Abstract
Background
Post-cardiac injury syndrome (PCIS) is an inflammatory condition following myocardial or pericardial damage. In response to catheter ablation, PCIS most frequently occurs after extensive radiofrequency (RF) ablation of large areas of atrial myocardium. Minor myocardial injury from right septal slow pathway ablation for atrioventricular nodal reentrant tachycardia (AVNRT) is not an established cause of the syndrome.
Case presentation
A 62-year-old women with a 6-year history of symptomatic narrow-complex tachycardia was referred to perform an electrophysiological study. During the procedure AVNRT was recorded and a total of two RF burns were applied to the region between the coronary sinus and the tricuspid annulus. Pericardial effusion was routinely ruled out by focused cardiac ultrasound. In the following days, the patient developed fever, elevated inflammatory and cardiac markers, new-onset pericardial effusion, characteristic ECG changes, and complained of pleuritic chest pain. An extensive workup for infectious, metabolic, rheumatologic, neoplastic, and toxic causes of pericarditis and myocarditis was unremarkable. Cardiac magnetic resonance imaging showed no signs of ischemia, infiltrative disease or structural abnormalities. The patient was diagnosed with PCIS and initiated on aspirin and low-dose colchicine. At a 1-month follow-up visit the patient was free of symptoms but still had a small pericardial effusion. After three months of treatment the pericardial effusion had resolved completely.
Conclusions
Inflammatory pericardial reactions can occur after minor myocardial damage from RF ablation without involvement of structures in close proximity to the pericardium.
Similar content being viewed by others
Background
Post-cardiac injury syndrome (PCIS) is an inflammatory reaction to myo-pericardial damage and constitutes a rare but important complication of radiofrequency (RF) catheter ablation [1, 2]. Serious clinical sequelae include massive pericardial effusion with delayed cardiac tamponade, pleural effusion, and hypoxemia [2]. Most frequently, PCIS is reported after ablation of large areas of atrial myocardium in close proximity to the pericardium [2,3,4,5,6]. Here, we describe a unique case of PCIS after right septal ablation for atrioventricular nodal reentrant tachycardia (AVNRT).
Case presentation
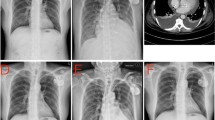
A 62-year-old female with a 6-year history of paroxysmal narrow-complex tachycardia was referred for an electrophysiologic study. On admission, the patient was asymptomatic and her routine clinical assessment and physical examination were unremarkable. During her electrophysiology study, sustained typical AVNRT was induced and RF ablation was performed with a non-irrigated Navistar ablation catheter (Biosense Webster) using three-dimensional electroanatomic guidance. A total of two RF burns were applied to the region between the coronary sinus and tricuspid annulus. The first RF burn (35 W [W], 12 Ohm impedance drop during 50 s) showed good junction response but more than 2 echo beats persisted after the energy application. A second burn (35 W, 11 Ohm impedance drop during 60 s) resulted in successful slow pathway ablation (Fig. 1). Pericardial effusion was ruled out by postprocedural focused cardiac ultrasound which is routinely performed at our centre. During the next days, the patient developed a low-grade fever of 38 degrees Celsius, mild tachycardia, leucocytosis, elevated cardiac markers, and complained of chest pain on inspiration. Creatinine kinase (CK) was elevated at 168 U/L and high sensitivity cardiac Troponin T at 294 pg/mL. A new-onset circumferential pericardial effusion was detected on echocardiography and the electrocardiogram (ECG) showed diffuse saddle-shaped ST segment elevations (Fig. 2). An extensive workup for infectious, metabolic, rheumatologic, neoplastic, and toxic causes of pericarditis and myocarditis was unremarkable. Gadolinium-enhanced cardiac magnetic resonance imaging showed no signs of ischemia, infiltrative disease or structural abnormalities. According to current clinical practice guidelines [1] a diagnosis of post-cardiac injury syndrome (PCIS) was made and the patient was started on aspirin and low-dose colchicine. Within three days of treatment, symptoms and ECG changes resolved, the pericardial effusion was reduced, and the patient could be discharged home. One month later, the patient still showed a small pericardial effusion and was continued on aspirin and colchicine. At a 3-month follow-up, the patient was doing well and the pericardial effusion had resolved completely.
