Abstract
A gap exists between guidelines and real-world clinical practice for the management and treatment of chronic obstructive pulmonary disease (COPD). Although this has narrowed in the last decade, there is room for improvement in detection rates, treatment choices and disease monitoring. In practical terms, primary care practitioners need to become aware of the huge impact of COPD on patients, have non-judgemental views of smoking and of COPD as a chronic disease, use a holistic consultation approach and actively motivate patients to adhere to treatment.
This article is based on discussions at a virtual meeting of leading Nordic experts in COPD (the authors) who were developing an educational programme for COPD primary care in the Nordic region. The article aims to describe the diagnosis and lifelong management cycle of COPD, with a strong focus on providing a hands-on, practical approach for medical professionals to optimise patient outcomes in COPD primary care.
Similar content being viewed by others
Background
Approximately 384 million people worldwide have chronic obstructive pulmonary disease (COPD) [1], and it is estimated that over half of patients with COPD may be undiagnosed [2]. According the World Health Organization, COPD is the third leading cause of death globally [3] and costs are estimated to be in excess of 100 billion dollars per year [4, 5]. Most patients with COPD are fully managed in primary care [6, 7]. As the first-line healthcare provider, and often the gatekeeper to secondary care, primary care is not only responsible for the early detection of chronic diseases like COPD, but it also has a unique opportunity to provide patients with evidence-based treatments. Currently, there is a gap between COPD guidelines and real-world clinical practice, and although this has narrowed in the last decade [8, 9], there is room for improvement in detection rates, treatment choices and disease monitoring [8, 10,11,12,13,14]. This article is based on discussions that took place during a virtual meeting on 15 June 2020 involving leading Nordic experts in COPD (the authors). The purpose of the meeting was to finalise a COPD educational programme that had been developed for primary care in the Nordic region. During the course of discussions, the authors agreed there was a scientific need to author this opinion piece, with a strong emphasis on providing a hands-on, practical approach for General Practice. Thus, we discuss the burden of disease, the impact of symptoms and exacerbations and the unmet needs in the lifelong clinical management cycle of COPD.
Main text
Burden of disease
COPD is a heterogeneous disease characterised by persistent respiratory symptoms and airflow limitation [1]. It provides a significant burden for patients and society due to the natural progression of COPD, reduced daily/physical activities, exacerbations and impact on work and social isolation, which often leads to psychological conditions such as anxiety and depression [1, 15, 16]. Together, these factors decrease health-related quality of life (HRQL) and increase mortality, compared with the general population [1], and are further confounded by a number of comorbidities that are frequently associated with COPD, including cardiovascular, metabolic and other chronic conditions (see the ‘Common comorbidities’ section for additional details [17, 18]).
How does the disease manifest?
Symptoms of COPD may include chronic and progressive dyspnoea, chronic cough, sputum production, chest tightness or fatigue [1, 19,20,21]. In many patients, chronic cough with or without sputum production may be intermittent and may precede the development of airflow limitation by many years [1, 22]. Indeed, the occurrence of a productive cough in young smokers constitutes a substantial risk of developing COPD in later life [23]. Conversely, dyspnoea and decline in health status are weakly correlated with airflow limitation [19, 21]. As a result of this variation, symptoms may not be obvious until forced expiratory volume in 1 s (FEV1) has declined to approximately 50–60% of predicted, therefore COPD typically remains undiagnosed until it has reached at least moderate severity [24]. COPD should therefore be considered in any patient with a history of exposure to risk factors. Patients with COPD may also be more prone to ‘winter colds’ or ‘acute bronchitis’, and primary care practitioners should consider the possibility of COPD in middle-aged or older smokers with recurrent respiratory tract infections [1, 25, 26].
Dyspnoea is a key everyday modality
Dyspnoea due to airflow limitation is the main symptom of COPD and is often the reason why patients with COPD seek medical care [19]. Dyspnoea is a problem not only in patients with severe disease, but also in patients with mild-to-moderate disease, where symptoms may only be evident during exercise [27, 28]. Milder symptoms may be dismissed by the patient as being related to age, general fitness or other factors [29], and patients typically do not seek medical help until symptoms have a substantial impact on their daily life [1, 30].
The cause of dyspnoea is multifactorial but is dominated by parenchymal destruction and loss of elastic recoil, which leads to the collapse of the small airways during expiration and thus longer expiration times (Fig. 1). As the respiratory rate increases during exercise, loss of elastic recoil means that patients may not be able to exhale completely before their next breath [31]. This, in turn, leads to a gradual increase in end-expiratory lung volume, resulting in ‘dynamic hyperinflation’, which contributes considerably to the sensation of dyspnoea during exercise [32,33,34] and leads to reduced daily physical activity [35]. Luminal obstruction due to mucus plugging and increased airway wall thickness may further aggravate dyspnoea [36, 37]. Furthermore, the severity of dyspnoea [38, 39] along with the magnitude of hyperinflation [40] are both strong predictors of mortality.
The pathophysiological background to dyspnoea. Alveolar wall destruction leads to loss of elastic ‘passive’ recoil of the alveoli and support for the bronchiole is lost, leading to bronchiole collapse, which in turn results in air trapping, static hyperinflation and increased functional residual capacity [32, 41,42,43]
Sarcopenia, which is common in COPD, adds to the impact of dyspnoea due to reduced muscle mass leading to decreased exercise capacity and increased breathlessness [44]. Heart failure is also a common comorbidity in patients with COPD and can contribute to a sensation of dyspnoea [17, 45].
Symptoms vary by day and season. Daily symptoms are typically bimodal in distribution, being particularly troublesome in the early morning and in the evening/at night-time, while seasonal variation in symptoms leads to a peak in exacerbations through autumn and winter [46,47,48].
Previous studies have found that 37% of all patients and 46% of patients with severe COPD reported worse symptoms in the morning than at any other time of day [47], and morning symptoms have been associated with general physical impairment [49]. Similarly, 46% of all patients and 61% of patients with severe COPD have reported evening/night-time symptoms [47, 48]. Singh et al. found that nearly two-thirds of patients experienced night-time symptoms, regardless of disease severity [50]. During the night, coughing was the most prevalent symptom, reported in 43% of patients; bringing up phlegm, dyspnoea and wheezing were also reported in around one-third of patients. Night-time symptoms significantly impact sleep quality [50], which may lead to exhaustion and further physical decline.
In a study by Partridge et al., although many patients with COPD regarded respiratory symptoms during morning routines as bothersome, most patients were not taking their COPD medication in time for it to exert its effect [47]. This suggests that physicians should actively question patients about their morning activities and evening/night-time symptoms to fully assess disease impact and optimise the timing of treatment [47].
Causes and drivers of COPD
According to the classical Fletcher–Peto model [51], FEV1 decreases gradually over a lifetime. In susceptible individuals exposed to smoke or other noxious gases who develop COPD, the decline progresses more rapidly. However, the rate of lung function decline in COPD is highly variable, being negatively affected by smoking and exacerbations, but also remains relatively stable for long periods in many patients [52]. Increased incidence of COPD has been associated with indoor and outdoor air pollution [53] (particularly the burning of biomass/solid fuels in developing countries and rural areas [54, 55]), occupational exposure to dust and gases [56, 57] and lower socioeconomic status and poverty [1, 58]; other risk factors include genetic predisposition, abnormal lung development and accelerated ageing [1].
One major driver of the disease process in COPD is ongoing chronic inflammation of the small airways, known as bronchiolitis [59]. Neutrophilic granulocytes, CD8+ lymphocytes and macrophages were initially identified as being among the most important in the pathogenesis of COPD [60], but we now know that other immune cells, such as eosinophils, are also involved [61]. Recruitment and activation of immune cells and release of inflammatory mediators lead to mucous hypersecretion, luminal obstruction/mucous plugging and tissue destruction [37, 41]. Inflammation is also coupled with a dysfunctional repair/remodelling process that destroys the alveolar walls and thickens the walls of the airways [37, 42]. Pulmonary vascular remodelling may also result in pulmonary hypertension and right-sided heart failure (cor pulmonale) [62]. Bronchiectasis may also add to the symptom burden [63].
Exacerbations
COPD is also characterised by periodic acute worsening of symptoms beyond normal day-to-day variation, known as acute exacerbations; symptoms can last several weeks, and severe exacerbations result in hospitalisation and increased risk of death (Table 1) [1, 64].
Exacerbations are characterised by an initial increase in airway inflammation, resulting in airway oedema, mucus production and bronchoconstriction (Fig. 2) [68]. An acute exacerbation is a serious event triggering a catastrophic cascade that is potentially overwhelming and life-threatening, akin to a ‘stroke of the lungs’ [69]. There is also emerging evidence showing that a proportion of patients with mild COPD may be susceptible to exacerbations [70]; however, at present, due to their mild disease, these patients might not be identified for intervention [71]. It is vital to improve early detection and diagnosis of patients with mild COPD in primary care. Smoking cessation and/or recognising harmful work exposures early may halt disease progression, and simple measures may be taken to reduce the risk of exacerbations, such as influenza and pneumococcal vaccinations.
