Abstract
Background
CZT-SPECT has good agreement in the evaluation of mechanical synchronization compared with conventional SPECT. The aim of this study was to evaluate the correlation between left ventricular mechanical contraction synchrony and left ventricular systolic function by gated myocardial perfusion imaging (GMPI) using cadmium–zine–telluride (CZT) single photon emission computed tomography (SPECT).
Methods
This retrospective study involved 371 patients (239 males and 132 females, mean age 61.06 ± 11.78 years old) who underwent GMPI at the Nuclear Medicine Department of Shanxi Cardiovascular Hospital from January 2020 to August 2020. Systolic synchrony parameters and left ventricular systolic function parameters were calculated via Emory Cardiac Toolbox, including PP, PSD, PHB, HS, HK, EDV, ESV, and LVEF. Based on LVEF value, patients were divided into the severe reduction group (group 1, 127 cases, EF < 35%), moderate reduction group (group 2, 47 cases, 35% ≤ EF < 45%), mild reduction group (group 3, 50 cases, 45% ≤ EF < 50%) and normal group (group 4, 147 cases, EF ≥ 50%). Differences in PP, PSD, PHB, HS and HK among the four groups were compared using one-way ANOVA. Differences between two groups were compared using LSD-t test. The correlation among functional and mechanical contraction synchrony factors were analyzed using Pearson test.
Results
PP, PSD, PHB, HS and HK were significantly different among the four groups (F = 5.20, 188.72, 202.88, 171.05, 101.36, P < 0.001). Pairwise comparison tests showed significant differences in PSD and PHB in each two groups, and HS and HK in each two groups except for group 2 and 3 (t = 0.28 and 0.39, both P > 0.001). PP was significantly higher in group 1, relative to group 3 (t = 2.43, P < 0.001) and group 4 (t = 3.67, P < 0.001). Pearson correlation analysis revealed that LVEF negatively correlates with PP, PSD, PHB (r = 0.194, − 0.790, − 0.799, all P < 0.001). HS and HK showed positive correlation for LVEF (r = 0.778 and 0.795, P < 0.001), PSD, PHB and ESV were had good positive correlation (r = 0.778, 0.795, P < 0.001), PSD, PHB and EDV had good positive correlation (r = 0.722, 0.732, P < 0.001). However, PP had poor correlation with EDV (r = 0.095, P > 0.001). HS and HK were negatively correlated with EDV and ESV (r = − 0.700 to − 0.594, P < 0.001).
Conclusion
CZT SPECT GMPI provided left ventricular mechanical contraction synchrony parameters that correlated well with left ventricular systolic function. Worse left ventricular mechanical contraction synchrony lead to decreased LVEF, making the systolic synchrony parameters valuable in the prediction of left ventricular systolic function.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Techniques that detect cardiac mechanical contraction synchrony [1,2,3] include M-mode ultrasound, tissue Doppler imaging (TDI), speckle tracking imaging (STI) technology, real time three dimensional echocardiography (RT-3DE), gated myocardial perfusion imaging (GMPI), and cardiac magnetic resonance imaging (CMR) [4]. GMPI phase analysis quantitatively evaluates left ventricular contraction synchrony and the important information such as myocardial blood perfusion, ventricular wall motion, left ventricular systolic function, and left ventricular mechanical contraction synchrony can be obtained through a “one-stop” collection. Due to the outstanding application values on cardiac mechanical contraction synchrony, GMPI phase analysis is widely used in CRT electrode implantation guidance and prognosis prediction [5, 6]. The novel cardiology focused SEPCT utilizes solid-state cadmium zinc telluride (CZT) crystal as a detector, and has numerous advantages including high sensitivity, high spatial resolution, short acquisition time, and less radiation dose [7]. However, research on left ventricular mechanical contraction synchrony is limited. Left ventricular ejection fraction (LVEF) is a powerful predictor of cardiac mortality for the patients with heart failure, mechanical dyssynchrony is also important for the patients with heart failure. Here, we analyzed correlation between left ventricular function parameters and quantitative parameters of mechanical contraction synchrony using CZT SPECT phase analysis software to explore the role of mechanical systolic synchrony parameters for predicting the prognosis of patients with heart failure in the future, and evaluated the application of CZT SPECT in mechanical contraction synchrony.