Region of energy application and catheter position during the procedure. Electroanatomic map showing the RF burns (purple and red), the coronary sinus (grey), and the His bundle region (orange) in right (A) and left (B) anterior oblique view. Appropriate position of the catheter tips (C) in the high right atrium (HRA), in the coronary sinus (CS), at the His region (His), and at the right ventricular apex (RV)
Discussion
PCIS is an umbrella term for a variety of inflammatory pericardial reactions following damage to the myocardium or pericardium. PCIS was first described by Dressler [7] and is characterized by fever, pleuritic chest pain, pericardial effusion and elevated inflammatory markers [1]. Such inflammatory syndromes are presumed to have an autoimmunologic pathogenesis which is supported by their tendency for recurrence [1, 8]. Aside from extensive injury secondary to myocardial infarction or open surgery involving pericardiotomy, PCIS can be caused by minimal cardiac damage from pacemaker lead insertion [9], transcatheter mitral valve repair [10], transcatheter aortic valve replacement [10], and percutaneous coronary intervention [11] in predisposed individuals. Overall, PCIS develops in up to 1-5% of percutaneous cardiac interventions [12].
In response to catheter ablation, PCIS most frequently occurs after extensive energy application during ablation of large areas of left or right atrial myocardium in close intimacy to the visceral pericardium [2]. According to a report by Li et al. [2], over 70% of cases due to catheter ablation are caused by left atrial ablation for atrial fibrillation and right atrial ablation for atrial flutter [2]. Interestingly, in our patient the syndrome occurred secondary to a very minor trauma by only two RF burns without involvement of structures in proximity to the pericardium supporting the concept of an underlying immunologic reaction. The pathophysiology of PCIS after catheter ablation is poorly understood [2], yet putative triggers may include myocardial necrosis from the RF burn leading to the release of auto-antigens [1, 2], mechanical trauma to the pericardium during the procedure, and intraprocedural tachycardia in combination with an underlying substrate, such as a subclinical myocarditis. While differential diagnoses, including infectious, metabolic, rheumatologic, neoplastic, and toxic aetiologies, were ruled out in an extensive clinical workup, we acknowledge that, in order to minimize patient risk, no confirmatory histopathological analyses of myocardial or pericardial specimens were conducted. A markedly shorter delay to symptom onset in patients with PCIS after catheter ablation [2,3,4,5,6, 13,14,15] compared to other cardiac injuries suggests different underlying mechanisms and distinguishes this entity from others within the spectrum of PCIS. In line with the literature [2,3,4,5,6, 13,14,15], our patient developed PCIS within the first week after the intervention and responded well to medical treatment with aspirin and low-dose colchicine.
Treatment of PCIS is based on anti-inflammatory agents including aspirin, non-steroidal anti-phlogistic drugs, corticosteroids, and colchicine [1, 16]. Aspirin is recommended as a first-line treatment of PCIS while colchicine may be considered as an add-on therapy [1]. Timely detection and medical therapy of PCIS commonly leads to complete resolution of signs and symptoms and is key to preventing long-term sequelae such as recurrent pericardial effusion and pericardial constriction [1, 12]. Given the increasing use of catheter ablation for the treatment of cardiac arrythmia, awareness of potential complications is critical to guide patient care.
Conclusions
Inflammatory pericardial reactions can be triggered by minor myocardial injury from right septal slow pathway ablation in susceptible individuals. Clinical surveillance in the postprocedural period helps to identify complications.
Availability of data and materials
All relevant data supporting the conclusions of this article are included in the article. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ANRT:
-
Atrioventricular nodal reentrant tachycardia
- CK:
-
Creatinine kinase
- CS:
-
Coronary sinus
- His:
-
His region
- ECG:
-
Electrocardiogram
- HRA:
-
High right atrium
- PCIS:
-
Post-cardiac injury syndrome
- PE:
-
Pericardial effusion
- RF:
-
Radiofrequency
- RV:
-
Right ventricular apex
- W:
-
Watt
References
Adler Y, Charron P, Imazio M, Badano L, Barón-Esquivias G, Bogaert J, et al. ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2015;36:2921–64.
