Abstract
Background
Primary care clinicians (PCCs) are typically the first practitioners to detect cognitive impairment in their patients, including those with Alzheimer’s disease or related dementias (ADRD). However, conversations around cognitive changes can be challenging for patients, family members, and clinicians to initiate, with all groups reporting barriers to open dialogue. With the expanding array of evidence-based interventions for ADRD, from multidomain care management to novel biotherapeutics for early-stage AD, incorporating conversations about brain health into routine healthcare should become a standard of care. We conducted a systematic review to identify barriers to and facilitators of brain health conversations in primary care settings.
Methods
We systematically searched PubMed, Scopus, Web of Science, and the Cochrane Library for qualitative or quantitative studies conducted in the US between January 2000 and October 2022 that evaluated perceptions of cognition and provider-patient brain health conversations prior to formal screening for, or diagnosis of, mild cognitive impairment or ADRD. We assessed the quality of the included studies using the Mixed Methods Appraisal Tool.
Results
In total, 5547 unique abstracts were screened and 22 articles describing 19 studies were included. The studies explored perceptions of cognition among laypersons or clinicians, or provider-patient interactions in the context of a patient’s cognitive concerns. We identified 4 main themes: (1) PCCs are hesitant to discuss brain health and cognitive concerns; (2) patients are hesitant to raise cognitive concerns; (3) evidence to guide clinicians in developing treatment plans that address cognitive decline is often poorly communicated; and (4) social and cultural context influence perceptions of brain health and cognition, and therefore affect clinical engagement.
Conclusions
Early conversations about brain health between PCCs and their patients are rare, and effective tools, processes, and strategies are needed to make these vital conversations routine.
Similar content being viewed by others
Background
Current evidence suggests that up to 40% of Alzheimer’s disease and related dementias (ADRD) may be partly attributable to modifiable risk factors, among them hypertension, physical inactivity, hearing loss, excessive alcohol consumption, smoking, and social isolation [1, 2], and new research continues to identify others. Primary prevention efforts, such as lifestyle changes (especially if adopted as a lifespan strategy), early intervention for clinically treatable risk factors, and amelioration of social determinants of poor cognitive health could help mitigate the societal burden associated with ADRD [1,2,3]. For example, the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER) trial demonstrated that a multidomain lifestyle intervention could provide cognitive benefits to older people at risk for ADRD [4,5,6], and studies of this and similar interventions are underway in several countries.
Because of the population-wide impacts of ADRD, the US National Plan to Address Alzheimer’s Disease now includes a public health initiative [7]. The Building Our Largest Dementia (BOLD) Infrastructure for Alzheimer’s Act of 2018 authorized the Centers for Disease Control and Prevention (CDC) to establish 3 centers of excellence for ADRD prevention, early detection, and caregiving, and to energize over 40 state and local public health and other entities to develop and implement new local initiatives [8]. However, strategies for implementing and measuring the impact of such efforts in clinical practice remain ill defined, especially with respect to primary care.
Approximately 4 of 5 primary care clinicians (PCCs) consider themselves on the frontlines of brain health [9]. In the US, PCCs are usually the first point of contact for patients worried about memory loss [10] and are typically the first to detect and evaluate patients experiencing mild cognitive impairment (MCI) or ADRD [11]. As such, PCCs are uniquely positioned to initiate early conversations about brain health—even before patients have symptoms of or are diagnosed with MCI or dementia—and they are the only medical discipline capable of improving population health [12]. PCCs already play a key role in preventing several chronic diseases by offering interventions that modify risk factors [13,14,15], and older adults are more likely to improve their diet and physical activity when encouraged to do so by their PCC [13, 16,17,18,19,20,21,22,23,24].
Thus, PCCs can play a vital role in making early conversations around brain health and cognitive concerns part of routine healthcare, long before symptoms appear. Some resources offer guidance regarding interventions for brain health [25], but understanding of barriers to early conversations about brain health in the primary care setting remains limited. This systematic review summarizes the existing literature and aims to inform the development of tools, processes, and strategies that could facilitate early brain health conversations between PCCs and their patients.
Methods
This review was conducted in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 2020 statement (Appendix A) [26].
All authors collaboratively identified key terms to be included in the search algorithms, and initial search strings were developed for each database using all key terms. On October 17, 2022, we searched PubMed, Scopus, Web of Science, and the Cochrane Library with predetermined algorithms using terms related to “brain health,” “cognitive dysfunction,” “cognitive impairment,” “cognitive decline,” and “dementia,” along with terms related to health knowledge, attitudes, behaviors, and communication (Appendix B). Two reviewers (QOB and AM) conducted test searches using the initial algorithms, which were then refined for each specific database to ensure a sufficient and feasible number of returned records. The first 30 titles returned by the test searches were reviewed to assess the overall relevance of the records returned by each algorithm. The initial search string appeared to be too restrictive for Scopus, Web of Science, and Cochrane Library databases; therefore, some groupings of search terms were removed from the algorithms to ensure a sufficient number of records to review.
We included studies that assessed perceptions of cognition or that evaluated PCC-patient conversations about brain health occurring before formal assessment or diagnosis of MCI/ADRD. Studies focused on evaluation, diagnosis, or treatment of MCI or ADRD were excluded. Notably, the term “Alzheimer’s” was omitted from the algorithms because our review specifically excluded studies that focused on individuals already diagnosed with ADRD. Furthermore, inclusion of “Alzheimer’s” as a term in early test searches led to an infeasible number of records to review. Other eligibility criteria included articles published in English on or after January 1, 2000. As global health systems vary widely, we limited our review to studies conducted in the US.
