Abstract
Background
The COVID-19 pandemic severely impacted care for non-COVID patients. Performance indicators to monitor acute care, timely reported and internationally accepted, lacked during the pandemic in OECD countries. This study aims to summarize the performance indicators available in the literature to monitor changes in the quality of acute care in OECD countries during the first year and a half of the pandemic (2020-July 2021) and to assess their trends.
Methods
Scoping review. Search in Embase and MEDLINE (07-07-2022). Acute care performance indicators and indicators related to acute general surgery were collected and collated following a care pathway approach. Indicators assessing identical clinical measures were grouped under a common indicator title. The trends from each group of indicators were collated (increase/decrease/stable).
Results
A total of 152 studies were included. 2354 indicators regarding general acute care and 301 indicators related to acute general surgery were included. Indicators focusing on pre-hospital services reported a decreasing trend in the volume of patients: from 225 indicators, 110 (49%) reported a decrease. An increasing trend in pre-hospital treatment times was reported by most of the indicators (n = 41;70%) and a decreasing trend in survival rates of out-of-hospital cardiac arrest (n = 61;75%). Concerning care provided in the emergency department, most of the indicators (n = 752;71%) showed a decreasing trend in admissions across all levels of urgency. Concerning the mortality rate after admission, most of the indicators (n = 23;53%) reported an increasing trend. The subset of indicators assessing acute general surgery showed a decreasing trend in the volume of patients (n = 50;49%), stability in clinical severity at admission (n = 36;53%), and in the volume of surgeries (n = 14;47%). Most of the indicators (n = 28;65%) reported no change in treatment approach and stable mortality rate (n = 11,69%).
Conclusion
This review signals relevant disruptions across the acute care pathway. A subset of general surgery performance indicators showed stability in most of the phases of the care pathway. These results highlight the relevance of assessing this care pathway more regularly and systematically across different clinical entities to monitor disruptions and to improve the resilience of emergency services during a crisis.
Similar content being viewed by others
Background
Since the World Health Organization (WHO) declared the COVID-19 outbreak a “Public Health Emergency of International Concern” [1] on the 30th of January, 2020, the COVID-19 pandemic has severely impacted health systems worldwide [2], alongside far-reaching economic and societal impact [3]. The surge of patients infected with SARS-CoV-2 led to staff deployment and reduced hospital capacity [4]. Furthermore, the containment measures enforced by national governments [5], patients’ hesitance to seek care [6, 7], and postponements of elective care contributed to disruptions in care pathways for non-COVID-19 patients, notably patients with noncommunicable diseases (NCDs) [8,9,10]. A care pathway or clinical pathway is a “structured multidisciplinary care plan” [11], which is used to translate evidence into local structures, to describe the steps of a treatment plan or care in a pathway or any “inventory of actions (i.e. the intervention has time-frames or criteria-based progression)” [11]. Furthermore, it intends to be a tool for care standardization for specific clinical problems in specific populations [11] and its ultimate aim is to improve quality of care [12]. Deleterious consequences of delayed care were reported among the Organization for Economic Co-operation and Development (OECD) member countries [9], such as increased mortality rates following hospital admissions with an acute cardiac event in several European countries in 2020 [8].
Emergency and trauma care are recognized by the WHO as part of Universal Health Coverage [13]. Emergency departments (EDs) are key to ensuring accessible, effective, and time-sensitive healthcare services, notably during crises [13, 14]. The WHO Emergency Care System Framework [15] provides a structured tool to appraise the essential functions of an emergency care system at the national level. During the pandemic, EDs worldwide faced the need to adapt quickly: services have reconfigured their structure to separate (potentially) infected from non-infected patients, build additional capacity, ensure physical distancing, and introduce new operational pathways, among others [16,17,18,19,20]. However, many OECD countries presented substantial data gaps to evaluate health services performance during this period [8], such as access and quality of ambulance and emergency care. To prepare emergency care systems in maintaining essential functions during crises, and ensure quality and equity of care [21], improvements in the regular monitoring of performance are paramount.
Healthcare performance measurement allows for regularly appraising health systems and informing policy-making [22]. Quality indicators can be defined as “quantitative measures that provide information about the effectiveness, safety and/or people-centeredness of care” [11]. Previous authors pursued efforts to identify indicators that could be used to monitor ED’s performance, from the literature and/or with consensus-based techniques [23,24,25,26]. Nonetheless, indicators that are fit for purpose and use [27], reported transparently, timely, internationally accepted, and grounded on robust health information systems lacked during the COVID-19 pandemic and are needed to guarantee the continuous monitoring of the quality of acute care provided and to tailor policy responses during a crisis [28, 29]. This scoping review intends to contribute to this knowledge, considering OECD member countries, which share a conceptual framework for performance measurement [30]. Therefore, we set out: 1) to summarize the performance indicators available in the literature, according to the phases of the acute care pathway, to monitor changes in the quality of acute care in OECD countries during the first year and a half of the COVID-19 pandemic (2020—July 2021) and 2) to assess their trends during this period.
Methods
Study design
We performed a scoping review following the methodological framework developed by Arksey and O’Malley [31] and Levac et al. [32]. Considering the heterogeneous methodologies of the studies assessing changes in the quality of care during the COVID-19 pandemic and the diversity of settings being studied [33], applying a scoping review methodology allows mapping the literature [32, 34, 35], specifically the performance indicators used to evaluate healthcare and the information they provide regarding changes in the quality of care [36]. Furthermore, it enables the synthesis and communication of emerging evidence [31, 34] and the identification of knowledge gaps [36]. This methodology has been described by the authors in two previous studies [37, 38], where different clinical areas were studied. The PRISMA checklist—extension for scoping reviews [39] was used for reporting (Additional file 1).
Eligibility criteria
The following inclusion criteria were considered: 1) original scientific articles providing empirical data on the use of health services (including literature reviews); 2) studies displaying performance indicators related to NCDs during the COVID-19 pandemic; and 3) studies applying quantitative and/or qualitative methods. Studies were excluded when they did not provide empirical data on health services, namely: 1) editorials and commentaries; 2) prediction models; 3) clinical case reports; 4) health services organization or diseases management guidelines; 5) studies assessing the impact on healthcare workers, patients diagnosed with COVID-19, children, or pregnant women; 6) studies primarily performed in non-OECD countries; 7) conference abstracts. No limitations were set regarding language or year.
Information sources & search strategy
The literature search was performed in Embase and MEDLINE databases. These two databases retrieve the most unique references in systematic reviews [40]. Relevant search terms were identified through pilot searches. The search strategy was elaborated by an experienced medical information specialist and refined following internal discussions among the research team. Search terms were grouped by key concepts: COVID-19, pandemic, noncommunicable disease, chronic disease, performance indicator, healthcare quality, healthcare utilization, and healthcare delivery. The information specialist conducted the search on 17–03-2021, which was updated on 14–12-2021 and 07–07-2022. The entire search strategy for Embase is available in Additional file 2. Duplicates were removed using EndNote reference management software.
Study selection
Two reviewers (ASVC, OBF) screened titles and abstracts independently with Rayyan [41]. Disagreements were solved through discussion or consultation with a third reviewer (NK). Following the updates of the search strategy, one reviewer (ASVC) screened titles and abstracts. The records deemed relevant were exported to a spreadsheet. Only articles related to healthcare utilization of emergent and urgent care were considered for this study. Articles focusing exclusively on acute neurological, cardiac diseases, and trauma were excluded, considering that previous publications have extensively studied these subjects [37, 42,43,44,45,46]. Taking into consideration that most of the patients presenting with surgical diseases in the emergency department are evaluated by general surgeons, surgical diseases not evaluated in the general surgery setting were excluded. Full-text articles were independently screened for eligibility by two reviewers (ASVC, BB). Disagreements were solved through discussion and the reasons for exclusion were recorded at this stage. Articles in a language other than English, Dutch, French, Spanish, or Portuguese were translated to English with Google Translate, considering its accuracy [47].
Data extraction and charting
A spreadsheet form was developed to collect data. First, we performed a pilot test with 10 studies, from which data were collected by one reviewer (BB) and revised by another (ASVC) (Additional file 3). Then, the spreadsheet form was consolidated through discussion. Subsequently, two reviewers (ASVC, BB) collected data independently, which were revised by one another. Extracted information from the studies comprised: generic and methodological aspects (e.g., title, country, study design), data regarding the indicators collected (e.g., indicator title as stated in the studies, numerator/denominator, inclusion/exclusion considerations), and the trend reported for every indicator (increase/decrease/stable). The trends regarding each indicator were collected as reported by the authors in each of the included studies. When the computation and/or the interpretation was not available, it was computed as: ((value during the COVID-19 pandemic) – (value before the COVID-19 pandemic)) / (value during the COVID-19 pandemic) * 100. The positive values were considered an increasing trend, the negative values were considered a decreasing trend, and values close to zero were considered stable.
Data synthesis
Indicators collected from studies assessing emergent/urgent care without focusing on specific diseases were collated together. Indicators collected from studies explicitly related to general surgery in the ED were analyzed separately.
Indicators assessing identical clinical measures were grouped. Given the heterogeneity of indicator titles referring to equivalent measures, the authors attributed a common indicator title to each group of indicators assessing similar aspects of healthcare (eg, “volume of patients contacting emergency medical services”). The trends from each group of indicators were collated, and the percentage of indicators reporting each trend (increase/decrease/stable) was computed. For groups of indicators retrieved in low numbers (< 10 indicators), a trend was not computed. The groups of indicators and their combined trends were reported according to the phases of the acute care pathway: pre-hospital setting, access to the ED, diagnostic and treatment in the ED, and outcomes.
Results
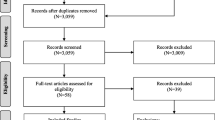
Database searches retrieved 15454 records. Following screening of titles and abstracts, 2393 studies met the inclusion criteria. From those, 624 acute care studies were assessed for eligibility, from which 319 were excluded, considering the clinical areas excluded for this review. A total of 305 acute care studies focusing on healthcare utilization and general surgery were considered for full-text screening. Two records were identified via hand-searching. Following the full-text screening, 152 were included and 155 studies were excluded (reasons for exclusion detailed in Fig. 1).
PRISMA flow diagram—literature search (17th March, 14th December 2021 and 07th July 2022). From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71
Studies characteristics
A total of 152 studies were included (Additional file 4), conveying information from 27 countries. The most frequent study design was the retrospective cohort (n = 141; 92.8%), followed by 5 prospective cohort studies (3.3%), 4 systematic reviews (2.6%), and 2 surveys (1.3%). Administrative data (n = 92; 56.8%) and clinical data (n = 49; 30.2%) were the most frequent data sources, followed by registries (n = 8), claims (n = 4), population-level data (n = 3), and surveys (n = 2). The most frequent countries reported on, excluding the literature reviews, were the United States of America (USA) (n = 39; 26.4%), Italy (n = 21; 14.2%), Canada (n = 12; 8.1%) and the United Kingdom (UK) (n = 10; 6.8%) (Table 1). The magnitude of the indicators in the year 2020, in each study, were compared to their magnitude in 2019 (n = 240; 36.9%), to the period immediately before the beginning of the pandemic (n = 162; 24.9%), or to the average in previous years, ranging from 2018 to 2019 (n = 111; 17.1%). Some studies compared the first half of the year 2021 to 2019 (n = 103; 15.8%) or the first half of the year 2021 to the previous years (n = 34; 5.2%).