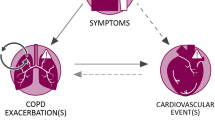
COPD exacerbations are associated with a more rapid decline in FEV1 [71,72,73,74], poorer HRQL [71, 75,76,77], hospitalisations [1, 72], increased risk of cardiovascular disease (CVD) [78,79,80,81], risk of further exacerbations [82] and increased mortality [1, 39, 82,83,84,85,86,87]. Moreover, the risk of severe exacerbation or death has been found to increase with each subsequent exacerbation [82]. Even a single exacerbation can drastically decrease HRQL (St George’s Respiratory Questionnaire total score) [75, 88], with HRQL remaining worse 6 months later in some patients, versus no exacerbations [89]. In addition, damage from exacerbations has been found to go beyond the lungs due to the associated systemic inflammation during the exacerbation [68] and may increase the risk of thromboembolism, stroke, myocardial infarction and cardiovascular mortality, particularly following a severe exacerbation [78, 90,91,92]. While in around 30% of exacerbation cases, no clear cause is found [93], exacerbations are known to be triggered by multiple factors, including infections and exposure to particulate matter [1, 94]. In patients with moderate/severe COPD, bacterial pathogens account for 40–50%, viral pathogens for 30–40% and atypical bacteria for 5–10% of exacerbations [94]; following an exacerbation, bacterial colonisation has been found to rise to 70%, with Haemophilus influenzae, Streptococcus pneumoniae and Moraxella catarrhalis being the most common species found [95]. While many patients take some action (e.g. rest, cut down on smoking, increase medication etc.), over 40% of patients do not contact healthcare providers during an exacerbation [96]. Under-treatment is also common in patients hospitalised because of severe COPD exacerbations [97]. Across four different studies, between 40 and 68% of exacerbations were under-recognised, under-reported and thus under-treated; moreover, this proportion was largely unchanged over 12 years (Fig. 3) [76, 98,99,100]. This suggests that patients with COPD require education on exacerbation symptoms and when to seek professional healthcare [101].
Several factors may predict risk of future exacerbations (Table 2) and should be considered when initiating treatment and at follow-up/annual review.
Elevated blood eosinophils are associated with higher COPD-related hospital readmission rates and all-cause readmission [108] (see the ‘Pharmacological treatment of COPD’ section).
Diagnosis of COPD
COPD should be considered in any patient with clinical symptoms and risk factors for the disease (predominantly smoking). Diagnosis is confirmed by a post-bronchodilator FEV1/forced vital capacity (FVC) ratio < 0.70 [1] or below the lower limit of normal. Of note, the FEV1/FVC ratio has a natural decline with age, and the fixed ratio may lead to an underestimation of COPD in younger patients and an overestimation in elderly patients [109,110,111].
Spirometry is important not only for the diagnosis of COPD, but also to classify the severity of airflow limitation (based on FEV1% predicted) [1]. In addition, baseline and post-baseline FEV1 measurements can be compared with future spirometric assessments to identify patients who demonstrate a rapid decline in lung function (rapid decliners), and may be used when considering alternative diagnoses, such as when symptoms appear disproportionate to the degree of airflow obstruction [1]. It is important to ensure that healthcare professionals first carry out spirometry [112] and that those who carry out spirometry are appropriately trained [113], as incorrect interpretation or performance of the procedure readily leads to misdiagnosis of COPD [114].
Reversibility with a fast-acting bronchodilator has historically been used to distinguish asthma from COPD; however, it is now accepted that significant reversibility (FEV1 ≥ 12% and ≥ 200 mL change from baseline) or FVC ≥10% is at least as common in patients with COPD, despite having no features of asthma [115,116,117,118], and can vary in the same patient between assessments for both asthma and COPD [119, 120]. A significantly improved FEV1 with normalisation of the FEV1/FVC ratio post-bronchodilator or post 4–12 weeks of inhaled corticosteroids (ICS) means that COPD, but not asthma, can be excluded.
Once confirmed as COPD, phenotyping is important to ensure optimal pharmacological and non-pharmacological treatment [1]. Typically, patients with COPD and low eosinophil counts have a poor response to ICS while patients with higher levels of eosinophils or asthma–COPD overlap have a better response to ICS [1]. Another phenotype of importance, with regard to medication, is the frequent exacerbator, defined as patients with ≥2 exacerbations per year [121]. Other phenotypes described are chronic bronchitis, emphysematous and rare exacerbator; emerging COPD phenotypes included pulmonary cachexia phenotype, overlap COPD and bronchiectasis, upper lobe-predominant emphysema phenotype, rapid decliner, comorbidities or systemic phenotype, α-1 antitrypsin deficiency and no-smoking COPD [122].
COPD is often overlooked in the initial consultation between physician and patient. Some patients with COPD appear to be asymptomatic, adapt to symptoms and adjust their daily activities to reduce their occurrence [29]; thus, it is vital that patients are asked the correct questions during the consultation with their physician so that as much information can be obtained as possible. It is only by understanding the impact of COPD on multi-morbidities or other health issues that a patient can be optimally prioritised in primary healthcare [123]. Furthermore, in order to maximise the window of opportunity to impact disease progression (e.g. via smoking cessation), it is necessary to be proactive and diagnose early during the mild disease stage [124].
COPD severity and characterisation by the ABCD assessment tool
Whereas the Global Initiative for Chronic Obstructive Lung Disease (GOLD) once focussed primarily on airflow limitation as a measure of COPD severity (GOLD stages 1–4 – mild-to-very-severe COPD) to characterise patients, the ABCD assessment tool adds patient symptoms (based on the COPD assessment test [CAT] and/or modified Medical Research Council dyspnoea scale [mMRC]) and exacerbation history in the previous 12 months to the assessment (Fig. 4) [1]. Patients in Group A have a low risk of future exacerbations with low symptom burden; patients in Group B have a low risk of future exacerbations but significant symptom burden; patients in Group C have a high risk of future exacerbations and low disease burden; patients in Group D have a high risk of future exacerbations and significant disease burden.
Disease characteristics and initial pharmacological treatment algorithm. aConsider if highly symptomatic (e.g. CAT > 20). bConsider if EOS ≥0.3 × 109 cells/L (≥300 cells/mm3). Reproduced with permission from: Global Initiative for Chronic Obstructive Lung Disease 2021 Report; Figure 4.2. Available from https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.0-16Nov20_WMV.pdf, accessed 18 November 2020. CAT COPD assessment test, COPD chronic obstructive pulmonary disease, EOS eosinophil count, ICS inhaled corticosteroids, LABA long-acting β2-agonist, LAMA long-acting muscarinic antagonist, mMRC modified Medical Research Council dyspnoea scale
In addition to the ABCD assessment, the 6-min walking test is a simple but very useful tool for assessing impaired exercise tolerance [125]; in patients who have experienced a severe exacerbation, lower physical activity levels are associated with increased all-cause mortality [126].
Differential diagnoses – could it be something else?
Diagnosing COPD can sometimes be challenging and, particularly as it is a lifelong diagnosis, it is of utmost importance that the clinician gives full consideration to alternative diagnoses and is aware of the many pitfalls and potential impact of misdiagnosis of COPD. Clinical history, patient characteristics and exposure are important considerations, in addition to spirometry, to differentiate not only between obstructive lung diseases (asthma, bronchiectasis and COPD) but also restrictive lung disease and heart failure, as these may both be misinterpreted as COPD or may co-exist with COPD (Table 3) [1, 127, 128].
Other useful diagnostic tools include blood tests for haemoglobin, erythrocyte sedimentation rate, eosinophil count and N-terminal pro B-type natriuretic peptide (NT-proBNP). Electrocardiograms, chest X-rays and echocardiography in patients with increased NT-proBNP may detect the presence of significant comorbidities, such as CVD, heart failure, lung cancer, pleural disease and changes associated with COPD [1, 129,130,131].
Computed tomography (CT) or high-resolution CT can be helpful for quantifying emphysema and for the differential diagnosis of bronchiectasis, suspected lung cancer or interstitial lung disease [1, 130]. Pulmonary lung function can further be evaluated by measuring the lung volumes in a plethysmograph and by measuring the diffusion capacity of the lungs for carbon monoxide (DLCO). DLCO may be helpful to differentiate between asthma (usually normal or increased DLCO) and mild COPD (impaired DLCO due to emphysema) but is not a routine examination [1, 132, 133].
Differential diagnoses of exacerbations
As the symptoms during an exacerbation are not specific to COPD worsening, relevant differential diagnoses should be considered e.g. pneumonia, pneumothorax, pulmonary embolism, cardiac arrhythmias or heart failure (Table 3) [134, 135]. Patients with COPD experiencing pneumonia typically present with very similar symptoms as patients experiencing an COPD exacerbation associated with infection [1]; however, while treatment is generally similar, the duration of antibiotic treatment for pneumonia can be longer in practice [136].
Common comorbidities
COPD often co-exists with other diseases that may have a significant impact on prognosis [17, 18, 137, 138]. Indeed, it has been suggested that almost all patients have ≥1 comorbidity, with half having ≥4 [139, 140]. Some comorbidities arise independently of COPD, whereas others are causally related, either with shared risk factors (e.g. age, smoking, systemic inflammation) or by one disease increasing the risk severity of the other [18, 141]. Common comorbidities include bronchiectasis, CVD, chronic kidney disease, dyslipidaemia, diabetes, hypertension, lung cancer, mental disorders, osteoporosis, obstructive sleep apnoea syndrome and skeletal muscle dysfunction [17, 18, 137]. Ellingsen et al. found that the strongest predictor of death in patients with COPD was comorbid heart failure, which was associated with a nearly doubled mortality risk [142]. Stroke and myocardial infarction were also associated with an approximately 50% increased risk of death. An observational retrospective registry study of > 21,000 patients with diagnosed COPD found that the frequency of comorbidities increased during 8 years of observation (Table 4) [8].
