobacter pylori (H. pylori) infection and non-steroidal anti-inflammatory drugs (NSAIDs)/aspirin (ASA) use are the major culprits for causing gastroduodenal mucosal injuries [9,10,11,12,13,14]. H. pylori is widely known to cause gastritis and peptic ulcer disease. Also, H. pylori is attributed to gastric cancer and gastric B-cell lymphoma, and is categorized as a class I carcinogen by the International Agency for Research on Cancer (IARC), a division of the World Health Organization (WHO) [9,10,11,12]. Use of NSAIDs is recognized to cause erosive gastritis and peptic ulcer disease. Prevalence of PUD was documented to be 14–25% among NSAIDs/ASA users [13,14,15]. Other less frequently implicated risk factors for PUD include genetics, stress, diet, smoking and alcohol [16, 17]. Global reports indicated that H. pylori infection rate among PUD patients was 14–21% in the United States, 60–70% in Asia, and 70–90 in sub-Saharan Africa [4, 5, 7, 18,19,20,21,22,23]. There was no recent document on H. pylori infection rate among PUD patients in Ethiopia. There are several invasive and non-invasive diagnostic tests to detect H. pylori infection. Invasive tests include endoscopic biopsy specimen for histology, culture and rapid urease test (RUT) and polymerase chain reaction (PCR). Non-invasive tests consist of urea breath test (UBT), serum antibody test, stool antigen test, saliva antibody test and urinary antibody test [24, 25]. The choice of diagnostic tests is based on the prevalence of H. pylori infection, the availability and cost of the diagnostic tests, and patient-related characteristics [19,20,21,22,23]. This study used fecal H. pylori antigen test to document active H. pylori infection, which has optimal diagnostic accuracy. The study aimed to determine the magnitude, H. pylori infection rate, and associated factors of PUD among dyspeptic patients at the University of Gondar hospital, Northwest Ethiopia. The study would give valuable information on the approach to treating dyspepsia in the setting and similar institutions.
Methods
Study design and setting
An institutional-based cross sectional study was conducted at the endoscopy unit, University of Gondar hospital, between June 1, 2020 and November 30, 2020. The hospital is located in Northwest Ethiopia, which is 750 km away from the capital, Addis Ababa. The hospital had a catchment population of 5 million people. The endoscopy unit was established in the hospital in 2000. It has provided endoscopic services for patients with gastrointestinal disorders. It was staffed by trained internists and surgeons, unit nurses, and a cleaner. The upper gastrointestinal endoscopy sessions were done three days per week, and on average, five to eight patients attended each of endoscopic days. The other two days of a week were for colonoscopy sessions.
Study population
All patients who underwent endoscopic evaluation at endoscopy unit, University of Gondar hospital was the study population.
Inclusion criteria
Adults 18 years or older who presented with a complaint of dyspepsia, and underwent endoscopic evaluation at the endoscopic unit, University of Gondar during the study period were included in the study.
Exclusion criteria
Study subjects who were on antibiotics or PPI in the last one month, had alarming gastro duodenal features, had active bleeding diathesis, and didn’t give consent to undergo endoscopic evaluation were excluded from the study.
Study variables
Dependent variable: peptic ulcer disease
Independent variables: (1) socio-demographic characteristics include age, gender, residence, marital status, and socioeconomic status. (2) clinical characteristics include H. pylori infection, NSAIDs/ASA use, and presence of co-morbidities such as cardiovascular diseases, rheumatologic diseases, chronic airway diseases, and HIV infection, (3) behavioral factors include cigarette smoking and alcohol consumption.
Sample size and sampling procedure
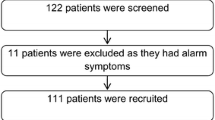
The sample size was calculated using a single population proportion formula with the assumption of 95% confidence level, 5% margin of error, and taking a 25% estimated proportion of peptic ulcer disease among dyspeptic patients [7, 8]. The sample size was determined for a study population size of 1000 during the study period. A convenience sampling method was used to recruit 224 study subjects.
