Abstract
Background
Predicting the prognosis of primary percutaneous coronary intervention(PPCI) in ST-segment elevation myocardial infarction (STEMI) patients in the perioperative period is of great clinical significance. The inflammatory response during the perioperative period is also an important factor. This study aimed to investigate the dynamic changes in the systemic immune inflammatory index (SII) during the perioperative period of PPCI and evaluate its predictive value for in-hospital and out-of-hospital outcomes in patients with STEMI.
Methods
This retrospective study included 324 consecutive patients with STEMI who were admitted to the cardiac care unit. Blood samples were collected before PPCI, 12 h (T1), 24 h, 48 h after PPCI, the last time before hospital discharge (T2), and 1 month after hospital discharge. The SII was calculated as (neutrophils×platelets)/lymphocytes. Based on whether the primary endpoint occurred, we divided the patients into event and non-event groups. Univariate and multivariate logistic regression analyses were performed to identify independent risk factors that might influence the occurrence of the primary endpoint. Dynamic curves of SII were plotted, and receiver operating characteristic (ROC) curves were drawn for each node to calculate the optimal critical value, sensitivity, and specificity to assess their predictive ability for in-hospital and out-of-hospital courses. Kaplan-Meier curves were used to analyze the differences in survival rates at different SII inflammation levels.
Results
High levels of SII were individually related to the occurrence of the in-hospital period and long-term outcomes during the post-operative follow-up of STEMI patients (in-hospital SII: T1:OR 1.001,95%CI 1.001–1.001, P < 0.001; SII following hospital discharge: T1M: OR 1.008,95%CI 1.006–1.010, P < 0.001). Patients with high SII levels had lower survival rates than those with low SII levels. The analysis showed that the SII 12 h after (T1) and SII 1 month (T1M) had excellent predictive values for the occurrence of in-hospital and out-of-hospital outcomes, respectively (AUC:0.896, P < 0.001; AUC:0.892, P < 0.001).
Conclusion
There is a significant relationship between the dynamic status of SII and prognosis in patients with STEMI. This study found that the 12 h and SII 1 month affected in-hospital and out-of-hospital outcomes, respectively. Consequently, we focused on the dynamic changes in the SII.
Similar content being viewed by others
Background
Acute ST-segment elevation myocardial infarction (STEMI) is a severe form of coronary atherosclerosis. It is associated with several serious complications, poor prognosis, and high mortality. Primary percutaneous coronary intervention (PPCI) is the most effective reperfusion strategy for the treatment of acute STEMI and can significantly improve prognosis in patients with acute myocardial infarction. However, despite significant progress in revascularization, adverse cardiovascular events still occur during the perioperative period. The in-hospital mortality rate of patients with STEMI remains at 4–12% and the mortality in the first year is still 10% [1]. Therefore, predicting the prognosis of PPCI in patients with STEMI during the perioperative period is clinically significant.
As we all know, several factors influence the prognosis of PPCI in STEMI patients, such as the elderly, the history of hypertension and myocardial infarction, Killip classification, degree of coronary artery disease, etc. [2, 3]. The inflammatory reaction is involved in the pathological process of atherosclerosis and plays an important role in the onset, development, and progression of acute myocardial infarction and the emergence of complications. Inflammation and oxidative stress lead to plaque rupture and consequent atherosclerotic thrombosis, inducing the appearance of acute myocardial infarction symptoms and adverse cardiovascular events [4, 5]. The inflammatory response during the perioperative period is an important factor that has attracted increasing attention. Therefore, the inflammatory response status during the perioperative period in patients with STEMI warrants attention.
Inflammatory biomarkers such as leukocytes, adhesion molecules, and cytokines have been used to study the status of the inflammatory response. Several inflammatory marker ratios, such as the neutrophil/lymphocyte ratio (NLR), lymphocyte/monocyte ratio (LMR), and platelet/lymphocyte ratio (PLR), are associated with the presence and severity of coronary artery disease (CAD) and may predict future coronary events and mortality [6]. NLR is associated with the degree of patency of infarct-related arteries (IRA) before PCI, no reflow after PCI, and cardiac mortality in patients with acute STEMI [7]. PLR is an independent predictor of cardiovascular events and mortality in patients with STEMI [8].