Due to the significant impact of comorbidities on prognosis and the rising incidence with time and disease progression [8, 141, 143], it is vital that comorbidities are assessed at diagnosis and at every follow-up review (Table 4). In addition, since the psychological impact of COPD (e.g. anxiety and depression) is known to be substantial [144, 145] and is associated with higher mortality [146], it is important that psychological health is assessed at diagnosis.
Treatment of COPD
COPD treatment goals include smoking cessation (or the termination of other exposure), symptom relief (improved physical capacity and reduced dyspnoea) and reduced risk of exacerbations and mortality [1]. The treatment approach for COPD should be based on clinical, functional and/or biological features that can be observed at the individual level, i.e. treat the treatable traits. Management options include pharmacological and non-pharmacological treatments carried out by a multidisciplinary team comprising a physician, specialist nurse and physiotherapist, as well as a counsellor/psychologist, occupational therapist and nutritionist in some cases [1, 147].
Pharmacological treatment of COPD
Most current therapies target the physiological changes and associated symptoms that result from and aim to improve airflow by altering smooth muscle tone (bronchodilators) or suppressing inflammation (corticosteroids, roflumilast), leading to improved HRQL and symptom control, while reducing the risk of exacerbations and mortality [1].
Initial pharmacological treatment is guided by use of the GOLD ABCD assessment tool at the time of diagnosis and depends on the symptom burden measured by CAT or mMRC, exacerbation history, blood eosinophil count and the presence of co-existing asthma (Fig. 4). Bronchodilators form the mainstay of symptomatic COPD therapy. These come in the form of short-acting β2-agonists and long-acting β2-agonists (LABAs) and short-acting muscarinic antagonists and long-acting muscarinic antagonists (LAMAs) [1]. Short-acting bronchodilators have typically been used as rescue medication; however, guidelines now recommend maintenance treatment with long-acting bronchodilators as a more effective means of reducing symptoms with an additional effect of preventing exacerbations [1]. When LAMAs and LABAs are combined, their complementary mechanisms of action provide greater improvements in lung function and greater reductions in symptoms than the respective monotherapies [1, 148].
There is strong evidence to support the use of ICS in combination with a LABA or LABA/LAMA (‘triple therapy’) in patients with a history of ≥2 moderate exacerbations in the previous year, ≥1 hospitalisation for COPD exacerbations, blood eosinophils ≥0.3 × 109 cells/L (≥300 cells/mm3) or a history of/or concomitant asthma [1, 65, 149,150,151]. GOLD also recommends that the use of ICS in combination with a long-acting bronchodilator be considered in patients with one exacerbation during the previous year or when blood eosinophils are 0.1–0.3 × 109 cells/L (100–300 cells/mm3) [1]. Combining an ICS with a LABA or with a LAMA/LABA combination has been shown to reduce exacerbations to a greater extent than bronchodilators alone [149, 151,152,153]. Recent clinical trials in symptomatic patients with COPD and a history of exacerbations, despite maintenance therapy, found that treatment with fixed-dose ICS/LABA/LAMA triple therapy significantly lowered rates of moderate or severe COPD exacerbations, improved lung function, reduced symptoms and improved HRQL versus treatment with LABA/LAMA or ICS/LABA [65, 150, 151].
Triple therapy has also been shown to reduce exacerbations versus LABA/LAMA in symptomatic patients with no exacerbations or only one exacerbation in the previous 12 months (i.e. patients who would be defined as GOLD Group B) [149, 154]. The GOLD recommendations around eosinophil counts are informed by evidence that the treatment effect of ICS is influenced by blood eosinophil levels, with the benefit generally increasing at eosinophil counts > 0.1 × 109 cells/L (100 cells/mm3) [1]. A pooled analysis of three clinical trials showed a 25% risk reduction in exacerbations with the addition of ICS at eosinophil counts of > 0.1 × 109 cells/L, which increased to 50% at eosinophil counts of > 0.34 × 109 cells/L (340 cells/mm3) [152].
The use of oral prophylactic macrolide antibiotics has been shown to reduce the risk of COPD exacerbations [155, 156]. For this reason, the GOLD guidelines suggest macrolide antibiotics as a possible add-on treatment for frequent exacerbators. However, long-term macrolide use remains controversial due to the risk of bacterial resistance and hearing test impairments [1].
Mortality
Mortality is the ultimate outcome in COPD and risk of mortality can be reduced in several ways: smoking cessation, reduced frequency and severity of exacerbations, lung rehabilitation, increased physical activity and pharmacological treatment [1]. Long-term oxygen therapy has also long been known to decrease mortality in patients with persistent hypoxia [157, 158]. In addition to oxygen therapy, non-invasive ventilation has been found to prolong the time to readmission or death and may benefit some patients with COPD [159].
Randomised trials and retrospective cohort analyses have suggested a benefit for survival with ICS-containing therapy in high-risk patients with COPD compared with placebo or non-ICS therapy [160,161,162,163]. Indeed, the TORCH study demonstrated a 17.5% reduction of risk of death with a borderline significance (p = 0.052) in favour of ICS/LABA treatment versus placebo [160].
Treatment with ICS/LABA/LAMA triple therapy has been demonstrated to significantly reduce the rate of moderate-to-severe exacerbations and improve lung function, symptoms and HRQL compared with LABA/LAMA and ICS/LABA treatment [65, 149,150,151]. Thus, triple therapy is currently recommended for patients with insufficient symptom control or exacerbations despite prior treatment with dual therapy treatment [1]. Recently, two large trials of fixed-dose combination treatment with ICS/LABA/LAMA (IMPACT [65] and ETHOS [151]) found that all-cause mortality was reduced in high-risk patients with COPD compared with LABA/LAMA treatment. Moreover, the study by Martinez et al. showed that the risk of death from any cause with triple therapy was 49% lower than that in the LABA/LAMA group [164], with the beneficial effect on mortality attributable to a reduction in cardiovascular death, and the risk reduction in parity with the effects observed in prevention of cardiovascular events observed in coronary heart disease and statin trials [165,166,167,168].
Despite these benefits, the use of ICS has been associated with a slightly increased risk of pneumonia [169] and use of ICS is not recommended for patients with repeated prior pneumonia events, mycobacterial infection or blood eosinophils < 0.1 × 109 cells/L (< 100 cells/mm3) [1]. Of note, withdrawal of ICS in patients with higher eosinophil counts increases the risk of exacerbations from 0.15 × 109 cells/L, being most pronounced at ≥0.3 × 109 cells/L [170], a finding that was not corroborated in another study [171]. In addition, according to the current GOLD guidelines, ICS should not be used in patients assessed as being in GOLD Group A or B, i.e. patients who have not yet experienced an exacerbation, unless the patient has asthma as a comorbidity [1].
Current guideline recommendations propose a reactive, stepwise approach for escalating pharmacological treatment of COPD, where a patient must have suffered ≥2 moderate exacerbations or one hospitalisation in the previous year, despite appropriate bronchodilator treatment [1]. This raises the question ‘why?’, since this approach is not applied in other chronic conditions, such as CVD [172]. Physicians must be vigilant in their work and be more ambitious in employing rigorous risk assessment to prevent even the first severe exacerbation leading to hospitalisation since those are associated with increased risk of mortality (Table 2). Indeed, one in five patients with COPD die within 1 year of their first-ever severe exacerbation leading to hospitalisation [86], while half die within 3.6 years of their first-ever severe exacerbation [82].
Non-pharmacological treatment of COPD
The risk of exacerbations has been shown to decrease by 22% in ex-smokers compared with current smokers [173], thus smoking cessation is the most important initial step in treatment; advice regarding smoking cessation should be combined with nicotine and non-nicotine replacement therapy to increase long-term smoking abstinence [1, 174]. Pulmonary rehabilitation, including physical activity and self-management education, relieves symptoms and improves HRQL [1, 175]. In addition, vaccinations are also very important: influenza vaccination is recommended for all COPD patients, as it reduces serious illness and death, and pneumococcal vaccination is recommended for patients aged ≥65 years, as it reduces the risk of pneumonia [1]. In malnourished patients with COPD, nutritional support is recommended as it may improve respiratory muscle strength and HRQL.
Reduced physical activity in patients with COPD has been independently linked with reduced HRQL [176], increased hospitalisations [177], physical deconditioning [27, 178] and mortality [179]. Thus, improvement in physical activity and behavioural intervention provides better long-term outcomes for patients with COPD [35, 180, 181].
Finally, long-term oxygen therapy (> 15 h per day) has been shown to improve survival in patients with severe resting hypoxemia [182], but has not been found to be beneficial for patients with stable COPD and moderate resting or exercise-induced arterial desaturation [183].
Patient education
In terms of education, it is paramount to explain to patients in plain, understandable language about their diagnosis and prognosis, and to encourage them to be an active participant in their self-management and treatment programme [1]. This will also involve training on how to use their inhaler effectively, as poor technique is a leading cause of poor response to treatment [184, 185]. In addition, patient education should be a shared duty of healthcare systems and wider society, including schools and workplaces. Community engagement alongside health promotion regulations, such as no smoking laws and anti-smoking campaigns, can contribute to disease prevention.