Acute care indicators
A total of 2953 indicators related to acute care were collected: 2354 indicators from 124 studies focusing on general emergent/urgent healthcare and 301 indicators from 28 studies related to acute general surgery (Table 2).
Indicators related to general emergent and urgent care
Indicators and their trends were collated according to the acute care pathway (pre-hospital services, admission to the emergency department, diagnosis, treatment, and outcomes), which are outlined as follows (Fig. 2).
Pre-hospital services
Volume of patients contacting emergency medical services
A total of 225 indicators from 20 studies [48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67] assessed the volume of patients contacting Emergency Medical Services (EMS). From those, most of the indicators (n = 110; 49%) showed a decreasing trend. These data came predominantly from Australia (n = 73 indicators; 33%) and Canada (n = 55 indicators; 24%).
One systematic review [68] reporting data from Australia, France, Italy, Spain, and the USA showed an increase of 120% in the number of out-of-hospital cardiac arrest (OHCA) events when comparing the year 2020 with a previous period.
Volume of bystander cardiopulmonary resuscitation
Twenty-six indicators from 10 studies [48, 56, 59, 60, 65, 66, 69,70,71,72] evaluated the volume of bystanders providing first aid in collapsed patients out-of-hospital. These indicators revealed, in most cases, a decreasing trend (n = 13;50%). Most data were from the USA (n = 9;35%) and France (n = 6;23%). Similarly, one systematic review [68] documented a decrease in bystander cardiopulmonary resuscitation (BCPR) rates during the pandemic, although not statistically significant. Two meta-analyses [73, 74] revealed no statistical difference in BCPR rates.
Proportion of patients with out-of-hospital cardiac arrest witnessed by bystanders
Twelve indicators from 9 studies [48, 56, 59, 60, 65, 66, 69,70,71] reported on the proportion of patients with OHCA witnessed by bystanders, most of those (7;59%) showed stability in this proportion.
Pre-hospital treatment times
The analysis of the treatment times in the pre-hospital setting revealed 59 indicators from 12 studies [48, 50, 52, 55, 57, 59, 63, 65, 69,70,71,72], predominantly from Australia (n = 14; 27%) and Finland (n = 12;20%). Most indicators (n = 41;70%) signaled an increasing trend. The treatment times assessed included: “response time: start of an emergency call to the arrival of the first ambulance at the scene” [63], “activation time: from the time someone reports to EMS to the time EMS departure” [72], “on-scene time: from the time arrival at scene to the time of departure for hospital” [72], “transport time: departure from the scene to arrival at the hospital” [63], among others. Similarly, the systematic reviews that assessed pre-hospital treatment times [68, 73, 75] documented significantly increased times from OHCA to ambulance arrival during the pandemic.
Survival rate of patients with out-of-hospital cardiac arrest
Concerning the survival rate of patients with out-of-hospital cardiac arrest, 81 indicators from 14 studies [48, 51, 52, 55,56,57, 59, 60, 64,65,66, 70, 72, 76] were identified. These indicators included the following sub-categories of indicators: “on-scene death rate”, “rate of pre-hospital return of spontaneous circulation (ROSC)”, “survival rate to hospital admission”, and “survival rate to hospital discharge”. Most indicators (n = 61;75%) signaled a decreasing trend in survival rates. Data came predominately from Spain (n = 44;62%) and the USA (n = 20;26%). Similarly, three of the systematic reviews documented a significant increase in the mortality rate following OHCA during the pandemic [68], lower rates of pre-hospital ROSC [74, 75], decreased survival rates to hospital admission [74] and to hospital discharge [74, 75].
Admission to the emergency department
Volume of emergency department visits
A total of 1066 indicators from 87 studies [50, 52, 61, 67, 76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158] provided information on the volume of patients admitted to the Emergency Department. From these, 752 (71%) indicators displayed a decreasing trend. Most of the data came from the USA (n = 309;29%), Italy (n = 163;15%), and the UK (n = 122;11%).
Arrival mode to the emergency department
Three indicator categories were identified regarding the arrival mode of patients to the ED. A total of 16 indicators from 9 studies [67, 77, 81, 86, 93, 110, 124, 133, 137] assessed the volume of patients arriving with their own transport, from which 15 (94%) indicators showed a decreasing trend. Twenty-two indicators from 12 studies [52, 67, 77, 81, 86, 91, 110, 112, 124, 133, 137, 159] evaluated the volume of patients reaching the ED with the Emergency Medical Services. Most indicators (13;57%) signaled a decreasing trend. One study from Germany [110] displayed 40 indicators evaluating the number of ED admissions with a referral by a doctor related to different diseases; of those, 29 (72%) indicators showed a decreasing trend.
Level of urgency by a triage system
A total of 51 indicators from 31 studies [52, 62, 77, 80,81,82, 86, 88,89,90,91, 97, 98, 102, 103, 105, 108, 113, 116, 119, 123, 124, 126, 130,131,132, 134, 137, 142, 144, 158] were identified regarding patients presenting with level 1/highly urgent conditions to ED, mainly from the USA (n = 21;41%) and Italy (n = 13;25%). Of these indicators, 51% (n = 26) signaled a decreasing trend. Of 36 indicators from 26 studies [52, 62, 77, 80,81,82, 86, 88, 91, 97, 98, 102, 103, 105, 108, 113, 123, 124, 126, 130, 134, 137, 142, 151, 157, 158] reporting on the volume of patients presenting with level 2/urgent conditions to ED, 56% (n = 20) reported a decreasing trend. These data came predominantly from the USA (n = 14;39%) and Italy (n = 6;16%). Concerning the stable conditions/levels 3 and 4, 46 indicators from 22 studies [52, 62, 77, 81, 86, 91, 97, 98, 102, 108, 113, 116, 119, 123, 126, 130, 131, 134, 137, 142, 144, 158] provided information on indicators’ trends from 7 countries. Most of these indicators reported a decreasing trend (n = 31;67%). Data came mainly from the USA (n = 23;50%). Concerning non-urgent/level 5 conditions, a total of 55 indicators from 32 studies [52, 62, 77, 80,81,82, 86, 88,89,90,91, 97, 98, 102, 108, 113, 116, 119, 123, 124, 126, 130,131,132, 134, 137, 142, 144, 151, 156,157,158] were identified. Of these, 78% (n = 43) reported a decreasing trend in the volume of these patients. Data were reported predominantly from the USA (n = 20;36%) and Italy (n = 15;27%).
Clinical severity at admission
Regarding patients’ clinical severity at admission, 26 indicators from 8 studies [83, 103, 120, 136, 143, 159,160,161] were identified. Most indicators reported an increasing trend (n = 18;69%). Data were reported mainly from the UK (n = 8.31%) and Switzerland (n = 5;19%). The indicators retrieved were related to the overall severity of medical admissions [120], clinical severity of patients diagnosed with urolithiasis [136], diverticulitis [160], pyelonephritis [83], pulmonary embolism [103], chronic obstructive pulmonary disease [143], and appendicitis [159].
Diagnosis
Volume of diagnostic procedures
Information on the volume of diagnostic procedures in the ED was retrieved from 131 indicators from 16 studies [82, 86, 92, 95, 103, 113, 125, 145, 160,161,162,163,164,165,166,167] reporting on 8 countries. They displayed information regarding laboratory testing [162, 168], ultrasound imaging [86, 166], radiological examinations [86, 92, 103, 125, 145, 160,161,162,163,164,165,166,167], nuclear imaging [86, 166], and biopsies [95]. Most of the indicators reported on computed topographies (CT) (n = 64;49%) and laboratory testing (n = 16;6%). The predominant trend was a decrease in the volume of diagnostic procedures (n = 85,65%) (trends for each diagnostic procedure are detailed in Additional file 5). Data came predominantly from the USA (n = 74 indicators;56%) and Italy (n = 19;14%).
Rate of positive findings after diagnostic testing
A total of 32 indicators from 4 studies reporting on 4 countries were retrieved regarding the rate of positive diagnostic findings, namely positive blood cultures [162] and positive CT findings [92, 161, 162, 164]. Of these, 9 (58%) indicators displayed an increasing trend. Most indicators were from the USA (n = 18; 55%) and Ireland (n = 7; 21%).
Treatment
Volume of therapeutic interventions
A total of 106 indicators from 18 studies [67, 82, 83, 88, 92, 93, 95, 98, 99, 108, 136, 148, 151, 155, 159, 161, 169, 170] and 11 countries reported on therapeutic interventions in the ED. Most indicators signaled a decreasing trend (n = 54; 51%). The therapeutic interventions assessed were invasive procedures (e.g., endoscopy, endovascular intervention, endoscopic retrograde cholangiopancreatography, paracentesis, thoracentesis), acute surgical interventions, and other procedures, such as bedside procedures.
Operational times
Seventeen indicators from 10 studies and 7 countries reported on the average operational times for emergent and urgent care, such as average waiting time for triage [123, 167], from triage to first medical assistance [52, 123, 126, 130], from consultation to treatment [52, 90, 148, 161, 162], and for hospital ward admission [131]. Of these, 9 (53%) indicators signaled a decreasing trend.
Length of stay
A total of 14 indicators from 11 studies [52, 86, 91, 98, 114, 120, 126, 130, 145, 151, 157] reported on the length of stay (LOS) in the ED, from which 11 (79%) indicators displayed a decreasing trend. Concerning the in-hospital LOS after ED admission, 8 indicators from 5 studies [127, 130, 139, 143, 159] were retrieved, from which 62% (n = 5) reported a decreasing trend.
Outcomes
Disposition after visit to the Emergency Department
Concerning the volume of patients discharged home, a total of 26 indicators from 15 studies [52, 82, 86, 98, 102, 112, 113, 116, 117, 120, 130, 136, 151, 157, 158] and 5 countries were retrieved. Most indicators (n = 15;58%) reported a decreasing trend. Regarding the volume of hospital admission after ED presentation (including admission to intensive care unit), from the 191 indicators from 46 studies [52, 67, 77, 78, 81, 83, 85,86,87,88, 90,91,92,93,94, 96, 98, 100, 102, 103, 107, 108, 112,113,114,115,116,117, 120,121,122,123, 127, 128, 130, 131, 134, 137, 144, 145, 147, 149, 151, 152, 157, 158] collected, 52% (n = 100) signaled a decreasing trend, and 39% (n = 74) showed an increasing trend. Most of the indicators were from the USA (n = 43;23%), Italy (n = 35;18%), and Croatia (n = 23;12%). Eleven indicators from 7 studies [77, 98, 113, 130, 151, 157, 171] and 3 countries reported on the volume of patients leaving the ED without completing treatment, including patients that left the ED without being seen, completing treatment, and against medical advice; of these, 9 (82%) indicators signaled a decreasing trend.
Mortality rate
A total of 43 indicators from 23 studies [50, 52, 67, 76, 85, 91, 92, 96, 98, 107, 113, 120, 123, 127, 130, 133, 137, 139, 143, 149, 153, 157, 162] reported on the mortality rate after an ED visit. Most of the indicators signaled an increasing trend (n = 23;53%). Data came predominantly from Canada (n = 9;21%), Turkey (n = 6;14%), and Norway (n = 5;11%).
Trend analysis by country and clinical entity did not show recognizable tendencies in any of the indicators retrieved (Additional file 5). The trends of the indicator categories related to general acute care comparing the COVID-19 period to a previous period are displayed in Fig. 2.
