Abstract
Background
Fractional Flow Reserve (FFR) is the gold standard for the functional evaluation of coronary arteries, which is effective in selecting patients for revascularization, avoiding unnecessary procedures, and reducing treatment costs. However, its use is limited due to invasiveness, high cost, and complexity. Therefore, the non-invasive estimation of FFR using artificial intelligence (AI) methods is crucial.
Objective
This study aimed to identify the AI techniques used for FFR estimation and to explore the features of the studies that applied AI techniques in FFR estimation.
Methods
The present systematic review was conducted by searching five databases, PubMed, Scopus, Web of Science, IEEE, and Science Direct, based on the search strategy of each database.
Results
Five hundred seventy-three articles were extracted, and by applying the inclusion and exclusion criteria, twenty-five were finally selected for review. The findings revealed that AI methods, including Machine Learning (ML) and Deep Learning (DL), have been used to estimate the FFR.
Conclusion
This study shows that AI methods can be used non-invasively to estimate FFR, which can help physicians diagnose and treat coronary artery occlusion and provide significant clinical performance for patients.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Cardiovascular Diseases (CVD) are the most crucial cause of death worldwide [1]. These diseases have been among the most critical concerns in the last few decades [2], so approximately 18.5 million people died due to CVDs in 2019. Expectedly, the death rate due to this disease will increase by the year 2030 to reach 23.6 million [3]. Coronary Artery Disease (CAD) is the most common CVD, affecting more than twenty million adults in the United States and accounting for approximately one-third of deaths [4]. In this disease, plaque accumulation causes narrowing of the coronary arteries [5, 6], which can be partial or in the form of complete blockage of the coronary arteries and causes disruption of blood supply to the heart tissue [7]. Coronary artery narrowing or blockage leads to severe symptoms such as angina pectoris and even myocardial ischemia [8].
Based on the evidence, the functional severity of coronary artery stenosis is the leading cause of myocardial ischemia [9, 10]. Physiological evaluation is a determining factor for patients with CAD treatment decisions [11]. The Fractional Flow Reserve (FFR) method is used in the physiological evaluation. This method uses a pressure wire passing through the stenosis to measure the flow and blood pressure before and after the stenosis after injecting an agent such as adenosine [12].
FFR is the gold standard for the functional assessment of coronary arteries. Many pieces of evidence show that revascularization should be performed based on the functional assessment of the vessels [13,14,15,16,17,18]. Based on considerable clinical evidence, using FFR helps select the appropriate patients and lesions for treatment, avoids unnecessary procedures, reduces medical costs, and improves clinical outcomes [12]. However, despite the recommendations of treatment guidelines, the use of FFR for diagnosing CAD is minimal due to its complexity, high cost, and invasiveness [19]. Therefore, non-invasive methods of estimating FFR are of great interest.
In the last three decades, Artificial Intelligence (AI) has been widely used to improve the accuracy of diagnostic methods and decision-making based on CVD datasets [20]. As a subfield of AI, Machine Learning (ML) describes algorithms that analyze data logically, similar to how humans conclude [21]. Recently, AI techniques have been used to estimate FFR using Computed Tomography Angiography (CTA), X-ray Coronary Angiography (XCA), Optical Coherence Tomography (OCT), and Intravascular Ultrasound (IVUS) images. These methods have been highly regarded due to their non-invasive nature. To our knowledge, there has not been systematic studies reviewing the AI techniques in FFR estimation. Knowing that the AI techniques present different performance depending on the type of technques, type of features, and validadtion approaches, we aimed to to obtaing a better understanding of AI techniques in FFR estimation through findings answers to the following questions:
-
1.
What AI methods have been used to estimate the FFR?
-
2.
What imaging tools have been used to estimate the FFR?
-
3.
How do AI techniques estimate the FFR?
Methods
Review methodology
Search strategy
The Preferred Reporting Items for Systematic Reviews and Metanalysis (PRISMA) [22] have been followed to perform this systematic review. The basic search string was ((“Deep Learning”) OR (“Machine Learning”) OR (“Artificial Intelligence”) OR (“Neural Network”) AND ((Fractional Flow Reserve)), and searches were performed without date constraint using IEEE Digital Library, Web of Science, PubMed, ScienceDirect, and Scopus databases. The search string syntax was adapted depending on the database requirements. The search was performed on the title, abstract, and keywords. Previously identified articles were also included in the process.