Follow-up visits to monitor COPD – why and how?
COPD is a complex, progressive disease, therefore routine, individualised monitoring/assessment at follow-up is essential. International and national guidelines suggest annual follow-up visits for stable, non-exacerbating patients at least once per year and a follow-up visit 1–4 weeks after an acute exacerbation for a thorough, overall medical assessment that includes spirometric measurements, documentation of symptom burden and optimisation of COPD medication [1, 186]. Ideally, patients with very severe COPD should be reviewed at least twice a year and multimorbid patients should see their physician at least once a year [186, 187]. The key issue for all members of the multidisciplinary team responsible for monitoring/follow-up is to plan for the next visit based on the patient’s individual needs.
Recent GOLD guidelines have included a pharmacological follow-up algorithm that can be applied to any patient who is already taking maintenance treatment(s) irrespective of the GOLD group allocated at treatment initiation (Fig. 5) [1]. At follow-up/annual review, the first priority is to identify whether the initial treatment was successful in helping the patients meet their treatment goals, whether disease progression has occurred and what the predominant symptom is (dyspnoea, exacerbations or both). If dyspnoea dominates, treatment should be stepped up to dual bronchodilator therapy or triple therapy depending on the patients’ current pharmacological maintenance treatment (Fig. 5a). If exacerbations dominate (or both dyspnoea and exacerbations), the alternative algorithm should be followed (Fig. 5b). In addition, patient handling of the inhaler and inhalation technique must be reviewed both annually and before stepping up medication [184, 185, 188]. Recommendations for the annual review are shown in Table 5.
Treatment algorithm for patients with a) dyspnoea or b) exacerbations at review. aConsider if EOS ≥0.3 × 109 cells/L (≥300 cells/mm3) or EOS ≥0.1 × 109 cells/L (≥100 cells/mm3) AND ≥ 2 moderate exacerbations/1 hospitalisation. bConsider de-escalation of ICS or switch in response to pneumonia, inappropriate original indication or lack of response to ICS. Reproduced with permission from: Global Initiative for Chronic Obstructive Lung Disease 2021 Report; Figure 4.4. Available from https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.0-16Nov20_WMV.pdf, accessed 18 November 2020. EOS eosinophil count, FEV1 forced expiratory volume in 1 s, ICS inhaled corticosteroid, LABA long-acting β2-agonist, LAMA long-acting muscarinic antagonist
Personnel
In many countries, specialist nurses play an important role in the management of COPD alongside physicians [189]. Nurse-led COPD clinics in primary care have been shown to reduce exacerbations, hospitalisations and costs [190]. Their role within the COPD disease management team may vary between countries; however, specialist nurses are invaluable in performing spirometry and providing education and advice to improve medication adherence and self-management. Often nurses are also responsible for performing annual patient reviews, thereby relieving the physician’s work burden, but nurses may not be able to easily detect COPD deterioration, distinguish symptoms from other serious comorbidities or adequately control other comorbidities.
Physicians therefore have an overall responsibility for the patient, as well as a more holistic overview of their health conditions. The physician is also responsible for initiating the multidisciplinary team contacts, as pulmonary rehabilitation is an essential part of moderate-to-severe COPD management and should thus be offered to these patients. The point of escalation from primary care to secondary care, such as hospitalisation, varies between countries and healthcare systems. In general, physicians should refer the patient to secondary care if the patient has severe disease at a young age, or is experiencing distressing breathlessness, fatigue, depression and/or anxiety, chronic hypoxia or a rapid decline in lung function [191]. Importantly, regardless of whether the patient is in primary or secondary care, a timely individualised care plan should be made when disease deterioration has reached the level of requiring palliative care.
Conclusions
COPD is a serious public health burden that is characterised by underdiagnosis, progressive deterioration and treatment difficulties, which all lead to significant disease burden and increased mortality among patients. Correct diagnostic methods are crucial to reduce both under- and overdiagnosis. Besides smoking cessation, physical activity and pulmonary rehabilitation, individualised pharmacological treatment based on symptom burden, exacerbation risk and inflammatory features, such as blood eosinophil count, is central for a favourable prognosis and reduced risk of mortality. Most patients with COPD are fully managed in primary care, presenting unique opportunities to provide patients with evidence-based treatments and individualised care plans. While progress in the correct use of COPD guidelines has been observed recently [8], there is scope for further improvement, particularly in detection rates, disease monitoring/treatment and structured follow-ups [8, 10].
Primary care practitioners need to become aware of the huge impact of COPD (especially in multimorbid patients), have a local support system (e.g. routines, flow charts and nurse-led COPD clinics at the primary healthcare centre), have non-judgemental views of smoking and of COPD as a chronic disease, use a holistic consultation approach and actively motivate the patient to adhere to treatment. Together, these factors could help optimise outcomes for patients with COPD seen in primary care settings.
Availability of data and materials
Not applicable.
Abbreviations
- CAT:
-
COPD assessment test
- COPD:
-
Chronic obstructive pulmonary disease
- CVD:
-
Cardiovascular disease
- EOS:
-
Eosinophil count
- FEV1 :
-
Forced expiratory volume in 1 second
- FVC:
-
Forced vital capacity
- GERD:
-
Gastro-oesophageal reflux disease
- GOLD:
-
Global Initiative for Chronic Obstructive Lung Disease
- HRQL:
-
Health-related quality of life
- ICS:
-
Inhaled corticosteroids
- LABA:
-
Long-acting β2-agonist
- LAMA:
-
Long-acting muscarinic antagonist
- mMRC:
-
Modified Medical Research Council dyspnoea scale
- NT-proBNP:
-
N-terminal pro B-type natriuretic peptide
References
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2021 report. 2021. https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.1-25Nov20_WMV.pdf. Accessed 5 Apr 2021.
Diab N, Gershon AS, Sin DD, Tan WC, Bourbeau J, Boulet LP, et al. Underdiagnosis and overdiagnosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;198(9):1130–9.
World Health Organization. The top 10 causes of death. 2018. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. Accessed 22 July 2020.
Guarascio AJ, Ray SM, Finch CK, Self TH. The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinicoecon Outcomes Res. 2013;5:235–45.
European Respiratory Society. European lung white book. 2013. https://www.erswhitebook.org/. Accessed 2 May 2018.
Löfdahl CG, Tilling B, Ekström T, Jörgensen L, Johansson G, Larsson K. COPD health care in Sweden - a study in primary and secondary care. Respir Med. 2010;104(3):404–11.
Perez X, Wisnivesky JP, Lurslurchachai L, Kleinman LC, Kronish IM. Barriers to adherence to COPD guidelines among primary care providers. Respir Med. 2012;106(3):374–81.
Ställberg B, Janson C, Johansson G, Larsson K, Stratelis G, Telg G, et al. Management, morbidity and mortality of COPD during an 11-year period: an observational retrospective epidemiological register study in Sweden (PATHOS). Prim Care Respir J. 2014;23(1):38–45.
Roche N, Lepage T, Bourcereau J, Terrioux P. Guidelines versus clinical practice in the treatment of chronic obstructive pulmonary disease. Eur Respir J. 2001;18(6):903–8.
Arne M, Emtner M, Lisspers K, Wadell K, Ställberg B. Availability of pulmonary rehabilitation in primary care for patients with COPD: a cross-sectional study in Sweden. Eur Clin Respir J. 2016;3:31601.
Jones RCM, Price D, Ryan D, Sims EJ, von Ziegenweidt J, Mascarenhas L, et al. Opportunities to diagnose chronic obstructive pulmonary disease in routine care in the UK: a retrospective study of a clinical cohort. Lancet Respir Med. 2014;2(4):267–76.
Rothnie KJ, Chandan JS, Goss HG, Mullerova H, Quint JK. Validity and interpretation of spirometric recordings to diagnose COPD in UK primary care. Int J Chron Obstruct Pulmon Dis. 2017;12:1663–8.
Heffler E, Crimi C, Mancuso S, Campisi R, Puggioni F, Brussino L, et al. Misdiagnosis of asthma and COPD and underuse of spirometry in primary care unselected patients. Respir Med. 2018;142:48–52.
Ragaišienė G, Kibarskyte R, Gauronskaite R, Giedraityte M, Dapsauskaite A, Kasiulevicius V, et al. Diagnosing COPD in primary care: what has real life practice got to do with guidelines? Multidiscip Respir Med. 2019;14:28.
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2095–128.
James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1789–858.
Ställberg B, Janson C, Larsson K, Johansson G, Kostikas K, Gruenberger JB, et al. Real-world retrospective cohort study ARCTIC shows burden of comorbidities in Swedish COPD versus non-COPD patients. NPJ Prim Care Respir Med. 2018;28(1):33.
Hillas G, Perlikos F, Tsiligianni I, Tzanakis N. Managing comorbidities in COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:95–109.
van der Molen T, Miravitlles M, Kocks JWH. COPD management: role of symptom assessment in routine clinical practice. Int J Chron Obstruct Pulmon Dis. 2013;8:461–71.
Yawn BP, Wollan P, Rank M. Exacerbations in the pre- and post-COPD diagnosis periods. Pragmat Obs Res. 2013;4:1–6.