Recently, a new marker of the inflammatory response, the Systemic Immune Inflammation Index (SII), derived from a combination of circulating neutrophils, platelets, and lymphocytes, which was initially useful as a predictor of clinical outcomes in oncology and other inflammatory diseases [9, 10], has now been investigated in cardiovascular diseases. The SII has been shown to be a potential predictor of major cardiovascular and cerebrovascular events and all-cause mortality after PCI in elderly patients of acute myocardial infarction (AMI) [11] and has been associated with the development of contrast nephropathy [12] and the emergence of the no-reflow phenomenon in patients with AMI [13]. Compared to NLR and PLR, SII represents three important immune response pathways, namely the inflammatory response, thrombosis, and stress response, which can reflect the state of the patient’s condition more comprehensively and therefore can be considered a more sensitive indicator of the inflammatory response in the body.
However, the prognostic value in previous studies is limited by the fact that they collected SII levels at baseline as a single item, reflecting only the immediate inflammatory status of patients on admission. The inflammatory response is a dynamic process during the perioperative period of PPCI in patients with STEMI, and a single item alone does not truly reflect the inflammatory process in patients. Serial changes in the SII must be observed. Therefore, we sought to determine whether dynamic changes in the SII during the perioperative period of PPCI in patients with STEMI were related to the development of intra- and extra-hospital cardiovascular outcomes.
Methods
Study population
In the Affiliated Hospital of Xuzhou Medical University between 2019.01.01 and 2021.12.31, 713 patients with acute STEMI in the cardiac care unit were evaluated. Finally, 324 patients met the inclusion criteria (Fig. 1). The study was approved by the hospital ethics committee (XYFY2022-KL420–01).
The collection of clinical data included general and laboratory data.
General data included gender, age, previous history of hypertension, diabetes, stroke/TIA, myocardial infarction /PCI/CABG, coronary artery disease, heart failure, smoking, and alcohol consumption; medications during hospitalization (aspirin, clopidogrel/Ticagrelor, CCB, statins, β-blockers, ACEI/ARB, diuretics), systolic and diastolic blood pressure on admission, heart rate on admission, and Killip classification. The data collected during PPCI included main diseased vessels (left coronary artery, left anterior descending coronary artery, left circumflex coronary artery, and right coronary artery), the total length of the implanted stent, the average diameter of the implanted stent, the number of implanted stents, type of PCI, IVUS assist, TIMI after PPCI, site of AMI, medications discharge (aspirin, P2Y12 receptor inhibitors, diuretics, statins, beta-blockers, ACEI/ARB, insulin), and Chest pain period (h), Pain-to-balloon time (h), Door-to-balloon time (h), hospitalization day, etc.
Laboratory data included hemoglobin, glycated hemoglobin, fasting glucose, glomerular filtration rate, serum creatinine, serum uric acid, AST, ALT, albumin, Troponin T, N-terminal pro-brain natriuretic peptide (NT-proBNP) on admission, monitor blood lipids, including low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), triglycerides, total cholesterol, lipoprotein-a (Lp(a)) on admission, white blood cell count, neutrophil count, monocyte count, lymphocyte count, platelet count, high-sensitivity C-reactive protein level (hs-CRP), cTnImax and CK-MBmax, etc.
Inclusion criteria: Primary percutaneous coronary intervention performed within 12 hours of symptom onset according to the 2017 STEMI treatment guidelines [14].
Exclusion criteria: (1) Thrombolysis before PPCI, (2) Chronic dependent renal replacement therapy, (3) Glomerular filtration rate (eGFR) < 15 ml/(min*1.73 m2) or severe hepatic insufficiency, (4) Primary hematologic disease or active malignancy, (5) Inflammation (febrile disease, autoimmune disease, acute or chronic inflammatory disease, or recent history of infection), (6) Treatment with chronic steroids or NSAIDs, history of organ transplantation, (7) Including a history of allergy to contrast medium, P2Y12 receptor inhibitors, angiotensin-converting enzyme inhibitors (ACEI), angiotensin II receptor blockers (ARB), aspirin, statins, beta-blockers, etc., (8) Thyroid function disease, heart valve disease, etc. (9) Pregnant or lactating patients.
Definitions and endpoints
Definition of STEMI: (1) when typical chest pain lasts more than 30 minutes, (2) ST-segment elevations at least at two consecutive leads (V2-V3 at least 0.2 mV for men; 0.15 mV for women and/or 0.1 mV for other leads). (3) Apparent or probable new-onset left bundle branch block; (4) V3R - V4R and V7–V9 leads with an elevation in the ST-segment obtained [1].
Hypertension: Systolic blood pressure > 140 mmHg and/or diastolic blood pressure > 90 mmHg on at least two measurements, or the use of any anti-hypertensive medication [15].
Diabetes mellitus: Fasting plasma glucose level > 7 mmol/L or > 11.1 mmol/L on any measurement, any anti-diabetic drug use, or HbA1c ≥6.5% [15].