All retrieved references were imported into Covidence (Veritas Health Innovation, www.covidence.org). Two reviewers (QOB and AM) independently screened all titles and abstracts for relevance, and disagreements were resolved by discussion between these 2 reviewers. The same 2 reviewers independently screened all full-text articles. Additional articles were identified for inclusion through searches of the reference lists of included articles. Data were manually extracted and organized into a data charting form developed by all authors. Results were synthesized into a table summarizing key findings from each study. After the data extraction process was complete, all authors reviewed the included articles, participated in finalization of the summary table, and collaboratively identified the themes that emerged from the included articles through iterative discussion of the key findings of each paper. These discussions continued until all authors agreed on the final set of themes, at which point each article was mapped to the theme or themes that represented its key findings.
The quality of each included study was independently evaluated by 2 reviewers (QOB and AM) using the mixed methods appraisal tool (MMAT) [27]. Because we expected to include studies with a wide variety of designs in our review, we selected the MMAT as it was designed to assess the methodological quality of qualitative, quantitative, and mixed methods studies (Appendix C).
Results
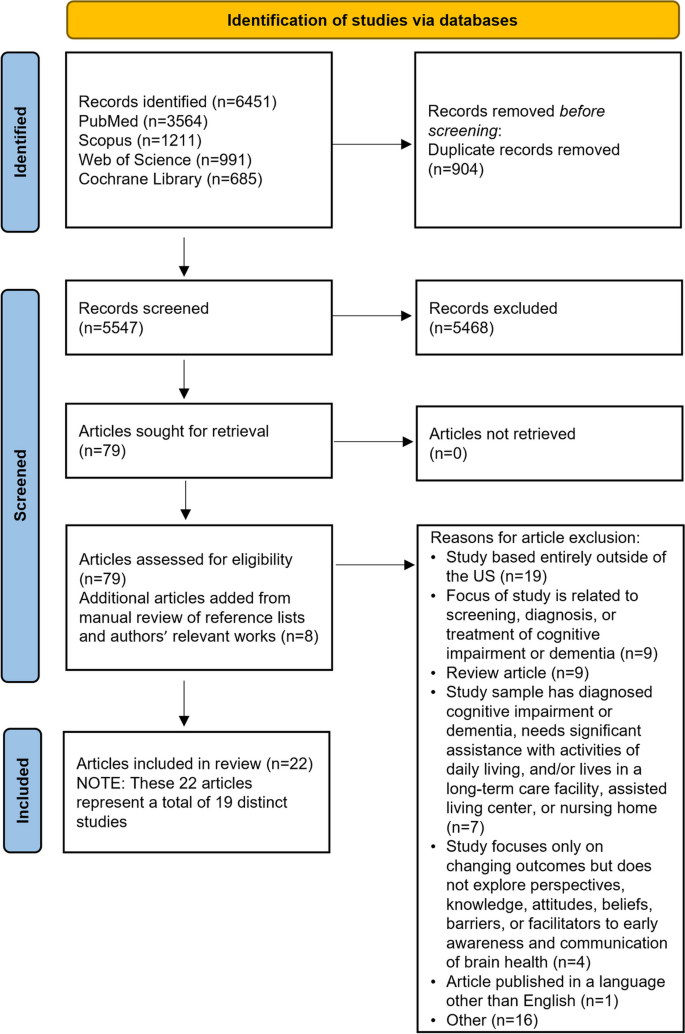
In total, 5547 unique records were identified. Of these, 5468 were excluded after title and abstract screening. Articles were excluded if they were published before the year 2000 or if they were published in a language other than English. Studies conducted outside the US were also excluded, as were those that focused on patients already diagnosed with Alzheimer’s disease or mild cognitive impairment, or that described specialist clinicians practicing outside of primary care settings. Additionally, review articles and studies that did not explore perspectives, knowledge, attitudes, beliefs, barriers, or facilitators to communication related to brain health or cognitive concerns were also excluded. In total, 79 full-text articles were assessed for eligibility. A manual review of reference lists and key authors’ works led to the inclusion of another 8 articles. After screening, 22 articles representing 19 unique studies were identified for inclusion (Fig. 1).
Characteristics of included studies are detailed in Table 1. Studies explored either perceptions of cognition or provider-patient interactions in the context of a patient’s cognitive complaints. We found no articles that specifically explored preventive brain health conversations. Most were descriptive in nature, using qualitative, quantitative, or mixed-methods approaches. The most common methods of data collection included focus groups, semi-structured individual interviews, surveys, or a combination. Notably, most articles (n = 15) were published more than 10 years ago.
The majority of articles (n = 20) included lay participants (e.g., patients, caregivers, and community members); 4 included PCCs (e.g., physicians, nurse practitioners, and physician assistants). One study included both laypersons and PCCs [28]. Several studies specifically explored the beliefs, attitudes, and knowledge of US racial and ethnic minority groups: 2 each were conducted with Black/African American [29, 30] or Asian American participants [31, 32], 3 with Latino participants [33,34,35], and 2 with racially and ethnically diverse participants [36,37,38,39,40].
Overall, the quality of the studies was high. Using the MMAT to appraise the quality of the studies, we found that 15 of the 16 qualitative studies adequately met all criteria for methodological quality. [29,30,31,32,33, 35,36,37,38,39,40,41,42,43,44] Quality was more varied among quantitative descriptive studies [28, 45, 46], and the lowest quality studies included in this review used mixed methods designs [34, 47, 48]. Detailed quality assessment results can be found in Appendix C.
Our review uncovered 4 main themes that provide insight into barriers to and facilitators of implementing early conversations about brain health between PCCs and their patients.
Theme 1: PCCs are hesitant to discuss brain health and cognitive concerns
Studies addressed discussions of cognitive concerns or impairment, rather than brain health as a general category of health or wellness. Many PCCs are uncomfortable discussing cognitive concerns with their patients, or lack resources and support for these conversations [47]. In a survey of 972 physicians, approximately half of whom were family or general practitioners, 31.9% of respondents reported that lack of reimbursement was the most frequent barrier to discussing cognitive impairment with patients [45]. Other barriers commonly reported by respondents included a lack of proven treatments and limited scientific evidence for prevention of MCI or ADRD (26.3%) and the need to address more pressing medical issues (24.6%) [45]. A qualitative study of 49 PCCs reported additional barriers to talking about cognition, such as a lack of time during appointments, therapeutic nihilism, insufficient evidence regarding prevention and treatment of cognitive impairment, and negative patient attitudes about cognition education [42]. Although these studies were conducted before the 2011 introduction of the Annual Wellness Visit, a preventive Medicare benefit that requires identification of any existing cognitive impairment [49], there is little evidence to suggest that PCCs’ attitudes and practices have dramatically changed.