Jones PW. Health status measurement in chronic obstructive pulmonary disease. Thorax. 2001;56(11):880–7.
Weiss ST, DeMeo DL, Postma DS. COPD: problems in diagnosis and measurement. Eur Respir J Suppl. 2003;21:4s–12s.
Guerra S, Sherrill DL, Venker C, Ceccato CM, Halonen M, Martinez FD. Chronic bronchitis before age 50 years predicts incident airflow limitation and mortality risk. Thorax. 2009;64(10):894–900.
Mapel DW, Dalal AA, Blanchette CM, Petersen H, Ferguson GT. Severity of COPD at initial spirometry-confirmed diagnosis: data from medical charts and administrative claims. Int J Chron Obstruct Pulmon Dis. 2011;6:573–81.
Sandelowsky H, Ställberg B, Nager A, Hasselström J. The prevalence of undiagnosed chronic obstructive pulmonary disease in a primary care population with respiratory tract infections - a case finding study. BMC Fam Pract. 2011;12:122.
Kim V, Criner GJ. Chronic bronchitis and chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187(3):228–37.
Shrikrishna D, Patel M, Tanner RJ, Seymour JM, Connolly BA, Puthucheary ZA, et al. Quadriceps wasting and physical inactivity in patients with COPD. Eur Respir J. 2012;40(5):1115–22.
Watz H, Waschki B, Meyer T, Magnussen H. Physical activity in patients with COPD. Eur Respir J. 2009;33(2):262–72.
Kaplan A, Thomas M. Screening for COPD: the gap between logic and evidence. Eur Respir Rev. 2017;26(143):160113.
van den Boom G, Rutten-van Mölken MP, Tirimanna PR, van Schayck CP, Folgering H, van Weel C. Association between health-related quality of life and consultation for respiratory symptoms: results from the DIMCA programme. Eur Respir J. 1998;11(1):67–72.
Ofir D, Laveneziana P, Webb KA, Lam YM, O’Donnell DE. Mechanisms of dyspnea during cycle exercise in symptomatic patients with GOLD stage I chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2008;177(6):622–9.
Al Talag A, Wilcox P. Clinical physiology of chronic obstructive pulmonary disease. BCMJ. 2008;50(2):97–102.
O'Donnell DE, Laveneziana P. Dyspnea and activity limitation in COPD: mechanical factors. COPD. 2007;4(3):225–36.
O'Donnell DE. Hyperinflation, dyspnea, and exercise intolerance in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2006;3(2):180–4.
Watz H, Pitta F, Rochester CL, Garcia-Aymerich J, ZuWallack R, Troosters T, et al. An official European Respiratory Society statement on physical activity in COPD. Eur Respir J. 2014;44(6):1521–37.
Okajima Y, Come CE, Nardelli P, Sonavane SK, Yen A, Nath HP, et al. Luminal plugging on chest CT scan: association with lung function, quality of life, and COPD clinical phenotypes. Chest. 2020;158(1):121–30.
Hogg JC, Chu F, Utokaparch S, Woods R, Elliott WM, Buzatu L, et al. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(26):2645–53.
Nishimura K, Izumi T, Tsukino M, Oga T. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest. 2002;121(5):1434–40.
Sundh J, Janson C, Lisspers K, Ställberg B, Montgomery S. The dyspnoea, obstruction, smoking, exacerbation (DOSE) index is predictive of mortality in COPD. Prim Care Respir J. 2012;21(3):295–301.
Casanova C, Cote C, de Torres JP, Aguirre-Jaime A, Marin JM, Pinto-Plata V, et al. Inspiratory-to-total lung capacity ratio predicts mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;171(6):591–7.
Barnes PJ. Inflammatory mechanisms in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2016;138(1):16–27.
Baraldo S, Turato G, Saetta M. Pathophysiology of the small airways in chronic obstructive pulmonary disease. Respiration. 2012;84(2):89–97.
Rossi A, Aisanov Z, Avdeev S, Di Maria G, Donner CF, Izquierdo JL, et al. Mechanisms, assessment and therapeutic implications of lung hyperinflation in COPD. Respir Med. 2015;109(7):785–802.
Kim SH, Shin MJ, Shin YB, Kim KU. Sarcopenia associated with chronic obstructive pulmonary disease. J Bone Metab. 2019;26(2):65–74.
Kupper N, Bonhof C, Westerhuis B, Widdershoven J, Denollet J. Determinants of dyspnea in chronic heart failure. J Card Fail. 2016;22(3):201–9.
Jenkins CR, Celli B, Anderson JA, Ferguson GT, Jones PW, Vestbo J, et al. Seasonality and determinants of moderate and severe COPD exacerbations in the TORCH study. Eur Respir J. 2012;39(1):38–45.
Partridge MR, Karlsson N, Small IR. Patient insight into the impact of chronic obstructive pulmonary disease in the morning: an internet survey. Curr Med Res Opin. 2009;25(8):2043–8.
Braghiroli A, Braido F, Piraino A, Rogliani P, Santus P, Scichilone N. Day and night control of COPD and role of pharmacotherapy: a review. Int J Chron Obstruct Pulmon Dis. 2020;15:1269–85.
van Buul AR, Kasteleyn MJ, Chavannes NH, Taube C. Association between morning symptoms and physical activity in COPD: a systematic review. Eur Respir Rev. 2017;26(143):160033.
Singh D, Miravitlles M, Vogelmeier C. Chronic obstructive pulmonary disease individualized therapy: tailored approach to symptom management. Adv Ther. 2017;34(2):281–99.
Fletcher C, Peto R. The natural history of chronic airflow obstruction. Br Med J. 1977;1(6077):1645–8.
Vestbo J, Edwards LD, Scanlon PD, Yates JC, Agusti A, Bakke P, et al. Changes in forced expiratory volume in 1 second over time in COPD. N Engl J Med. 2011;365(13):1184–92.
Wang M, Aaron CP, Madrigano J, Hoffman EA, Angelini E, Yang J, et al. Association between long-term exposure to ambient air pollution and change in quantitatively assessed emphysema and lung function. JAMA. 2019;322(6):546–56.
Balcan B, Akan S, Ugurlu AO, Handemir BO, Ceyhan BB, Ozkaya S. Effects of biomass smoke on pulmonary functions: a case control study. Int J Chron Obstruct Pulmon Dis. 2016;11:1615–22.
Po JYT, FitzGerald JM, Carlsten C. Respiratory disease associated with solid biomass fuel exposure in rural women and children: systematic review and meta-analysis. Thorax. 2011;66(3):232–9.
Bergdahl IA, Torén K, Eriksson K, Hedlund U, Nilsson T, Flodin R, et al. Increased mortality in COPD among construction workers exposed to inorganic dust. Eur Respir J. 2004;23(3):402–6.
Humerfelt S, Gulsvik A, Skjærven R, Nilssen S, Kvåle G, Sulheim O, et al. Decline in FEV1 and airflow limitation related to occupational exposures in men of an urban community. Eur Respir J. 1993;6(8):1095–103.
Burney P, Jithoo A, Kato B, Janson C, Mannino D, Niżankowska-Mogilnicka E, et al. Chronic obstructive pulmonary disease mortality and prevalence: the associations with smoking and poverty—a BOLD analysis. Thorax. 2014;69(5):465–73.
Cosio Piqueras MG, Cosio MG. Disease of the airways in chronic obstructive pulmonary disease. Eur Respir J. 2001;34(34 suppl):41s–9s.
Barnes PJ. Immunology of asthma and chronic obstructive pulmonary disease. Nat Rev Immunol. 2008;8(3):183–92.
Tashkin DP, Wechsler ME. Role of eosinophils in airway inflammation of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2018;13:335–49.
Weitzenblum E, Chaouat A. Cor pulmonale. Chron Respir Dis. 2009;6(3):177–85.
Martinez-Garcia MA, Miravitlles M. Bronchiectasis in COPD patients: more than a comorbidity? Int J Chron Obstruct Pulmon Dis. 2017;12:1401–11.
Seemungal TAR, Donaldson GC, Bhowmik A, Jeffries DJ, Wedzicha JA. Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000;161(5):1608–13.
Lipson DA, Barnhart F, Brealey N, Brooks J, Criner GJ, Day NC, et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med. 2018;378(18):1671–80.
Swedish Medical Products Agency. Kroniskt obstruktiv lungsjukdom (KOL) – behandlingsrekommendation. 2015. https://www.lakemedelsverket.se/48d8f2/globalassets/dokument/behandling-och-forskrivning/behandlingsrekommendationer/behandlingsrekommendation/behandlingsrekommendation-kroniskt-obstruktiv-lungsjukdom-kol.pdf. Accessed 7 Sept 2020.
Burge S, Wedzicha JA. COPD exacerbations: definitions and classifications. Eur Respir J. 2003;21(41):46s–53s.
Wedzicha JA, Seemungal TAR. COPD exacerbations: defining their cause and prevention. Lancet. 2007;370(9589):786–96.
Hillas G, Perlikos F, Tzanakis N. Acute exacerbation of COPD: is it the “stroke of the lungs”? Int J Chron Obstruct Pulmon Dis. 2016;11:1579–86.