Hyperlipidemia: Total cholesterol > 5.2 mmol/L, low-density lipoprotein cholesterol (LDL-C) > 3.4 mmol/L, triglyceride > 1.7 mmol/L, or anti-lipid treatment [15].
Smokers: Currently smoked or quit smoking within the last year [15].
Drinkers: Currently drink or quit drinking within the last year [15].
Follow-up Period: Clinical data of the patients during hospitalization and by review at the clinic or telephone follow-up discharge. The follow-up period at discharge was 12 months.
The main endpoints were as follows.
The hospitalization outcomes included cardiogenic shock, acute respiratory failure, acute renal injury, ventricular arrhythmia, recurrent infarction, vascular reconstruction (PCI/CABG), and all-cause death.
The cardiovascular outcomes (12 months follow-up) included all-cause death, recurrent infarction, revascularization (PCI/CABG), and ventricular arrhythmia.
Before administering any medication, an anterior venous blood sample was drawn from the elbow of each patient in the emergency department on admission. Complete blood counts, including platelet, total leukocyte, neutrophil, and lymphocyte counts, were collected using a full blood count analyzer (Sysmex XT-1800, Sysmex Corporation). Biochemical parameters, such as blood urea nitrogen (BUN), serum creatinine, uric acid, lipid profile, and cardiac enzyme levels, were obtained in our central laboratory using an auto-analyzer (Hitachi 747, Tokyo, Japan).
Peripheral blood was collected from STEMI patients who met the inclusion criteria before PPCI (T0), within 12 h after (T1), within 24 h after (T24), within 48 h after (T48), within the last time before hospital discharge (T2), and 1 month after hospital discharge (T1M), respectively, and SII levels were calculated.
The SII was calculated as total peripheral platelet count (P) × (neutrophil count/lymphocyte ratio) NLR (N/L) (SII = P × N/L ratio).
All patients included in this study were administered 300 mg chewable preoperative aspirin, ticagrelor 180 mg orally, and unfractionated heparin 70–100 U/kg IV. PCI was performed by experienced physicians qualified for coronary intervention. Primary PCI was performed using a standard radial approach with a 6 or 7 French catheter. The stent type (bare metal or drug-eluting stent) and thrombus aspiration were determined by the operator. Glycoprotein IIb/IIIa receptor inhibitors were selected by the operator and were administered during PCI by intra-coronary push of 10 μg/kg followed by an intravenous infusion of 0.15 μg/kg/min. If necessary, balloon dilatation was performed to ensure stent appositioning. The coronary artery lesions were treated using standard PCI techniques. The standard Judkins technique (Expo; Boston Scientific Corporation, Natick, Massachusetts, USA) and Siemens Axiom Sensis XP device (Munich, Germany) were used for selective coronary angiography. An iopromide contrast agent (Ultravist-370 Schering AG, Berlin, Germany) was used. Medications taken by the patients during hospitalization and after hospital discharge were in accordance with the guidelines of the European Society of Cardiology.
Statistics and analysis
Baseline characteristics of the patients were categorized according to the occurrence of the primary endpoint. The Kolmogorov-Smirnov test was used to test for normality. The measured normal data were expressed as mean ± standard deviation (x ± s), and the differences between groups were compared with a t-test. The measurement deviation data are expressed as median (interquartile distance), and the M-U test was used to compare the differences between groups. Numerical data are presented as numbers and percentages, and intergroup comparisons were assessed using the chi-square test and Fisher’s exact test. Univariate and multivariate analyses were performed using logistic regression models to analyze risk factors that may influence the occurrence of the primary endpoint. Receiver operating characteristic (ROC) curves were used to assess the ability of the SII to predict in-hospital and out-of-hospital outcomes after PPCI in patients with STEMI. Survival conditions in the two groups were compared using Kaplan-Meier analysis. The overall survival rate from the date of diagnosis to the date of death or last follow-up was calculated to analyze whether high SII levels correlated with the occurrence of the primary endpoints. The log-rank test was used to analyze differences between groups. P < 0.05 was considered as a statistically significant difference at the α = 0.05 test level, and the confidence interval (CI) for all hazard ratios was 95%. SPSS 26.0 statistical analysis software, GraphPad Prism (version 7.0) was used for the statistical analysis.
Results
General information data
This study included 324 patients with STMEI who underwent PPCI. The patients were divided into event and non-event groups based on the results of follow-up during hospitalization and 12 months after hospital discharge. The clinical and laboratory data were compared between the two groups.