According to the articles included in the present review, addressing these barriers would require resolving constraints related to time, clinic resources, and reimbursement; tailoring education to improve PCCs’ comfort and cultural awareness around discussing cognitive difficulties and interventions with their patients; and increasing their confidence in the evidence supporting the value of interventions. In a study of PCCs across 3 states, practitioners reported using a variety of sources, such as continuing medical education, popular media, and online resources to educate themselves on brain health [48], a finding corroborated by another study [45]. Effective dissemination of educational material related to brain health, cognition, and cognitive disorder care can and should occur through multiple approaches (e.g., online sources, continuing medical education, and professional journals). Strategies for establishing effective collaboration between PCCs and cognitive disorder specialists—who are scarce in many regions—have not yet been described in the literature. Productive areas for exploration include how best to facilitate knowledge transfer, how to provide PCCs with up-to-date understanding of interventions usable in primary care settings [48], and how best to define the clinical contributions of generalists and specialists in the evaluation and care of people with cognitive impairments.
Theme 2: patients are hesitant to raise cognitive concerns
In a study of older, primarily White patients attending a first visit to an outpatient geriatric practice, patients identified several barriers to discussing cognitive concerns with their physician [47]. Most often, patients felt it was the physician’s responsibility to initiate the discussion. Others intended to initiate the conversation during the appointment but forgot. In this same study, researchers noted that some patients may hesitate to raise cognitive concerns due to feelings of embarrassment or shame, resulting from stigma surrounding MCI and ADRD [47]. The role of stigma was also reported in a study of ethnically diverse older adults [38]. In that study, 42 focus groups were conducted with older adults representing 6 racial and ethnic groups (i.e., African American, Native American, Chinese American, Latino, White, and Vietnamese American). Researchers found that Native American, Chinese American, and Vietnamese American respondents were specifically concerned about stigma associated with MCI or ADRD and how stigma may impact their family relationships [38]. Two other studies suggested that individuals may not distinguish normal aging from cognitive decline [32, 41]. For example, in a study of 62 older Asian American participants, 95% of participants assumed that memory loss was part of normal aging [32].
The studies included in the present review also highlighted the need for solutions that address patients’ hesitance to initiate important brain health discussions and provided examples of such solutions. For instance, if patients believe it is the responsibility of their PCC to start discussions regarding cognition and if patients are likely to forget to raise cognitive concerns during appointments, then PCCs can remove this barrier by taking the lead [47]. However, as mentioned previously, PCCs are also often hesitant to start these conversations [42, 45, 47, 48]. One approach to successful, practical implementation is to treat discussions of cognitive concerns as routine by embedding questions around cognition within a medical review of systems [47]; however, additional resources are clearly needed to aid clinicians in leading these conversations.
Theme 3: evidence to guide clinicians in developing treatment plans that address cognitive decline is often poorly communicated
Both lay media and scientific discussions of brain health are often confusing, contradictory, or limited [30, 36,37,38, 48]. Thus, although most people recognize the importance of aging well and maintaining brain health [28, 30,31,32,33,34, 36, 37, 39,40,41, 48, 50], many remain skeptical of brain health research and unsure about which cognitive interventions are worthwhile, leading to therapeutic nihilism [43, 44, 46]. This theme was common across multiple studies reviewed. To date, no study has addressed whether the perception of ADRD as a disease that affects only elderly individuals may have promoted catastrophic thinking and reinforced avoidance on the part of both clinicians and their patients. In addition, many publications have described ADRD as a “terminal illness” rather than a manageable chronic condition [51,52,53]. Although this characterization may have been intended to elevate the importance of ADRD in public and medical discourse, this portrayal may have reinforced fear and avoidance.
To facilitate action around brain health, the studies included in the present review suggest that both laypersons and PCCs should be educated on the existing evidence that supports a range of interventions for brain health and cognitive disorders [29, 50]. This education should be communicated clearly, concisely, and consistently [30, 33, 43].
Theme 4: social and cultural context influence perceptions of brain health and cognition, and therefore affect clinical engagement
Several studies found that differences in beliefs about brain health and cognitive decline among racial and ethnic minority groups could be attributed to cultural differences. For example, in one study, Black people—and particularly Black women—were more likely to use language expressing spiritual elements when discussing brain health and concerns about cognitive decline; this fact highlights the importance of recognizing differences in the way individuals frame their concerns; one study suggests that Black women may respond more positively to messages that incorporate spiritual ideas [30]. Similarly, in 2 other studies, Latin American participants expressed spiritual and supernatural ideas related to brain health and cognitive decline [34, 35]. Both studies highlighted the value of collaborating with faith-based organizations to more effectively tailor messages for Latin American populations, and emphasized references to prayer, church-going, gratitude to a higher power, and a connection with God [35]. One study found beliefs and knowledge about memory loss differed across and within Asian American and Pacific Islander (AAPI) participants, and these beliefs were informed by the unique social and structural factors of each AAPI ethnic group [32]. Immigration status and language barriers among various AAPI groups were also found to limit opportunities to engage in social and economic activities in the US, leading to a need for messaging that is not only culturally sensitive but that can also help surmount barriers to accessing appropriate health care [32]. On the other hand, another study found that Filipino American individuals often have a strong biomedical understanding of brain health through workplace exposure to individuals with cognitive impairment; many are employed in healthcare professions, including in long-term care [31].