Singh D, D'Urzo AD, Donohue JF, Kerwin EM. Weighing the evidence for pharmacological treatment interventions in mild COPD; a narrative perspective. Respir Res. 2019;20(1):141.
Hurst JR, Vestbo J, Anzueto A, Locantore N, Müllerova H, Tal-Singer R, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128–38.
Donaldson GC, Seemungal TAR, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002;57(10):847–52.
Halpin DMG, Decramer M, Celli BR, Mueller A, Metzdorf N, Tashkin DP. Effect of a single exacerbation on decline in lung function in COPD. Respir Med. 2017;128:85–91.
Watz H, Tetzlaff K, Magnussen H, Mueller A, Rodriguez-Roisin R, Wouters EFM, et al. Spirometric changes during exacerbations of COPD: a post hoc analysis of the WISDOM trial. Respir Res. 2018;19(1):251.
Roche N, Wedzicha JA, Patalano F, Frent SM, Larbig M, Shen S, et al. COPD exacerbations significantly impact quality of life as measured by SGRQ-C total score: results from the FLAME study. Eur Respir J. 2017;50:OA1487.
Seemungal TAR, Donaldson GC, Paul EA, Bestall JC, Jeffries DJ, Wedzicha JA. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157(5 Pt 1):1418–22.
Halpin DMG, Decramer M, Celli B, Kesten S, Liu D, Tashkin DP. Exacerbation frequency and course of COPD. Int J Chron Obstruct Pulmon Dis. 2012;7:653–61.
Donaldson GC, Hurst JR, Smith CJ, Hubbard RB, Wedzicha JA. Increased risk of myocardial infarction and stroke following exacerbation of COPD. Chest. 2010;137(5):1091–7.
Halpin DMG, Decramer M, Celli B, Kesten S, Leimer I, Tashkin DP. Risk of nonlower respiratory serious adverse events following COPD exacerbations in the 4-year UPLIFT® trial. Lung. 2011;189(4):261–8.
Rothnie KJ, Yan R, Smeeth L, Quint JK. Risk of myocardial infarction (MI) and death following MI in people with chronic obstructive pulmonary disease (COPD): a systematic review and meta-analysis. BMJ Open. 2015;5(9):e007824.
Rothnie KJ, Connell O, Müllerová H, Smeeth L, Pearce N, Douglas I, et al. Myocardial infarction and ischemic stroke after exacerbations of chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2018;15(8):935–46.
Suissa S, Dell'Aniello S, Ernst P. Long-term natural history of chronic obstructive pulmonary disease: severe exacerbations and mortality. Thorax. 2012;67(11):957–63.
Rodriguez-Roisin R. Toward a consensus definition for COPD exacerbations. Chest. 2000;117(5 Suppl. 2):398S–401S.
Rothnie KJ, Müllerová H, Smeeth L, Quint JK. Natural history of chronic obstructive pulmonary disease exacerbations in a general practice-based population with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;198(4):464–71.
Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60(11):925–31.
Ho T-W, Tsai YJ, Ruan SY, Huang CT, Lai F, Yu CJ, et al. In-hospital and one-year mortality and their predictors in patients hospitalized for first-ever chronic obstructive pulmonary disease exacerbations: a nationwide population-based study. PLoS One. 2014;9(12):e114866.
Lindenauer PK, Dharmarajan K, Qin L, Lin Z, Gershon AS, Krumholz HM. Risk trajectories of readmission and death in the first year after hospitalization for chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;197(8):1009–17.
Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10(4):407–15.
Spencer S, Jones PW, Globe Study Group. Time course of recovery of health status following an infective exacerbation of chronic bronchitis. Thorax. 2003;58(7):589–93.
Cao Y-Q, Dong L-X, Cao J. Pulmonary embolism in patients with acute exacerbation of chronic obstructive pulmonary disease. Chin Med J. 2018;131(14):1732–7.
Wang M, Lin EP, Huang LC, Li CY, Shyr Y, Lai CH. Mortality of cardiovascular events in patients with COPD and preceding hospitalization for acute exacerbation. Chest. 2020;158(3):973–85.
Kunisaki KM, Dransfield MT, Anderson JA, Brook RD, Calverley PMA, Celli BR, et al. Exacerbations of chronic obstructive pulmonary disease and cardiac events. A post hoc cohort analysis from the SUMMIT randomized clinical trial. Am J Respir Crit Care Med. 2018;198(1):51–7.
Connors AF Jr, Dawson NV, Thomas C, Harrell FE, Desbiens N, Fulkerson WJ, et al. Outcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (study to understand prognoses and preferences for outcomes and risks of treatments). Am J Respir Crit Care Med. 1996;154(4 Pt 1):959–67.
Sethi S. Infectious etiology of acute exacerbations of chronic bronchitis. Chest. 2000;117(5 Suppl. 2):380s–5s.
Wilkinson TMA, Hurst JR, Perera WR, Wilks M, Donaldson GC, Wedzicha JA. Effect of interactions between lower airway bacterial and rhinoviral infection in exacerbations of COPD. Chest. 2006;129(2):317–24.
Barnes N, Calverley PMA, Kaplan A, Rabe KF. Chronic obstructive pulmonary disease and exacerbations: patient insights from the global hidden depths of COPD survey. BMC Pulm Med. 2013;13:54.
Janson C, Nwaru BI, Wiklund F, Telg G, Ekström M. Management and risk of mortality in patients hospitalised due to a first severe COPD exacerbation. Int J Chron Obstruct Pulmon Dis. 2020;15:2673–82.
Wilkinson TMA, Donaldson GC, Hurst JR, Seemungal TA, Wedzicha JA. Early therapy improves outcomes of exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2004;169(12):1298–303.
Langsetmo L, Platt RW, Ernst P, Bourbeau J. Underreporting exacerbation of chronic obstructive pulmonary disease in a longitudinal cohort. Am J Respir Crit Care Med. 2008;177(4):396–401.
Xu W, Collet J-P, Shapiro S, Lin Y, Yang T, Wang C, et al. Negative impacts of unreported COPD exacerbations on health-related quality of life at 1 year. Eur Respir J. 2010;35(5):1022–30.
Sandelowsky H, Krakau I, Modin S, Ställberg B, Nager A. COPD patients need more information about self-management: a cross-sectional study in Swedish primary care. Scand J Prim Health Care. 2019;37(4):459–67.
Guerra B, Gaveikaite V, Bianchi C, Puhan MA. Prediction models for exacerbations in patients with COPD. Eur Respir Rev. 2017;26(143):160061.
Hoogendoorn M, Feenstra TL, Boland M, Briggs AH, Borg S, Jansson S-A, et al. Prediction models for exacerbations in different COPD patient populations: comparing results of five large data sources. Int J Chron Obstruct Pulmon Dis. 2017;12:3183–94.
Rassouli F, Baty F, Stolz D, Albrich WC, Tamm M, Widmer S, et al. Longitudinal change of COPD assessment test (CAT) in a telehealthcare cohort is associated with exacerbation risk. Int J Chron Obstruct Pulmon Dis. 2017;12:3103–9.
Kim V, Han MK, Vance GB, Make BJ, Newell JD, Hokanson JE, et al. The chronic bronchitic phenotype of COPD: an analysis of the COPDGene study. Chest. 2011;140(3):626–33.
Pavord ID, Jones PW, Burgel P-R, Rabe KF. Exacerbations of COPD. Int J Chron Obstruct Pulmon Dis. 2016;11(Spec. Iss):21–30.
Vedel-Krogh S, Nielsen SF, Lange P, Vestbo J, Nordestgaard BG. Blood eosinophils and exacerbations in chronic obstructive pulmonary disease. The Copenhagen General Population Study. Am J Respir Crit Care Med. 2016;193(9):965–74.
Couillard S, Larivée P, Courteau J, Vanasse A. Eosinophils in COPD exacerbations are associated with increased readmissions. Chest. 2017;151(2):366–73.
Swanney MP, Ruppel G, Enright PL, Pedersen OF, Crapo RO, Miller MR, et al. Using the lower limit of normal for the FEV1/FVC ratio reduces the misclassification of airway obstruction. Thorax. 2008;63(12):1046–51.
Richter DC, Joubert JR, Nell H, Schuurmans MM, Irusen EM. Diagnostic value of post-bronchodilator pulmonary function testing to distinguish between stable, moderate to severe COPD and asthma. Int J Chron Obstruct Pulmon Dis. 2008;3(4):693–9.
Hardie JA, Buist AS, Vollmer WM, Ellingsen I, Bakke PS, Mørkve O. Risk of over-diagnosis of COPD in asymptomatic elderly never-smokers. Eur Respir J. 2002;20(5):1117–22.
Abramson MJ, Schattner RL, Sulaiman ND, Del Colle EA, Aroni R, Thien F. Accuracy of asthma and COPD diagnosis in Australian general practice: a mixed methods study. Prim Care Respir J. 2012;21(2):167–73.
Eaton T, Withy S, Garrett JE, Mercer J, Whitlock RM, Rea HH. Spirometry in primary care practice: the importance of quality assurance and the impact of spirometry workshops. Chest. 1999;116(2):416–23.
Hangaard S, Helle T, Nielsen C, Hejlesen OK. Causes of misdiagnosis of chronic obstructive pulmonary disease: a systematic scoping review. Respir Med. 2017;129:63–84.