Indicators related to acute general surgery care
Indicators on acute general surgery care were collected and grouped following the care pathway (admission, diagnosis, treatment, and outcomes), and their respective trends are summarized in Fig. 3.
Admission
Volume of emergency department visits
A total of 101 indicators from 17 studies [172,173,174,175,176,177,178,179,180,181,182,183,184,185,186,187,188] and 10 countries reported on the volume of ED visits related to acute general surgery. Of those, almost half of the indicators (n = 50;49%) signaled a decreasing trend. Most of the data were from Canada (n = 19;18%), the UK (n = 14;14%), and New Zealand (n = 12; 12%).
Clinical severity at admission
Indicators assessing patients’ clinical severity included clinical, laboratory and imaging features at admission, severity grading according to diseases-specific scores, operative findings, and the American Society of Anesthesiologists (ASA) score. Sixty-eight indicators were retrieved from 19 studies; of those, 36 (53%) indicators showed a stable clinical severity and 29 (43%) indicators signaled increased severity. The countries most represented were the USA (n = 19;28%), Israel (n = 15; 22%), and the UK (n = 11;16%).
Diagnosis
Eight indicators from four studies evaluated the diagnosis phases of the pathway, which did not provide sufficient information regarding trends.
Treatment
Volume of emergency surgeries
Data related to the volume of acute surgeries was retrieved from 30 indicators and 10 studies [174, 176, 185, 186, 188,189,190,191,192,193], from 8 countries. Most of the indicators (n = 14;47%) signaled stability in the volume of acute surgeries. Data came predominantly from Italy (n = 16;54%).
Change in treatment approach
A total of 43 indicators from 19 studies [173,174,175,176,177, 179, 180, 182, 183, 186, 188,189,190,191, 194,195,196,197,198] were retrieved. These indicators evaluated the treatment strategy in the acute surgical setting related to diseases such as appendicitis, acute cholecystitis, and bowel obstruction. Most of the indicators (n = 28;65%) signaled no change in the treatment approach. Data were predominantly from the UK (n = 12;28%) and Germany (n = 9;21%).
Length of hospital stay
Concerning the LOS in-hospital (including in the intensive care unit), 25 indicators from 20 [175,176,177,178,179,180,181, 183, 184, 186, 189,190,191, 193,194,195,196,197,198,199] studies were collected. Most of the indicators showed stability of the LOS (n = 19;76%). Data came mostly from the UK (n = 7;28%), USA (n = 4;16%), and Ireland (n = 4; 16%).
Outcomes
Post-operative complications
Ten indicators from 8 studies [174, 175, 179, 182, 186, 194,195,196] reported on post-operative complications. Most of these indicators (n = 7;70%) signaled stability in this outcome.
Mortality rate
Concerning the mortality rate, 16 indicators from 12 studies [174, 176,177,178, 182, 183, 186, 187, 189, 190, 195, 198] were collected. Of these, 69% (n = 11) signaled stability.
Discussion
In this scoping review, we aimed to summarize the performance indicators available in the literature to monitor changes in the quality of acute care in OECD countries and to assess their trends for the first year and a half of the COVID-19 pandemic (2020-July 2021). A total of 2953 indicators were collected from 152 studies reporting on 27 countries. Concerning access to acute care, indicators signaled a decreasing trend in the volume of patients, as well as increased clinical severity at presentation, and treatment delays. Trends regarding acute diagnostic and treatment procedures showed decreases in volume, as well as worsened outcomes. Similarly, the subset of indicators focusing on acute general surgery signaled a decrease in the volume of patients and increased clinical severity. Conversely, our results showed stable trends in acute general surgery regarding the volume of surgeries, length of hospital stay, treatment approaches, and outcomes.
Looking in detail at the stages of the acute care pathway, starting from the pre-hospital setting, our results showed a decrease in the volume of patients contacting EMS, which is in line with findings of other studies reporting reductions in access to primary care [8] and to hospital care by patients with acute myocardial infarction (AMI) [8], cancer [200], and stroke [201]. Our findings support that patients delayed care considering the increased time from symptom until calling the EMS, as reported in previous studies [202]. The decision to delay care might be related to fear of overwhelming the health system [7, 142] or getting infected with SARS-CoV2 [203]. This fear could also explain the decreasing trend in bystanders providing first aid that our results show. The possibility of reductions in the incidence of some diagnoses is a hypothesis to consider. However, it is difficult to quantify the exact number of “missed” diagnoses during the COVID-19 pandemic, as these are affected by several factors, such as changes in the mortality rates, lifestyle, or migration in each country. A study from the UK, conducting an analysis between March 2020 and December 2021, found a persistent decrease in the incidence rate of some respiratory diseases (such as asthma and chronic obstructive pulmonary disease), strokes, and heart diseases (such as coronary heart disease and atrial fibrillation), when compared to pre-pandemic levels [204]. Concerning stroke, the avoidance in care seeking is generally hypothesized as one of the justifications rather than the hypothesis of a real decrease in the incidence of stroke [205, 206]. Regarding the respiratory conditions, the social distance measures may have led to a reduced number of acute exacerbations of these diseases. Nonetheless, the restrictions in access to diagnostic testing (spirometry) could also have contributed to this decrease [204]. The impact of the pandemic in the outcomes of patients with cardiac diseases remains unclear. Factors such as the misclassification of cardiovascular deaths as COVID-19 deaths, the lack of population data and the lack of regular monitoring of the quality of cardiovascular care and outcomes makes it difficult to formulate accurate conclusions [207].
Despite the reduced demand, our results signaled an increasing trend in pre-hospital times, suggesting the timeliness of acute care was compromised. Delays triggered by patients, as signaled by our results, and insufficient timely response have most likely contributed to the worsening of survival rate trends in patients with OHCA that we report. Some authors have also reported increased pre-hospital times and worsened outcomes in patients with acute stroke [202] and AMI [208].
Regarding access to the ED, our results also signal substantial disruptions. We found a decreasing trend in the volume of patients regardless of triage classification or mean of arrival. This decrease was neither condition- nor country-specific, suggesting that fear and delay were relevant for patients with different clinical conditions and across different countries. Our results also signal a trend toward increased clinical severity at admission to the ED, as previous studies reported for specific diseases such as acute stroke [203]. These delays in access to pre-hospital care and to the ED highlight the need to improve communication strategies directed to patients with symptoms related to time-sensitive and life-threatening conditions during crises. Care provided at the ED should primarily focus on the most urgent patients, therefore the decreasing trend in access by non-urgent patients could provide a window of opportunity to avoid unjustified use of the ED, emphasizing the need to strengthen and integrate primary care support.
The reduced demand for access to acute care settings resulted in decreasing trends in acute diagnosis and treatment procedures. Noteworthy, our results also showed higher rates of positive findings after diagnostic testing, which is in line with the more severe clinical condition displayed in our results.
Our results feature a small sample of indicators concerning the timeliness of care in the ED that signal a decreasing trend in operational times and in LOS in the ED. Although this small sample of indicators was insufficient to compare trends among different periods, previous studies reported variations in the LOS during 2020 [209, 210] and for different clinical severities [211].
Regarding the outcomes after ED admission, we report a decreasing trend in the volume of patients discharged home and in the volume of hospital admissions, which are most likely related to the reduced demand. Additionally, our results signal a trend towards increased mortality rates after admission to the ED. This adverse outcome could be a consequence of delays in seeking care and increased pre-hospital treatment times. Worse clinical outcomes were previously reported for specific acute diseases during the pandemic, such as acute stroke [202] and AMI in several European countries [8, 212].
The analysis of the subset of indicators assessing acute general surgery care did not show similar disruptions. We found a decreasing trend in the volume of patients at the ED, however our results display no change in treatment approaches, length of stay, and outcomes. The small sample of indicators needs to be taken into consideration to interpret these findings. Notwithstanding, these results suggest that the quality of care provided to these patients has not substantially changed during the pandemic. The difference of these results compared to the general acute healthcare justify the need to monitor the pathways of acute diseases separately to identify and act upon changes in the quality of care regarding different clinical entities in a timely manner.
The disruptions signaled by these results highlight that the inclusion of this performance information as part of the continuous monitoring and more systematic assessment of emergency care systems is pivotal to tailoring policy responses timely and to building more resilient health systems. Performance intelligence, defined as “the structured approach to acting on health policies, using knowledge and information generated by the application of scientific methods to comparable healthcare data to systematically measure indicators of health systems performance” [28], can be a valuable tool to prepare for future crises [28]. Investment in data infrastructure is an essential component to enable performance intelligence [28] and to improve healthcare systems resilience [213]: the “ability of systems to prepare for, absorb, recover from and adapt to major shocks” [213].
Substantial advancements to health information systems were triggered by the COVID-19 pandemic, such as improved data linkage between data sets in the public sector, improved timeliness of national datasets, and adoption of digital tools [29]. Nonetheless, relevant hindrances still need to be addressed, namely related to regulatory barriers, data interoperability, quality and linkage, as well as the need for a skilled workforce in health information [29]. Good practices to inform further improvements are, for instance, Korea’s Emergency Medicine Monitoring System, a nationwide information network constructed in 2013 that links public sources to calculate key indicators at the entire acute care pathway, providing real-time information [168, 214, 215]. The Israeli National Hospital Discharge Register [216] also assesses performance indicators related to stroke and AMI regularly.
Our results expose only a few of indicators reflecting the impact on outcomes and experiences of patients or patient safety culture in hospitals, both recognized as relevant for international benchmarking and healthcare quality improvement [8, 217]. Future research is needed to provide a deeper analysis of the impact on specific acute clinical entities in a comparable way across countries. Moreover, stratified analyses of these indicators by patients’ sociodemographic characteristics will be useful to enhance the understanding of the trends we report and assess possible inequalities. Future studies to develop performance intelligence that is actionable to decision-making will be crucial in the years to come.
Strengths and limitations
Previous studies have investigated the impact of the COVID-19 pandemic in the acute care setting on specific countries [24, 209, 211, 218], phases of the pathway [142, 211], or diseases [203, 212, 219]. This scoping review provides a comprehensive overview of the changes reported on the quality of acute care during the first year and a half of the COVID-19 pandemic, covering OECD countries, multiple diseases, and following a care pathway approach. In addition, this review provides a summary of performance indicators from pre-hospital to in-hospital outcomes, which could be useful tools, if further developed and systematically collected, to inform policymaking. Some national and international reports [9, 220] proposed standards for acute care, where some of the performance indicators we retrieved were proposed to drive care improvements.
This study has some limitations. First, the heterogeneity of study designs, sample sizes, and indicators definitions did not allow to perform a meta-analysis to quantify the impact of the COVID-19 pandemic on the indicator categories identified, or to assess inequalities related to gender or socio-economic status. Secondly, despite the inclusion of all OECD countries, the heterogeneity in the number of studies per country comprised a skewed sample. Therefore, it needs to be considered that the professionals experiencing the most severe disruptions were likely the ones that were more inclined to report it.
Conclusion
This study signals relevant disruptions across the acute care pathway during the first year and a half of the COVID-19 pandemic, such as decreasing trends in the volume of patients, in the volume of diagnostic and treatment procedures, increased clinical severity at presentation, treatment delays, and worsened outcomes. A subset of general surgery indicators showed stability in most of the phases of the care pathway. This evidence underscores the relevance of monitoring the acute care pathway more regularly and systematically to assess the care processes and outcomes of these patients. This would allow to monitor care disruptions more efficiently. Furthermore, our results could contribute to strengthening health information infrastructures worldwide, which is an urgent step to monitor structure, process, and outcome information regarding patients with time-sensitive and life-threatening conditions. This is of paramount importance to improve the resilience of health systems during crises.