Methods
Patient characteristics
We retrospectively enrolled 371 patients (239 males and 132 females, mean age 61.06 ± 11.78 years old) who underwent CZT SPECT resting GMPI at the Nuclear Medicine Department of Shanxi Cardiovascular Hospital from January 2020 to August 2020. Based on LVEF value, patients were divided into the severe reduction group (group 1, 127 cases, EF < 35%), moderate reduction group (group 2, 47 cases, 35% ≤ EF < 45%), mild reduction group (group 3, 50 cases, 45% ≤ EF < 50%) and normal group (group 4, 147 cases, EF ≥ 50%). Exclusion criteria were frequent premature beats, atrial fibrillation, and some patients could not meet the CZT SPECT gated sampling criteria (the exclusion rate was more than 10% of the total collection heart rate). All participants gave written informed consent and the study adhered to Declaration of Helsinki principles.
Myocardial perfusion imaging acquisition protocol
Patients were underwent in CZT SPECT (Discovery NM 530c; GE Healthcare, Haifa, Israel), The patient was intravenously injected 99mTc-MIBI (370–555 mBq), and rest GMPI was performed 1.0–1.5 h after injection, the total acquisition time was about 6–12 min. A array of multi-detector in the CZT SPECT system, the 19 detectors system remain in a fixed position on the cardiac volume. Per cardiac cycle was divided into 8 frames for ECG-gated data acquisition. All images were acquired (matrix size 32 × 32); energy window 20%; energy peak140 keV; pixels width 4 mm). Images were reconstructed on a standard workstation (Xeleris II; GE Healthcare) using a previously validated dedicated iterative algorithm with 50 iterations, no attenuation or scatter correction was done, but the patients with suspected diaphragmatic attenuation artifacts were collected in the prone position to improve image quality.
Gated images analysis and phase analysis
CZT SPECT data were reconstructed using ordered subsets expectation maximization (OSEM) and analyzed by two experienced nuclear medicine physicians. The left ventricular mechanical systolic synchronization parameters were calculated using Emory Cardiac Toolbox™ (US, version 3.2) software. The quantitative parameters of left ventricular function, including end-diastolic volume (EDV), end-systolic volume (ESV) and left ventricular ejection fraction (LVEF) were obtained. Through GMPI phase analysis, 5 quantitative indicators reflection synchrony of left ventricular myocardial contraction were obtained: peak phase (PP), which is the peak of the phase diagram; phase standard deviation (PSD), which is the distribution range of the phase; phase histogram bandwidth (PHB), which is 95% width of the phase histogram; histogram skewness (HS), that is the symmetry of the histogram; histogram kurtosis (HK), which is the width from the beginning of the histogram to the peak.
Statistic analysis
Data are shown as mean ± SD. Differences between PP, PSD, PHB, HS, HK were evaluated using one-way ANOVA. LSD-t test was used to compare differences between 2 groups. Correlation among functional and mechanical contraction synchrony factors were analyzed using Pearson test. SPSS software (IBM SPSS Statistics, version 23.0) was used for data analysis, P < 0.001 indicated statistical significances.
Results
Clinical characteristics
Clinical characteristics of the study four group patients are presented in Table 1. There was no significant difference in age (P = 0.431), weight (P = 0.626), and height (P = 0.336) among the four groups, but gender distribution and BMI showed significant difference (P < 0.001). The proportion of men in abnormal left ventricular function groups (EF < 50%) was higher than normal left ventricular function group 4 (EF ≥ 50%). The reason may be due to the fact that men have more smoking, drinking history, etc. than women. There was no significant difference in the prevalence of diabetes mellitus, hypertension, dyslipidemia, smoking, and drinking (P = 0.415, 0.005, 0.342, 0.020, 0.350) among the four groups.
Analysis of mechanical dyssynchrony
Significant mechanical dyssynchrony was defined as Phase SD ≥ 43°. 76% had dyssynchrony among patients with EF < 35% and this group has the highest proportion of mechanical dyssynchrony than the other 3 groups. Those patients with 35% ≤ EF < 45% (40% dyssynchrony), 45% ≤ EF < 50% (32% dssynchrony). The patients with EF ≥ 50% had a lowest prevalence of dssynchrony (1%) (Fig. 1). Typical cases in each group are shown in Fig. 2.
