Abstract
Background
Unscheduled return visits (URVs) to emergency departments (EDs) are used to assess the quality of care in EDs. Machine learning (ML) models can incorporate a wide range of complex predictors to identify high-risk patients and reduce errors to save time and cost. However, the accuracy and practicality of such models are questionable. This review compares the predictive power of multiple ML models and examines the effects of multiple research factors on these models’ performance in predicting URVs to EDs.
Methods
We conducted the present scoping review by searching eight databases for data from 2010 to 2023. The criteria focused on eligible articles that used ML to predict ED return visits. The primary outcome was the predictive performances of the ML models, and results were analyzed on the basis of intervals of return visits, patient population, and research scale.
Results
A total of 582 articles were identified through the database search, with 14 articles selected for detailed analysis. Logistic regression was the most widely used method; however, eXtreme Gradient Boosting generally exhibited superior performance. Variations in visit interval, target group, and research scale did not significantly affect the predictive power of the models.
Conclusion
This is the first study to summarize the use of ML for predicting URVs in ED patients. The development of practical ML prediction models for ED URVs is feasible, but improving the accuracy of predicting ED URVs to beyond 0.75 remains a challenge. Including multiple data sources and dimensions is key for enabling ML models to achieve high accuracy; however, such inclusion could be challenging within a limited timeframe. The application of ML models for predicting ED URVs may improve patient safety and reduce medical costs by decreasing the frequency of URVs. Further research is necessary to explore the real-world efficacy of ML models.
Similar content being viewed by others
Introduction
Hospitals have been using unscheduled return visit (URV) rates and reattendance rates to assess the quality of care in their emergency departments (EDs) for many years. Higher URV rates not only increase health-care costs but also prolong wait times for patients who need immediate ED care. Studies have revealed that frequent visits to EDs significantly contribute to overcrowding in EDs, which can lead to delays in treatment and consequently higher mortality rates [1, 2]. Therefore, developing a predictive model for health-care systems is crucial for the adoption of early interventions to reduce ED revisits [3, 4].
Accurate predictive modeling is crucial for the development of interventions. URVs can be classified into illness-, doctor-, and patient-related returns; however, differentiating between these categories can be difficult [5]. Because of the multifaceted and complex nature of ED URVs a number of variables may affect URVs. Conventional statistical models are limited in their ability to identify high-risk patients because of these models’ reliance on preprogrammed rules derived from specific clinical predictors. By contrast, machine learning (ML) prediction models utilize nonparametric algorithms, which can incorporate a relatively comprehensive range of complex predictors while maintaining strong predictive performance [6, 7]. In addition, using ML-based methods can reduce errors, yield time and cost savings, and improve the quality of care services [8]. The use of ML models in predicting URVs to EDs has been investigated previously, and some studies have published their results [3, 9,10,11,12,13,14,15,16,17,18,19,20,21]. However, variations in methodology, patient population, research scale, and time interval have made determining the accuracy and practicality of using ML models to predict URVs to EDs difficult [22].
The present scoping review compared the predictive power of multiple ML models, assessed the proportion of methods used among the selected articles of each of these models, and examined the effects of multiple research factors on the performance of the models in predicting URVs. Additionally, we explored the clinical relevance of current ML models in predicting ED URVs.
Materials and methods
Information sources and search strategy
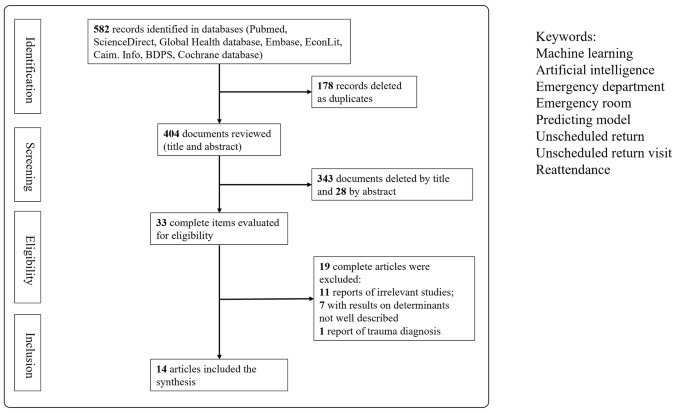
The protocol for this scoping review was developed on the basis of guidelines of the preferred reporting items for systematic review and meta-analysis (PRISMA) protocols statement [23] and was registered with the Open Science Framework [24]. The reporting of the present scoping review adheres to the PRISMA extension for scoping reviews [25]. We conducted a systematic search of eight databases (PubMed, ScienceDirect, the Global Health database, Embase, EconLit, Caim. Info, BDPS, and the Cochrane Library), using the following search terms of “Machine learning,” “Artificial intelligence,” “Emergency department,” “Emergency room,” “Predicting model,” “Predictive model,” “Unscheduled return,” “Unscheduled return visits,” “Reattendance,” and “Revisits.” Only studies published between January 2010 and February 2023 were selected to assess developments.