Tables 1 and 2 summarize the demographic and laboratory data and previous treatment information for all patients. Event and non-event groups were divided according to the presence or absence of out-of-hospital outcomes after hospital discharge. The degree of multiple vascular lesions > 50%, number of implanted stents, IVUS-assisted application of P2Y12 receptor inhibitors, LDL-C, NT-proBNP, hs-CRPmax, and six groups of SII levels were statistically significant in the event group compared to the non-event group (P < 0.05).
Tables 3 and 4 summarize the demographic and laboratory data and previous treatment information for all patients. Event and non-event groups were divided based on the presence or absence of in-hospital outcomes. Compared with the non-event group, the chest pain period (h), pain-to-balloon time (h), Killip classification, stent length, glucose, cTnImax, hs-CRPmax and the five groups of SII levels were statistically significant in the event group. (P < 0.05).
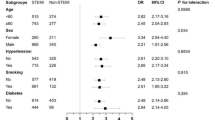
In the multivariable logistic regression model, IVUS assistance, LDL-C level, and SII at 1 month (T1M)(OR: 0.05, 1,95%, CI: 0.010–0.251, P < 0.001; OR: 1.890, 95%, CI: 1.214–2.941, P = 0.005; OR: 1.008, 95%, CI: 1.006–1.010, P < 0.001), predict the out-of-hospital outcomes, respectively (Table 5). Additionally, SII 12 h after (T1), cTnImax, and hs-CRPmax (OR: 1.001, 95%, CI: 1.001–1.001, P < 0.001; OR: 1.075, 95%, CI: 1.008–1.148, P = 0.029; OR: 1.008, 95%, CI: 1.002–1.015, P = 0.012) respectively, were independently associated with in-hospital outcomes (Table 6).
The overall levels of change in blood SII and hs-CRP levels at different onset times
The time profile showed that the SII started to rise before PPCI (T0), peaked at 12 h after PPCI, and then gradually decreased to a valley level 1 month after discharge. The hs-CRP level started to rise before PPCI (T0), gradually increased to a peak at 48 h after PPCI, and then rapidly decreased. In addition, we saw that the time of SIImax level appeared earlier than hs-CRPmax (Fig. 2(a), (b)).
Predictive value of ROC curve analysis of SII levels, hs-CRPmax, cTnImax, CK-MBmax for the occurrence of outcomes both hospitalization and discharge after PPCI in STEMI patients
To predict in-hospital and out-of-hospital outcomes, receiver operating characteristic (ROC) curves of six groups of SII, hs-CRPmax, cTnImax, and CK-MBmax were plotted (Fig. 3(a), (b)). The optimal critical values, sensitivities, and specificities were calculated (Tables 7 and 8). In-hospital ROC analysis illustrated that the best cutoff value of the SII (T1) to predict outcomes during hospitalization was 1915.77 with 89.70% sensitivity and 81.40% specificity (AUC:0.896; 95%, CI: 0.852–0.941; P < 0.001). The discriminative value of SII 12 h after PPCI was higher than that of the others. Out-of-hospital ROC analysis indicated that the best cut-off value of the SII 1 month, to predict the outcomes of discharge was 696.43 with 76.70% sensitivity and 88.00% specificity (AUC: 0.892; 95%, CI: 0.846–0.937; P < 0.001). The discriminative value of the SII at 1 month after discharge was the highest.
a Receiver-operating characteristic (ROC) curve analyses of five groups of SII, hs-CRPmax, cTnImax, CK-MBmax for predicting in-hospital outcomes in STEMI patients. b. Receiver-operating characteristic (ROC) curve analyses of six groups of SII, hs-CRPmax, cTnImax, CK-MBmax for predicting out-of hospital outcomes in STEMI patients
Correlation of high and low SII level groups with cumulative all-cause mortality in STEMI patients after PPCI
There was the occurrence of in-hospital and out-of-hospital outcomes (Tables 9, 10). Kaplan-Meier curves were used to analyze the differences in survival rates at different SII inflammation levels according to T1, T2, and T1M during hospitalization and after hospital discharge (Fig. 4 (a)–(d)).
a Kaplan-Meier Survival Curves for All-cause Mortality during hospitalization according to SII 12 h after PPCI(T1). b Kaplan-Meier Survival Curves for All-cause Mortality during hospitalization according to SII before hospital discharge(T2). c. Kaplan-Meier Survival Curves for All-cause Mortality after hospital discharge according to SII 1 month after discharge(T1M). d. Kaplan-Meier Survival Curves for All-cause Mortality after hospital discharge according to SII before hospital discharge(T2)
Kaplan-Meier survival curves for all-cause mortality during hospitalization according to SII 12 h after PPCI (T1) and SII before hospital discharge (T2)
The upper panel shows patients with a critical SII (T1) below or above 1915.77. The lower figure showed 779.79 at T2 (h). SII value <cutoff (blue curve), values ≥cutoffs (red curve). The functions in T1 (P = 0.0017) and T2 (P = 0.0354) showed that patients with an SII value below (blue curve) had a significantly higher cumulative survival than patients with an SII cutoff value above (red curve) (Fig. 4 (a), (b)).