Availability of data and materials
The datasets generated and analysed during the current study are freely and openly available in the Zenodo.org repository, at https://doi.org/https://doi.org/10.5281/zenodo.7726234 [221].
Abbreviations
- AMI:
-
Acute myocardial infarction
- ASA:
-
American Society of Anesthesiologists
- ASVC:
-
Ana Sofia V. Carvalho
- BB:
-
Bente Broekema
- BCPR:
-
Bystander cardiopulmonary resuscitation
- CT:
-
Computed topographies
- EMS:
-
Emergency Medical Services
- LOS:
-
Length of stay
- NCDs:
-
Non-communicable diseases
- NK:
-
Niek Klazinga
- OBF:
-
Óscar Brito Fernandes
- OECD:
-
Organisation for Economic Co-operation and Development
- OHCA:
-
Out-of-hospital cardiac arrest
- ROSC:
-
Return of spontaneous circulation
- UK:
-
United Kingdom
- USA:
-
United States of America
References
World Health Organization. A year without precedent: WHO’s COVID-19 response. 2020 [cited 2023 Feb 2]. Available from: https://reliefweb.int/report/world/year-without-precedent-who-s-covid-19-response.
World Health Organization: Geneva. The impact of the COVID-19 pandemic on noncommunicable disease resources and services: results of a rapid assessment. 2020.
Committee for the Coordination of Statistical activities. How COVID-19 is changing the world: a statistical perspective, Volume III. 2021 [cited 2023 Feb 2]. Available from: https://data.unicef.org/resources/how-covid-19-is-changing-the-world-a-statistical-perspective-volume-iii/.
World Health Organization. Rapid assessment of service delivery for NCDs during the COVID-19 pandemic. 2020 [cited 2023 Feb 2]. Available from: https://www.who.int/publications/m/item/rapid-assessment-of-service-delivery-for-ncds-during-the-covid-19-pandemic.
OECD. Flattening the COVID-19 peak: Containment and mitigation policies. Tackling coronavirus (COVID-19)- Policy responses. 2020 [cited 2023 Feb 2]. Available from: https://www.oecd.org/coronavirus/policy-responses/flattening-the-covid-19-peak-containment-and-mitigation-policies-e96a4226/.
Czeisler MÉ, Marynak K, Clarke KE, Salah Z, Howard ME. Delay or avoidance of medical care because of COVID-19–Related concerns–United States. Morb Mortal Wkly Rep. 2020;69(36):1250.
Nab M, van Vehmendahl R, Somers I, Schoon Y, Hesselink G. Delayed emergency healthcare seeking behaviour by Dutch emergency department visitors during the first COVID-19 wave: a mixed methods retrospective observational study. BMC Emerg Med. 2021;21(1):56.
OECD, European Union. Health at a Glance: Europe 2022: State of Health in the EU Cycle. OECD; 2022 [cited 2023 Jan 6]. (Health at a Glance: Europe). Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-europe-2022_507433b0-en.
OECD. Health at a Glance 2021: OECD Indicators, OECD Publishing, Paris. 2021. Available from: https://doi.org/10.1787/ae3016b9-en.
World Health Organization. Pulse survey on continuity of essential health services during the COVID-19 pandemic - Key informant findings from 135 countries, territories and areas - Quarter 1 2021 Reporting period: 3 months preceding date of survey submission. [cited 2022 Jan 18]. Available from: https://www.who.int/docs/default-source/coronaviruse/finalupdate_22-april-2021_summary-ppt_ehs-pulse-survey_second-round.pdf?sfvrsn=a965e121_8.
Busse R, Klazinga N, Panteli D, Quentin W. Improving Healthcare Quality in Europe: Characteristics, Effectiveness and Implementation of Different Strategies. OECD; 2019 [cited 2022 Mar 2]. Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/improving-healthcare-quality-in-europe_b11a6e8f-en.
Vanhaecht K. The impact of clinical pathways on the organisation of care processes. 2007 [cited 2023 Dec 11]. Available from: https://lirias.kuleuven.be/retrieve/92842.
World Health Organization. SEVENTY-SECOND WORLD HEALTH ASSEMBLY - Emergency care systems for universal health coverage: ensuring timely care for the acutely ill and injured. WHA72.16. Resolution 72.16. 2019 [cited 2023 Feb 6]. Available from: https://apps.who.int/gb/ebwha/pdf_files/WHA72/A72_R16-en.pdf.
World Health Organization. SEVENTY-FOURTH WORLD HEALTH ASSEMBLY - Provisional agenda item 33. Emergency care systems for universal health coverage: ensuring timely care for the acutely ill and injured. 2021 [cited 2023 Feb 2]. Available from: https://apps.who.int/gb/ebwha/pdf_files/WHA74/A74_39-en.pdf.
World Health Organization. WHO Emergency Care System Framework. 2018 [cited 2023 Feb 2]. Available from: https://www.who.int/publications/i/item/who-emergency-care-system-framework.
The Royal College of Emergency Medicine. RCEM Position Statement; COVID-19: Resetting Emergency Department Care; 6 May 2020. [cited 2023 Jan 6]. Available from: https://res.cloudinary.com/studio-republic/images/v1633444736/RCEM_Position_statement_Resetting_Emergency_Care_20200506/RCEM_Position_statement_Resetting_Emergency_Care_20200506.pdf?_i=AA.
Choi A, Kim HY, Cho A, Noh J, Park I, Chung HS. Efficacy of a four-tier infection response system in the emergency department during the coronavirus disease-2019 outbreak. Pietrantonio F, editor. PLoS ONE. 2021;16(8):e0256116.
Barten DG, Kusters RWJ, Peters NALR. A swift and dynamic strategy to expand emergency department capacity for COVID-19. Disaster Med Public Health Prep. 2022;16(3):1190–3.
Garra G, Gupta S, Ferrante S, Apterbach W. Dedicated area within the emergency department versus an outside dedicated area for evaluation and management of suspected coronavirus disease 2019. J Am Coll Emerg Physicians Open. 2020;1(6):1349–53.
Australasian College for Emergency Medicine. The New Normal ED – Living with COVID-19. [cited 2023 Jan 6]. Available from: https://acem.org.au/Content-Sources/Advancing-Emergency-Medicine/COVID-19/Resources/Clinical-Guidelines/The-New-Normal-ED-%E2%80%93-Living-with-COVID-19.
World Health Organization: Geneva. SCORE for health data technical package: global report on health data systems and capacity, 2020. 2021.
Leatherman S. Performance measurement for health system improvement: Experiences, challenges and prospects. Smith PC, Mossialos E, Papanicolas I, editors. Cambridge: Cambridge University Press; 2010 [cited 2022 Apr 21]. Available from: http://ebooks.cambridge.org/ref/id/CBO9780511711800.
Schull MJ, Guttmann A, Leaver CA, Vermeulen M, Hatcher CM, Rowe BH, et al. Prioritizing performance measurement for emergency department care: consensus on evidencebased quality of care indicators. CJEM. 2011;13(05):300–9.
Etu EE, Monplaisir L, Aguwa C, Arslanturk S, Masoud S, Markevych I, et al. Identifying indicators influencing emergency department performance during a medical surge: a consensus-based modified fuzzy Delphi approach. Kuo YH, editor. PLoS ONE. 2022;17(4):e0265101.
Madsen M, Kiuru S, Castrèn M, Kurland L. The level of evidence for emergency department performance indicators: systematic review. Eur J Emerg Med. 2015;22(5):298–305.
Burgemeister S, Kutz A, Conca A, Holler T, Haubitz S, Huber A, et al. Comparative quality measures of emergency care: an outcome cockpit proposal to survey clinical processes in real life. Open Access Emerg Med. 2017;9:97–106.
Barbazza E, Klazinga NS, Kringos DS. Exploring the actionability of healthcare performance indicators for quality of care: a qualitative analysis of the literature, expert opinion and user experience. BMJ Qual Saf. 2021;30(12):1010–20.
Kringos D, Carinci F, Barbazza E, Bos V, Gilmore K, Groene O, et al. Managing COVID-19 within and across health systems: why we need performance intelligence to coordinate a global response. Health Res Policy Syst. 2020;18(1):80.
Health data and governance developments in relation to COVID-19: How OECD countries are adjusting health data systems for the new normal. 2022 [cited 2023 Jan 25]. (OECD Health Working Papers; vol. 138). Report No.: 138. Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/health-data-and-governance-developments-in-relation-to-covid-19_aec7c409-en.
Towards actionable international comparisons of health system performance: expert revision of the OECD framework and quality indicators. Int J Qual Health Care. 2015 [cited 2022 Apr 24]; Available from: https://academic.oup.com/intqhc/article/27/2/137/1787909/Towards-actionable-international-comparisons-of.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69.
Tolonen H, Reinikainen J, Koponen P, Elonheimo H, Palmieri L, Tijhuis MJ, et al. Cross-national comparisons of health indicators require standardized definitions and common data sources. Arch Public Health. 2021;79(1):208.
Lockwood C, dos Santos KB, Pap R. Practical guidance for knowledge synthesis: scoping review methods. Asian Nurs Res. 2019;13(5):287–94.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143.
Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119–26.
de Lange M, Carvalho AS, Brito Fernandes Ó, Lingsma H, Klazinga N, Kringos D. The Impact of the COVID-19 pandemic on hospital services for patients with cardiac diseases: a scoping review. Int J Environ Res Public Health. 2022;19(6):3172.
Carvalho AS, Fernandes ÓB, de Lange M, Lingsma H, Klazinga N, Kringos D. Changes in the quality of cancer care as assessed through performance indicators during the first wave of the COVID-19 pandemic in 2020: a Scoping Review. medRxiv.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Bramer WM, Rethlefsen ML, Kleijnen J, Franco OH. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev. 2017;6(1):245.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
Nguyen TN, Qureshi MM, Klein P, Yamagami H, Mikulik R, Czlonkowska A, et al. Global impact of the COVID-19 pandemic on stroke volumes and cerebrovascular events: a 1-year follow-up. Neurology. 2023;100(4):e408–21.
Raymaekers V, Demeestere J, Bellante F, De Blauwe S, De Raedt S, Dusart A, et al. The impact of COVID-19 on acute stroke care in Belgium. Acta Neurol Belg. 2021;121(5):1251–8.
Hakkenbrak NAG, Loggers SAI, Lubbers E, de Geus J, van Wonderen SF, Berkeveld E, et al. Trauma care during the COVID-19 pandemic in the Netherlands: a level 1 trauma multicenter cohort study. Scand J Trauma Resusc Emerg Med. 2021;29(1):130.
Sheets NW, Fawibe OS, Mahmoud A, Chawla-Kondal B, Ayutyanont N, Plurad DS. Impact of the COVID-19 pandemic on trauma encounters. Am Surg. 2023;89(3):434–9.
Jojczuk M, Pawlikowski J, Kamiński P, Głuchowski D, Naylor K, Gajewski J, et al. Evaluating changes in trauma epidemiology during the COVID-19 lockdown: insights and implications for public health and disaster preparedness. Healthc Basel Switz. 2023;11(17):2436.