Typical examples of each group are shown. A Group 1, EF = 20%, EDV = 195 ml, ESV = 156 ml, PP = 133.0, PSD = 68.1°, PHB = 232.0°, HS = 2.1, HK = 4.5. B Group 2, EF = 41%, EDV = 120 ml, ESV = 71 ml, PP = 121.0, PSD = 52.1°, PHB = 156.0°, HS = 2.4, HK = 5.3. C Group 3, EF = 48%, EDV = 138 ml, ESV = 72 ml, PP = 147.0, PSD = 18.8°, PHB = 60.0°, HS = 3.3, HK = 10.7. D Group 4, EF = 69%, EDV = 68 ml, ESV = 21 ml, PP = 133.0, PSD = 11.3°, PHB = 34.0°, HS = 4.6, HK = 23.9
Comparison of mechanical contraction synchrony parameters among four groups
One-way ANOVA revealed statistically significant differences in PP, PSD, PHB, HS, HK among four groups (F = 5.20, 188.72, 202.88, 171.05, 101.36, all P < 0.001, Table 2). PSD and PHB differed significantly between the 4 groups (P < 0.001); There was no statistically significant difference in HS (P = 0.780) and HK (P = 0.969) between group 2 and 3 group. There were statistically significant differences between the other groups (P < 0.001); There were no statistically significant differences in PP between the other groups (P > 0.05) except for group 1 and group 3 (t = 2.43, P < 0.05) or group 4 (t = 3.67, P < 0.001).
Correlation analysis between left ventricular function and mechanical contraction synchrony parameters
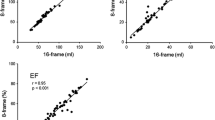
Cardiac function parameters for each group are shown. LVEF (20.76 ± 7.48)%, EDV (213.52 ± 75.12) ml, ESV (213.52 ± 75.12) ml in group 1, LVEF (39.66 ± 3.13)%, EDV (141.30 ± 41.36) ml, ESV (86.98 ± 30.95) ml in group 2, LVEF (47.68 ± 1.32)%, EDV (116.77 ± 22.14) ml, ESV (61.41 ± 12.15) ml in group 3, LVEF (63.79 ± 7.41)%, EDV (79.29 ± 21.35) ml, ESV (29.93 ± 14.22) ml in group 4. Pearson correlation analysis (Table 3) showed that PP, PSD, PHB and LVEF were negatively correlated (r = 0.194, − 0.790, − 0.799, all P < 0.001). Among them, PP had poor correlation with LVEF while PSD and PHB were significantly negatively correlated with LVEF, HS, HK and LVEF were positively correlated (r = 0.767, 0.676, P < 0.001). PSD, PHB and ESV were significantly positively correlated (r = 0.778, 0.795, P < 0.001), while PP and ESV were not well correlated (r = 0.145, P > 0.05), PSD, PHB and EDV were significantly positively correlated (r = 0.722, 0.732, P < 0.001), but PP had no correlation with EDV (r = 0.095, P = 0.078), HS, HK, EDV and ESV were all negatively correlated (r = − 0.700 to − 0.594, P < 0.001) (Figs. 3, 4, 5).
Discussion
GMPI phase analysis is a new technique to quantitatively evaluate left ventricular myocardial mechanical synchronization. Phase analysis is a short axis diagram of 8 phases in one cardiac cycle from GMPI image as input information. The left ventricle is divided into more than 700 areas and 3D count distributions are extracted from each of the left ventricle short-axis data sets, then you can get phase distribution of the initial time of myocardial contraction in different parts and the whole phase of the left ventricle distribution by calculating the radioactivity count rate of each area [8, 9]. Since CZT SPECT directly converts γ-rays into electrical signals and performs meter mode acquisition, it has a higher count rate and spatial resolution. Image quality is high even in a short acquisition time with reduced injection doses [10,11,12]. Enough evidence has been collected from multiple laboratories in many countries and the CZT technology was considered as the ‘‘gold standard’’ of SPECT imaging [13]. CZT SPECT completes gated acquisition to obtain relevant quantitative parameters for severe heart failure, especially for patients who require CRT installation with mechanical synchrony and latest excitement evaluation. Here, 127 patients (group 1) with severely reduced LVEF had an average LVEF of 20.76 ± 7.48%, and all of them successfully completed gated collection. Studies showed that CZT SPECT (Discovery NM 530c) is consistent with conventional SPECT in detecting left ventricular mechanical contraction synchrony (98%) [14]. Cardiac function parameters measured by CZT SPECT are in good agreement with MRI [15]. The coordination and synchrony of ventricular wall motion for each segment of the left ventricular myocardium directly affects overall systolic and diastolic function of the left ventricle. Ultrasound technology application showed that the left ventricular mechanical contraction is not synchronized in the part of heart failure with preserved ejection fraction [16]. Other studies have confirmed that early heart failure is accompanied by left ventricular mechanical contraction asynchrony [17]. Based on the cardiac function classification