Among laypersons, sex and gender may also play a role in conceptions of brain health and behaviors to maintain or improve brain health. Women often take the lead in providing healthcare information for their families, highlighting the need to specifically engage this population in early conversations on brain health [44]. Societally influenced traditional gender roles also appeared to affect specific beliefs and behaviors related to cognition. For example, while both women and men understood the importance of physical exercise and social engagement for maintaining cognitive functioning, women endorsed social and physical activities like group exercise classes, whereas men indicated that manual labor and formal employment could fulfill physical exercise and social needs [44].
The studies included in the present review also highlight that conversations around cognition should be tailored to specific patients and audiences, include culturally relevant information, and consider both the social and cultural contexts in which patients live [29,30,31, 37, 39]. The literature also reveals that primary care is just one setting in which to circulate this information; partnering with local communities’ trusted media sources and institutions is important for disseminating brain health messages [31, 33].
Discussion
Our systematic review revealed 4 themes describing barriers to and facilitators of conversations around brain health in primary care: (1) PCCs are hesitant to discuss brain health and cognitive concerns; (2) patients are hesitant to raise cognitive concerns; (3) evidence to guide clinicians in developing treatment plans that address cognitive decline is often poorly communicated; and (4) social and cultural context influence perceptions of brain health and cognition, and therefore can affect clinical engagement.
Although PCCs’ and patients’ hesitation to discuss brain health and cognition was identified in literature from over a decade ago, this hesitation still looms large in clinical practice today. A recent report by the Alzheimer’s Association found that although 75% of PCCs provide direct care for patients with MCI or ADRD, many are uncomfortable diagnosing ADRD, and the vast majority had little to no residency training in ADRD diagnosis [54]. Additionally, stigma [38] and the perception that ADRD interventions are not available or effective [43, 44, 46, 55] make these discussions challenging. These perceptions may be partially due to the need for multimodal rather than singular interventions to effectively address and potentially slow cognitive decline [56].The recent approval of AD disease-modifying therapies may lend new impetus for these conversations by decreasing therapeutic nihilism.
Important innovations in clinician and health system training are occurring now. For example, the Gerontological Society of America has developed the Kickstart, Assess, Evaluate, Refer (KAER) Toolkit for Primary Care Teams to provide practical tools, processes, and strategies for PCCs who wish to initiate conversations about brain health, detect and diagnose ADRD, and provide patients with community-based support [57]. The KAER model identifies 4 broad steps to achieve greater awareness of brain health (“Kickstart”), increase detection of cognitive impairment (“Assess”), initiate earlier diagnostic evaluation (“Evaluate”), and refer people with ADRD (“Refer”). The “Kickstart” phase includes practical recommendations for initiating conversations around brain health and cognitive concerns. These recommendations include raising the topic of brain health during initial patient visits, asking patients about their memory and cognition, and making these discussions part of routine care, among others.
The BOLD Public Health Center of Excellence on Early Detection of Dementia (EDD) has developed a basic toolkit for health systems [58]. Like the KAER model, the BOLD toolkit provides practitioners with practical guidance for having conversations with patients before performing formal dementia screening. The BOLD toolkit emphasizes ways to build trust, use positive framing to normalize conversations about cognition in health care settings, and be ready with simple statements that explain the importance of cognition in everyday functioning.
Although resources like the KAER model and the BOLD EDD toolkit provide practical strategies that can be adapted to meet the needs of PCCs and their patients, evidence regarding their use in clinical practice is undeveloped. To further assist PCCs, Figs. 2 and 3 provide examples of hypothetical conversations about cognition, initiated by a PCC, both with patients who do and do not express concerns about cognitive decline. Both conversations incorporate elements from the KAER and BOLD toolkits, starting with raising the topic of brain health and normalizing the conversation as part of a routine healthcare visit. After specifically asking the patient if they have any memory or cognition concerns, the PCC builds trust by listening and responding to the patient’s concerns, offering guidance that reassures the patient that the PCC is a trusted source of information on brain health. Finally, the PCC encourages the brain health conversation to continue by providing tangible resources and explaining how brain health fits into a larger picture of overall health.
These conversations are quick but informative and allow PCCs to incorporate conversations about brain health into routine visits, even when no cognitive concern exists. Building basic brain health awareness as part of primary care is an important foundation for preventive interventions, when possible, and identifying decline when it does occur. When cognitive impairment is suspected, the language and content of these conversations should be tailored to the patient’s social and cultural context. For example, nurse-led, faith-based, culturally tailored educational programs about ADRD and early detection have generally been positively received by members of the Black community [59]. Although this education is provided in a group setting instead of in an individual encounter, the culturally relevant messaging developed as part of these programs can serve as a guide for physicians. This point is particularly important given how stigma and sociocultural differences can negatively impact health-seeking behaviors related to cognitive concerns and discourage inclusion in clinical research and advances in clinical care [60,61,62,63,64,65]. Starting conversations in individuals who are at risk because of age, comorbid conditions, or known risk factors—but are still cognitively normal—may increase a patient’s trust and openness, as well as the clinician’s comfort in initiating discussion should cognitive symptoms start to appear.
In addition to the resources and strategies that can help guide provider-patient conversations about brain health, there is also a need for a system-level approach to implementation that creates demand for these provider-patient conversations. The Agile processes (i.e., Agile Innovation, Agile Implementation, and Agile Diffusion) provide a framework for facilitating the rapid uptake and diffusion of evidence-based solutions [66, 67]. The Agile framework has been used to guide the implementation and evaluation of evidence-based interventions for dementia care [68], and the Agile principles can also be applied to early conversations around brain health in the primary care setting. One concept used within the Agile processes is the “nudge,” which refers to a small change in environment that can positively influence individuals’ behaviors and choices. A simple and easily implemented strategy could be a poster on a clinic wall encouraging patients to ask questions about their cognition. Another key component of the approach is the idea of creating market demand for an evidence-based intervention prior to rollout and scale-up within an organization. In the context of discussions about brain health, healthcare policies may play a role in driving this demand. As one example, in 2011, Medicare established the Annual Wellness Visit, which requires providers to discuss cognition and cognitive concerns with their Medicare patients [49]. Although the literature has not conclusively determined the effectiveness of the Annual Wellness Visit in improving dementia diagnosis [69,70,71], this policy feature provides an avenue for incentivizing brain health conversations. We recommend considering Agile processes and concepts such as nudges and market demand when looking to implement early conversations about cognition at the practice or system level.