Eligibility criteria
This study analyzed only original articles published in English designed and developed AI methods to estimate the FFR.
Study selection
In the screening stage, three authors reviewed the articles based on their titles and abstract and removed the irrelevant articles. In the next step, the full text of the selected articles was evaluated by two researchers separately based on inclusion/exclusion criteria. Disagreements were resolved with the help of the third author through consensus and brainstorming.
Data extraction
In the data extraction stage, the type of imaging tool, number of patients, number and type of lesion, AI method, problem type, features used, feature extraction method, segmentation type, and model efficiency were extracted. The name of the first author, year, and place of publication of the article were also extracted. Finally, the obtained results were displayed in the form of structured tables (Table 1).
Critical review and quality assessment
The quality of studies was examined by two authors F.A and R.R, and disagreements were resolved by a third reviewer A.H. The quality of included studies was assessed based on the Quality Assessment for Diagnostic Accuracy Studies (QUADAS-2) tool to assess the risk of bias and applicability of primary diagnostic accuracy studies. This tool categorizes the risk of bias for individual studies as “low,” “medium,” or “high” [23].
Results
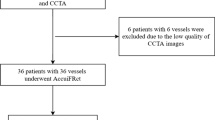
The present study surveyed the title and abstracts of 384 articles. The full text of 107 articles was carefully examined, and eighty-two articles were excluded for reasons such as lack of full text, use of methods other than AI, conference articles, articles other than English, and articles with unclear results, and twenty-five articles were included in the study (Fig. 1).
The overall quality of most included studies was high. The subject selection method and follow and timing may have introduced high bias and applicability concerns in the reviewed studies.
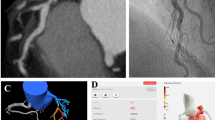
This study demonstrated that various imaging tools have been used, including CCTA [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40], OCT [41,42,43], XCA [44], and IVUS [45]. Several studies used a combination of CCTA with OCT [46], IVUS [47], and XCA [48], and a study combined IVUS and XCA [49] to estimate the FFR. Most of the studies used CCTA to estimate the FFR. AI methods used include methods based on DL [25, 27,28,29, 34, 40, 41, 48] and ML [26, 42, 30, 32, 33, 37, 39, 44, 46, 49]. Some studies have used a combination of DL and ML techniques [24, 32, 37, 38, 45, 47].
In addition to the features extracted from the images, other features such as morphological, flow, biometric, clinical, radiomic, and centerline information have been used to estimate the FFR.
The extraction of parameters from imaging tools has been done manually, automatically, and in some cases with semi-automatic methods. Additionally, some of these studies used the segmentation technique to extract parameters from the images. This study shows that in some of these studies, DL methods were used for segmentation, and in others, the segmentation was done manually and using commercial software. Various parameters have been used to evaluate the diagnostic power of the models. The most used parameters are AUC, Accuracy, Sensitivity, Specificity, PPV, and NPV.
Discussion
CADs are one of the severe complications in recent years, leading to myocardial ischemia. Numerous shreds of evidence show that the functional severity of coronary artery stenosis is the main reason for myocardial ischemia. The FFR is the gold standard for the physiological evaluation of coronary artery stenosis and for deciding on the revascularization of coronary artery stenosis. However, despite considerable clinical evidence, the use of this method is minimal due to limitations such as cost, complexity, and invasiveness. In this research, twenty-five studies have been systematically examined, and the findings are as follows:
1. AI methods
Various methods of AI, including methods based on DL and ML and a combination of them, have been used to estimate the FFR. A meta-analysis study needs to be conducted to evaluate these methods, which is practically impossible due to the variety of datasets.