Kaplan-Meier survival curves for all-cause mortality discharge according to SII 1 month after discharge and SII before discharge(T2)
The upper panel showed patients with a critical SII value (T1M) below or above 696.43. The lower panel showed 735.32 at T2. SII value <cut-off (blue curve), values ≥cutoffs (red curve). The SII-value (SII 1 month after) (P = 0.0025) and T2 (P = 0.0124) showed that patients with an SII value below (blue curve) had significantly higher cumulative survival than those with SII cut-off values above (red curve) (Fig. 4 (c), (d)).
Discussion
This retrospective analysis found that the SII, a novel inflammatory marker, was associated with the occurrence of hospitalization and discharge outcomes in patients with acute STEMI after PPCI. Between the event and non-event groups, SII levels responded differently to high and low inflammatory statuses, which had an impact on prognosis. Patients with a highly inflammatory state have a relatively poor prognosis.
Inflammation plays a key role in the development of atherosclerosis, acute myocardial infarction, and poor prognosis after myocardial infarction. Plaque rupture triggers an inflammatory response, which releases highly thrombogenic components and promotes thrombus formation [16]. In the acute phase of myocardial infarction, the inflammatory response becomes significant with acute exacerbation, and the higher the degree of inflammation, the larger the area of myocardial ischemic necrosis. The COLCOT trial showed that the use of low-dose colchicine within 3 days after myocardial infarction (MI) reduced the occurrence of ischemic cardiovascular events. Patients can benefit from the early in-hospital use of colchicine after MI [17]. This suggests that the occurrence of MI is associated with inflammatory involvement and that early suppression of inflammation after MI provides even greater benefits.
Leukocytes and their subtypes, such as neutrophils, monocytes, lymphocytes, and platelets, are important inflammatory cells in the circulation and have been shown in several studies to be associated with the prognosis of patients with acute MI. Leukocyte count is an independent predictor of AM I[18], and elevated leukocyte levels are associated with increased mortality in patients with STEMI [19]. During inflammation, pre-stimulated neutrophils infiltrating the vessel wall release reactive oxygen species, cytokines, and myeloperoxidases that damage the vascular endothelium to promote inflammation progression. Elevated neutrophil counts are associated with a high risk of ischemic events [20] and AMI mortality [21]. In the inflammatory state of AMI, cortisol levels are elevated and lymphocytes are affected by cortisol levels, resulting in decreased lymphocyte levels [22]. Lymphocytopenia was independently associated with mechanical complications and mortality in patients with acute STEMI [23]. Monocytes, a basic component of the immune system, are considered to be predictors of coronary events [24], and an increase in their number has been shown to correlate with the prognosis of AMI [25]. Platelets play a role in inflammatory and immune responses through the release of pro-inflammatory cytokines and interactions with endothelial cells, leukocytes, and smooth muscle cells [26, 27] and are significantly associated with inflammation and atherothrombosis [28].
Monitoring several inflammatory markers in peripheral blood has been proposed to assess cardiovascular risk in patients with acute myocardial infarction. Markers such as the NLR, PLR, and LMR have been introduced as new markers. High NLR was significantly associated with cardiovascular and all-cause mortality in patients with ST-segment elevation myocardial infarction during hospitalization or in the long term [29, 30]. Low LMR correlates with poor outcomes in patients [31]. PLR is associated with long-term mortality in STEMI patients [32]. Recently, Hu et al. developed an innovative predictive marker called the SII based on a prospective cohort study [33]. SII is a novel inflammatory parameter calculated as (N × P)/L (N, P, and L represent the neutrophil count, platelet count, and lymphocyte count, respectively) and represents three important immune response pathways: inflammatory response, thrombosis, and organismal stress response. It is a prognostic indicator of poor outcomes in various types [34, 35]. Its study in cardiovascular disease has also been conducted. SII has been found to predict clinical outcomes in patients with coronary artery disease [36]. Su et al. [37] demonstrated that a high SII was independently associated with all-cause mortality at 30 days, 90 days, and 1 year in patients with acute coronary syndrome. Öcal et al. [15] demonstrated that the SII was independently associated with all-cause mortality and adverse cardiovascular events during hospitalization and at 3-year follow-up after PPCI in patients with acute STEMI. Additionally, other studies have shown that the SII may indicate short- and long-term mortality in patients with heart failure (HF) with reduced ejection fraction (HFrEF) and acute type A aortic dissection (ATAD) undergoing surgery and with infective endocarditis [38,39,40]. SII can also be used as an independent predictor of NOAF following STEMI [41]. All these studies used a single SII level at baseline and illustrated that higher SII levels were associated with a poorer prognosis.