Dorinsky PM, Reisner C, Ferguson GT, Menjoge SS, Serby CW, Witek TJ Jr. The combination of ipratropium and albuterol optimizes pulmonary function reversibility testing in patients with COPD. Chest. 1999;115(4):966–71.
Tashkin DP, Celli B, Decramer M, Liu D, Burkhart D, Cassino C, et al. Bronchodilator responsiveness in patients with COPD. Eur Respir J. 2008;31(4):742–50.
Donohue JF. Therapeutic responses in asthma and COPD. Bronchodilators. Chest. 2004;126(2 Suppl):125S–37S discussion 59S-61S.
Janson C, Malinovschi A, Amaral AFS, Accordini S, Bousquet J, Buist AS, et al. Bronchodilator reversibility in asthma and COPD: findings from three large population studies. Eur Respir J. 2019;54(3):1900561.
Calverley PMA, Burge PS, Spencer S, Anderson JA, Jones PW. Bronchodilator reversibility testing in chronic obstructive pulmonary disease. Thorax. 2003;58(8):659–64.
Kerstjens HAM, Brand PL, Quanjer PH, van der Bruggen-Bogaarts BA, Koëter GH, Postma DS. Variability of bronchodilator response and effects of inhaled corticosteroid treatment in obstructive airways disease. Dutch CNSLD Study Group. Thorax. 1993;48(7):722–9.
Le Rouzic O, Roche N, Cortot AB, Tillie-Leblond I, Masure F, Perez T, et al. Defining the “frequent exacerbator” phenotype in COPD: a hypothesis-free approach. Chest. 2018;153(5):1106–15.
Corlateanu A, Mendez Y, Wang Y, Garnica RJA, Botnaru V, Siafakas N. Chronic obstructive pulmonary disease and phenotypes: a state-of-the-art. Pulmonology. 2020;26(2):95–100.
Sandelowsky H, Hylander I, Krakau I, Modin S, Ställberg B, Nager A. Time pressured deprioritization of COPD in primary care: a qualitative study. Scand J Prim Health Care. 2016;34(1):55–65.
Larsson K, Janson C, Ställberg B, Lisspers K, Olsson P, Kostikas K, et al. Impact of COPD diagnosis timing on clinical and economic outcomes: the ARCTIC observational cohort study. Int J Chron Obstruct Pulmon Dis. 2019;14:995–1008.
Spruit MA, Polkey MI, Celli B, Edwards LD, Watkins ML, Pinto-Plata V, et al. Predicting outcomes from 6-minute walk distance in chronic obstructive pulmonary disease. J Am Med Dir Assoc. 2012;13(3):291–7.
Moy ML, Gould MK, Liu I-LA, Lee JS, Nguyen HQ. Physical activity assessed in routine care predicts mortality after a COPD hospitalisation. ERJ Open Res. 2016;2(1):00062–2015.
Yawn BP. Differential assessment and management of asthma vs chronic obstructive pulmonary disease. Medscape J Med. 2009;11(1):20.
Chilosi M, Poletti V, Rossi A. The pathogenesis of COPD and IPF: distinct horns of the same devil? Respir Res. 2012;13:3.
de Miguel Díez J, Chancafe Morgan J, Jiménez García R. The association between COPD and heart failure risk: a review. Int J Chron Obstruct Pulmon Dis. 2013;8:305–12.
Dou S, Zheng C, Ji X, Wang W, Xie M, Cui L, et al. Co-existence of COPD and bronchiectasis: a risk factor for a high ratio of main pulmonary artery to aorta diameter (PA:A) from computed tomography in COPD patients. Int J Chron Obstruct Pulmon Dis. 2018;13:675–81.
Cote C, Zilberberg MD, Mody SH, Dordelly LJ, Celli B. Haemoglobin level and its clinical impact in a cohort of patients with COPD. Eur Respir J. 2007;29(5):923–9.
Criner RN, Hatt CR, Galban CJ, Kazerooni EA, Lynch DA, McCormack MC, et al. Relationship between diffusion capacity and small airway abnormality in COPDGene. Respir Res. 2019;20(1):269.
McCormack MC, Enright PL. Making the diagnosis of asthma. Respir Care. 2008;53(5):583–90.
Kim V, Aaron SD. What is a COPD exacerbation? Current definitions, pitfalls, challenges and opportunities for improvement. Eur Respir J. 2018;52(5):1801261.
Falk JA, Kadiev S, Criner GJ, Scharf SM, Minai OA, Diaz P. Cardiac disease in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2008;5(4):543–8.
Berild AG, Erichsen D, Berild D. Treatment of community-acquired pneumonia. Tidsskr Nor Laegeforen. 2018;138(19) English, Norwegian. https://doi.org/10.4045/tidsskr.17.1115.
Divo M, Cote C, de Torres JP, Casanova C, Marin JM, Pinto-Plata V, et al. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186(2):155–61.
Sin DD, Anthonisen NR, Soriano JB, Agusti AG. Mortality in COPD: role of comorbidities. Eur Respir J. 2006;28(6):1245–57.
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43.
Vanfleteren LEGW, Spruit MA, Groenen M, Gaffron S, van Empel VP, Bruijnzeel PL, et al. Clusters of comorbidities based on validated objective measurements and systemic inflammation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187(7):728–35.
Fabbri LM, Luppi F, Beghé B, Rabe KF. Complex chronic comorbidities of COPD. Eur Respir J. 2008;31(1):204–12.
Ellingsen J, Johansson G, Larsson K, Lisspers K, Malinovschi A, Ställberg B, et al. Impact of comorbidities and commonly used drugs on mortality in COPD - real-world data from a primary care setting. Int J Chron Obstruct Pulmon Dis. 2020;15:235–45.
Lee AL, Goldstein RS. Gastroesophageal reflux disease in COPD: links and risks. Int J Chron Obstruct Pulmon Dis. 2015;10:1935–49.
Yohannes AM, Willgoss TG, Baldwin RC, Connolly MJ. Depression and anxiety in chronic heart failure and chronic obstructive pulmonary disease: prevalence, relevance, clinical implications and management principles. Int J Geriatr Psychiatry. 2010;25(12):1209–21.
Marsh S, Guck TP. Anxiety and depression: easing the burden in COPD patients. J Fam Pract. 2016;65(4):246–56.
Sikjær MG, Løkke A, Hilberg O. The influence of psychiatric disorders on the course of lung cancer, chronic obstructive pulmonary disease and tuberculosis. Respir Med. 2018;135:35–41.
Sundh J, Lindgren H, Hasselgren M, Montgomery S, Janson C, Ställberg B, et al. Pulmonary rehabilitation in COPD – available resources and utilization in Swedish primary and secondary care. Int J Chron Obstruct Pulmon Dis. 2017;12:1695–704.
Rogliani P, Calzetta L, Braido F, Cazzola M, Clini E, Pelaia G, et al. LABA/LAMA fixed-dose combinations in patients with COPD: a systematic review. Int J Chron Obstruct Pulmon Dis. 2018;13:3115–30.
Ferguson GT, Rabe KF, Martinez FJ, Fabbri LM, Wang C, Ichinose M, et al. Triple therapy with budesonide/glycopyrrolate/formoterol fumarate with co-suspension delivery technology versus dual therapies in chronic obstructive pulmonary disease (KRONOS): a double-blind, parallel-group, multicentre, phase 3 randomised controlled trial. Lancet Respir Med. 2018;6(10):747–58.
Papi A, Vestbo J, Fabbri L, Corradi M, Prunier H, Cohuet G, et al. Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): a double-blind, parallel group, randomised controlled trial. Lancet. 2018;391(10125):1076–84.
Rabe KF, Martinez FJ, Ferguson GT, Wang C, Singh D, Wedzicha JA, et al. Triple inhaled therapy at two glucocorticoid doses in moderate-to-very-severe COPD. N Engl J Med. 2020;383(1):35–48.
Bafadhel M, Peterson S, De Blas MA, Calverley PM, Rennard SI, Richter K, et al. Predictors of exacerbation risk and response to budesonide in patients with chronic obstructive pulmonary disease: a post-hoc analysis of three randomised trials. Lancet Respir Med. 2018;6(2):117–26.
Pascoe S, Barnes N, Brusselle G, Compton C, Criner GJ, Dransfield MT, et al. Blood eosinophils and treatment response with triple and dual combination therapy in chronic obstructive pulmonary disease: analysis of the IMPACT trial. Lancet Respir Med. 2019;7(9):745–56.
Martinez FJ, Ferguson GT, Bourne E, Ballal S, Darken P, Aurivillius M, et al. Budesonide/glycopyrrolate/formoterol fumarate metered dose inhaler improves exacerbation outcomes in patients with COPD without a recent exacerbation history: a subgroup analysis of KRONOS. Int J Chron Obstruct Pulmon Dis. 2021;16:179–89.
Herath SC, Normansell R, Maisey S, Poole P. Prophylactic antibiotic therapy for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. 2018;(10):CD009764.
Ni W, Shao X, Cai X, Wei C, Cui J, Wang R, et al. Prophylactic use of macrolide antibiotics for the prevention of chronic obstructive pulmonary disease exacerbation: a meta-analysis. PLoS One. 2015;10(3):e0121257.
Medical Research Council Working Party. Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Report of the Medical Research Council Working Party. Lancet. 1981;1(8222):681–6.