2. Imaging tools
This study revealed that various imaging tools, including CCTA, XCA, IVUS, and OCT, were used. In addition, some studies have used a combination of imaging tools to estimate the FFR. The mentioned imaging tools are suitable for the anatomical assessment of coronary arteries. However, CHU et al., in a systematic review study, showed that by using the anatomical data extracted from these imaging tools, estimating FFR is possible [50]. This study’s findings specifically show the use of AI methods to estimate the FFR using different imaging tools, which can help the physician diagnose by aggregating anatomical and physiological parameters regardless of the type of imaging tool and treating the disease, which can significantly improve clinical performance for patients.
3. Type of vessels
Regarding frequency and type of vessels (Distribution of lesion types), angiographic interventions on the LAD branch are crucial [51]. This branch has the most CAD vulnerability, and the FFR is performed on it the most [25]. The present study findings also show that in most studies, the number of LAD branches is more than in other vessels, and since there is a better relationship between anatomical and functional parameters in this branch than in other branches, more studies are needed to generalize the results to other branches [52]. On the other hand, these vessels’ flow and anatomy differ [53]. Several studies show that the accuracy of predicting the FFR can be different according to the type of branches [54]. This study also shows that the results obtained separately for each vessel and each segment (proximal, mid, and distal) are different [25, 32, 41, 48]. Therefore, the separation of the type of vessels and the separation of each vessel according to the type of segment to determine the accuracy of the FFR estimation model is essential.
4. Features and Feature Engineering
Extracting quantitative imaging biomarkers using DL methods has two significant advantages. Firstly, they always return the same qualitative results from a specific input; secondly, like humans, there is no variance due to fatigue [55]. This study also shows that in several studies, image segmentation steps and feature extraction using DL methods have been done [27, 29, 32, 34, 35, 37, 38, 40, 41, 43]. In addition, in some studies, the parameters in the images were extracted using manual methods and commercial software [25, 28, 30, 42, 46, 30, 26, 45, 33, 44, 49, 39]. Due to the advantages of using automatic methods to extract the features of images, most studies have used automatic methods to extract features in the past year. According to the clinical guidelines of the American Society of Cardiology and the European Society of Cardiology, parameters such as age, sex, heart rate, blood pressure (BP), and past medical history are used to make decisions about ischemic heart disease [56, 57]. This study also shows that some of these studies have considered parameters such as age, gender, and clinical data to estimate the FFR. However, this study demonstrates that the effective parameters for estimating the FFR depend on the type of AI model used. For example, age and gender were essential parameters in the XGBoost model. However, they did not have much effect in RF [47], and the gender parameter in the model XGBoost was considered one of the critical parameters, but the age parameter was not influential [44]. In addition, in the RF model, age and gender are not important parameters, but BP is considered one of the influential parameters [42]. Numerous studies should evaluate these parameters with more data and different models to determine the effective parameters for determining the FFR.
5. Current challenges & future research
In recent years, end-to-end frameworks have been introduced in the field of DL, and the benefits of using them in health have been investigated [58, 59]. The present study shows that several studies used this framework to estimate FFR [27, 29, 32, 34, 35, 37, 38, 40, 41, 43]. Due to the need for the end-to-end framework for a large amount of data and the lack of data in these studies, the overfitting problem should also be considered [34], for which we need many data. Nevertheless, in this study, the number of patients in 85% of the studies is less than 250 people, which is a fundamental challenge because high-quality and large-volume data is needed in AI studies to achieve the desired result. Therefore, to solve this problem, some studies using accurate data have produced a synthetic coronary tree to train the model [27, 40]. In addition, the need for a dataset with labeled data and a large volume seems very necessary for studies of this kind. Another important challenge in these studies appears to be external validation, and it is suggested that researchers pay attention to it in future studies so that by accurate validation of these techniques, they could be applied in practice in FFR estimation. The importance of performing non-invasive FFR estimation with the aid of artificial intelligence techniques and the significant implications cannot be underestimated. In the future, cardiologists could benefit from the implications of AI in Estimation of FFR.
Eventually, the current study illustrates that AI methods for estimating the FFR have received the attention of researchers, and these methods are of great interest to cardiologists and patients due to their non-invasive nature and low cost.
Limitations
In this study, the research for finding the revelvant literature was limited to studies published in English, and conference articles were not included in this study. In addition, the diversity of datasets used in different studies could impact the comparsion of different AI techniques in FFR estimation.