Selection process and eligibility criteria
Inclusion and exclusion criteria were established to identify relevant articles for this study. Published studies of any study design were considered eligible for inclusion, whereas conference abstracts and grey literature such as unpublished research, policy statements, and government reports were excluded.
Selected articles were required to meet the following criteria: (i) they included patient information within the scope of emergency care, with internal medical issues as the chief complaints; (ii) ML was utilized for making predictions, and the performance of the employed ML model was assessed using evaluation metrics; (iii) the prediction outcome involved ED URVs; (iv) the study report clearly defined the interval between a patient’s first and return visits; and (v) the study report provided a clear description of the scale of its analyzed patient population.
By contrast, articles with the following features were excluded from this study: (i) not written in English; (ii) related to traumatic diagnoses; (iii) not using ML methods for prediction; and (iv) the prediction of other outcomes—such as mortality, intensive care unit admission, and ED length of stay—without URV prediction.
Study selection and data extraction
Two reviewers independently screened the titles and abstracts of the articles found and conducted a full-text review of each to determine its eligibility for inclusion in this study. To increase efficiency, we divided the study selection and data extraction processes into blocks based on the publication date, beginning with articles published between 2010 and the search date of February 2023. All acceptable articles were then screened independently by the same two reviewers in full-text form, with each reviewer kept unaware of the other’s findings. Any conflicts that arose during study selection or data extraction process were resolved through discussion and consultation with a third member of the research team.
Outcome measures and data synthesis
The primary outcomes of this study were the determination of the efficacy of each analyzed ML model in predicting ED return visits and the determination of the proportion of methods used among the selected articles. We employed descriptive statistics to summarize the characteristics of the studies included in our analysis. Furthermore, the predictive performance of each ML model was analyzed and reported on the basis of the interval of return visits, patient population, and research scale.
Results
Study characteristics
Of the 582 articles identified through our electronic search, 33 were selected for full-text review. Finally, 14 articles published between 2010 and 2022 were analyzed in detail, as shown in Fig. 1 and summarized in Table 1. These 14 studies were conducted in multiple countries, namely seven in the United States, three in Taiwan, two in Singapore, one in the United Kingdom, and one in Portugal.
The selected studies analyzed the interval between each patient’s first visit and return visit; these intervals were then divided into groups of 72 h, 9 days, and 1 month. Nine articles exclusively predicted 72-hour return visits; Hong et al. predicted two outcomes, namely return visits within 72 h and return visits within 9 days [17]; and four articles predicted return visits within 30 days.
Data sample and predictors
In all the 14 selected articles, the study population comprised patients visiting EDs, with sample sizes approximately ranging from 200 to 1.25 million individuals. The study conducted by Suffoletto et al. [12] had the fewest participants; that study focused on patients older than 65 years, was conducted in two hospitals with 404 and 520 beds, and analyzed only 202 participants. By contrast, Poole et al. used the dataset of the Indiana Public Health Emergency Surveillance System, which covers more than 1.25 million patients and contains medical data from multiple institutions [11]. Although the data used for ML model implementation were specific to each study, several common categories were identified. These categories included demographic variables (e.g., age, sex), clinical variables (e.g., vital signs, diagnoses based on International Classification of Diseases codes), arrival information (e.g., arrival time, triage level, transport mode), and types of examinations (e.g., blood tests, images). Ten of the 14 analyzed articles included information regarding comorbidities or medical history [3, 9, 11, 12, 15, 17,18,19,20,21]. In addition, six of the articles considered chief or triage complaints, with those without chief complaints as variables using diagnoses instead [12,13,14, 16, 20, 21]. Four studies presented information regarding the use of hospital metrics (e.g., number of prior ED visits, number of prior hospitalizations) [3, 14, 19, 20]. Finally, in addition to using clinical variables, five articles linked their data to paramedical information, such as ethnicity, socioeconomic status, educational level, and insurance status [3, 10, 11, 20, 21].