Li W, Sun J, Yu Y, Wang ZQ, Zhang PP, Guo K, et al. Clinical features of post cardiac injury syndrome following catheter ablation of arrhythmias: systematic review and additional cases. Heart Lung Circ. 2019;66:1689–96.
Torihashi S, Shiraishi H, Hamaoka T, Imai M, Kuroyanagi A, Nakanishi N, et al. Two cases of delayed cardiac tamponade due to pericarditis after pulmonary vein (PV) isolation for atrial fibrillation. Intern Med. 2015;54:791–6.
Wood MA, Ellenbogen KA, Hall J, Kay GN. Post-pericardiotomy syndrome following linear left atrial radiofrequency ablation. J Interv Card Electrophysiol. 2003;9:55–7.
Koller ML, Maier SK, Bauer WR, Schanzenbächer P. Postcardiac injury syndrome following radiofrequeny ablation of atrial flutter. Z Kardiol. 2004;93:560–5.
Goossens K, Caenepeel A, De Greef Y. Delayed tamponade triggering Dressler’s syndrome after pulmonary vein isolation. Acta Cardiol. 2012;67:595–8.
Dressler W. A post-myocardial infarction syndrome; preliminary report of a complication resembling idiopathic, recurrent, benign pericarditis. J Am Med Assoc. 1956;160:1379–83.
Bonaventura A, Vecchié A, Mauro AG, Brucato AL, Imazio M, Abbate A. An update on the pathophysiology of acute and recurrent pericarditis. Panminerva Med. 2021;63(3):249–60.
Sedaghat-Hamedani F, Zitron E, Kayvanpour E, Lorenz HM, Katus HA, Meder B. Post cardiac injury syndrome after initially uncomplicated CRT-D implantation: a case report and a systematic review. Clin Res Cardiol. 2014;103:781–9.
Alachkar MN, Lehrke M, Marx N, Almalla M. Post-cardiac injury syndrome after transcatheter mitral valve repair using MitraClip system: a case report. Eur Heart J Case Rep. 2020;4:1–5.
Park JS, Kim DH, Choi WG, Woo SI, Kwan J, Park KS, et al. Postcardiac injury syndrome after percutaneous coronary intervention. Yonsei Med J. 2010;51:284–6.
Imazio M, Hoit BD. Post-cardiac injury syndromes. An emerging cause of pericardial diseases. Int J Cardiol. 2013;168:648–52.
Liu Y, Wang C, Zhao R, Wan D, Xie H, Jin G, et al. Incidence and clinical characteristics of postcardiac injury syndrome complicating cardiac perforation caused by radiofrequency catheter ablation for cardiac arrhythmias. Int J Cardiol. 2013;168:3224–9.
Turitto G, Abordo MG Jr, Mandawat MK, Togay VS, El-Sherif N. Radiofrequency ablation for cardiac arrhythmias causing postcardiac injury syndrome. Am J Cardiol. 1998;81:369–70.
Tang RB, Liu XH, Dong JZ, Liu XP, Kang JP, Ma CS. Postcardiac injury syndrome complicating circumferential pulmonary vein radiofrequency ablation for atrial fibrillation. Chin Med. 2007;J120:1940–2.
Casula M, Andreis A, Avondo S, Imazio M. Post cardiac injury syndromes: diagnosis and management. Panminerva Med. 2021;63:270–5.
Acknowledgements
Not applicable.
Funding
The authors received no funding for this work.
Author information
Authors and Affiliations
Contributions
FAW and EHB conceived the manuscript and collected the data. FAW drafted the manuscript. MM, SW, DS, and EHB provided important intellectual content and critically reviewed the manuscript. All authors have contributed significantly. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The patient has provided written and informed consent to the publication of the article.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wenzl, F.A., Manninger, M., Wunsch, S. et al. Post-cardiac injury syndrome triggered by radiofrequency ablation for AVNRT. BMC Cardiovasc Disord 21, 611 (2021). https://doi.org/10.1186/s12872-021-02436-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-021-02436-1