Abstract
Objective
To estimate the association between the aggregation and pair-wise combination of selected cardiovascular risk factors (CVRF) and 10-year all-cause mortality.
Methods
Secondary data analysis of the PERU MIGRANT study, a prospective population-based cohort. Ten-year all-cause mortality was determined for participants originally enrolled in the PERU MIGRANT Study (baseline in 2007) through the National Registry of Identification and Civil Status. The CVRF included hypertension, type 2 diabetes mellitus, hypercholesterolemia, and overweight/obesity. Exposures were composed of both the aggregation of the selected CVRF (one, two, and three or more CVRF) and pair-wise combinations of CVRF. Cox regression models were used to calculate hazard ratios (HR) and 95% confidence intervals (95% CI).
Findings
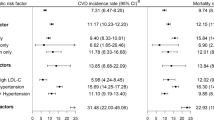
Of the 989 participants evaluated at baseline, 976 (98.8%) had information about vital status at 10 years of follow-up (9992.63 person-years), and 63 deaths were recorded. In the multivariable model, adjusting for sociodemographic and lifestyle variables, participants with two CVRF (HR: 2.48, 95% CI: 1.03–5.99), and those with three or more CVRF (HR: 3.93, 95% CI: 1.21–12.74) had higher all-cause mortality risk, compared to those without any CVRF. The pair-wise combinations associated with the highest risk of all-cause mortality, compared to those without such comorbidities, were hypertension with type 2 diabetes (HR: 11.67, 95% CI: 3.67–37.10), and hypertension with overweight/obesity (HR: 2.76, 95% CI: 1.18–6.71).
Conclusions
The aggregation of two or more CVRF and the combination of hypertension with type 2 diabetes or overweight/obesity were associated with an increased risk of 10-year all-cause mortality. These risk profiles will inform primary and secondary prevention strategies to delay mortality from cardiovascular risk factors.
Similar content being viewed by others
Introduction
Cardiovascular diseases represent the main cause of mortality worldwide. Of the total (17.7 million) estimated deaths worldwide from cardiovascular disease, more than three-quarters occurred in low- and middle-income countries (LMICs) [1]. These death rates are mainly driven by the presence of different cardiovascular risk factors, including high blood pressure, type 2 diabetes mellitus, obesity, and hypercholesterolemia [2]. However, in many cases, these cardiovascular risk factors are not in isolation, but aggregated with other chronic conditions, in a way that increases the risk of disability, development of cardiovascular events, and mortality.
Multimorbidity, defined as the presence of two or more chronic conditions without any one disease taking priority over the other, is still more common in high-income countries (HICs). Previous research conducted in developed countries found that the risk of mortality is higher among individuals with more than two diseases compared to disease-free individuals or those with one disease [3, 4]. In low- and middle-income countries, the risk of mortality due to multimorbidity is rapidly increasing [3], including Peru, where the prevalence of cardiovascular risk factors are in the rise [6, 7]. Despite the burden of multimorbidity in LMICs, the characterization and long-term consequences of having multiple chronic conditions remain largely unknown. As a result, medical care in LMICs often focuses on treating one disease rather than multiple diseases at once.
Current evidence evaluates the potential effect of multimorbidity on disability and mortality, but do not determine which of the risk factors or chronic conditions are really associated with important outcomes. Evaluating which combination of conditions occurs more frequently and is associated with worse outcomes, such as mortality, should be particularly important in LMICs. Understanding which higher-risk combinations should be target will help allocate resources more efficiently, especially in resource-constrained settings. Although some cohort studies have explored which are the most prevalent and lethal combinations of chronic conditions, one of them explored two to five diseases [8], whereas another one explored two and three conditions [9]. Moreover, the first study included individuals aged ≥ 65 years and the second study included a limited sample of individuals ≥ 85 years [9]. Thus, multimorbidity is not only a problem for the elderly and in order to intervene efficiently it is necessary to focus on the general population.
Cardiovascular risk factors are associated with lifestyle and have changed rapidly in recent decades, some driven by urbanization [10]. Environmental changes and population flows have led to increased urbanization around the world, especially in low- and middle-income countries. The degree of urbanization is closely related to the distinctive characteristics of the health profile of rural and urban inhabitants, as well as of migrants from rural to urban areas, causing in the latter group a change in their lifestyle. The multimorbidity profile of these migrant groups is largely unknown and needs to be further examined.
Therefore, in order to provide evidence on the long-term effects of multimorbidity in LMICs, we aimed to estimate the 10-year all-cause mortality risk associated with the aggregation of selected cardiovascular risk factors. In addition, we also evaluated the strength and magnitude of the association between each pair-wise combination of these cardiovascular risk factors and the all-cause mortality risk.
Materials and methods
Study design
The PERU MIGRANT Study is a prospective population-based cohort [4], that was established to assess the risk factors of cardiovascular disease in three population groups in Peru: urban dwellers, who were born and currently live in Pampas de San Juan de Miraflores, a periurban area in Lima; rural inhabitants from San José de Secce and Chacas in Ayacucho (highlands settings); and rural-to-urban migrants, inhabitants born in Ayacucho (rural) who migrated to Pampas de San Juan de Miraflores (urban).
Participants
Participants were recruited from 2007 to 2008 using a random sampling technique stratified by sex and age (30–39, 40–49, 50–59 and 60 + years) in each population group using household census data [4]. For all study groups, men and women ≥ 30 years of age and habitual residents (≥ 6 months) of the study area were considered eligible. Pregnant women and people with mental disorders that prevented them from giving informed consent were excluded.