This systematic review is subject to several limitations. Only English-language studies conducted in the US were included, so some relevant literature was excluded by design during the screening process. Studies assessing conversations with patients formally screened for or diagnosed with MCI or ADRD were also excluded, though the results of these studies may also contain valuable information that can be applied earlier in a patient’s journey. However, many patients are unaware they have been diagnosed with MCI or ADRD [72, 73], which means that the studies we reviewed may have included patients who qualify for a formal diagnosis. In addition, a majority of the included articles were published more than 10 years ago, presenting another limitation and highlighting a gap in the literature. This gap presents an opportunity to conduct research on barriers and facilitators to early conversations around brain health and cognitive concerns in primary care settings. Such research should include implementation research to evaluate the real-world effectiveness of interventions that aim to mitigate barriers and optimize facilitators to these important conversations.
Conclusions
In this systematic review we sought to identify barriers to and facilitators of early conversations around brain health and cognitive concerns between PCCs and their patients before patients receive a formal screening or diagnosis of MCI or ADRD. Findings from this review revealed that both PCCs and patients are hesitant to initiate these conversations, evidence to inform brain health interventions is often poorly communicated, and social and cultural factors impact clinical engagement between PCCs and their patients.
These themes highlight the importance of framing discussions about brain health and cognitive concerns as part of routine primary care, clearly translating knowledge about the effectiveness of brain health interventions to clinicians in order to reduce therapeutic nihilism, and partnering with communities to tailor education to patients’ social and cultural contexts. Putting these key suggestions within the context of the broader literature also underscores the importance of implementing system-level approaches to facilitate these conversations between PCCs and their patients. Future research should identify additional barriers that hinder early conversations about brain health and cognition between PCCs and their patients and evaluate the effectiveness and feasibility of both interpersonal and system-level approaches to address these barriers.
Availability of data and materials
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
Abbreviations
- AAPI:
-
Asian American and Pacific Islander
- ADRD:
-
Alzheimer’s disease and related dementias
- BOLD:
-
Building Our Largest Dementia Infrastructure for Alzheimer’s Act
- CDC:
-
Centers for Disease Control and Prevention
- EDD:
-
Early Detection of Dementia
- FINGER:
-
Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability trial
- KAER:
-
Kickstart, Assess, Evaluate, Refer
- MMAT:
-
Mixed methods appraisal tool
- MCI:
-
Mild cognitive impairment
- PCC:
-
Primary care clinician
- PRISMA:
-
Preferred Reporting Items for Systematic reviews and Meta-Analyses
References
Norton S, Matthews FE, Barnes DE, Yaffe K, Brayne C. Potential for primary prevention of Alzheimer’s Disease: an analysis of population-based data. Lancet Neurol Aug. 2014;13(8):788–94. https://doi.org/10.1016/S1474-4422(14)70136-X.
Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet Aug. 2020;8(10248):413–46. https://doi.org/10.1016/S0140-6736(20)30367-6.
Majoka MA, Schimming C. Effect of social determinants of health on cognition and risk of Alzheimer Disease and related Dementias. Clin Ther Jun. 2021;43(6):922–9. https://doi.org/10.1016/j.clinthera.2021.05.005.
Marengoni A, Rizzuto D, Fratiglioni L, et al. The effect of a 2-year intervention consisting of diet, physical exercise, cognitive training, and monitoring of vascular risk on chronic morbidity-the FINGER randomized controlled trial. J Am Med Dir Assoc Apr. 2018;19(4):355–360e1. https://doi.org/10.1016/j.jamda.2017.09.020.
Ngandu T, Lehtisalo J, Solomon A, et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet Jun. 2015;6(9984):2255–63. https://doi.org/10.1016/S0140-6736(15)60461-5.
Rosenberg A, Ngandu T, Rusanen M, et al. Multidomain lifestyle intervention benefits a large elderly population at risk for cognitive decline and Dementia regardless of baseline characteristics: the FINGER trial. Alzheimers Dement Mar. 2018;14(3):263–70. https://doi.org/10.1016/j.jalz.2017.09.006.
U.S. Department of Health and Human Services. National Plan to Address Alzheimer’s Disease: 2022 Update. 2022; https://aspe.hhs.gov/index.php/reports/national-plan-2022-update. Accessed April 27, 2023.
Centers for Disease Control and Prevention. BOLD Infrastructure for Alzheimer’s Act. 2021; https://www.cdc.gov/aging/bold/index.html. Accessed April 27, 2023.
Alzheimer’s Association. 2020 Alzheimer’s disease facts and figures. Alzheimers Dement. Mar 10 2020;https://doi.org/10.1002/alz.12068.
De Vreese LP, De Salvatore L, Rovesta L, Fabbo A. The management of Dementia in Primary Care. In: Capelli O, editor. Primary care in practice – integration is needed. IntechOpen; 2016.
Bernstein A, Rogers KM, Possin KL, et al. Dementia assessment and management in primary care settings: a survey of current provider practices in the United States. BMC Health Serv Res Nov. 2019;29(1):919. https://doi.org/10.1186/s12913-019-4603-2.
Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon BE, Phillips RS. Association of primary care physician supply with population mortality in the United States, 2005–2015. JAMA Intern Med. Apr 1 2019;179(4):506–514. https://doi.org/10.1001/jamainternmed.2018.7624.
Bardach SH, Schoenberg NE. The role of primary care providers in encouraging older patients to change their lifestyle behaviors. Clin Gerontol Jul-Sep. 2018;41(4):326–34. https://doi.org/10.1080/07317115.2017.1376029.
Reynolds R, Dennis S, Hasan I, et al. A systematic review of chronic Disease management interventions in primary care. BMC Fam Pract Jan. 2018;9(1):11. https://doi.org/10.1186/s12875-017-0692-3.
Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. https://doi.org/10.1111/j.1468-0009.2005.00409.x.
Fernandes B, Goodarzi Z, Holroyd-Leduc J. Optimizing the diagnosis and management of Dementia within primary care: a systematic review of systematic reviews. BMC Fam Pract Aug. 2021;11(1):166. https://doi.org/10.1186/s12875-021-01461-5.
Giezendanner S, Monsch AU, Kressig RW, et al. General practitioners’ attitudes towards early diagnosis of Dementia: a cross-sectional survey. BMC Fam Pract May. 2019;20(1):65. https://doi.org/10.1186/s12875-019-0956-1.
Holsinger T, Boustani M, Abbot D, Williams JW. Acceptability of Dementia screening in primary care patients. Int J Geriatr Psychiatry Apr. 2011;26(4):373–9. https://doi.org/10.1002/gps.2536.
Karimi L, Mahboub-Ahari A, Jahangiry L, Sadeghi-Bazargani H, Farahbakhsh M. A systematic review and meta-analysis of studies on screening for mild cognitive impairment in primary healthcare. BMC Psychiatry Feb. 2022;9(1):97. https://doi.org/10.1186/s12888-022-03730-8.
Liss JL, Seleri Assuncao S, Cummings J, et al. Practical recommendations for timely, accurate diagnosis of symptomatic Alzheimer’s Disease (MCI and Dementia) in primary care: a review and synthesis. J Intern Med Aug. 2021;290(2):310–34. https://doi.org/10.1111/joim.13244.
Moore A, Frank C, Chambers LW. Role of the family physician in Dementia care. Can Fam Physician Oct. 2018;64(10):717–9.
Porsteinsson AP, Isaacson RS, Knox S, Sabbagh MN, Rubino I. Diagnosis of early Alzheimer’s Disease: clinical practice in 2021. J Prev Alzheimers Dis. 2021;8(3):371–86. https://doi.org/10.14283/jpad.2021.23.
Sabbagh MN, Boada M, Borson S, et al. Early detection of mild cognitive impairment (MCI) in primary care. J Prev Alzheimers Dis. 2020;7(3):165–70. https://doi.org/10.14283/jpad.2020.21.
Scott J, Mayo AM. Instruments for detection and screening of cognitive impairment for older adults in primary care settings: a review. Geriatr Nurs May-Jun. 2018;39(3):323–9. https://doi.org/10.1016/j.gerinurse.2017.11.001.
Sabbagh MN, Perez A, Holland TM, et al. Primary prevention recommendations to reduce the risk of cognitive decline. Alzheimers Dement Aug. 2022;18(8):1569–79. https://doi.org/10.1002/alz.12535.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev Mar. 2021;29(1):89. https://doi.org/10.1186/s13643-021-01626-4.
Hong QN, Gonzalez-Reyes A, Pluye P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the mixed methods Appraisal Tool (MMAT). J Eval Clin Pract. 2018;24(3):459–67. https://doi.org/10.1111/jep.12884.
Friedman DB, Rose ID, Anderson LA et al. Beliefs and communication practices regarding cognitive functioning among consumers and primary care providers in the United States, 2009. Prev Chronic Dis. Apr 18 2013;10:E58; quiz 8–13. https://doi.org/10.5888/pcd10.120249.
Corwin SJ, Laditka JN, Laditka SB, Wilcox S, Liu R. Attitudes on aging well among older African americans and whites in South Carolina. Prev Chronic Dis Oct. 2009;6(4):A113.
Price AE, Corwin SJ, Friedman DB, Laditka SB, Colabianchi N, Montgomery KM. Older adults’ perceptions of physical activity and cognitive health: implications for health communication. Health Educ Behav Feb. 2011;38(1):15–24. https://doi.org/10.1177/1090198110369764.
Laditka SB, Tseng W, Price AE, et al. Beliefs about promoting cognitive health among Filipino americans who care for persons with Dementia. Int J Aging Hum Dev. 2012;75(3):273–96. https://doi.org/10.2190/AG.75.3.d.
Zhai S, Kim B, Li J, et al. Perceptions and beliefs of memory loss and Dementia among Korean, Samoan, Cambodian, and Chinese older adults: a cross-cultural qualitative study. J Gerontol Nurs Jun. 2022;48(6):40–8. https://doi.org/10.3928/00989134-20220506-03.
Light SW, Dohan D, Possin KL, et al. Perceptions of and knowledge acquisition about brain health and aging among latin American immigrants: a qualitative paper. Clin Gerontol Mar-Apr. 2023;46(2):180–94. https://doi.org/10.1080/07317115.2022.2088324.
Sharkey JR, Sharf BF, St John JA. Una persona derechita (staying right in the mind): perceptions of spanish-speaking Mexican American older adults in South Texas colonias. Gerontologist Jun. 2009;49(Suppl 1):79–85. https://doi.org/10.1093/geront/gnp086.
Weiner-Light S, Rankin KP, Lanata S, Possin KL, Dohan D, Bernstein Sideman A. The role of spirituality in conceptualizations of health maintenance and healthy aging among latin American immigrants. Am J Geriatr Psychiatry Nov. 2021;29(11):1079–88. https://doi.org/10.1016/j.jagp.2021.04.017.
Friedman DB, Laditka JN, Hunter R, et al. Getting the message out about cognitive health: a cross-cultural comparison of older adults’ media awareness and communication needs on how to maintain a healthy brain. Gerontologist Jun. 2009;49(Suppl 1):50–60. https://doi.org/10.1093/geront/gnp080.
Friedman DB, Laditka SB, Laditka JN, et al. Ethnically diverse older adults’ beliefs about staying mentally sharp. Int J Aging Hum Dev. 2011;73(1):27–52. https://doi.org/10.2190/AG.73.1.b.