ML process
Candidate variable handling and feature engineering
In most of the selected studies, all the variables were included in the implemented models. Both Fernandes et al. [16] and Poole et al. [11] used stepwise methods for feature selection to reduce the number of input variables.
Data resampling
In most of the selected articles, the datasets were randomly divided into training and testing datasets. Cross-validation, which can help prevent the overfitting or underfitting of a model, was used in five of the selected studies [3, 9, 15, 17, 19].
Prediction algorithms and calibration of parameters
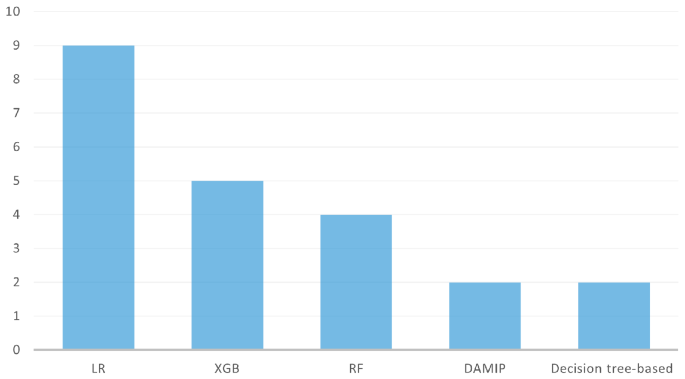
In total, 33 models were used to predict ED return visits. Logistic regression (LR; n = 9/14 articles) and eXtreme Gradient Boosting (XGB; n = 5/14) were the two most widely used methods, followed by random forest (RF; n = 3/14) and then discriminant analysis using mixed integer programming (DAMIP; n = 2/14) and decision tree–based models (n = 2/14) (Fig. 2). Some models were used in only one study. Only nine models in five studies used the cross-validation method to validate the model performance or to tune hyperparameters. R and Python were the most commonly used tools.
Evaluation metrics
The metrics used to evaluate the performances of the tested models included the area under the receiver operating characteristic (ROC) curve (AUC), sensitivity and specificity, and accuracy. The ROC-AUC metrics were the most frequently used.
Model agnostic methods
The majority of the authors used LR coefficients to determine significant variables. Feature importance analysis was implemented in seven studies to calculate the importance of the predictors [10, 11, 13, 17, 19,20,21].
Model performance assessment
Interval between two visits (72 h, 9 days, 30 days)
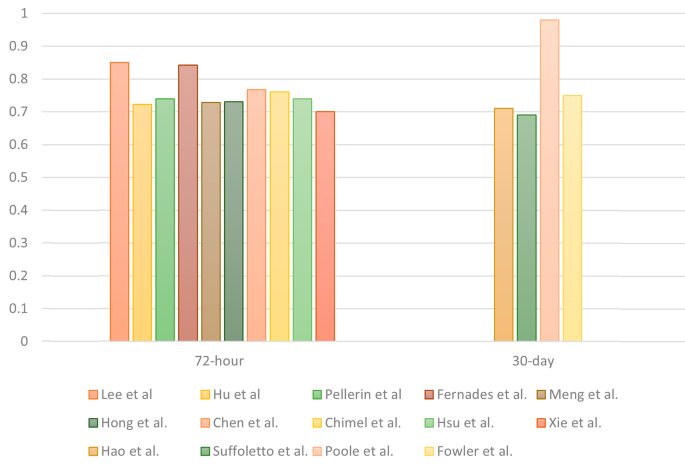
Most of the studies (n = 11/14) focused on predicting URVs within a 72-hour interval. A total of 25 models were developed to predict 72-hour URVs, whereas two models were developed for 9-day URVs and six were developed for 30-day URVs. The AUC was used to evaluate the performances of the predictive models; the corresponding results are presented in Table 1. For 72-hour URVs, LR was the most commonly adopted method, with a median AUC of 0.72 and an interquartile range (IQR) of 0.69–0.77. XGB exhibited similar predictive power across all the studies where it was used, with a median AUC of 0.73 and an IQR of 0.71–0.76. For 30-day URVs, the AUC ranged from 0.69 to 0.98, with LR achieving the lowest score of 0.69 in the study with 202 patients [12]. The RF model achieved the highest score, namely 0.98 in the study with approximately 1.25 million patients [11]. The highest AUCs of all the studies are presented in Fig. 3.