Conclusion
This study reveals that various AI methods, including ML and DL and hybrid methods for predicting the FFR, have been designed and developed in recent years. These methods use different parameters, such as parameters extracted from different imaging tools for non-invasive estimation of FFR have been taken into consideration. There are a variety of imaging tools that have been used for predicting FFR, though these tools have limitations for physiological assessment. Studies suggest the significance of combining both anatomical and physiological parameters for diagnosing and treatment of the coronary disease in different stages of the disease. Due to the excellent performance of these methods, AI methods are an ideal, non-invasive, and cost-effective solution to solve the existing problem, which can bring good clinical performance for patients.
Data Availability
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- A:
-
Automatically
- AI:
-
Artificial Intelligence
- ANN:
-
Artificial neural network
- BRNN:
-
Bidirectional Multilayer Recursive Neural Network
- BRNN:
-
Bidirectional Multilayer Recursive Neural Network
- CAD:
-
Coronary Artery Disease
- CCTA:
-
Coronary Computed Tomography Angiography
- cGAN:
-
Conditional Generative Adversarial Network
- CVD:
-
Cardiovascular Diseases
- DL:
-
Deep Learning
- DNN:
-
Deep Neural Networks
- FFR:
-
Fractional Flow Reserve
- GB:
-
Gradient Boosting
- GP:
-
LogitBoost
- GRU:
-
Gated Recurrent Units
- IVUS:
-
Intravascular Ultrasound
- LAD:
-
Left Anterior Descending artery
- LCA:
-
Left Coronary Artery
- LCX:
-
Left Circumflex artery
- LR:
-
Logistic Regression
- LVM:
-
Left Ventricular Myocardial
- M:
-
Manually
- ML:
-
Machine Learning
- MLNN:
-
Multilevel Neural Network
- MLP:
-
Multilayer Perceptron
- OCT:
-
Optical Coherence Tomography
- RCA:
-
Right Coronary Artery
- RCNN:
-
Recurrent Convolutional Neural Network
- RF:
-
Random Forest
- SVM:
-
Support Vector Machine
- XCA:
-
X-ray Coronary Angiography
References
Roth GA, et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70(1):1–25. https://doi.org/10.1016/j.jacc.2017.04.052].
Organization WH. Global status report on noncommunicable diseases 2014. World Health Organization; 2014. https://apps.who.int/iris/handle/10665/148114].
Do NT, et al. The quality of medical products for cardiovascular diseases: a gap in global cardiac care. BMJ global health. 2021;6(9):e006523. https://doi.org/10.1136/bmjgh-2021-006523].
Go AS, et al. Heart disease and stroke statistics–2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6–e245. https://doi.org/10.1161/CIR.0b013e31828124ad].
Vlachopoulos C, O’Rourke M, Nichols WW. McDonald’s blood flow in arteries: theoreticxperimental and clinical principles. 2011: CRC press. [DOI: https://doi.org/10.1201/b13568].
Feigl EJPr. Coron Physiol. 1983;63(1):1–205. https://doi.org/10.1152/physrev.1983.63.1.1].
Rodrigues DL et al. Automated detection of coronary artery stenosis in X-ray angiography using deep neural networks. 2021. arXiv:2103.02969. [DOI: arXiv.2103.02969].
Wu W, et al. Automatic detection of coronary artery stenosis by convolutional neural network with temporal constraint. Comput Biol Med. 2020;118:103657. https://doi.org/10.1016/j.compbiomed.2020.103657].
Gaede L, et al. Coronary angiography with pressure wire and fractional Flow Reserve. Dtsch Arztebl Int. 2019;116(12):205–11. https://doi.org/10.3238/arztebl.2019.0205].
Neumann FJ, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165. https://doi.org/10.1093/eurheartj/ehy394].
Ciccarelli G et al. Angiography Versus Hemodynamics to Predict the Natural History of Coronary Stenoses 2018. 137(14): p. 1475–1485. [DOI: 10.1161/CIRCULATIONAHA.117.028782].
Park SJ, Ahn JM. Should we be using fractional flow reserve more routinely to select stable coronary patients for percutaneous coronary intervention? Curr Opin Cardiol. 2012;27(6):675–81. https://doi.org/10.1097/HCO.0b013e328358f587].