Laditka JN, Laditka SB, Liu R, et al. Older adults’ concerns about cognitive health: commonalities and differences among six United States ethnic groups. Ageing Soc. 2011;31(7):1202–28.
Laditka SB, Corwin SJ, Laditka JN, et al. Attitudes about aging well among a diverse group of older americans: implications for promoting cognitive health. Gerontologist Jun. 2009;49(Suppl 1):30–9. https://doi.org/10.1093/geront/gnp084.
Wilcox S, Sharkey JR, Mathews AE, et al. Perceptions and beliefs about the role of physical activity and nutrition on brain health in older adults. Gerontologist Jun. 2009;49(Suppl 1):61–71. https://doi.org/10.1093/geront/gnp078.
Abdelrahman NG, Haque R, Polverento ME, Wendling A, Goetz CM, Arnetz BB. Brain health: attitudes towards technology adoption in older adults. Healthc (Basel). 2020;9(1):23. https://doi.org/10.3390/healthcare9010023.
Hochhalter AK, Bryant LL, Hunter R, et al. Multisite qualitative study of primary care physicians’ and midlevel providers’ self-reported practices and perceptions about maintaining cognitive health. Prev Chronic Dis. 2012;9:E169. https://doi.org/10.5888/pcd9.120050.
Olscamp K, Tang W, Choi SK, Kannaley K, Wilcox S, Friedman DB. Physical activity and brain health: an analysis of messages from organizations and caregiver perceptions. Gerontol Geriatr Med Jan-Dec. 2019;5:2333721419855794. https://doi.org/10.1177/2333721419855794.
Wu B, Goins RT, Laditka JN, Ignatenko V, Goedereis E. Gender differences in views about cognitive health and healthy lifestyle behaviors among rural older adults. Gerontologist Jun. 2009;49(Suppl 1):72–8. https://doi.org/10.1093/geront/gnp077.
Day KL, Friedman DB, Laditka JN, et al. Prevention of cognitive impairment: physician perceptions and practices. J Appl Gerontol. 2012;31(6):743–54.
Onafraychuk D, Sanders EC, Harrell ER, Boot WR. Exploring individuals’ willingness to engage in interventions to improve cognitive health and prolong late-life independence: an extension of Harrell, Kmetz, and Boot (2019). J Cogn Enhanc. Jun 2021;5(2):259–265. https://doi.org/10.1007/s41465-020-00197-x.
Adelman RD, Greene MG, Friedmann E. Discussions about cognitive impairment in first medical visits: older patients’ perceptions and preferences. Am J Alzheimers Dis Other Demen Jul-Aug. 2004;19(4):233–8. https://doi.org/10.1177/153331750401900409.
Warren-Findlow J, Price AE, Hochhalter AK, Laditka JN. Primary care providers’ sources and preferences for cognitive health information in the United States. Health Promot Int Dec. 2010;25(4):464–73. https://doi.org/10.1093/heapro/daq043.
Jacobson M, Thunell J, Zissimopoulos J. Cognitive assessment at Medicare’s annual wellness visit in fee-for-service and Medicare Advantage plans. Health Aff (Millwood) Nov. 2020;39(11):1935–42. https://doi.org/10.1377/hlthaff.2019.01795.
Mace RA, Popok PJ, Hopkins SW, Fishbein NS, Vranceanu AM. Adaptation and virtual feasibility pilot of a mindfulness-based lifestyle program targeting modifiable Dementia risk factors in older adults. Aging Ment Health Feb 1 2022:1–13. https://doi.org/10.1080/13607863.2022.2032600.
Wolf-Klein G, Pekmezaris R, Chin L, Weiner J. Conceptualizing Alzheimer’s Disease as a terminal medical Illness. Am J Hosp Palliat Care. 2007;24(1):77–82. https://doi.org/10.1177/1049909106295297.
Hickman RA, Faustin A, Wisniewski T. Alzheimer Disease and its growing epidemic: risk factors, biomarkers, and the urgent need for therapeutics. Neurol Clin. 2016;34(4):941–53. https://doi.org/10.1016/j.ncl.2016.06.009.
Timmons S, Fox S. Palliative care for people with Dementia. Handb Clin Neurol. 2023;191:81–105. https://doi.org/10.1016/B978-0-12-824535-4.00013-6.
Alzheimer’s Association. 2022 Alzheimer’s disease facts and figures. Alzheimers Dement. Apr 2022;18(4):700–789. https://doi.org/10.1002/alz.12638.
Judge D, Roberts J, Khandker R, Ambegaonkar B, Black CM. Physician perceptions about the barriers to prompt diagnosis of mild cognitive impairment and Alzheimer’s Disease. Int J Alzheimers Dis. 2019;2019:3637954. https://doi.org/10.1155/2019/3637954.
Chalfont G, Milligan C, Simpson J. A mixed methods systematic review of multimodal non-pharmacological interventions to improve cognition for people with Dementia. Dement (London) May. 2020;19(4):1086–130. https://doi.org/10.1177/1471301218795289.
Gerontological Society of America. The GSA KAER Toolkit for primary care teams: supporting conversations about brain health, timely detection of cognitive impairment, and accurate diagnosis of dementia. Accessed September 20., 2022. https://www.geron.org/images/gsa/Marketing/KAER/GSA_KAER-Toolkit_2020_Final.pdf.
BOLD Public Health Center of Excellence. Early Detection of Dementia Toolkit – Health Systems. Accessed January 6., 2023. https://bolddementiadetection.org/wp-content/uploads/2022/09/2022-BOLD-Early-Detection-of-Dementia-Toolkit-Health-systems.pdf.
Epps F, Alexander K, Brewster GS, et al. Promoting Dementia awareness in African-American faith communities. Public Health Nurs. 2020;37(5):715–21. https://doi.org/10.1111/phn.12759.
Alzheimer’s Association. Issues Brief: LGBT and Dementia. Accessed January 30., 2023. https://www.alz.org/media/documents/lgbt-dementia-issues-brief.pdf.