Patient population
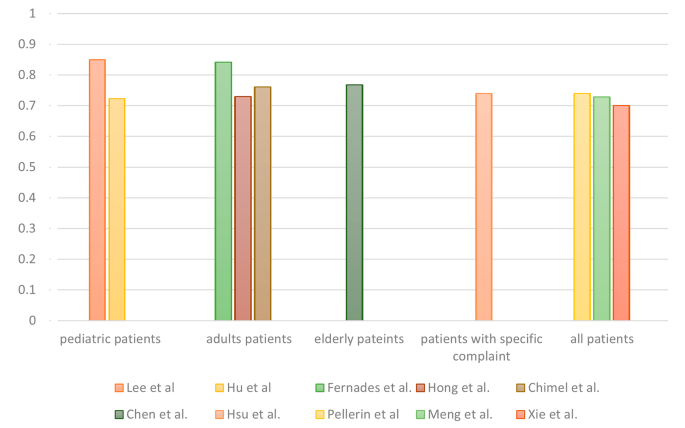
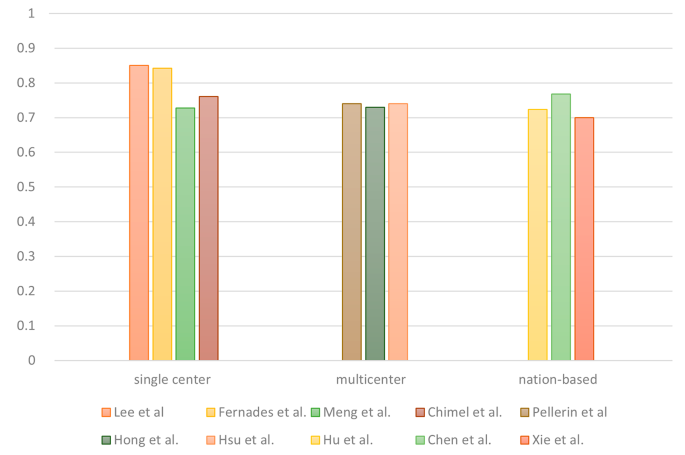
Different target groups were present in the 14 analyzed studies. Six articles analyzed all patients who visited the included EDs, whereas others focused on specific age groups, including adult patients (n = 3/14), pediatric patients (n = 2/14) and older adult patients (n = 2/14). Hsu et al. conducted the only study that focused on adult patients with abdominal pain [20]. For 72-hour URV prediction across the various patient populations, the AUCs ranged from 0.7 to 0.85, and no significant differences between target groups were observed (Fig. 4).
Research scale
The selected articles were divided into single-center, multicenter, and national database studies on the basis of their research scale. Five of the articles used data from a single hospital, and four articles analyzed data from multiple hospitals. In addition, five articles employed national or statewide databases from the United States, Taiwan, Singapore, or the American state of Indiana. For 72-hour URVs, no evident differences in AUCs were observed among studies with different research scales (Fig. 5).
Discussion
To the best of our knowledge, the present study was the first to attempt to provide a comprehensive overview of the use of ML models for predicting URVs among patients who presented to EDs. Our study discusses the application of ML-based decision support systems for predicting the probability of URVs to EDs based on existing literature. Regarding the ED revisit intervals, the initial timeframe we selected for inclusion was within 1 month, a cutoff borrowed from Medicare’s Hospital Readmission Reduction Program [26]. Although periods ranging up to 30 days have been used as timeframes for ED return visits in previous studies, a shorter timeframe of 72 h may be more useful in identifying return visits related to the previous episode of care and also identifying preventable revisits [27]. In our analysis, no evident differences in prediction accuracy between different timeframes were observed among the selected studies, with the exception of the country-based study conducted by Poole et al., which aimed to predict ED revisits within 1 to 6 months [11]. Developing ML models to predict 72-hour URVs to an acceptable degree of accuracy is feasible according to our review given that 72-hour URVs, rather than 30-day URVs or longer-term URVs, are more relevant to quality of care in EDs.