Our study differs from the above studies in that we assessed the process of dynamic changes in SII levels. The process of inflammatory activity is dynamic. During the intraoperative and postoperative periods, the stent, as a foreign object, stimulates endothelial cells and increases inflammatory radical responses, which may manifest as an increase in inflammatory indices. During hospitalization and after hospital discharge, the patients were treated with appropriate antiplatelet and lipid-regulating drugs, which also affected the inflammatory process. Therefore, dynamic changes in SII levels can better reflect the overall situation than a single SII level. In our study, we attempted to determine whether dynamic changes in the SII were related to in-hospital and out-of-hospital outcomes in patients with STEMI undergoing PPCI. This study analyzed the relationship between serial changes in the SII during the perioperative period of PPCI and the occurrence of the primary endpoint. The results showed that high SII levels were independently associated with the primary endpoint during the postoperative follow-up period of patients (P < 0.05). In contrast, patients with high SII had lower survival rates than those with low SII. By dynamically analyzing SII levels in six groups, hs-CRPmax, cTnImax, cTnImax, CK-MBmax, and constructing ROC curves at each node, the analysis showed that the SII 12 h after PPCI (T1) and 1 month after hospital discharge (T1M) had excellent predictive value for the occurrence of in-hospital and out-of-hospital outcomes. This can be attributed to two reasons. First, inflammation may be closely related to the prognosis of in-hospital outcomes in patients with STEMI due to the intense inflammatory response during the AMI phase. Second, 1 month after hospital discharge, most patients benefited from the appropriate use of antiplatelet and lipid-regulating drugs, which can improve the local inflammatory state of the myocardium, while a small number of patients still had local myocardial inflammation, thus leading to different prognoses. This inspired us to focus on peak SII levels during hospitalization. When the peak in-hospital SII was > 1915.77, timely intervention was required to effectively reduce in-hospital outcomes. Meanwhile, focusing on the lowest level of the SII at 1 month after hospital discharge and maintaining it below 696.43 can effectively reduce the occurrence of out-of-hospital outcomes. Thus, this study provides guidance for improving patient prognosis.
However, as there are few studies on the correlation between dynamic changes in SII levels during the perioperative period of PPCI and primary endpoint occurrence in patients with STEMI, several limitations were present: 1. This was a single-center, retrospective study with a small sample size. These conclusions may have been affected by a selection bias. 2. Other conventional factors that respond to the inflammatory status, such as calcitonin, IL-6, and myeloperoxidase, were not included in this study. 3. Although independent risk factors were identified by multivariate regression, some undefined factors remained, which affected the study results. We believe that future prospective multicenter studies with large sample sizes could confirm the inflammatory status to meet the control standard and thus reduce major cardiovascular events, similar to the application of lipid-regulating medications to lower lipid levels and bring lipids into general standards.
Conclusion
This study obtained important prognostic information from the normal blood tests of patients with STEMI who underwent PPCI. This study showed that dynamic changes in the SII in patients with STEMI during the perioperative period of PPCI were correlated with the occurrence of in-hospital and out-of-hospital outcomes. SII is a simple and practical indicator for identifying high-risk patients after PPCI. Based on the trend of serial changes in SII levels, preventive measures can be taken in patients with high inflammatory status to reduce the occurrence of cardiovascular events.
Availability of data and materials
Raw data supporting the conclusions of this article were provided by the author (AL) without unnecessary reservations. Additional information on this article had been added to the attachment.
References
Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77.
Morrow DA, Antman EM, Charlesworth A, et al. TIMI risk score for ST-elevation myocardial infarction: a convenient, bedside, clinical score for risk assessment at presentation: an intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation. 2000;102(17):2031–7.
Fox KA, Dabbous OH, Goldberg RJ, et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE). Bmj. 2006;333(7578):1091.
Libby P, Ridker PM, Hansson GK. Inflammation in atherosclerosis: from pathophysiology to practice. J Am Coll Cardiol. 2009;54(23):2129–38.