Jackson JL, Kuriyama A, Anton A, Choi A, Fournier JP, Geier AK, et al. The accuracy of google translate for abstracting data from non–english-language trials for systematic reviews. Ann Intern Med. 2019;171(9):677.
Ball J, Nehme Z, Bernard S, Stub D, Stephenson M, Smith K. Collateral damage: Hidden impact of the COVID-19 pandemic on the out-of-hospital cardiac arrest system-of-care. Resuscitation. 2020;156:157–63.
Goldberg SA, Cash RE, Peters G, Weiner SG, Greenough PG, Seethala R. The impact of COVID-19 on statewide EMS use for cardiac emergencies and stroke in Massachusetts. J Am Coll Emerg Physicians Open. 2021;2(1):e12351.
Şan İ, Usul E, Bekgöz B, Korkut S. Effects of COVID‐19 Pandemic on Emergency Medical Services. Int J Clin Pract. 2021 [cited 2023 Feb 17];75(5). Available from: https://doi.org/10.1111/ijcp.13885.
Handberry M, Bull-Otterson L, Dai M, Mann NC, Chaney E, Ratto J, et al. Changes in emergency medical services before and during the COVID-19 pandemic in the United States, January 2018–December 2020. Clin Infect Dis. 2021;73(Supplement_1):S84-91.
Lane DJ, Blanchard IE, Buick JE, Shaw M, McRae AD. Changes in presentation, presenting severity and disposition among patients accessing emergency services during the first months of the COVID-19 pandemic in Calgary, Alberta: a descriptive study. CMAJ Open. 2021;9(2):E592-601.
Inokuchi R, Morita K, Iwagami M, Watanabe T, Ishikawa M, Tamiya N. Changes in the proportion and severity of patients with fever or common cold symptoms utilizing an after-hours house call medical service during the COVID-19 pandemic in Tokyo, Japan: a retrospective cohort study. BMC Emerg Med. 2021;21(1):64.
Grunau B, Helmer J, Lee S, Acker J, Deakin J, Armour R, et al. Decrease in emergency medical services utilization during early stages of the COVID-19 pandemic in British Columbia. Can J Emerg Med. 2021;23(2):237–41.
Laukkanen L, Lahtinen S, Liisanantti J, Kaakinen T, Ehrola A, Raatiniemi L. Early impact of the COVID-19 pandemic and social restrictions on ambulance missions. Eur J Public Health. 2021;31(5):1090–5.
Mathew S, Harrison N, Chalek AD, Gorelick D, Brennan E, Wise S, et al. Effects of the COVID-19 pandemic on out-of-hospital cardiac arrest care in Detroit. Am J Emerg Med. 2021;46:90–6.
Rollman JE, Kloner RA, Bosson N, Niemann JT, Gausche-Hill M, Williams M, et al. Emergency medical services responses to out-of-hospital cardiac arrest and suspected ST-segment–elevation myocardial infarction during the COVID-19 pandemic in Los Angeles County. J Am Heart Assoc. 2021;10(12):e019635.
Müller F, Hummers E, Jablonka A, Schmidt T, Noack EM. Auswirkung des COVID-19-Lockdowns auf Rettungseinsätze (Impact of the COVID-19 lockdown on emergency medical service operations). Notf Rettungsmedizin. 2022;25(5):341–7.
Grübl T, Plöger B, Sassen MC, Jerrentrup A, Schieffer B, Betz S. Prähospitaler Kreislaufstillstand im Lockdown: Auswirkungen der übergreifenden Infektionspräventionsmaßnahmen während der ersten SARS-CoV-2-Welle (Out-of-hospital cardiac arrest during lockdown). Notf Rettungsmedizin. 2021;1–6.
Glober NK, Supples M, Faris G, Arkins T, Christopher S, Fulks T, et al. Out-of-hospital cardiac arrest volumes and characteristics during the COVID-19 pandemic. Am J Emerg Med. 2021;48:191–7.
D’Ascenzi F, Cameli M, Forni S, Gemmi F, Szasz C, Fabrizio VD, et al. reduction of emergency calls and hospitalizations for cardiac causes: effects of Covid-19 pandemic and lockdown in Tuscany region. Front Cardiovasc Med. 2021;8:625569.
Ferron R, Agarwal G, Cooper R, Munkley D. The effect of COVID-19 on emergency medical service call volumes and patient acuity: a cross-sectional study in Niagara, Ontario. BMC Emerg Med. 2021;21(1):39.
Andrew E, Nehme Z, Stephenson M, Walker T, Smith K. The Impact of the COVID-19 Pandemic on Demand for Emergency Ambulances in Victoria, Australia. Prehosp Emerg Care. 2021;1–7.
Domont P, Debaize S, Curac S. Impact du SARS-CoV-2 sur les arrêts cardiaques extrahospitaliers. Rev Med Brux. 2022;43:110–6.
Damjanovic D, Pooth JS, Steger R, Boeker M, Steger M, Ganter J, et al. Observational study on implications of the COVID-19-pandemic for cardiopulmonary resuscitation in out-of-hospital cardiac arrest: qualitative and quantitative insights from a model region in Germany. BMC Emerg Med. 2022;22(1):85.
Chavez S, Huebinger R, Chan HK, Gill J, White L, Mendez D, et al. The impact of COVID-19 on incidence and outcomes from out-of-hospital cardiac arrest (OHCA) in Texas. Am J Emerg Med. 2022;57:1–5.
Lastrucci V, Collini F, Forni S, D’Arienzo S, Di Fabrizio V, Buscemi P, et al. The indirect impact of COVID-19 pandemic on the utilization of the emergency medical services during the first pandemic wave: a system-wide study of Tuscany Region, Italy. Baratta F, editor. PLoS ONE. 2022;17(7):e0264806.
Lim ZJ, Reddy MP, Afroz A, Billah B, Shekar K, Subramaniam A. Incidence and outcome of out-of-hospital cardiac arrests in the COVID-19 era: a systematic review and meta-analysis. Resuscitation. 2020;157:248–58.
Baert V, Jaeger D, Hubert H, Lascarrou JB, Debaty G, Chouihed T, et al. Assessment of changes in cardiopulmonary resuscitation practices and outcomes on 1005 victims of out-of-hospital cardiac arrest during the COVID-19 outbreak: registry-based study. Scand J Trauma Resusc Emerg Med. 2020;28(1):119.
Rosell Ortiz F, Fernández del Valle P, Knox EC, Jiménez Fábrega X, Navalpotro Pascual JM, Mateo Rodríguez I, et al. Influence of the Covid-19 pandemic on out-of-hospital cardiac arrest. A Spanish nationwide prospective cohort study. Resuscitation. 2020;157:230–40.
Burns TA, Touzeau C, Kaufman BT, Butsch AL, Vesselinov R, Stone RM. Decreases in out of hospital cardiac arrest (OHCA) outcome metrics persist when known COVID patients are excluded from analysis. Am J Emerg Med. 2022;51:64–8.
Chung H, Namgung M, Lee DH, Choi YH, Bae SJ. Effect of delayed transport on clinical outcomes among patients with cardiac arrest during the coronavirus disease 2019 pandemic. Australas Emerg Care. 2022;25(3):241–6.
Masuda Y, Teoh SE, Yeo JW, Tan DJH, Jimian DL, Lim SL, et al. Variation in community and ambulance care processes for out-of-hospital cardiac arrest during the COVID-19 pandemic: a systematic review and meta-analysis. Sci Rep. 2022;12(1):800.
Bielski K, Szarpak A, Jaguszewski MJ, Kopiec T, Smereka J, Gasecka A, et al. The influence of COVID-19 on out-hospital cardiac arrest survival outcomes: an updated systematic review and meta-analysis. J Clin Med. 2021;10(23):5573.
Scquizzato T, Landoni G, Paoli A, Lembo R, Fominskiy E, Kuzovlev A, et al. Effects of COVID-19 pandemic on out-of-hospital cardiac arrests: a systematic review. Resuscitation. 2020;157:241–7.
Jain N, Berkenbush M, Feldman DC, Eskin B, Allegra JR. Effect of COVID19 on prehospital pronouncements and ED visits for stroke and myocardial infarction. Am J Emerg Med. 2021;43:46–9.
Westgard BC, Morgan MW, Vazquez-Benitez G, Erickson LO, Zwank MD. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann Emerg Med. 2020;76(5):595–601.
Cole V, Atkinson P, Hanlon R, Dutton DJ, Liu T, Fraser J, et al. CO-aVoID: coronavirus outbreak affecting variability of presentations to a local emergency department. Can J Emerg Med. 2021;23:232–6.
Poyser A, Deol SS, Osman L, Kuht HJ, Sivagnanasithiyar T, Manrique R, et al. Impact of COVID-19 pandemic and lockdown on eye emergencies. Eur J Ophthalmol. 2021;31(6):2894–900.
Işık GÇ, Çevik Y. Impact of COVID-19 pandemic on visits of an urban emergency department. Am J Emerg Med. 2021;42:78–82.
Sekine I, Uojima H, Koyama H, Kamio T, Sato M, Yamamoto T, et al. Impact of non‐pharmaceutical interventions for the COVID‐19 pandemic on emergency department patient trends in Japan: a retrospective analysis. Acute Med Surg. 2020 [cited 2023 Feb 17];7(1). Available from: https://doi.org/10.1002/ams2.603.
Novara G, Bartoletti R, Crestani A, De Nunzio C, Durante J, Gregori A, et al. Impact of the COVID-19 pandemic on urological practice in emergency departments in Italy. BJU Int. 2020;126(2):245.
Borgmann H, Struck JP, Mattigk A, Wenzel M, Pilatz A, Kranz J, et al. Increased severe adverse outcomes and decreased emergency room visits for pyelonephritis: first report of collateral damage during COVID-19 pandemic in urology. Urol Int. 2021;105(3–4):199–205.
Lange SJ, Ritchey MD, Goodman AB, Dias T, Twentyman E, Fuld J, et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions — United States, January–May 2020. Am J Transplant. 2020;20(9):2612–7.
Franchini S, Spessot M, Landoni G, Piani C, Cappelletti C, Mariani F, et al. Stranger months: how SARS-CoV-2, fear of contagion, and lockdown measures impacted attendance and clinical activity during February and March 2020 at an urban Emergency Department in Milan. Disaster Med Public Health Prep. 2021;15(5):e33-42.
Sharperson C, Hanna TN, Herr KD, Zygmont ME, Gerard RL, Johnson JO. The effect of COVID-19 on emergency department imaging: what can we learn? Emerg Radiol. 2021;28:339–47.
Kuitunen I, Ponkilainen VT, Launonen AP, Reito A, Hevonkorpi TP, Paloneva J, et al. The effect of national lockdown due to COVID-19 on emergency department visits. Scand J Trauma Resusc Emerg Med. 2020;28(1):1–8.
Madanelo M, Ferreira C, Nunes-Carneiro D, Pinto A, Rocha MA, Correia J, et al. The impact of the coronavirus disease 2019 pandemic on the utilisation of emergency urological services. BJU Int. 2020;126(2):256–8.
Moon JY, Miller JB, Katz R, Ta T, Szypko C, Garg I, et al. The impact of the COVID-19 pandemic on ophthalmic care at an eye-specific emergency department in an outbreak hotspot. Clin Ophthalmol. 2020;4155–63.
Garrafa E, Levaggi R, Miniaci R, Paolillo C. When fear backfires: Emergency department accesses during the Covid-19 pandemic. Health Policy. 2020;124(12):1333–9.