According to our results, LR was the most widely utilized method; however, it may not consistently yield the highest predictive accuracy compared with other models, even after undergoing multiple corrections and adjustments. In addition, linear relationships may not exist between variables; thus, a nonlinear model is necessary. RF has been frequently employed in related studies because it is a robust classifier. XGB has also been used extensively because of its ability perform well with imbalanced data by autoregulating class weights during training [28]. Among the commonly used models, XGB usually demonstrates the best predictive ability [29]; however, XGB has some shortcomings, such as false-negative preference [20]. An ensemble model, like voting classifier, combining multiple models with a specific weighting ratio has been adopted in some studies to achieve relatively favorable balance [16, 20, 21].
Overall, although some studies have achieved high predictive accuracy, improving the accuracy of predicting ED URVs to beyond 0.75 appears to be challenging. A primary limitation is that many studies record only reattendance without describing reasons for such reattendance or subsequent outcomes. Such a lack of differentiation can make distinguishing between patients with conditions with varying levels of severity difficult and ultimately can hinder the accuracy of prediction [30, 31]. URVs can be related to diseases, physicians, or patients. URVs caused by physician- or disease-related problems may be predicted by certain metrics; however, repeated ED attendance for patient-related reasons—such as free medical consultation cards, psychiatric problems, and social problems—is relatively difficult to predict given the complexity of such reasons, including health status and behavior. Most related studies have used only quantitative data, such as that related to lab values and vital signs, and have overlooked other types of data, such as imaging and text-based records, psychiatric and behavioral problems, and socioeconomic status. Such data may be difficult to extract from electronic health records; nevertheless, the accuracy of predictive models may be limited without the information [16, 18]. Additionally, most data used in ML models are collected only from the hospitals that patients visited first and do not include records from other nearby medical institutions; this drawback can result in incomplete patient histories or data [17, 27]. For example, patients may not return to the same hospital after their first visit because the accessibility of different hospitals in some country is high [20].
The models presented by most of the studies analyzed in the present study had similar predictive accuracies, and three of the studies had a higher-than-average accuracy [9, 11, 16]. Lee et al. conducted their study in a pediatric ED with a relatively low daily visit count and a relatively uniform patient population with few underlying conditions. The DAMIP approach used in their study established a classification rule based on a training set, which helped achieve higher blind predictive accuracy with small numbers of variables and an independent sample of patients [9, 15].
Poole et al. achieved exceptionally high predictive accuracy by using the RF model [32]. That study used a dataset that covered more than 1.25 million patients and medical data from multiple institutions and thus provided comprehensive patient histories. Additionally, those researchers focused on predicting URVs at the patient level rather than at each encounter, which allowed for more accurate prediction of the overall revisit risk [11, 13].
Compared with other studies that have used only quantifiable data, the study conducted by Fernandes et al. demonstrated a significant increase in accuracy when both textual and numerical data were employed for prediction. However, the precision of their model was low, which led to a relatively high false-positive rate [16]. In summary, data extraction from multiple nearby medical institutions and the inclusion of both textual and numerical data may increase the accuracy of ML models in predicting ED URVs; however, some conditions limit their practicality and range of applicability.
Previous studies have indicated that older age is associated with a higher risk of ED reattendance, and the presence of atypical or nonspecific geriatric syndromes may decrease the accuracy of return visit prediction [33]. Conversely, pediatric patients tend to have simpler medical histories, leading to higher predictive accuracy [15]. However, our review found no significant differences in predictive power among the patient subgroups of older adult patients, pediatric patients, adult patients, and all patients between the selected studies. Even when specific chief complaints were considered, predictive accuracy remained similar [20]. With regard to research scale, some studies have suggested that the results of single-center and multicenter studies may not fully capture return visits to EDs in other hospital systems, potentially leading to the underestimation of ED URVs [3, 5, 17]. Accordingly, in the present study, no evident superiority in predictive accuracy was noted for the national-level or multicenter research scales; however, this comparison was imprecise because many differences in conditions between the selected studies were present.