Zhang DP, Mao XF, Wu TT, et al. The fibrinogen-to-albumin ratio is associated with outcomes in patients with coronary artery disease who underwent percutaneous coronary intervention. Clin Appl Thromb Hemost. 2020;26:1076029620933008.
Guclu K, Celik M. Prognostic value of inflammation parameters in patients with non-ST elevation acute coronary syndromes. Angiology. 2020;71(9):825–30.
Akpek M, Kaya MG, Lam YY, et al. Relation of neutrophil/lymphocyte ratio to coronary flow to in-hospital major adverse cardiac events in patients with ST-elevated myocardial infarction undergoing primary coronary intervention. Am J Cardiol. 2012;110(5):621–7.
Toprak C, Tabakci MM, Simsek Z, et al. Platelet/lymphocyte ratio was associated with impaired myocardial perfusion and both in-hospital and long-term adverse outcome in patients with ST-segment elevation acute myocardial infarction undergoing primary coronary intervention. Postepy Kardiol Interwencyjnej. 2015;11(4):288–97.
Jomrich G, Gruber ES, Winkler D, et al. Systemic immune-inflammation index (SII) predicts poor survival in pancreatic Cancer patients undergoing resection. J Gastrointest Surg. 2020;24(3):610–8.
Zhou ZQ, Pang S, Yu XC, et al. Predictive values of postoperative and dynamic changes of inflammation indexes in survival of patients with resected colorectal Cancer. Curr Med Sci. 2018;38(5):798–808.
Huang J, Zhang Q, Wang R, et al. Systemic immune-inflammatory index predicts clinical outcomes for elderly patients with acute myocardial infarction receiving percutaneous coronary intervention. Med Sci Monit. 2019;25:9690–701.
Bağcı A, Aksoy F, Baş HA. Systemic immune-inflammation index may predict the development of contrast-induced nephropathy in patients with ST-segment elevation myocardial infarction. Angiology. 2022;73(3):218–24.
Esenboğa K, Kurtul A, Yamantürk YY, Tan TS, Tutar DE. Systemic immune-inflammation index predicts no-reflow phenomenon after primary percutaneous coronary intervention. Acta Cardiol. 2022;77(1):59–65.
Thiele H, Desch S, de Waha S. Acute myocardial infarction in patients with ST-segment elevation myocardial infarction : ESC guidelines 2017. Herz. 2017;42(8):728–38.
Öcal L, Keskin M, Cerşit S, et al. Systemic immune-inflammation index predicts in-hospital and long-term outcomes in patients with ST-segment elevation myocardial infarction. Coron Artery Dis. 2022;33(4):251–60.
Zhou J, Chen R, Liu C, et al. Associations of NETs with inflammatory risk and atherosclerotic severity in ST-segment elevation myocardial infarction. Thromb Res. 2021;203:5–11.
Bouabdallaoui N, Tardif JC, Waters DD, et al. Time-to-treatment initiation of colchicine and cardiovascular outcomes after myocardial infarction in the colchicine cardiovascular outcomes trial (COLCOT). Eur Heart J. 2020;41(42):4092–9.
Ates AH, Canpolat U, Yorgun H, et al. Total white blood cell count is associated with the presence, severity and extent of coronary atherosclerosis detected by dual-source multislice computed tomographic coronary angiography. Cardiol J. 2011;18(4):371–7.
Chung S, Song YB, Hahn JY, et al. Impact of white blood cell count on myocardial salvage, infarct size, and clinical outcomes in patients undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a magnetic resonance imaging study. Int J Card Imaging. 2014;30(1):129–36.
Horne BD, Anderson JL, John JM, et al. Which white blood cell subtypes predict increased cardiovascular risk? J Am Coll Cardiol. 2005;45(10):1638–43.
óH B, Bosch JA, Thomas GN, et al. Which leukocyte subsets predict cardiovascular mortality? From the LUdwigshafen RIsk and cardiovascular health (LURIC) study. Atherosclerosis. 2012;224(1):161–9.
Thomson SP, McMahon LJ, Nugent CA. Endogenous cortisol: a regulator of the number of lymphocytes in peripheral blood. Clin Immunol Immunopathol. 1980;17(4):506–14.
Dragu R, Huri S, Zukermann R, et al. Predictive value of white blood cell subtypes for long-term outcome following myocardial infarction. Atherosclerosis. 2008;196(1):405–12.
Olivares R, Ducimetière P, Claude JR. Monocyte count: a risk factor for coronary heart disease? Am J Epidemiol. 1993;137(1):49–53.