Alzheimer’s Association. African-Americans and Alzheimer’s disease: the silent epidemic. Accessed January 31., 2023. https://www.alz.org/media/documents/african-americans-silent-epidemic-r.pdf.
Alzheimer’s Impact Movement, Alzheimer’s Association. Race, ethnicity, and Alzheimer’s fact sheet. Accessed January 31., 2023. https://aaic.alz.org/downloads2020/2020_Race_and_Ethnicity_Fact_Sheet.pdf.
Alzheimer’s Disease International. World Alzheimer Report. 2012. Accessed January 30, 2023. https://www.alzint.org/resource/world-alzheimer-report-2012/.
Hargrave R. Dementia Assessment in African americans. In: Yeo G, Gerdner LA, Gallagher-Thompson D, editors. Ethnicity and the Dementias. 3rd ed. Routledge; 2018. Chap. 4.
Jernigan M, Boyd AD, Noonan C, Buchwald D. Alzheimer’s Disease knowledge among American indians and Alaska Natives. Alzheimers Dement (N Y). 2020;6(1):e12101. https://doi.org/10.1002/trc2.12101.
Boustani M, Holden RJ, Azar J, Solid CA. The Agile Network: a model to Foster Innovation, implementation, and Diffusion in Healthcare Settings. Beaver’s Pond Press; 2020.
Holden RJ, Boustani MA, Azar J. Agile Innovation to transform healthcare: innovating in complex adaptive systems is an everyday process, not a light bulb event. BMJ Innovations. 2021;7(2):499–505.
Boustani M, Alder CA, Solid CA. Agile implementation: a blueprint for implementing evidence-based healthcare solutions. J Am Geriatr Soc Jul. 2018;66(7):1372–6. https://doi.org/10.1111/jgs.15283.
Fowler NR, Campbell NL, Pohl GM, et al. One-year effect of the Medicare annual wellness visit on detection of cognitive impairment: a cohort study. J Am Geriatr Soc May. 2018;66(5):969–75. https://doi.org/10.1111/jgs.15330.
Lind KE, Hildreth K, Lindrooth R, Morrato E, Crane LA, Perraillon MC. The effect of direct cognitive assessment in the Medicare annual wellness visit on Dementia diagnosis rates. Health Serv Res Apr. 2021;56(2):193–203. https://doi.org/10.1111/1475-6773.13627.
Thunell JA, Jacobson M, Joe EB, Zissimopoulos JM. Medicare’s annual wellness visit and diagnoses of Dementias and cognitive impairment. Alzheimers Dement (Amst). 2022;14(1):e12357. https://doi.org/10.1002/dad2.12357.
Amjad H, Roth DL, Sheehan OC, Lyketsos CG, Wolff JL, Samus QM. Underdiagnosis of Dementia: an observational study of patterns in diagnosis and awareness in US older adults. J Gen Intern Med. 2018;33(7):1131–8. https://doi.org/10.1007/s11606-018-4377-y.
Chambers D, Cantrell A, Sworn K, Booth A. Assessment and management pathways of older adults with mild cognitive impairment: descriptive review and critical interpretive synthesis. Health and Social Care Delivery Research. 2022. https://doi.org/10.3310/XLUJ6074. ;Health and Social Care Delivery Research.
Acknowledgements
Editorial support was provided by Clare Sonntag and Jennifer Reed of Health & Wellness Partners, LLC, and funded by Genentech, Inc., a member of the Roche Group, in accordance with Good Publication Practice guidelines.
Funding
Quentin O’Brien and Andrea Morrello are employees of Health & Wellness Partners, LLC, which received payment from Genentech for services rendered.
Author information
Authors and Affiliations
Contributions
SB, GS, QO, AM, and MB contributed to the conception of the work and contributed to the design of the work. QO and AM performed data acquisition/analysis, and SB, GS, QO, AM, and MB interpreted the data. The work was drafted and substantively revised by SB, GS, QO, AM, and MB, and all authors read, revised, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Dr. Borson (SB) conducts research focused on improving early detection of dementia in health care settings and is supported by grants from the Centers for Disease Control and Prevention and the National Institutes of Health. SB owns the copyright on the Mini-Cog, a cognitive screening tool for dementia detection in primary care. SB co-leads the BOLD Public Health Center of Excellence on Early Detection of Dementia. SB provides technical assistance to health care and public health organizations and is an advisor to multiple pharmaceutical and educational companies (Biogen, Eisai, Lilly, Genentech, and Medscape) seeking to disseminate best practices for dementia detection and care. Dr. Small (GS) is an advisor for Acadia, Biogen, Corium, Genentech, Roche, Handok, Herbalife, Lundbeck, McCormick Science Institute, Otsuka, Reckitt Bencksier Group, and Theravaules. He also has equity in Ceremark Pharma. Dr. Boustani (MB) serves as a chief scientific officer and cofounder of BlueAgilis; and the chief health officer of DigiCARE Realized, Inc. MB has equity interest in Blue Agilis, Inc; DigiCARE Realized, Inc; Preferred Population Health Management LLC; and MyShyft, Inc (previously known as RestUp, LLC). MB serves as an advisory board member for Acadia Pharmaceuticals; Eisai, Inc; Biogen; Lilly, and Genentech. These conflicts have been reviewed by Indiana University and has been appropriately managed to maintain objectivity. Quentin O’Brien and Andrea Morrello are employees of Health & Wellness Partners, LLC, which received payment from Genentech for services rendered. They have no other conflicts of interest to disclos
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix A.
PRISMA 2020 Checklist
Additional file 2: Appendix B.
Database Search Algorithms
Additional file 3: Appendix C.
Mixed Methods Appraisal Tool (MMAT) Quality Assessment
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Borson, S., Small, G.W., O’Brien, Q. et al. Understanding barriers to and facilitators of clinician-patient conversations about brain health and cognitive concerns in primary care: a systematic review and practical considerations for the clinician. BMC Prim. Care 24, 233 (2023). https://doi.org/10.1186/s12875-023-02185-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-023-02185-4