While developing a practical ML model for predicting ED URVs to a reasonable degree of accuracy appears feasible, it’s important to acknowledge that achieving this accuracy relies on the integration of multiple data sources and dimensions, as indicated by previous research [30, 34]. However, integrating detailed data within a limited timeframe could be a challenging task [27, 31]. In addition, although models that predict ED URVs improve patient safety and reduce costs, these models may have limited efficacy when applied in the real world. Thus, further empirical research is necessary.
Limitations
This study had some limitations. First, this study was a scoping review study, and thus although the inclusion of qualitative content enabled contextualization of the current ML evidence base, related quantitative outcomes may have been inadequate. Second, ML techniques and skills are evolving rapidly, and thus the conditions governing ML models, as well as their performances, could change quickly. Finally, the present study selected only articles published in English, and thus some key information published in another language or other languages may have been overlooked.
Conclusion
To the best of our knowledge, this study is the first to summarize the use of ML models for predicting URVs in ED patients. The results indicated the feasibility of developing practical ML models for predicting ED URVs. LR was the most widely utilized method, whereas XGB generally demonstrated the highest predictive ability. In addition, this study found that including multiple data sources and dimensions is vital for enabling ML models to achieve higher accuracy but that such inclusion could be challenging within a limited timeframe. Finally, the application of ML models for predicting ED URVs may improve patient safety and reduce medical costs; however, further research is necessary to explore the real-world effects of such application.
Data availability
All data used and analyzed during this study are included in this published article.
Abbreviations
- URV:
-
Unscheduled return visit
- ED:
-
Emergency department
- ML:
-
Machine learning
- PRISMA:
-
Preferred reporting items for systematic review and meta-analysis
- LR:
-
Logistic regression
- XGB:
-
eXtreme Gradient Boosting
- RF:
-
Random forest
- DAMIP:
-
Discriminant analysis using mixed integer programming
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
References
Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52(2):126–36.e1.
Navanandan N, et al. Seventy-two-hour return initiative: improving emergency department discharge to decrease returns. Pediatric Quality & Safety; 2020;5.
Pellerin G, Gao K, Kaminsky L. Predicting 72-hour emergency department revisits. Am J Emerg Med. 2018;36(3):420–4.
Schenkel S. Promoting patient safety and preventing medical error in emergency departments. Acad Emerg Med. 2000;7(11):1204–22.
Chan AHS, et al. Characteristics of patients who made a return visit within 72 hours to the emergency department of a Singapore tertiary hospital. Singapore Med J. 2016;57(6):301.
Gao F et al. Predictive Models for Emergency Department Triage using machine learning: a systematic review. Obstet Gynecol Res. 2022;5(02).
Rajkomar A, Dean J, Kohane I. Machine learning in medicine. N Engl J Med. 2019;380(14):1347–58.
Mueller B, et al. Artificial intelligence and machine learning in emergency medicine: a narrative review. Acute Med Surg. 2022;9(1):e740.
Lee EK et al. A clinical decision tool for predicting patient care characteristics: patients returning within 72 hours in the emergency department. in AMIA Annual Symposium Proceedings. 2012. American Medical Informatics Association.
Hao S, et al. Risk prediction of emergency department revisit 30 days post discharge: a prospective study. PLoS ONE. 2014;9(11):e112944.
Poole S, Grannis S, Shah NH. Predicting emergency department visits AMIA Summits on Translational Science Proceedings, 2016. 2016;438.
Suffoletto B, et al. Predicting older adults who return to the hospital or die within 30 days of emergency department care using the ISAR tool: subjective versus objective risk factors. Emerg Med J. 2016;33(1):4–9.
Fowler B et al. Predicting patient revisits at the University of Virginia health system emergency department. in 2017 Systems and Information Engineering Design Symposium (SIEDS). 2017. IEEE.
Hu Y-H et al. Predicting return visits to the emergency department for pediatric patients: applying supervised learning techniques to the Taiwan National Health Insurance Research Database. Computer methods and programs in biomedicine, 2017;144:105–112.