Mitchell RD, O’Reilly GM, Mitra B, Smit DV, Miller J, Cameron PA. Impact of COVID-19 State of Emergency restrictions on presentations to two Victorian emergency departments. Emerg Med Australas. 2020;32(6):1027–33.
Griffith AM, Ockerse P, Shaaban A, Kelly C. Effect of the COVID-19 pandemic on CT scans ordered from the emergency department for abdominal complaints. Emerg Radiol. 2021;28(3):485–95.
Grasso AAC, Massa G, Castelnuovo M. The impact of COVID-19 pandemic on urological emergencies: a multicenter experience on over 3,000 patients. Urol Int. 2021;105(1–2):17–20.
Fahrner R, Bähler S, Lindner G. COVID-19 lock-down significantly reduced number of surgical presentations in an emergency department. Wien Klin Wochenschr. 2021;133(7–8):399–402.
Isoletta E, Vassallo C, Brazzelli V, Giorgini C, Tomasini CF, Sabena A, et al. Emergency accesses in Dermatology Department during the Covid‐19 pandemic in a referral third level center in the north of Italy. Dermatol Ther. 2020 [cited 2023 Feb 17];33(6). Available from: https://doi.org/10.1111/dth.14027.
Kastritis E, Tsitsimpis K, Anninos E, Stamatelopoulos K, Kanakakis I, Lampropoulos C, et al. Significant reduction in the visits to the emergency room department during the COVID-19 pandemic in a tertiary hospital in Greece: indirect victims of the pandemic? Medicine (Baltimore). 2020;99(52):e23845.
Giannouchos TV, Biskupiak J, Moss MJ, Brixner D, Andreyeva E, Ukert B. Trends in outpatient emergency department visits during the COVID-19 pandemic at a large, urban, academic hospital system. Am J Emerg Med. 2021;40:20–6.
Walker LE, Heaton HA, Monroe RJ, Reichard RR, Kendall M, Mullan AF, et al. Impact of the SARS-cov-2 pandemic on emergency department presentations in an integrated health system. Mayo Clin Proc. 2020;95(11):2395–407.
Porreca A, Colicchia M, D’Agostino D, Amenta M, Corsaro A, Zaramella S, et al. Urology in the time of coronavirus: reduced access to urgent and emergent urological care during the coronavirus disease 2019 outbreak in Italy. Urol Int. 2020;104(7–8):631–6.
Barten DG, Latten GHP, van Osch FHM. Reduced emergency department utilization during the early phase of the COVID-19 pandemic: viral fear or lockdown effect? Disaster Med Public Health Prep. 2022;16(1):36–9.
Boserup B, McKenney M, Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am J Emerg Med. 2020;38(9):1732–6.
Comelli I, Scioscioli F, Cervellin G. Impact of the COVID-19 epidemic on census, organization and activity of a large urban emergency department.: COVID-19 epidemic in a large emergency department. Acta Bio Medica Atenei Parm. 2020;91(2):45–9.
Nopp S, Janata-Schwatczek K, Prosch H, Shulym I, Königsbrügge O, Pabinger I, et al. Pulmonary embolism during the COVID-19 pandemic: decline in diagnostic procedures and incidence at a university hospital. Res Pract Thromb Haemost. 2020;4(5):835–41.
Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, et al. Impact of the COVID-19 pandemic on emergency department visits — United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704.
Franzolin E, Casati S, Albertini O, Antonelli G, Marchetti P, Bonora A, et al. Impact of Covid-19 pandemic on ophthalmic emergency department in an Italian tertiary eye centre. Eur J Ophthalmol. 2022;32(1):680–7.
Kociejowski A, Hobart C, Jina R, Aberman I, Backhurst E, Beaumont A, et al. Comparison of presentations to the emergency department during the COVID-19 pandemic (COPED-C). J Public Health. 2021;43(4):731–8.
Görmeli Kurt N, Çamcı M. COVID‐19: how do emergency departments fare after normalisation steps? Int J Clin Pract. 2021 [cited 2023 Feb 17];75(2). Available from: =https://doi.org/10.1111/ijcp.13912.
Motterle G, Morlacco A, Iafrate M, Bianco M, Federa G, Xhafka O, et al. The impact of COVID-19 pandemic on urological emergencies: a single-center experience. World J Urol. 2021;39(6):1985–9.
Jeffery MM, D’Onofrio G, Paek H, Platts-Mills TF, Soares WE, Hoppe JA, et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med. 2020;180(10):1328.
Stöwhas M, Lippert H. Impact of COVID-19 outbreak on emergency department admissions in a specialized hospital (Entwicklung der Notaufnahmefallzahlen eines Schwerpunktversorgers im Verlauf der Corona-Pandemie in Mecklenburg-Vorpommern). Gesundheitswesen Bundesverb Arzte Offentlichen Gesundheitsdienstes Ger. 2021;83(04):265–73.
Shreffler J, Shoff H, Thomas JJ, Huecker M. Brief report: the impact of COVID-19 on emergency department overdose diagnoses and county overdose deaths. Am J Addict. 2021;30(4):330–3.
Honeyford K, Coughlan C, Nijman R, Expert P, Burcea G, Maconochie I, et al. Changes in emergency department activity and the first COVID-19 lockdown: a cross-sectional study. West J Emerg Med. 2021 [cited 2023 Feb 17];22(3). Available from: https://escholarship.org/uc/item/2s7818zq.
Long A, Fillinger M, April MD, Hudson IL, Trueblood W, Schmitz G, et al. Changes in emergency department volumes at the largest U.S. military hospital during the COVID-19 pandemic. Mil Med. 2022;187(Special Issue_13):e1538–43.
Flamm A, Lee A, Mencl F. COVID-19: a comprehensive analysis of the pandemic’s effect on an emergency department. Disaster Med Public Health Prep. 2022;16(6):2367–70.
Wartelle A, Mourad-Chehade F, Yalaoui F, Chrusciel J, Laplanche D, Sanchez S. Effect of the COVID-19 pandemic lockdown on non-COVID-19 emergency department visits in Eastern France: reduced risk or avoidance behavior? Public Health Pract. 2021;2:100109.
Lowe J, Brown I, Duriseti R, Gallegos M, Ribeira R, Pirrotta E, et al. Emergency Department Access During COVID-19: Disparities in Utilization by Race/Ethnicity, Insurance, and Income. West J Emerg Med. 2021 [cited 2023 Feb 17];22(3). Available from: https://escholarship.org/uc/item/2hq8516p.
Sless RT, Hayward NE, Ryan PM, Deasy C, Dasari K. Emergency department attendances during the COVID-19 pandemic: a retrospective analysis of attendances following Irish governmental pandemic measures. Emerg Med J. 2021;38(6):439–45.
Venkatesh AK, Janke AT, Shu-Xia L, Rothenberg C, Goyal P, Terry A, et al. Emergency department utilization for emergency conditions during COVID-19. Ann Emerg Med. 2021;78(1):84–91.
İlhan B, Bozdereli Berikol G, Dogan H. Impact of COVID-19 outbreak on emergency visits and emergency consultations: a cross-sectional study. Cureus. 2021;13(3):e14052.
Reschen ME, Bowen J, Novak A, Giles M, Singh S, Lasserson D, et al. Impact of the COVID-19 pandemic on emergency department attendances and acute medical admissions. BMC Emerg Med. 2021;21(1):143.
Lee S, Santarelli A, Choi H, Ashurst J. Impact of the COVID-19 Pandemic on Emergency Department Transfers to a Higher Level of Care. West J Emerg Med. 2021 [cited 2023 Feb 17];22(3). Available from: https://escholarship.org/uc/item/620099vp.
Bergrath S, Strapatsas T, Tuemen M, Reith T, Deussen M, Aretz O, et al. Impact of the COVID-19 pandemic on emergency medical resources: An observational multicenter study including all hospitals in a major urban center of the Rhein-Ruhr metropolitan region. Anaesthesiol. 2022;71(S2):171–9.
Montero-Pérez FJ, Jiménez Murillo LM. Impact of the first COVID-19 pandemic wave on the care and quality indicators of a hospital emergency department. Emerg Rev Soc Espanola Med Emerg. 2021;33(5):345–53.
Wyatt S, Mohammed MA, Fisher E, McConkey R, Spilsbury P. Impact of the SARS-CoV-2 pandemic and associated lockdown measures on attendances at emergency departments in English hospitals: a retrospective database study. Lancet Reg Health - Eur. 2021;2:100034.
Kiliç P, Şendur HN. Impacts of COVID-19 pandemic on computed tomography usages in emergency department: cross-sectional study. Turk Klin J Med Sci. 2021;41(3):274–9.
Lee DD, Lou W, Rauchwerger D, Chartier L, Masood S, Taher AK. The Impact of COVID-19 on a Large, Canadian Community Emergency Department. West J Emerg Med. 2021 [cited 2023 Feb 17];22(3). Available from: https://escholarship.org/uc/item/0xk8j1fj.
Rennert-May E, Leal J, Thanh NX, Lang E, Dowling S, Manns B, et al. The impact of COVID-19 on hospital admissions and emergency department visits: a population-based study. Buttigieg SC, editor. PLoS ONE. 2021;16(6):e0252441.
Kalanj K, Marshall R, Karol K, Tiljak MK, Orešković S. The impact of COVID-19 on hospital admissions in Croatia. Front Public Health. 2021;9:720948.
Russo V, Boggian G, Bolognesi MG, Carretta DM, Cencetti S, De Laura D, et al. The impact of COVID-19 outbreak on syncope units activities in Italy: a report from the italian multidisciplinary working group on syncope (GIMSI). Int J Environ Res Public Health. 2021;18(17):9194.
Kwok E, Clapham G, Calder-Sprackman S. The impact of COVID-19 pandemic on emergency department visits at a Canadian academic tertiary care center. West J Emerg Med. 2021;22(4):851–9.
Muselli M, Cofini V, Mammarella L. The impact of covid-19 pandemic on emergency services.Ann Ig Med Prev E COMUNITÀ. 2021 [cited 2023 Feb 17]; Available from: https://doi.org/10.7416/ai.2021.2480.
Alwood S, Musso MW, Jones GN, Mosley J, Wippel B, Theriot L, et al. The impact of the COVID-19 pandemic and governor mandated stay at home order on emergency department super utilizers. Am J Emerg Med. 2021;48:114–9.
Vollmer MAC, Radhakrishnan S, Kont MD, Flaxman S, Bhatt S, Costelloe C, et al. The impact of the COVID-19 pandemic on patterns of attendance at emergency departments in two large London hospitals: an observational study. BMC Health Serv Res. 2021;21(1):1008.
Nok CN, Axeen S, Terp S, Burner E, Dworkis D, Arora S, et al. Who stayed home under safer-at-home? Impacts of COVID-19 on volume and patient-mix at an emergency department. West J Emerg Med. 2021;22(2):234.
Daniels NF, Ridwan R, Barnard EB, Amanullah TM, Hayhurst C. A comparison of emergency department presentations for medically unexplained symptoms in frequent attenders during COVID-19. Clin Med. 2021;21(4):e399-402.
Nourian A, Uppaluri C, Chen M, Ghiraldi EM, Friedlander JI. Comparison of management and outcomes of symptomatic urolithiasis during the COVID-19 pandemic to a comparative cohort. Urology. 2022;165:178–83.