Data collection instrument and procedures
All relevant clinical information, endoscopic findings and H. pylori test results were recorded on predesigned semi-structured questionnaire.
Clinical procedures
Patients were interviewed to obtain socio-demographic data and relevant clinical history before the upper gastrointestinal endoscopy. The clinical history includes indication for endoscopy (dyspepsia), duration of dyspepsia, use of NSAIDs/ASA, history of cigarette smoking and alcohol consumption, and presence of co-morbidities. Focused physical examination was done to each of the patients.
Endoscopic procedures
All endoscopic procedures were conducted by trained physicians (internists and surgeons). Olympus flexible fiber-optic endoscope (Olympus GIF-E 600, Olympus Corp., Hamburg, Germany) was used for the procedure. Informed consent was obtained from all patients before the procedure. Lidocaine (2%) throat spray and IV midazolam (2 mg/ml) were used as local anesthetic and sedative agents respectively. All procedures were conducted in the morning on an empty stomach. Diagnoses of endoscopic appearances (site, size, and number of gastro duodenal lesions) were at the discretion of the endoscopist.
Diagnosis of H. pylori infection
Diagnosis of active H. pylori infection was made using the ‘Fecal H. pylori Antigen 25 T Card Test’ (Anamol Lab., Pvt. Ltd., Palghar, India). Fecal H. pylori antigen test is a lateral flow chromatographic immunoassay for qualitative detection of H. pylori antigen in human fecal specimen. Positive test result indicates an active H. pylori infection.
‘Fecal H. pylori Antigen 25 T Card Test’ procedures
The membrane strip was inserted into the cassette. Adequate volume of fecal specimen was dispensed into the sample well of the test cassette. The H. pylori antigen in the stool sample (for positive test) reacted with the H. pylori antibody conjugate in the test device. The immune-complex moved along the membrane chromatographically to the test region. The pre-coated antibody of the test-band captured the immune-complex to give the test result. Positive H. pylori test was indicated by the red color test-band. Negative test result showed no color change in test-band. Internal procedural control was included in the test. A red colored band appearing in the control region was the internal procedural control. The test result was interpreted within 15 min of the procedure.
Data analysis
Data were entered into and cleaned in EPI Info™ version 4.6.0.2 (EPI Info™ Inc., Atlanta, USA) and transported to and analyzed in SPSS version 20 (SPSS Inc., Chicago, USA). Categorical variables were reported as frequencies (percentages) and continuous variables as mean with standard deviation. The results were summarized by using frequency, tables and graphs. Risk factors for PUD were analyzed by applying logistic regression model. The goodness of fit of the model was judged from the Hosmer–Lemeshow test. The fit of the model was considered acceptable (P value = 0.67). Those variables with a P value < 0.25 in the bi-variate analysis were exported to multi-variate analysis. The results were presented as odds ratio with 95% confidence interval. P value < 0.05 was used to declare significant association.
Ethical considerations
The research protocol complied with the Declaration of Helsinki and ethical clearance was obtained from the Institutional Review Board (IRB) of the College of Medicine and Health Sciences, University of Gondar (19/02/2020, IRB No. 1267/02/2020). Study subjects were recruited only after written informed consent was obtained. All data obtained were treated confidentially. Dyspeptic patients who were found to have endoscopic proven peptic ulcer disease and positive fecal H. pylori antigen test were taken care of as per the recommendation of 2017 ACG clinical guideline: Treatment of Helicobacter pylori infection [26].
Definition of terms
Dyspepsia is predominant epigastric pain lasting for at least one month [1].
Peptic ulcer disease is a visible defect in the gastric or duodenal mucosa more than 5 mm with peripheral edema and overlying white exudate [9].
Alarming gastro duodenal features include family history of gastrointestinal cancer, intractable vomiting, progressive dysphagia or odynophagia, anemia, unexplained weight loss, or gastrointestinal bleeding (hematemesis or melena).