recommended by 2018 SPECT myocardial perfusion imaging guidelines, we evaluated correlation between cardiac function and left ventricular mechanical contraction synchrony in a relatively large sample size [18]. We found that synchronization parameters of mechanical contractions in each group were significantly different among groups with different LVEF values. Pairwise comparison results indicate that phase standard deviation and phase histogram bandwidth can more sensitively distinguish among groups synchronization caused by LVEF differences, while the histogram skewness, histogram kurtosis, and peak phase suggest poorly sensitive differentiation among groups. This study found that the greater the left ventricular systolic and end-diastolic volume, the more severe the damage to the left ventricular systolic function, and the worse the left ventricular mechanical contraction synchrony. As shown in Fig. 1, larger phase distribution range brings wide bandwidth, large deflection, small skewness, and a broad asymmetrical peak phase. Jianfeng Wang et al. confirmed that LVEF negatively correlated with phase histogram bandwidth upon synchronization evaluation in patients with old myocardial infarction (r = − 0.807) [19]. Hongbo Yang et al. found that phase standard deviation and bandwidth negatively correlated with LVEF in chronic total occlusion (CTO) lesions, while the skewness and kurtosis of the phase map positively correlated with LVEF [20], which is consistent with our findings. Note that LVEF is a powerful predictor of cardiac mortality [21]. Our study showed that the worse left ventricular mechanical contraction synchrony leads to decreased LVEF, making the systolic synchrony parameters valuable in the prediction of cardiac mortality. Hence, the role of mechanical systolic synchrony parameters should be considered for predicting the prognosis of patients belonging to the severe reduction group and moderate reduction group. PSD, PHB, HS, and HK have similar correlations with left ventricular systolic function, the worse left ventricular mechanical contraction synchrony leads to decreased LVEF, but PSD and PHB are rougher and more sensitive, suggesting that HS and HK can be used to evaluate mechanical contraction synchronization. However, larger studies are needed to determine if HS and HK are more sensitive than PSD and PHB, and if phase peak and left ventricular function parameters are poorly correlated or uncorrelated. Previous studies used PSD and PHB as the most sensitive evaluation indicators of mechanical synchrony due to their good consistency with TDI synchronization parameters. Another study showed that TDI is insufficient for detecting left ventricular asynchrony and predicting CRT efficacy [22]. Recently, synchronization evaluations based on ultrasound, including RT-3DE [23] and STI [24] have emerged and offered numerous advantages for assessing synchronization and evaluating prognosis [25]. Studies showed that conventional SPECT is consistent with RT-3DE in detecting left ventricular mechanical contraction synchrony for the patients with heart failure [26]. Future comparison studies should validate CZTSPECT sensitivity using other techniques, including RT-3DE, STI, and MRI, and evaluate the capability of HS and HK on synchronization consistency.
Study limitations
This study has some limitations. First, we did not strictly exclude the influence of patients with occasional arrhythmia on the acquisition of synchronization parameters of ventricular mechanical contraction during the gated acquisition process. Moreover, we were unable to reach all patients for prognosis information. Future follow-ups are needed to determine the predictive effect of systolic synchrony parameters.
Conclusion
CZT SPECT GMPI provided left ventricular mechanical contraction synchrony parameters that correlated well with left ventricular systolic function. The worse left ventricular mechanical contraction synchrony leads to decreased LVEF, making the systolic synchrony parameters valuable in the prediction of left ventricular systolic function.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author upon request.
References
van’t Sant J, ter Horst IAH, Wijers SC, et al. Measurements of electrical and mechanical dyssynchrony are both essential to improve prediction of CRT response. J Electrocardiol. 2015;48:601–8.
Tang J, Chen S, Liu L, et al. Assessment of permanent selective his bundle pacing in left ventricular synchronization using 3-D speckle tracking echocardiography. Ultrasound Med Biol. 2018. https://doi.org/10.1016/j.ultrasmedbio.2018.10.006.