Bardin A, Buja A, Barbiellini Amidei C, Paganini M, Favaro A, Saia M, et al. Elderly people’s access to emergency departments during the COVID-19 pandemic: results from a large population-based study in Italy. J Clin Med. 2021;10(23):5563.
Soares WE, Melnick ER, Nath B, D’Onofrio G, Paek H, Skains RM, et al. Emergency department visits for nonfatal opioid overdose during the COVID-19 pandemic across six US health care systems. Ann Emerg Med. 2022;79(2):158–67.
Jodal HC, Juul FE, Barua I, Bretthauer M, Kalager M, Løberg M, et al. Emergency hospital admissions, prognosis, and population mortality in Norway during the first wave of the Covid-19 epidemic. Scand J Public Health. 2022;50(6):795–802.
DelPozo-Banos M, Lee SC, Friedmann Y, Akbari A, Torabi F, Lloyd K, et al. Healthcare contacts with self-harm during COVID-19: an e-cohort whole-population-based study using individual-level linked routine electronic health records in Wales, UK, 2016—March 2021. Torok M, editor. PLoS ONE. 2022;17(4):e0266967.
Antonazzo IC, Fornari C, Maumus-Robert S, Cei E, Paoletti O, Conti S, et al. Impact of COVID-19 lockdown, during the two waves, on drug use and emergency department access in people with epilepsy: an interrupted time-series analysis. Int J Environ Res Public Health. 2021;18(24):13253.
Jessup RL, Bramston C, Beauchamp A, Gust A, Cvetanovska N, Cao Y, et al. Impact of COVID-19 on emergency department attendance in an Australia hospital: a parallel convergent mixed methods study. BMJ Open. 2021;11(12):e049222.
Lawless M, Burgess M, Bourke S. Impact of COVID-19 on hospital admissions for COPD exacerbation: lessons for future care. Medicina (Mex). 2022;58(1):66.
Ghaderi H, Stowell JR, Akhter M, Norquist C, Pugsley P, Subbian V. Impact of COVID-19 pandemic on emergency department visits: a regional case study of informatics challenges and opportunities. AMIA Annu Symp Proc AMIA Symp. 2021;2021:496–505.
Loftus TM, Wessling EG, Cruz DS, Schmidt MJ, Kim HS, McCarthy DM, et al. Impact of the COVID pandemic on emergency department CT utilization: where do we go from here? Emerg Radiol. 2022;29(5):879–85.
Lopez-Villegas A, Bautista-Mesa RJ, Baena-Lopez MA, Garzon-Miralles A, Castellano-Ortega MA, Leal-Costa C, et al. Impact of the COVID-19 pandemic on healthcare activity in the regional hospitals of Andalusia (Spain). J Clin Med. 2022;11(2):363.
Meurice L, Vilain P, Maillard L, Revel P, Caserio-Schonemann C, Filleul L. Impact des deux confinements sur le recours aux soins d’urgence lors de l’épidémie de COVID-19 en Nouvelle-Aquitaine (Impact of the two lockdowns on the use of a hospital emergency department during the COVID-19 epidemic in the Nouvelle-Aquitaine region). Santé Publique. 2021;33(3):393–7.
Vest A, Keilani C, Chaumet-Riffaud P, Barale PO, Tuil E, Ayello-Scheer S, et al. Incidence and characteristics of rhegmatogenous retinal detachment during coronavirus-19 pandemic: A French study. Eur J Ophthalmol. 2022;32(6):3644–9.
Sarc I, Lotric Dolinar A, Morgan T, Sambt J, Ziherl K, Gavric D, et al. Mortality, seasonal variation, and susceptibility to acute exacerbation of COPD in the pandemic year: a nationwide population study. Ther Adv Respir Dis. 2022;16:175346662210810.
Inglin L, Wikström K, Lamidi ML, Laatikainen T. The adverse effect of the COVID-19 pandemic on health service usage among patients with type 2 diabetes in North Karelia, Finland. BMC Health Serv Res. 2022;22(1):725.
Baugh JJ, White BA, McEvoy D, Yun BJ, Brown DFM, Raja AS, et al. The cases not seen: patterns of emergency department visits and procedures in the era of COVID-19. Am J Emerg Med. 2021;46:476–81.
Haklai Z, Applbaum Y, Myers V, Saban M, Gordon ES, Luxenburg O, et al. The effect of the COVID-19 pandemic on non-COVID respiratory ED visits in Israel. Am J Emerg Med. 2022;53:215–21.
Sagy YW, Cicurel A, Battat E, Saliba W, Lavie G. The impact of COVID-19 pandemic on emergency department visits and associated mortality during 14 months of the pandemic in Israel. Intern Emerg Med. 2022;17(6):1699–710.
Başer HY, Başer A. The impact of the Covid-19 pandemic on the short and mid-term urological emergencies and the emergency department. J Exp Clin Med. 2021;38(4):466–70.
Musajee M, Biasi L, Thulasidasan N, Green M, Francia F, Arissol M, et al. The Impact of the COVID-19 Pandemic on the Workload, Case Mix and hospital Resources at a Tertiary Vascular Unit. Ann Vasc Surg. 2022;80:104–12.
Zeppieri M, Maria Letizia Salvetat, Salati CS. The influence of COVID-19 lockdowns on presentation with spontaneous posterior vitreous detachment to the emergency department in Italy. Front Biosci-Elite. 2021;13(2):259.
Maclagan LC, Wang X, Emdin A, Jones A, Jaakkimainen RL, Schull MJ, et al. Visits to the emergency department by community-dwelling people with dementia during the first 2 waves of the COVID-19 pandemic in Ontario: a repeated cross-sectional analysis. CMAJ Open. 2022;10(3):E610–21.
Lucero A, Lee A, Hyun J, Lee C, Kahwaji C, Miller G, et al. Underutilization of the Emergency Department During the COVID-19 Pandemic. West J Emerg Med. 2020 [cited 2023 Feb 17];21(6). Available from: https://escholarship.org/uc/item/00p3c3fm.
Burgard M, Cherbanyk F, Nassiopoulos K, Malekzadeh S, Pugin F, Egger B. An effect of the COVID-19 pandemic: Significantly more complicated appendicitis due to delayed presentation of patients! Chen RJ, editor. PLoS ONE. 2021;16(5):e0249171.
Gibson AL, Chen BY, Rosen MP, Paez SN, Lo HS. Impact of the COVID-19 pandemic on emergency department CT for suspected diverticulitis. Emerg Radiol. 2020;27:773–80.
Anderson S, McNicholas D, Murphy C, Cheema I, McLornan L, Davis N, et al. The impact of COVID-19 on acute urinary stone presentations: a single-centre experience. Ir J Med Sci 1971 -. 2022;191(1):45–9.
Miyagami T, Uehara Y, Harada T, Watari T, Shimizu T, Nakamura A, et al. Delayed treatment of bacteremia during the COVID-19 pandemic. Diagnosis. 2021;8(3):327–32.
Houshyar R, Tran-Harding K, Glavis-Bloom J, Nguyentat M, Mongan J, Chahine C, et al. Effect of shelter-in-place on emergency department radiology volumes during the COVID-19 pandemic. Emerg Radiol. 2020;27:781–4.
Agarwal M, Udare A, Alabousi A, van der Pol CB, Ramonas L, Mascola K, et al. Impact of the COVID-19 pandemic on emergency CT head utilization in Ontario—an observational study of tertiary academic hospitals. Emerg Radiol. 2020;27(6):791–7.
Garlisi C, Licandro D, Siani A, Rodolfi S, Pansini S, Garcia Navarro LI, et al. Impact of the COVID-19 pandemic on the activity of the Radiological Emergency Department: the experience of the Maggiore della Carità Hospital in Novara. Emerg Radiol. 2021;28(4):705–11.
Parikh KD, Ramaiya NH, Kikano EG, Tirumani SH, Pierce J, Butcher C, et al. Quantifying the decrease in emergency department imaging utilization during the COVID-19 pandemic at a multicenter healthcare system in Ohio. Emerg Radiol. 2020;27(6):765–72.
Konson A, Kuniavsky M, Bronshtein O, Goldschmidt N, Hanhart S, Mahalla H, et al. Quality of care indicator performance was minimally changed in 2020 despite the COVID-19 pandemic. Isr J Health Policy Res. 2022;11(1):9.
Lee KS, Min HS, Moon JY, Lim D, Kim Y, Ko E, et al. Patient and hospital characteristics predict prolonged emergency department length of stay and in-hospital mortality: a nationwide analysis in Korea. BMC Emerg Med. 2022;22(1):183.
Eppenberger LS, Golla K, Schmid MK. Emergency vitrectomies for retinal detachment before and during the coronavirus pandemic – a retrospective single centre analysis. Klin Monatsblätter Für Augenheilkd. 2022;239(04):476–83.
Barış ME, Çiftçi MD, Güven Yılmaz S, Ateş H. Impact of COVID-19-related lockdown on glaucoma patients. Turk J Ophthalmol. 2022;52(2):91–5.
Giusti GD, Cozzolino MR, Gili A, Ceccagnoli A, Ceccarelli M, Groff P, et al. Patients who leave the emergency department without being seen. Has COVID-19 affected this phenomenon? Acta Biomed Atenei Parm. 2022;93(S2):e2022188.
O’Brien CM, Jung K, Dang W, Jang HJ, Kielar AZ. Collateral damage: the impact of the COVID-19 pandemic on acute abdominal emergency presentations. J Am Coll Radiol. 2020;17(11):1443–9.
Nishida Y, Otagiri N, Tauchi K. Emergency abdominal surgeries remain unchanged in the COVID‐19 affected environment: a single‐center experience at a community hospital in Japan. Acute Med Surg. 2021 [cited 2023 Feb 17];8(1). Available from: https://doi.org/10.1002/ams2.623.
Aviran E, Laks S, Benvenisti H, Khalilieh S, Assaf D, Aviran N, et al. The impact of the COVID-19 pandemic on general surgery acute admissions and urgent operations: a comparative prospective study. Isr Med Assoc J IMAJ. 2020;11(22):673–9.
Köhler F, Acar L, van den Berg A, Flemming S, Kastner C, Müller S, et al. Impact of the COVID-19 pandemic on appendicitis treatment in Germany—a population-based analysis. Langenbecks Arch Surg. 2021;406(2):377–83.
O’Connell RM, Khan MA, Amir M, Bucheeri M, Khan W, Khan IZ, et al. The impact of COVID-19 on emergency general surgery admissions and operative volumes: a single centre experience. The Surgeon. 2021;19(5):e207–12.
McGuinness MJ, Hsee L. Impact of the COVID-19 national lockdown on emergency general surgery: Auckland City Hospital’s experience. ANZ J Surg. 2020;90(11):2254–8.
Dick L, Green J, Brown J, Kennedy E, Cassidy R, Othman S, et al. Changes in emergency general surgery during covid-19 in scotland: a prospective cohort study. World J Surg. 2020;44(11):3590–4.
Gomez D, Simpson AN, Sue-Chue-Lam C, de Mestral C, Dossa F, Nantais J, et al. A population-based analysis of the impact of the COVID-19 pandemic on common abdominal and gynecological emergency department visits. Can Med Assoc J. 2021;193(21):E753–60.
Aboul-Enein MS, Ishak P, Bhambra M, Ricart P, Al-makdase L, Mourad M, et al. At a glance: the impact of COVID-19 on emergency general surgery. Surg Pract. 2021;25(1):16–24.