NSAIDs/ASA user refers to a patient who consumes NSAIDs/ASA at any dosage for at least three months [27].
Cigarette smoker refers to someone who has smoked more than 100 cigarettes in their lifetime and has smoked in the last 28 days [28].
Alcohol consumption is defined as alcohol intake more than two drinks for men and one drink for women in a day [29].
Results
Socio-demographic characteristics of study subjects
Two hundred eighteen patients were included in the study to give a response rate of 97.3%. Six (2.7%) study subjects were exempted from statistical analysis due to incomplete data. The mean (+ SD) age of the patients was 42 ± 16.4 years. Majority of study subjects were males (118/218, 54%), urban residents (126/218, 58%) married (139/218, 64%), and had joined school (146/218, 67%). Most (186/218, 85%) of study subjects were Orthodox Christian followers (Table 1). More than a third (78/218, 36%) had a history of alcohol consumption, while less than five percent (10/218, 4.6%) were cigarette smokers (Table 2).
Clinical characteristics of study subjects
Clinical features
The average duration of dyspepsia was 12.4 (± 7.6) months, which ranged from 2 months to 4 years. Abdominal tenderness was elicited in one-third (63/218, 29%) of patients.
Endoscopic findings
Peptic ulcer disease (PUD) was diagnosed in 35% (95% CI 31.4–39.2) of patients with dyspepsia. Two-thirds (55/76, 72%) of PUD cases had duodenal ulcers. Other organic causes of dyspepsia were gastritis/doudenitis (41/218, 19%), gastric mass (13/218, 6%) and pyloric obstruction (10/218, 4%). More than one-third (78/218, 36%) had functional dyspepsia (Fig. 1).
H. pylori infection rate
Forty nine percent (95% CI 42.4–56.2), 107/218, of dyspeptic patients had active H. pylori infection (Table 2). Seventy-one (95% CI 66.7–77.5) 54/76, PUD patients had active H. pylori infection. The majority (46/54, 85%) of H. pylori infections among PUD patients had duodenal ulcer.
NSAIDs/ASA users
NSAIDs/ASA was used by forty percent (86/218, 40%) of dyspeptic patients (Table 2). More than half (47/86, 55%) of NSAIDs/ASA users were diagnosed to have PUD.
Co-morbidities
One-fifth (43/218, 20%) of study subjects had co-morbidities, including cardiovascular diseases (25/43, 58%), rheumatologic diseases (12/43, 28%), chronic airway diseases (4/43, 9%), and HIV infection (2/43, 5%).
Factors associated with risk of developing PUD among dyspeptic patients
Multivariate logistic regression analysis revealed that dyspeptic patients with H. pylori infection (AOR = 6.298, 95% CI 2.965–13.378, P value = 0.000) and NSAIDs/ASA use (AOR = 6.252, 95% CI 2.925–13.362, P value = 0.000) were at risk of developing PUD, while non-married study subjects were protected from developing PUD (AOR = 0.367, 95% CI = 0.154–0.887, P value = 0.024) (Table 3). There was no statistically significant difference in the magnitude of peptic ulcer disease among age groups, gender, residence, cigarette smoking, alcohol consumption, and presence of co-morbidities.