Balta S, Celik T, Ozturk C, et al. The relation between monocyte to HDL ratio and no-reflow phenomenon in the patients with acute ST-segment elevation myocardial infarction. Am J Emerg Med. 2016;34(8):1542–7.
von Hundelshausen P, Weber C. Platelets as immune cells: bridging inflammation and cardiovascular disease. Circ Res. 2007;100(1):27–40.
Ueno K, Nomura Y, Morita Y, Eguchi T, Masuda K, Kawano Y. Circulating platelet-neutrophil aggregates play a significant role in Kawasaki disease. Circ J. 2015;79(6):1349–56.
Akhtar T, Bandyopadhyay D, Ghosh RK, Aronow WS, Lavie CJ, Yadav N. Advances in the pharmacogenomics of antiplatelet therapy. Am J Ther. 2020;27(5):e477–e84.
Shen XH, Chen Q, Shi Y, Li HW. Association of neutrophil/lymphocyte ratio with long-term mortality after ST elevation myocardial infarction treated with primary percutaneous coronary intervention. Chin Med J. 2010;123(23):3438–43.
Gazi E, Bayram B, Gazi S, et al. Prognostic value of the neutrophil-lymphocyte ratio in patients with ST-elevated acute myocardial infarction. Clin Appl Thromb Hemost. 2015;21(2):155–9.
Kiris T, Çelik A, Variş E, et al. Association of Lymphocyte-to-Monocyte Ratio with the mortality in patients with ST-elevation myocardial infarction who underwent primary percutaneous coronary intervention. Angiology. 2017;68(8):707–15.
Temiz A, Gazi E, Güngör Ö, et al. Platelet/lymphocyte ratio and risk of in-hospital mortality in patients with ST-elevated myocardial infarction. Med Sci Monit. 2014;20:660–5.
Hu B, Yang XR, Xu Y, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20(23):6212–22.
Ji Y, Wang H. Prognostic prediction of systemic immune-inflammation index for patients with gynecological and breast cancers: a meta-analysis. World J Surg Oncol. 2020;18(1):197.
Huang Y, Gao Y, Wu Y, Lin H. Prognostic value of systemic immune-inflammation index in patients with urologic cancers: a meta-analysis. Cancer Cell Int. 2020;20:499.
Yang YL, Wu CH, Hsu PF, et al. Systemic immune-inflammation index (SII) predicted clinical outcome in patients with coronary artery disease. Eur J Clin Investig. 2020;50(5):e13230.
Su G, Zhang Y, Xiao R, Zhang T, Gong B. Systemic immune-inflammation index as a promising predictor of mortality in patients with acute coronary syndrome: a real-world study. J Int Med Res. 2021;49(5):3000605211016274.
Hayıroğlu M, Çınar T, Çinier G, et al. Evaluating systemic immune-inflammation index in patients with implantable cardioverter defibrillator for heart failure with reduced ejection fraction. Pacing Clin Electrophysiol. 2022;45(2):188–95.
Xu H, Li Y, Wang H, et al. Systemic immune-inflammation index predicted short-term outcomes in ATAD patients undergoing surgery. J Card Surg. 2022;37(4):969–75.
Agus HZ, Kahraman S, Arslan C, et al. Systemic immune-inflammation index predicts mortality in infective endocarditis. J Saudi Heart Assoc. 2020;32(1):58–64.
Bağcı A, Aksoy F. Systemic immune-inflammation index predicts new-onset atrial fibrillation after ST elevation myocardial infarction. Biomark Med. 2021;15(10):731–9.
Acknowledgements
Not applicable
Funding
This study was funded by Defeng Pan’s Applied Basic Research Project of Xuzhou.
Author information
Authors and Affiliations
Contributions
AL contributed to the conception and design of the study. NS, FG collected the clinical information. AL analyzed the data and made a draft of the manuscript. NS and FG and XW made a part of the manuscript and provided advice for the analysis. DP guided the analysis and made substantial improvements to the paper. HZ supervised the study and contributed to the data analysis program. AL and NS contributed equally to this work. All authors have read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Research on human participants had been reviewed and approved by the Affiliated Hospital of Xuzhou Medical University. This study has been approved by the Ethics Committee of Affiliated Hospital of Xuzhou Medical University (XYFY2022-KL420–01). No written informed consent was required for participation in this study, the informed consent has been exempted from the Ethics Committee of Affiliated Hospital of Xuzhou Medical University. All methods are carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, A., Sun, N., Gao, F. et al. The prognostic value of dynamic changes in SII for the patients with STEMI undergoing PPCI. BMC Cardiovasc Disord 24, 67 (2024). https://doi.org/10.1186/s12872-023-03679-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03679-w