Pijls NH, et al. Fractional flow reserve. A useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Circulation. 1995;92(11):3183–93. https://doi.org/10.1161/01.cir.92.11.3183].
Kern MJ, et al. Physiological assessment of coronary artery disease in the cardiac catheterization laboratory: a scientific statement from the American Heart Association Committee on Diagnostic and Interventional Cardiac catheterization, Council on Clinical Cardiology. Circulation. 2006;114(12):1321–41. https://doi.org/10.1161/CIRCULATIONAHA.106.177276].
Tu S, et al. Fractional flow reserve calculation from 3-dimensional quantitative coronary angiography and TIMI frame count: a fast computer model to quantify the functional significance of moderately obstructed coronary arteries. JACC Cardiovasc Interv. 2014;7(7):768–77. https://doi.org/10.1016/j.jcin.2014.03.004].
Zimmermann FM, et al. Deferral vs. performance of percutaneous coronary intervention of functionally non-significant coronary stenosis: 15-year follow-up of the DEFER trial. Eur Heart J. 2015;36(45):3182–8. https://doi.org/10.1093/eurheartj/ehv452].
Ono M, Onuma Y, Serruys PW. The era of single angiographic view for physiological assessment has come. Is simplification the ultimate sophistication? Catheter Cardiovasc Interv, 2021. 97 suppl 2: p. 964–5. [DOI: https://doi.org/10.1002/ccd.29662].
Terentes-Printzios D, et al. Angiography-based estimation of coronary physiology: a frame is worth a thousand words. Trends Cardiovasc Med. 2022;32(6):366–74. https://doi.org/10.1016/j.tcm.2021.07.004].
Desai NR et al. Appropriate use criteria for coronary revascularization and trends in utilization, patient selection, and appropriateness of percutaneous coronary intervention. 2015. 314(19): p. 2045–53. [DOI: https://doi.org/10.1001/jama.2015.13764].
Alizadehsani R, et al. Coronary artery disease detection using artificial intelligence techniques: a survey of trends, geographical differences and diagnostic features 1991–2020. Comput Biol Med. 2021;128:104095. https://doi.org/10.1016/j.compbiomed.2020.104095].
Monkam P, et al. Detection and classification of pulmonary nodules using Convolutional neural networks: a Survey. IEEE Access. 2019;7:78075–91. https://doi.org/10.1109/ACCESS.2019.2920980].
Liberati A, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–e34. https://doi.org/10.1371/journal.pmed.1000100].
Whiting PF, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–36. https://doi.org/10.7326/0003-4819-155-8-201110180-00009.
Lee HJ, et al. Optimization of FFR prediction algorithm for gray zone by hemodynamic features with synthetic model and biometric data. Comput Methods Programs Biomed. 2022;220:106827. https://doi.org/10.1016/j.cmpb.2022.106827].
Fossan FE, et al. Machine learning augmented reduced-order models for FFR-prediction. Comput Methods Appl Mech Eng. 2021;384. https://doi.org/10.1016/j.cma.2021.113892].
He XX et al. Classification of Lesion Specific Myocardial Ischemia Using Cardiac Computed Tomography Radiomics. in Conference on Medical Imaging - Computer-Aided Diagnosis. 2020. Houston, TX. [DOI: https://doi.org/10.1117/12.2548471].
Gao Z, et al. Learning physical properties in complex visual scenes: an intelligent machine for perceiving blood flow dynamics from static CT angiography imaging. Neural Netw. 2020;123:82–93. https://doi.org/10.1016/j.neunet.2019.11.017].
Carson J, et al. Artificial intelligence approaches to predict coronary stenosis severity using non-invasive fractional flow reserve. Proc Institution Mech Eng Part H J Eng Med. 2020;234. https://doi.org/10.1177/09544119209465.
Zreik M et al. Combined analysis of coronary arteries and the left ventricular myocardium in cardiac CT angiography for detection of patients with functionally significant stenosis. in Conference on Medical Imaging - Image Processing. 2021. Electr Network. [DOI: https://doi.org/10.48550/arXiv.1911.04940].