Discussion
Among a total of 218 dyspeptic patients, active H. pylori infection was documented in 49% (95% CI 42.4–56.2) of study subjects. Likewise, the H. pylori infection rate among PUD patients was 71% (95% CI 66.7–77.5). These findings were congruent with hospital-based sub-Saharan African (SSA) reports. The African reports verified that 40–65% of dyspeptic and 65–90% PUD patients were positive for H. pylori infection [7, 8, 19, 20, 23, 24]. The Ethiopian pooled prevalence of H. pylori infection was 52.2% (95% CI 45.8–58.6) in a recent hospital-based meta-analysis [30]. The global magnitude of H. pylori infection was 34% in Western Europe, 37% in Northern America, 55% in Asia, and 70% in Africa [31]. The global difference in the magnitude of the H. pylori infection rate could be explained by the difference in socio-economic status, environmental sanitation, living conditions, and personal hygiene. In this study, PUD (35%) was the commonly observed abnormal endoscopic lesion, followed by gastritis/duodenitis (19%) and gastric mass (6%). More than one-third (36%) had functional dyspepsia. Recent Nigerian study reported that gastritis/duodenitis (27%) and PUD (28%) were the frequently documented abnormal endoscopic findings. Gastric cancer (2.3%) was less frequently reported [7]. Studies in Tanzania and Ethiopia reported that gastritis/duodenitis (80–98%) followed by PUD (25–32%) were the commonly observed endoscopic pathologies. Gastric cancer was detected in 3–7% of dyspeptic patients [8, 19]. PUD (62%) followed by gastric cancer (12%) was the frequently detected endoscopic finding in Ghanaian study [23]. While, studies in Nigeria and Kenya witnessed gastritis/duodenitis (72–79%) was the commonest endoscopic finding. PUD (6.5–13%) and gastric cancer (1.4–2.3%) were less frequently reported [20, 24]. The difference in the type of gastro duodenal lesions among dyspeptic patients in African reports could be explained by differences in patient-related characteristics (age, genetics), H. pylori virulence strain, NSAIDs/ASA exposure rate, lifestyle preferences (smoking, alcohol), and other environmental factors [19, 20, 23, 24]. This study revealed that nearly forty percent (39.5%) of dyspeptic patients had a history of NSAIDs/ASA use, and more than half (55%) of NSAIDs/ASA users developed PUD. Western literature reviews documented that dyspepsia occurred in up to half (50–60%) of patients taking NSAIDs/ASA and up to a third (15–30%) of patients using NSAIDs/ASA developed PUD [13,14,15]. On multivariable logistic regression analysis, odds of developing PUD was sixfold higher among dyspeptic patients with H. pylori infections than those with negative H. pylori infections (AOR = 6.298, 95% CI 2.965–13.378, P value < 0.001). It was confirmed that H. pylori establishes prolonged gastro duodenal mucosal infection, and leads to chronic active gastritis and PUD [9,10,11,12, 19, 20, 23, 24]. Dyspeptic patients who use NSAIDs/ASA had sixfold increased risk of developing PUD as compared to non-NSAIDs/ASA users (AOR = 6.252, 95% CI 2.925–13.362, P value < 0.001). NSAIDs/ASA interferes with the cyclo-oxygenase (COX) pathway and depletes biosynthesis of gastric prostaglandins. In addition, NSAIDs/ASA are weak acids which cause direct gastric mucosal toxic injury [9, 10, 13,14,15,16,17]. Study subjects with non-married status were 60% protected from developing PUD as compared to their counter parts (AOR = 0.367, 95% CI = 0.154–0.887, P value = 0.024). Reduced family size and non-crowded living condition among non-married subjects might contribute to reduced H. pylori infection rate and occurrence of PUD.
Limitation of the study
The study subjects were referred patients to the hospital, which was more likely to be the severely ill study candidates. In addition, the convenience sampling method might introduce selection bias.
Conclusions
H. pylori infection was often detected in dyspeptic patients. Majority of PUD patients were diagnosed to have H. pylori infection. Dyspeptic patients with H. pylori infection and NSAIDs/ASA use were at risk of developing PUD.
Availability of data and materials
All data generated and analyzed were included in this research article.
Abbreviations
- ACG:
-
American College of Gasrtoenterology
- ASA:
-
Aspirin
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- CDC:
-
Center for Disease Control and Prevention
- COR:
-
Crude odds ratio
- H. pylori :
-
Helicobacter pylori
- IV:
-
Intravenous
- NSAIDs:
-
Nonsteroidal anti-inflammatory drugs
- PPI:
-
Proton pump inhibitors
- PUD:
-
Peptic ulcer disease
References
Moayyedi PM, Lacy BE, Andrews CN, Enns RA, Howden CW, Vakil N. ACG and CAG clinical guideline: management of dyspepsia. Off J Am Coll Gastroenterol: ACG. 2017;112(7):988–1013.