Vallès KF, Neufeld MY, Caron E, Sanchez SE, Brahmbhatt TS. COVID-19 pandemic and the cholecystitis experience at a major urban safety-net hospital. J Surg Res. 2021;264:117–23.
Amendola A, Palomba G, Gaudiello M, Dinuzzi VP, Marra E, Fusco F, et al. Impact of SARS-Cov-2 pandemic on emergency general surgery. A single-center observational study. Ann Ital Chir. 2021;92:317–22.
Callan R, Assaf N, Bevan K. Impact of the COVID-19 pandemic on acute general surgical admissions in a district general hospital in the United Kingdom: a retrospective cohort study. Surg Res Pract. 2020;2020:1–7.
Rajesh J, Valentelyte G, McNamara DA, Sorensen J. Impact of the COVID-19 pandemic on provision and outcomes of emergency abdominal surgery in Irish public hospitals. Ir J Med Sci 1971 -. 2022;191(5):2275–82.
Vissio E, Falco EC, Scozzari G, Scarmozzino A, Trinh DAA, Morino M, et al. The adverse impact of the COVID-19 pandemic on abdominal emergencies: a retrospective clinico-pathological analysis. J Clin Med. 2021;10(22):5254.
Siegel R, Hohenstein S, Anders S, Strik M, Kuhlen R, Bollmann A. Access to surgery and quality of care for acute cholecystitis during the COVID-19 pandemic in 2020 and 2021 — an analysis of 12,545 patients from a German-wide hospital network. J Gastrointest Surg. 2022;26(7):1462–71.
Reinke CE, Wang H, Thompson K, Paton BL, Sherrill W, Ross SW, et al. Impact of COVID-19 on common non-elective general surgery diagnoses. Surg Endosc. 2023;37(1):692–702.
Balvardi S, Cipolla J, Touma N, Vallipuram T, Barone N, Sivarajan R, et al. Impact of the Covid-19 pandemic on rates of emergency department utilization and hospital admission due to general surgery conditions. Surg Endosc. 2022;36(9):6751–9.
Karlafti E, Benioudakis ES, Paramythiotis D, Sapalidis K, Kaiafa G, Didangelos T, et al. Does the COVID-19 pandemic affect morbidity and mortality rates of emergency general surgery? A retrospective study from a single-center tertiary Greek hospital. Medicina (Mex). 2021;57(11):1185.
Lund S, MacArthur T, Fischmann MM, Maroun J, Dang J, Markos JR, et al. Impact of COVID-19 governmental restrictions on emergency general surgery operative volume and severity. Am Surg. 2021;000313482110111.
Farber ON, Gomez GI, Titan AL, Fisher AT, Puntasecca CJ, Arana VT, et al. Impact of COVID-19 on presentation, management, and outcomes of acute care surgery for gallbladder disease and acute appendicitis. World J Gastrointest Surg. 2021;13(8):859–70.
Kurihara H, Marrano E, Ceolin M, Chiara O, Faccincani R, Bisagni P, et al. Impact of lockdown on emergency general surgery during first 2020 COVID-19 outbreak. Eur J Trauma Emerg Surg. 2021;47(3):677–82.
Ma JLG, Yogaraj V, Siddiqui M, Chauhan K, Tobin VA, Pilgrim CHC. The impact of COVID-19 on emergency cholecystectomy. ANZ J Surg. 2022;92(3):409–13.
Bajomo O, Hampal R, Sykes P, Miah A. Managing appendicitis during the COVID-19 era: a single centre experience & implications for future practice. Ann Med Surg. 2021;63:102168.
Antakia R, Xanthis A, Georgiades F, Hudson V, Ashcroft J, Rooney S, et al. Acute appendicitis management during the COVID-19 pandemic: a prospective cohort study from a large UK centre. Int J Surg. 2021;86:32–7.
Rudnicki Y, Soback H, Mekiten O, Lifshiz G, Avital S. The impact of COVID-19 pandemic lockdown on the incidence and outcome of complicated appendicitis. Surg Endosc. 2022;36(5):3460–6.
Lapsekili E, Buldanlı MZ, Peker YS. Comparison of outcomes of the patients with acute cholecystitis treated in the COVID-19 pandemic and pre-pandemic period. Rev Assoc Médica Bras. 2021;67(11):1681–6.
Derebey M, Yüksek MA, Karabacak U, Mutlu V, Mi̇Zan SR, Tarim İA, et al. Effects of COVID-19 pandemic on management of acute cholecystitis: A single tertiary center’s experience. J Exp Clin Med. 2022;39(1):164–8.
Hossain N, Naidu V, Hosny S, Khalifa M, Mathur P, Al WM. Hospital presentations of acute diverticulitis during COVID-19 pandemic may be more likely to require surgery due to increased severity: a single-centre experience. Am Surg. 2022;88(1):133–9.
Fujisawa, Rie. Impact of the COVID-19 pandemic on cancer care in OECD countries. OECD Health Working Papers. 2022 [cited 2022 May 27]. (OECD Health Working Papers; vol. 141). Report No.: 141. Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/impact-of-the-covid-19-pandemic-on-cancer-care-in-oecd-countries_c74a5899-en.
Reddy ST, Satani N, Beauchamp JES, Selvaraj S, Rajan SS, Rahbar MH, et al. A meta-analysis of the global impact of the COVID-19 pandemic on stroke care & the Houston Experience. Ann Clin Transl Neurol. 2021;8(4):929–37.
Seo AR, Lee WJ, Woo SH, Moon J, Kim D. Pre-Hospital delay in patients with acute stroke during the initial phase of the coronavirus disease 2019 outbreak. J Korean Med Sci. 2022;37(6):e47.
Aref HM, Shokri H, Roushdy TM, Fathalla F, El Nahas NM. Pre-hospital causes for delayed arrival in acute ischemic stroke before and during the COVID-19 pandemic: a study at two stroke centers in Egypt. Barboza MA, editor. PLoS ONE. 2021;16(7):e0254228.
Research and analysis. Direct and indirect health impacts of COVID-19 in England: emerging Omicron impacts. 2023. Available from: https://www.gov.uk/government/publications/direct-and-indirect-health-impacts-of-covid-19-in-england-emerging-omicron-impacts/direct-and-indirect-health-impacts-of-covid-19-in-england-emerging-omicron-impacts#category-c-indirect-impacts-of-covid-19-on-po.
D’Anna L, Brown M, Oishi S, Ellis N, Brown Z, Bentley P, et al. Impact of national lockdown on the hyperacute stroke care and rapid transient ischaemic attack outpatient service in a comprehensive tertiary stroke centre during the COVID-19 pandemic. Front Neurol. 2021;12:627493.
Stroke Association. Stroke recoveries at risk report: key findings. [cited 2023 Dec 14]. Available from: https://www.stroke.org.uk/stroke-recoveries-at-risk-report/key-findings.
Roth GA, Vaduganathan M, Mensah GA. Impact of the COVID-19 pandemic on cardiovascular health in 2020: JACC state-of-the-art review. J Am Coll Cardiol. 2022;80(6):631–40.
Tomasoni D, Adamo M, Italia L, Branca L, Chizzola G, Fiorina C, et al. Impact of COVID-2019 outbreak on prevalence, clinical presentation and outcomes of ST-elevation myocardial infarction. J Cardiovasc Med. 2020;21(11):874–81.
Cummins NM, Garavan C, Barry LA, Devlin C, Corey G, Cummins F, et al. The impact of COVID-19 on an Irish Emergency Department (ED): a cross-sectional study exploring the factors influencing ED utilisation prior to and during the pandemic from the patient perspective. BMC Emerg Med. 2022;22(1):176.
Lucero A, Sokol K, Hyun J, Pan L, Labha J, Donn E, et al. Worsening of emergency department length of stay during the COVID‐19 pandemic. J Am Coll Emerg Physicians Open. 2021 [cited 2023 Jan 5];2(3). Available from: https://doi.org/10.1002/emp2.12489.
Kim YS, Kim IB, Kim SR, Cho BJ. Changes in emergency department case severity and length of stay before and after COVID-19 outbreak in Korea. Healthcare. 2022;10(8):1540.
Chew NWS, Ow ZGW, Teo VXY, Heng RRY, Ng CH, Lee CH, et al. The global effect of the COVID-19 pandemic on STEMI care: a systematic review and meta-analysis. Can J Cardiol. 2021;37(9):1450–9.
OECD. Ready for the Next Crisis? Investing in Health System Resilience. OECD; 2023 [cited 2023 Mar 1]. (OECD Health Policy Studies). Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/ready-for-the-next-crisis-investing-in-health-system-resilience_1e53cf80-en.
Sung HK, Paik JH, Lee YJ, Kang S. Impact of the COVID-19 outbreak on emergency care utilization in patients with acute myocardial infarction: a nationwide population-based study. J Korean Med Sci. 2021;36(16):e111.
Lee SY, Ro YS, Shin SD, Moon S. Epidemiologic trends in cancer-related emergency department utilization in Korea from 2015 to 2019. Sci Rep. 2021;11(1):21981.
Haklai Z, Mostovoy D, Gordon ES, Chaim J, Reichert A. The Israel National Hospital Discharge Register: an Essential Component of Data Driven Healthcare.
Developing international benchmarks of patient safety culture in hospital care: Findings of the OECD patient safety culture pilot data collection and considerations for future work. 2022 [cited 2023 Mar 1]. (OECD Health Working Papers; vol. 134). Report No.: 134. Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/developing-international-benchmarks-of-patient-safety-culture-in-hospital-care_95ae65a3-en.
Liu SA, Wu CL, Chou IJ, Wang PC, Hsu CL, Chen CP. The impacts of COVID-19 on healthcare quality in tertiary medical centers—a retrospective study on data from Taiwan clinical performance indicators system. Int J Environ Res Public Health. 2022;19(4):2278.
Cai X, Bi J, Zheng Z, Liu Y. Decision-making changes for patients and medical personnel in the management of acute appendicitis during the COVID-19 pandemic. BMC Emerg Med. 2022;22(1):170.
NHS England. Clinically led review of urgent and emergency care standards: measuring performance in a transformed system. [cited 2023 Jan 23]. Available from: https://www.england.nhs.uk/publication/clinically-led-review-of-urgent-and-emergency-care-standards-measuring-performance-in-a-transformed-system/.
V Carvalho AS, Broekema B, Brito Fernandes Ó, Klazinga N, Kringos D. Dataset_CarvalhoASV_ScopReviewAcuteCare.xlsx. Zenodo. 2023 [cited 2023 Mar 12]. Available from: https://doi.org/10.5281/zenodo.7726234.
Acknowledgements
The authors wish to thank Wichor Bramer and the team from the Erasmus MC Medical Library for developing and updating the search strategies used in this study.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to conceptualize the study. ASVC and BB performed the data collection. ASVC performed the data analysis, which was revised by BB. ASVC drafted the article. All authors provided feedback and contributed to revising the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist.
Additional file 2.
Search strategy.
Additional file 3.
Data Extraction Form.
Additional file 4.
List and characteristics of the studies included, from which indicators were extracted and collated.
Additional file 5.
Analysis of specific indicator trends by country, clinical entity, and/or diagnostic procedures.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
V. Carvalho, A.S., Broekema, B., Brito Fernandes, Ó. et al. Acute care pathway assessed through performance indicators during the COVID-19 pandemic in OECD countries (2020–2021): a scoping review. BMC Emerg Med 24, 19 (2024). https://doi.org/10.1186/s12873-024-00938-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-024-00938-7