Yin M, Yazdani A, Karniadakis GE. One-dimensional modeling of fractional flow reserve in coronary artery disease: uncertainty quantification and bayesian optimization. Comput Methods Appl Mech Eng. 2019;353:66–85. https://doi.org/10.1016/j.cma.2019.05.005].
Dey D, et al. Integrated prediction of lesion-specific ischaemia from quantitative coronary CT angiography using machine learning: a multicentre study. Eur Radiol. 2018;28(6):2655–64. [DOI: 10.1007/s00330-017-5223-z].
Zreik M, et al. Deep learning analysis of coronary arteries in Cardiac CT Angiography for detection of patients requiring invasive coronary angiography. IEEE Trans Med Imaging. 2020;39(5):1545–57. [DOI: 10.1109/TMI.2019.2953054].
Kawasaki T, et al. Evaluation of significant coronary artery Disease based on CT fractional Flow Reserve and Plaque characteristics using Random Forest Analysis in Machine Learning. Acad Radiol. 2020;27(12):1700–8. https://doi.org/10.1016/j.acra.2019.12.013].
Kumamaru KK, et al. Diagnostic accuracy of 3D deep-learning-based fully automated estimation of patient-level minimum fractional flow reserve from coronary computed tomography angiography. Eur Heart J Cardiovasc Imaging. 2020;21(4):437–45. https://doi.org/10.1093/ehjci/jez160].
Wang Z, et al. Diagnostic accuracy of a deep learning approach to calculate FFR from coronary CT angiography. J Geriatric Cardiol. 2019;16(1):42–8. https://doi.org/10.11909/j.issn.1671-5411.2019.01.010].
Denzinger F et al. Deep learning algorithms for coronary artery plaque characterisation from CCTA scans. in Informatik aktuell. 2020. [DOI: 10.48550/arXiv.1912.06417].
van Hamersvelt RW, et al. Deep learning analysis of left ventricular myocardium in CT angiographic intermediate-degree coronary stenosis improves the diagnostic accuracy for identification of functionally significant stenosis. Eur Radiol. 2019;29(5):2350–9. https://doi.org/10.1007/s00330-018-5822-3].
Zreik M, et al. Deep learning analysis of the myocardium in coronary CT angiography for identification of patients with functionally significant coronary artery stenosis. Med Image Anal. 2018;44:72–85. https://doi.org/10.1016/j.media.2017.11.008].
Han D, et al. Incremental role of resting myocardial computed tomography perfusion for predicting physiologically significant coronary artery disease: a machine learning approach. J Nuclear Cardiol. 2018;25(1):223–33. https://doi.org/10.1007/s12350-017-0834-y].
Itu L, et al. A machine-learning approach for computation of fractional flow reserve from coronary computed tomography. J Appl Physiol. 2016;121(1):42–52. https://doi.org/10.1152/japplphysiol.00752.2015].
Hatfaludi C-A et al. Towards a Deep-Learning Approach for Prediction of Fractional Flow Reserve from Optical Coherence Tomography. 2022. 12(14): p. 6964. [DOI: https://doi.org/10.3390/app12146964].
Cha JJ, et al. Optical coherence tomography-based machine learning for predicting fractional flow reserve in intermediate coronary stenosis: a feasibility study. Sci Rep. 2020;10(1). https://doi.org/10.1038/s41598-020-77507-y].
Roguin A, et al. Early feasibility of automated Artificial Intelligence Angiography Based Fractional Flow Reserve Estimation. Am J Cardiol. 2021;139:8–14. https://doi.org/10.1016/j.amjcard.2020.10.022].
Cho H, et al. Angiography-based machine learning for Predicting Fractional Flow Reserve in Intermediate Coronary artery lesions. J Am Heart Association. 2019;8(4). https://doi.org/10.1161/JAHA.118.011685].
Lee JG, et al. Intravascular ultrasound-based machine learning for predicting fractional flow reserve in intermediate coronary artery lesions. Atherosclerosis. 2020;292:171–7. https://doi.org/10.1016/j.atherosclerosis.2019.10.022].