Marsan NA, Henneman MM, Chen J, Ypenburg C, Dibbets P, Ghio S, et al. Left ventricular dyssynchrony assessed by two three-dimensional imaging modalities: phase analysis of gated myocardial perfusion SPECT and tri-plane tissue Doppler imaging. Eur J Nucl Med Mol Imaging. 2008;35(1):166–73. https://doi.org/10.1007/s00259-007-0539-6.
Ahmed W, Samy W, Tayeh O, et al. Left ventricular scar impact on left ventricular synchronization parameters and outcomes of cardiac resynchronization therapy. Int J Cardiol. 2016;222:665–70. https://doi.org/10.1016/j.ijcard.2016.07.158.
Lin X, Xu H, Zhao X, et al. Sites of latest mechanical activation as assessed by SPECT myocardial perfusion imaging in ischemic and dilated cardiomyopathy patients with LBBB. Eur J Nucl Med Mol Imaging. 2014;41(6):1232–9.
Hage FG. Left ventricular mechanical dyssynchrony by phase analysis as a prognostic indicator in heart failure. J Nucl Cardiol. 2014;21(1):67–70. https://doi.org/10.1007/s12350-013-9822-z.
de Amorim Fernandes F, Peix A, Giubbini R, Karthikeyan G, Massardo T, Patel C, et al. Reproducibility of global LV function and dyssynchrony parameters derived from phase analysis of gated myocardial perfusion SPECT: A multicenter comparison with core laboratory setting. J Nucl Cardiol. 2022;29(3):952–61.
Bois JP, Scott C, Chareonthaitawee P, Gibbons RJ, Rodriguez-Porcel M. Phase analysis single-photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) detects dyssynchrony in myocardial scar and increases specificity of MPI. EJNMMI Res. 2019;9(1):11. https://doi.org/10.1186/s13550-019-0476-y.
Zhou W, Jiang Z, Chen J, Garcia EV, Li D. Development and validation of a phase analysis tool to measure interventricular mechanical dyssynchrony from gated SPECT MPI. J Nucl Cardiol. 2017;24(5):1680–6. https://doi.org/10.1007/s12350-016-0503-6.
Tanaka H, Chikamori T, et al. Comparison of myocardial perfusion imaging between the new high-speed gamma camera and the standard anger camera. Circ J. 2013;77:1009–17. https://doi.org/10.1253/circj.CJ-12-1093.
Lin W-L, Wang S-Y, Shiau Y-C, Wu Y-W. The clinical usefulness of phase analysis in detecting coronary artery disease using dipyridamole thallium-201-gated myocardial perfusion imaging with a cadmium–zinc–telluride camera. J Nucl Cardiol. 2020;27(1):241–50. https://doi.org/10.1007/s12350-018-1417-2.
Claudin M, Imbert L, Djaballah W, Veran N, Poussier S, Roch V, et al. Routine evaluation of left ventricular function using CZT-SPECT, with low injected activities and limited recording times. J Nucl Cardiol. 2018;25(1):249–56. https://doi.org/10.1007/s12350-016-0615-z.
Henzlova MJ, Duvall L. Is the CZT technology the future of nuclear cardiology? J Nucl Cardiol. 2020. https://doi.org/10.1007/s12350-020-02399-4.
Pazhenkottil AP, Buechel RR, Herzog BA, et al. Ultrafast assessment of left ventricular dyssynchrony from nuclear myocardial perfusion imaging on a new high-speed gamma camera. Eur J Nucl Med Mol Imaging. 2010;37:2086–92. https://doi.org/10.1007/s00259-010-1507-0.
Claudin M, Imbert L, et al. Routine evaluation of left ventricular function using CZT-SPECT, with low injected activities and limited recording times. J Nucl Cardiol. 2018;25(1):249–56.
Lee PW, Zhang Q, Yip GW, et al. Left ventricular systolic and diastolic dyssynchrony in coronary artery disease with preserved ejection fraction. Clin Sci (Lond). 2009;1(16):521–9.
Takahashi N, Yamamoto A, Tezuka S, Ishikawa M, Abe J, Amitani K, et al. Assessment of left ventricular dyssynchrony during development of heart failure by a novel program using ECG-gated myocardial perfusion SPECT. Circ J. 2008;72(3):370–7. https://doi.org/10.1253/circj.72.370.