Nocturnal Oxygen Therapy Trial Group. Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: a clinical trial. Ann Intern Med. 1980;93(3):391–8.
Murphy PB, Rehal S, Arbane G, Bourke S, Calverley PMA, Crook AM, et al. Effect of home noninvasive ventilation with oxygen therapy vs oxygen therapy alone on hospital readmission or death after an acute COPD exacerbation: a randomized clinical trial. JAMA. 2017;317(21):2177–86.
Calverley PMA, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356(8):775–89.
Wedzicha JA, Calverley PM, Seemungal TA, Hagan G, Ansari Z, Stockley RA. The prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromide. Am J Respir Crit Care Med. 2008;177(1):19–26.
Soriano JB, Kiri VA, Pride NB, Vestbo J. Inhaled corticosteroids with/without long-acting beta-agonists reduce the risk of rehospitalization and death in COPD patients. Am J Respir Med. 2003;2(1):67–74.
Briggs AH, Lozano-Ortega G, Spencer S, Bale G, Spencer MD, Burge PS. Estimating the cost-effectiveness of fluticasone propionate for treating chronic obstructive pulmonary disease in the presence of missing data. Value Health. 2006;9(4):227–35.
Martinez FJ, Rabe KF, Ferguson GT, Wedzicha JA, Singh D, Wang C, et al. Reduced all-cause mortality in the ETHOS trial of budesonide/glycopyrrolate/formoterol for chronic obstructive pulmonary disease. A randomized, double-blind, multicenter, parallel-group study. Am J Respir Crit Care Med. 2021;203(5):553–64.
LaRosa JC, He J, Vupputuri S. Effect of statins on risk of coronary disease: a meta-analysis of randomized controlled trials. JAMA. 1999;282(24):2340–6.
Heart Protection Study Collaborative Group. MRC/BHF heart protection study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360(9326):7–22.
Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian simvastatin survival study (4S). Lancet. 1994;344(8934):1383–9.
Heart Outcomes Prevention Evaluation Study Investigators, Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000;342(3):145–53.
Janson C, Johansson G, Ställberg B, Lisspers K, Olsson P, Keininger DL, et al. Identifying the associated risks of pneumonia in COPD patients: ARCTIC an observational study. Respir Res. 2018;19(1):172.
Watz H, Tetzlaff K, Wouters EFM, Kirsten A, Magnussen H, Rodriguez-Roisin R, et al. Blood eosinophil count and exacerbations in severe chronic obstructive pulmonary disease after withdrawal of inhaled corticosteroids: a post-hoc analysis of the WISDOM trial. Lancet Respir Med. 2016;4(5):390–8.
Oshagbemi OA, Franssen FME, van Kraaij S, Braeken DCW, Wouters EFM, Maitland-van der Zee AH, et al. Blood eosinophil counts, withdrawal of inhaled corticosteroids and risk of COPD exacerbations and mortality in the Clinical Practice Research Datalink (CPRD). COPD. 2019;16(2):152–9.
Agusti A, Alcazar B, Cosio B, Echave JM, Faner R, Izquierdo JL, et al. Time for a change: anticipating the diagnosis and treatment of COPD. Eur Respir J. 2020;56(1):2002104.
Au DH, Bryson CL, Chien JW, Sun H, Udris EM, Evans LE, et al. The effects of smoking cessation on the risk of chronic obstructive pulmonary disease exacerbations. J Gen Intern Med. 2009;24(4):457–63.
van Eerd EAM, van der Meer RM, van Schayck OCP, Kotz D. Smoking cessation for people with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2016;2016(8):CD010744.
McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;(2):CD003793.
Waschki B, Spruit MA, Watz H, Albert PS, Shrikrishna D, Groenen M, et al. Physical activity monitoring in COPD: compliance and associations with clinical characteristics in a multicenter study. Respir Med. 2012;106(4):522–30.
Donaire-Gonzalez D, Gimeno-Santos E, Balcells E, de Batlle J, Ramon MA, Rodriguez E, et al. Benefits of physical activity on COPD hospitalisation depend on intensity. Eur Respir J. 2015;46(5):1281–9.
Waschki B, Kirsten AM, Holz O, Mueller K-C, Schaper M, Sack A-L, et al. Disease progression and changes in physical activity in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2015;192(3):295–306.
Waschki B, Kirsten A, Holz O, Müller K-C, Meyer T, Watz H, et al. Physical activity is the strongest predictor of all-cause mortality in patients with COPD: a prospective cohort study. Chest. 2011;140(2):331–42.
Troosters T, van der Molen T, Polkey M, Rabinovich RA, Vogiatzis I, Weisman I, et al. Improving physical activity in COPD: towards a new paradigm. Respir Res. 2013;14:115.
Demeyer H, Louvaris Z, Frei A, Rabinovich RA, de Jong C, Gimeno-Santos E, et al. Physical activity is increased by a 12-week semiautomated telecoaching programme in patients with COPD: a multicentre randomised controlled trial. Thorax. 2017;72(5):415–23.
Cranston JM, Crockett A, Moss J, Alpers JH. Domiciliary oxygen for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2005;2005(4):CD001744.
Group L-TOTTR. A randomized trial of long-term oxygen for COPD with moderate desaturation. N Engl J Med. 2016;375(17):1617–27.
Melani AS, Bonavia M, Cilenti V, Cinti C, Lodi M, Martucci P, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med. 2011;105(6):930–8.
Lavorini F, Janson C, Braido F, Stratelis G, Løkke A. What to consider before prescribing inhaled medications: a pragmatic approach for evaluating the current inhaler landscape. Ther Adv Respir Dis. 2019;13:1753466619884532.
National Institute for Health and Care Excellence. Chronic obstructive pulmonary disease in over 16s: diagnosis and management. NICE guideline [NG115]. 2018. https://www.nice.org.uk/guidance/ng115. Accessed 23 Jan 2020.
Morrison D, Agur K, Mercer S, Eiras A, González-Montalvo JI, Gruffydd-Jones K. Managing multimorbidity in primary care in patients with chronic respiratory conditions. NPJ Prim Care Respir Med. 2016;26:16043.
Lindh A, Theander K, Arne M, Lisspers K, Lundh L, Sandelowsky H, et al. Errors in inhaler use related to devices and to inhalation technique among patients with chronic obstructive pulmonary disease in primary health care. Nurs Open. 2019;6(4):1519–27.
Fletcher MJ, Dahl BH. Expanding nurse practice in COPD: is it key to providing high quality, effective and safe patient care? Prim Care Respir J. 2013;22(2):230–3.
Lisspers K, Johansson G, Jansson C, Larsson K, Stratelis G, Hedegaard M, et al. Improvement in COPD management by access to asthma/COPD clinics in primary care: data from the observational PATHOS study. Respir Med. 2014;108(9):1345–54.
British Thoracic Society Standards of Care Committee. BTS statement on criteria for specialist referral, admission, discharge and follow-up for adults with respiratory disease. Thorax. 2008;63(Suppl. 1):i1–i16.
Acknowledgements
Editorial support, under the direction of the authors, was provided by Richard Knight, PhD, CMC Connect, McCann Health Medical Communications, and was funded by AstraZeneca in accordance with Good Publication Practice (GPP3) guidelines (Ann Intern Med. 2015;163(6):461-4).
Funding
Open access funding provided by Karolinska Institute. This review was funded by AstraZeneca.
Author information
Authors and Affiliations
Contributions
HS, UMW, BBA, JS, KH, GS, AL, CJa, CJe and KL contributed to data analysis, drafting or revising the article, read and gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Authors’ information
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
HS has served on an advisory board or participated in educational activities arranged by AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline and Novartis.
UMW has served on an advisory board, as a speaker and/or participated in educational activities arranged by AstraZeneca, Boehringer Ingelheim, Chiesi, Fisher and Paykel Healthcare, GlaxoSmithKline, Novartis, Orion Pharma, Pfizer and Teva. In addition, UMW has received travel grants from Fisher and Paykel Healthcare.
BBA has served on an advisory board, as a speaker and/or participated in educational activities arranged by AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Novartis and Sanofi-Aventis.
JS has served as a speaker and/or participated in educational activities arranged by AstraZeneca, Boehringer Ingelheim, Chiesi and Novartis.
KH has served on an advisory board, as a speaker and/or participated in educational activities arranged by ALK, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Novartis, Orion Pharma, Sanofi-Aventis and Teva.
GS is a full-time employee of AstraZeneca.
AL has served on an advisory board, as a speaker, as principal investigator and/or participated in educational activities arranged by AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Novartis, Orion Pharma, Pfizer and Teva. Additionally, AL has received unrestricted research grants from Boehringer Ingelheim, Chiesi and Pfizer.
CJa has received honoraria for educational activities and lectures from AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Novartis and Orion and has served on advisory boards arranged by AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline and Novartis.
CJe has served on an advisory board, as a speaker and/or participated in educational activities arranged by AstraZeneca, Boehringer Ingelheim, Chiesi, Novartis and Sanofi-Aventis.
KL has served on an advisory board, as a speaker and/or participated in educational activities arranged by AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Novartis, Orion, Sanofi and Teva.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sandelowsky, H., Weinreich, U.M., Aarli, B.B. et al. COPD – do the right thing. BMC Fam Pract 22, 244 (2021). https://doi.org/10.1186/s12875-021-01583-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-021-01583-w