Kim Y, et al. Coronary artery decision algorithm trained by two-step machine learning algorithm. RSC Adv. 2020;10:4014–22. https://doi.org/10.1039/C9RA08999C].
Kim G, et al. Prediction of FFR from IVUS images using machine learning. 7th Joint International Workshop on Computing Visualization for Intravascular Imaging and Computer Assisted Stenting (CVII-STENT) / 3rd International Workshop on Large-scale Annotation of Biomedical data and Expert Label Synthesis (LABELS). 2018. https://doi.org/10.1007/978-3-030-01364-6_9. Granada, SPAIN.
Xue J, et al. Functional evaluation of intermediate coronary lesions with integrated computed tomography angiography and invasive angiography in patients with stable coronary artery disease. J Translational Intern Med. 2022;0(0). https://doi.org/10.2478/jtim-2022-0018].
Hae H, et al. Machine learning assessment of myocardial ischemia using angiography: Development and retrospective validation. PLoS Med. 2018;15(11):e1002693. https://doi.org/10.1371/journal.pmed.1002693].
Chu M, et al. A systematic review of imaging anatomy in predicting functional significance of coronary stenoses determined by fractional flow reserve. Int J Cardiovasc Imaging. 2017;33(7):975–90. https://doi.org/10.1007/s10554-017-1085-3].
Ilia R et al. Left anterior descending artery length in left and right coronary artery dominance. 2001. 12(1): p. 77–8. [DOI: 10.1097/00019501-200102000-00011].
Yang H-M et al. Relationship between intravascular ultrasound parameters and fractional flow reserve in intermediate coronary artery stenosis of left anterior descending artery: intravascular ultrasound volumetric analysis. 2014. 83(3): p. 386–94. [DOI: https://doi.org/10.1002/ccd.25088].
Wieneke H et al. Determinants of coronary blood flow in humans: quantification by intracoronary doppler and ultrasound. 2005. 98(3): p. 1076–82. [DOI: https://doi.org/10.1152/japplphysiol.00724.2004].
Müller LO, et al. Impact of baseline coronary flow and its distribution on fractional flow reserve prediction. Int J Numer Method Biomed Eng. 2021;37(11):e3246. https://doi.org/10.1002/cnm.3246].
Hagiwara A, et al. Variability and standardization of quantitative imaging: Monoparametric to Multiparametric quantification, Radiomics, and Artificial Intelligence. Invest Radiol. 2020;55(9):601–16. [DOI: 10.1097/RLI.0000000000000666].
Anderson JL, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing Committee to revise the 2002 guidelines for the management of patients with unstable Angina/Non-ST-Elevation myocardial infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007;50(7):e1–e157. https://doi.org/10.1161/CIRCULATIONAHA.107.181940].
Roffi M et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC) Eur Heart J, 2016. 37(3): p. 267–315. [DOI: https://doi.org/10.1093/eurheartj/ehv320].
Wang F, Casalino LP, Khullar D. Deep learning in Medicine—Promise, Progress, and Challenges. JAMA Intern Med. 2019;179(3):293–4. https://doi.org/10.1001/jamainternmed.2018.7117].
Yazhini K, Loganathan D. A State of Art Approaches on Deep Learning Models in Healthcare: An Application Perspective. in 2019 3rd International Conference on Trends in Electronics and Informatics (ICOEI). 2019. [DOI:https://doi.org/10.1109/ICOEI.2019.8862730].
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
The initial project idea was conceived, managed, and supervised by F.A. and R.R. and A.H. All authors then contributed to the refinement of the idea, and to the formal analysis of the results. F.A., R.R., and A.H. conducted the initial and full-text screenings. A.G. and A.R. drafted the first version of the manuscript with significant revisions and feedback from A.H., M.A., and Z.K. All authors contributed to discussions on the direction of the Systematic Literature Review, and subsequent manuscript revisions and all agreed to the final manuscript version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
IR.SBMU.RETECH.REC.1401.665.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Farhad, A., Reza, R., Azamossadat, H. et al. Artificial intelligence in estimating fractional flow reserve: a systematic literature review of techniques. BMC Cardiovasc Disord 23, 407 (2023). https://doi.org/10.1186/s12872-023-03447-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03447-w