Stanghellini V, Chan FK, Hasler WL, Malagelada JR, Suzuki H, Tack J, et al. Gastroduodenal disorders. Gastroenterology. 2016;150(6):1380–92.
Groenen MJ, Kuipers EJ, Hansen BE, Ouwendijk RJT. Incidence of duodenal ulcers and gastric ulcers in a Western population: back to where it started. Can J Gastroenterol. 2009;23(9):604–8.
Latif A, Karim S, Ali H, Hussain M, Mujtaba G, Majid S. The burden of duodenal ulcers among dyspeptic patients. Cureus. 2021;13(5):e15115.
Xia B, Xia H, Ma C, Wong K, Fung F, Hui C, et al. Trends in the prevalence of peptic ulcer disease and Helicobacter pylori infection in family physician-referred uninvestigated dyspeptic patients in Hong Kong. Aliment Pharmacol Ther. 2005;22(3):243–9.
Archampong TN, Asmah RH, Richards CJ, Martin VJ, Bayliss CD, Botão E, et al. Gastro-duodenal disease in Africa: Literature review and clinical data from Accra, Ghana. World J Gastroenterol. 2019;25(26):3344.
Okoye OG, Olaomi OO, Nwofor AM, Jibrin P, Batta CS, Yaú AG, et al. Correlation of clinical, endoscopic, and pathological findings among suspected peptic ulcer disease patients in Abuja, Nigeria. Gastroenterol Res Pract. 2021;2021:1–7.
Asrat D, Nilsson I, Mengistu Y, Ashenafi S, Ayenew K, Al-Soud WA, et al. Prevalence of Helicobacter pylori infection among adult dyspeptic patients in Ethiopia. Ann Trop Med Parasitol. 2004;98(2):181–9.
Malfertheiner P, Chan FK, McColl KE. Peptic ulcer disease. Lancet. 2009;374(9699):1449–61.
Kavitt RT, Lipowska AM, Anyane-Yeboa A, Gralnek IM. Diagnosis and treatment of peptic ulcer disease. Am J Med. 2019;132(4):447–56.
McColl KE. Zakażenie Helicobacter pylori. N Engl J Med. 2010;362:1597–604.
Mladenova I. Clinical relevance of Helicobacter pylori infection. J Clin Med. 2021;10(16):3473.
Russell R. Non-steroidal anti-inflammatory drugs and gastrointestinal damage—problems and solutions. Postgrad Med J. 2001;77(904):82–8.
Garcia Rodriguez LA, Hernández-Díaz S. Risk of uncomplicated peptic ulcer among users of aspirin and nonaspirin nonsteroidal antiinflammatory drugs. Am J Epidemiol. 2004;159(1):23–31.
Frech EJ, Go MF. Treatment and chemoprevention of NSAID-associated gastrointestinal complications. Ther Clin Risk Manag. 2009;5:65.
Lee SP, Sung I-K, Kim JH, Lee S-Y, Park HS, Shim CS. Risk factors for the presence of symptoms in peptic ulcer disease. Clin Endosc. 2017;50(6):578.
Asali AM, Alghamdi MA, Fallatah SA, Alholaily WA, Aldandan RG, Alnosair AH, et al. Risk factors leading to peptic ulcer disease: systematic review in literature. Int J Community Med Public Health. 2018;5(10):4617–24.
Sonnenberg A, Turner KO, Genta RM. Low prevalence of Helicobacter pylori-positive peptic ulcers in private outpatient endoscopy centers in the United States. Off J Am Coll Gastroenterol: ACG. 2020;115(2):244–50.