Dorbala S, Ananthasubramaniam K, et al. Single photon emission computed tomography (SPECT) myocardial perfusion imaging guidelines: instrumentation, acquisition, processing, and interpretation. J Nucl Cardiol. 2018. https://doi.org/10.1007/s12350-018-1283-y.
Jianfeng W, Yuetao W, Xiaoli Z, et al. Left ventricular systolic synchrony assessed by phase analysis of gated myocardial perfusion imaging in patients with old myocardial infarction. Chin J Cardiol. 2015;43(7):599–604.
Yang H, Dai Y, Li C, Lu H, Chang S, Qian J, Ge J. Two cases of successful revascularization of chronic total occlusions by the first use of a new guide extension catheter in unbelievable tortuous right coronary arteries. Int J Cardiol. 2016;223:98–100. https://doi.org/10.1016/j.ijcard.2016.08.186.
Karabulut U, Keskin K, Karabulut D, Yiğit E, Yiğit Z. Effect of sacubitril/valsartan combined with dapagliflozin on long-term cardiac mortality in heart failure with reduced ejection fraction. Angiology. 2022;73(4):350–6. https://doi.org/10.1177/00033197211047329.
Marsan NA, Henneman MM, et al. Left ventricular dyssynchrony assessed by two three-dimensional imaging modalities: phase analysis of gated myocardial perfusion SPECT and tri-plane tissue Doppler imaging. Eur J Nucl Med Mol Imaging. 2008;35:166–73. https://doi.org/10.1007/s00259-007-0539-6.
Zhong S-W, Zhang Y-Q, Chen L-J, Zhang Z-F, Wu L-P, Hong W-J. Ventricular function and dyssynchrony in children with a functional single right ventricle using real time three-dimensional echocardiography after fontan operation.
Sun Z, Di B, Gao H, Lan D, Peng H. Assessment of ventricular mechanical synchronization after left bundle branch pacing using 2-D speckle tracking echocardiography.
Marsan NA, Henneman MM, Chen J, Ypenburg C, Dibbets P, Ghio S, Bleeker GB, Stokkel MP, van der Wall EE, Tavazzi L, Garcia EV, Bax JJ. Real-time three-dimensional echocardiography as a novel approach to quantify left ventricular dyssynchrony: a comparison study with phase analysis of gated myocardial perfusion single photon emission computed tomography. J Am Soc Echocardiogr. 2008;21(7):801–7. https://doi.org/10.1016/j.echo.2007.12.006.
Marsan NA, Henneman MM, Chen J, Ypenburg C, Dibbets P, Ghio S, Bleeker GB, Stokkel MP, van der Wall EE, Tavazzi L, Garcia EV, Bax JJ. Left ventricular dyssynchrony assessed by two three-dimensional imaging modalities: phase analysis of gated myocardial perfusion SPECT and tri-plane tissue Doppler imaging. Eur J Nucl Med Mol Imaging. 2008;35(1):166–73. https://doi.org/10.1007/s00259-007-0539-6.
Acknowledgements
Not applicable.
Funding
The research was financially supported by Shanxi Provincial Basic Research Program Youth Scientific Project Fund (20210302124695); Shanxi Medical Science and Technology Innovation Team Fund (2020TD24). Shanxi Medical Science and Technology Innovation Team Fund Research Incentive Program of Shanxi Cardiovascular Hospital (XYS20190204).
Author information
Authors and Affiliations
Contributions
QS: Writing the original manuscript and analyzing SPECT imaging; methodology, visualization, data analysis. RH: Contributing to conception and design. SF: SPECT imaging acquisition, analyzing SPECT imaging. CW: Acquisition of data and statistical analysis, analyzing SPECT imaging. XG: Acquisition of data and statistical analysis, analyzing SPECT imaging. TL: Analyzing imaging. YH: analyzing imaging. FW Interpreting the clinical significance in cardiovascular aspects. RX: Interpreting the clinical significance. SL: Drafting the article or revising it critically for important intellectual content; final approval of the version to be submitted. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study design was approved by the Institutional Ethics Committee of the Shanxi Cardiovascular Hospital and performed in accordance with the Declaration of Helsinki and its later amendments. All the study participants provided informed consents.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, Q., Huang, R., Fu, S. et al. Relationship between left ventricular mechanical synchrony and left ventricular systolic function: a CZT-SPECT analysis. BMC Cardiovasc Disord 22, 420 (2022). https://doi.org/10.1186/s12872-022-02863-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-022-02863-8