Meng F, et al. Predicting 72-hour reattendance in emergency departments using discriminant analysis via mixed integer programming with electronic medical records. J Industrial Manage Optim. 2019;15(2):947.
Fernandes M, et al. Risk of mortality and cardiopulmonary arrest in critical patients presenting to the emergency department using machine learning and natural language processing. PLoS ONE. 2020;15(4):e0230876.
Hong WS, Haimovich AD, Taylor RA. Predicting 72-hour and 9-day return to the emergency department using machine learning. JAMIA open. 2019;2(3):346–52.
Chen R-F, et al. Predicting unscheduled emergency department return visits among older adults: population-based retrospective study. JMIR Med Inf. 2021;9(7):e22491.
Chmiel F, et al. Using explainable machine learning to identify patients at risk of reattendance at discharge from emergency departments. Sci Rep. 2021;11(1):21513.
Hsu C-C, et al. A machine learning Model for Predicting unscheduled 72 h return visits to the Emergency Department by patients with Abdominal Pain. Diagnostics. 2022;12(1):82.
Xie F, et al. Benchmarking emergency department prediction models with machine learning and public electronic health records. Sci Data. 2022;9(1):658.
Rising KL, et al. Patient returns to the emergency department: the time-to‐return curve. Acad Emerg Med. 2014;21(8):864–71.
Moher D, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Reviews. 2015;4(1):1–9.
Lee J. Machine Learning Model for Predicting Unscheduled Return Visits to the Emergency Department: A Scoping Review. https://archive.org/details/osf-registrations-phc8n-v1. 2023 [accessed 06 May 2003].
Tricco AC, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Catalyst N. Hospital readmissions reduction program (HRRP). NEJM Catalyst; 2018.
Martin-Gill C, Reiser RC. Risk factors for 72-hour admission to the ED. Am J Emerg Med. 2004;22(6):448–53.
Wang C, Deng C, Wang S. Imbalance-XGBoost: leveraging weighted and focal losses for binary label-imbalanced classification with XGBoost. Pattern Recognit Lett. 2020;136:190–7.
Hancock J, Khoshgoftaar TM. Performance of catboost and xgboost in medicare fraud detection. in 2020 19th IEEE International Conference on Machine Learning and Applications (ICMLA). 2020. IEEE.
Johnson AE, et al. Machine learning and decision support in critical care. Proc IEEE. 2016;104(2):444–66.
Lindsay P, et al. The development of indicators to measure the quality of clinical care in emergency departments following a modified-Delphi approach. Acad Emerg Med. 2002;9(11):1131–9.
Song J et al. The random forest model has the best accuracy among the four pressure ulcer prediction models using machine learning algorithms. Risk Manage Healthc Policy, 2021;1175–87.
Corbett HM, et al. Care coordination in the Emergency Department: improving outcomes for older patients. Aust Health Rev. 2005;29(1):43–50.
Hayward J, et al. Predictors of admission in adult unscheduled return visits to the emergency department. Western J Emerg Med. 2018;19(6):912.
Acknowledgements
This research was supported by Chang Gung Memorial Hospital. In addition, we are thankful to our colleagues who contributed their expertise, which greatly assisted this research even though those colleagues may not have agreed with all the interpretations provided in this paper.
Funding
This work was supported by Chang Gung Memorial Hospital (CMRPG3M0491).
Author information
Authors and Affiliations
Contributions
The study design was conceived by YCL and agreed upon by CCH and SYC. The methodology was formulated by YCL with advice from SYC. YCL performed the search of the databases and removed duplicates. Title and abstract searching were completed by YCL with SYC carrying out the 10% inter-reliability check. CJN is responsible for revision and administrative supervision, and CWC is responsible for writing reviews and conducting statistical analysis. The full texts were screened independently by YCL, CCH, and SYC with agreement on the final selection. YCL drafted the first version of the manuscript, and all authors contributed to, read, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Was not applicable to this research.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lee, YC., Ng, CJ., Hsu, CC. et al. Machine learning models for predicting unscheduled return visits to an emergency department: a scoping review. BMC Emerg Med 24, 20 (2024). https://doi.org/10.1186/s12873-024-00939-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-024-00939-6