Quach DT, Vilaichone R-K, Van Vu K, Yamaoka Y, Sugano K, Mahachai AA. Helicobacter pylori infection and related gastrointestinal diseases in southeast Asian countries: an expert opinion survey. Asian Pac J Cancer Prev: APJCP. 2018;19(12):3565.
Archampong TN, Asmah RH, Wiredu EK, Gyasi RK, Nkrumah KN. Factors associated with gastro-duodenal disease in patients undergoing upper GI endoscopy at the Korle-Bu Teaching Hospital, Accra, Ghana. African Health Sci. 2016;16(2):611–9.
Jemilohun AC, Otegbayo JA, Ola SO, Oluwasola OA, Akere A. Prevalence of Helicobacter pylori among Nigerian patients with dyspepsia in Ibadan. Pan Afr Med J. 2010;6(1):18.
Ayana SM, Swai B, Maro V, Kibiki GS. Upper gastrointestinal endoscopic findings and prevalence of Helicobacter pylori infection among adult patients with dyspepsia in northern Tanzania. Tanzan J Health Res. 2014;16(1):16–22.
Mwangi CN, Njoroge S, Rajula A, Laving A, Kamenwa R, Devani S, et al. Prevalence and endoscopic findings of Helicobacter pylori infection among dyspeptic patients in Kenya. Open J Med Microbiol. 2020;10(04):233.
Talebi Bezmin Abadi A. Diagnosis of Helicobacter pylori using invasive and noninvasive approaches. J Pathog. 2018;2018:1–13.
Hussein RA, Al-Ouqaili MT, Majeed YH. Detection of Helicobacter Pylori infection by invasive and non-invasive techniques in patients with gastrointestinal diseases from Iraq: a validation study. PLoS ONE. 2021;16(8):e0256393.
Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG clinical guideline: treatment of Helicobacter pylori infection. Off J Am Coll of Gastroenterol: ACG. 2017;112(2):212–39.
Abdu N, Mosazghi A, Teweldemedhin S, Asfaha L, Teshale M, Kibreab M, et al. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Usage and co-prescription with other potentially interacting drugs in elderly: a cross-sectional study. PLoS ONE. 2020;15(10):e0238868.
Laugesen M, Swinburn B. New Zealand’s tobacco control programme 1985–1998. Tob Control. 2000;9(2):155–62.
Research A, Staff CRE. Drinking patterns and their definitions. Alcohol Res Current Rev. 2018;39(1):17.
Melese A, Genet C, Zeleke B, Andualem T. Helicobacter pylori infections in Ethiopia; prevalence and associated factors: a systematic review and meta-analysis. BMC Gastroenterol. 2019;19(1):1–15.
Hooi JK, Lai WY, Ng WK, Suen MM, Underwood FE, Tanyingoh D, et al. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology. 2017;153(2):420–9.
Acknowledgements
We are grateful to thank the study participants and their health personnel.
Funding
Funding for research was obtained from the ‘Research and Publication Office’ of the College of Medicine and Health Sciences, University of Gondar. The funding body had no role in the design of the study, data collection, analysis and interpretation of the data.
Author information
Authors and Affiliations
Contributions
Belete Assefa contributed to the conception, design, data collection, analysis, writing, and review of the manuscript. Abilo Tadesse contributed to the conception, design, analysis, writing and review of the manuscript. Zenahbizu Abay, Alula Abebe, Tsebaot Tesfaye, Melaku Tadesse and Ayenew Molla contributed to conception, design, analysis and review of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The research protocol complied with the Declaration of Helsinki and ethical clearance was obtained from the Institutional Review Board (IRB) of the College of Medicine and Health Sciences, University of Gondar (19/02/2020, IRB No. 1267/02/2020). Study subjects were recruited only after written informed consent was obtained.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Assefa, B., Tadesse, A., Abay, Z. et al. Peptic ulcer disease among dyspeptic patients at endoscopy unit, University of Gondar hospital, Northwest Ethiopia. BMC Gastroenterol 22, 164 (2022). https://doi.org/10.1186/s12876-022-02245-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-022-02245-6