Following a random selection process, participants were invited to participate. They provided consent to participate in the study, completed a questionnaire, and had their anthropometric measurements assessed [4]. Survival data were retrieved through the National Registry of Identification and Civil Status (RENIEC) information to ascertain vital status and date of death (or censoring) when relevant.
Variables
Outcome
All-cause mortality at 10 years of follow-up was the outcome of interest. After the RENIEC database was searched, participants were classified as alive or dead. Those participants who were not available in that database (i.e. their national identity number was incorrectly recorded), were considered censored at the last time of contact (i.e. first or second in-person follow-up) [5, 6].
Independent variables
Aggregation and pair-wise combinations of cardiovascular risk factors were the independent variables. Risk factors included hypertension, type 2 diabetes mellitus, hypercholesterolemia, and overweight/obesity. These chronic cardiovascular risk factors were studied at baseline following standard procedures for all participants [4]. Hypertension was defined as systolic blood pressure (SBP) ≥ 140 mm Hg, diastolic blood pressure (DBP) ≥ 90 mm Hg or self-reported diagnosis with the use of anti-hypertensive medications [7]. Type 2 diabetes mellitus was defined based on fasting blood glucose ≥ 126 mg/dl or self-reported diagnosis with the use of anti-diabetic medications [8]. Overweight/obesity was defined as a body mass index (BMI) ≥ 25 kg/m2 [9]. Hypercholesterolemia was defined as total cholesterol ≥ 200 mg/dl [10], and was assessed from blood samples drawn after an 8-h fasting period.
We examined mortality rates with different cardiovascular risk profiles. In the first part, cardiovascular risk factors were aggregated and then split into one, two, and three or more cardiovascular risk factors. On the other hand, the second part comprised six groups of analysis with selected cardiovascular risk factors (e.g., group 1: hypertension with type 2 diabetes mellitus; group 2: hypertension with hypercholesterolemia, etc.) Each group was evaluated in four categories: disease-free individuals (reference), people with only one disease (e.g., only hypertension and only type 2 diabetes mellitus), and the pair-wise combination (e.g., hypertension with type 2 diabetes mellitus). The rationale of using this approach was to capture the individual effect of each chronic condition in addition with the pair-wise combination using the same model, and in this way, avoiding misclassification bias.
Covariables
Other variables were included in the analysis as potential confounders. Sociodemographic variables included age (30–39, 40–49, 50–59, and 60 + years), sex, migrant status (rural, migrant or urban), education level (< 7 years of education vs. ≥ 7 years of education), and socioeconomic status (low, medium, or high), measured using a wealth index based on household income, assets and household facilities. Lifestyle variables included tobacco use (having smoked at least one cigarette per day compared to never users in the 6 months prior to the interview, and classified as yes or no), alcohol consumption (self-reported consumption of ≥ 6 beers or its equivalent in alcohol with other beverages on the same occasion at least once a month, and classified into low or high), HDL cholesterol (> HDL-c 40 mg/dl in men and > 50 mg/dl in women) [10], and high waist circumference (> 80 cm in women and > 90 cm in men) [11].
Statistical analysis
The statistical analysis was conducted in STATA 14 for Windows (STATA Corp, College Station, TX, USA). The characteristics of the study population were tabulated according to the population group at baseline, and Chi-squared tests were used to compare categorical variables.
For the bivariate analysis, the log rank test was used to evaluate the association between sociodemographic variables, lifestyles, each cardiovascular risk factor, and aggregated cardiovascular risk factors and all-cause mortality. The Cox proportional hazard model was used to estimate the effect of the aggregation of cardiovascular risk factors on all-cause mortality. Crude and adjusted models were computed. Adjusted models included sociodemographic and lifestyle variables.
The association between the pair-wise combinations of cardiovascular risk factors and all-cause mortality were evaluated separately using crude and adjusted Cox regression models. Adjusted models included sociodemographic and lifestyles variables, as well as the cardiovascular risk factors not included in the pair-wise combination. Cox regression assumptions of independent observations, and independent censorship of survival and proportional risks were assessed. The latter assumption was evaluated using the global test of Schoenfeld residuals. Given the number of confounding variables, the variance inflation factor was also utilized to evaluate the presence of collinearity.
Results
Characteristics of the study population
We analyzed the data of 989 participants included at baseline. Mean age was 47.9 years (SD: 12.0), and 52.8% of the cohort was female. Regarding population groups, 201 (20.3%), 589 (59.6%), and 199 (20.1%) were rural, rural-to-urban migrants, and urban participants, respectively (Table 1).
Prevalence of multimorbidity at baseline and 10-year all-cause mortality
At baseline, the prevalence of multimorbidity was 31.6% (95% CI: 28.7%–34.6%). Two cardiovascular risk factors were present in 25.0% (95% CI: 22.4%–27.8%) of the study population. Three or more risk factors were present in 6.6% (95% CI: 5.3%–8.5%). These estimates were higher in the urban group than in the other two population groups (Table 1).
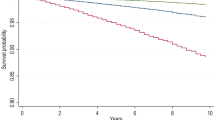
At 10-years of follow-up, the mortality incidence of 976 (98.8%; 9992.6 person-years) participants was assessed. There were 63 deaths, resulting in an overall mortality rate of 6.3 (95% CI: 4.9–8.1) per 1,000 person-years, distributed as follows: 9.1 (95% CI: 5.7–14.4) in the rural group, 6.4 (95% CI: 3.7–11.1) in the urban group, and 5.3 (95% CI: 3.8–7.5) in the rural to urban migrant group. Male sex, older age, low education level, low asset index, high waist circumference, type 2 diabetes, and hypertension were characteristics associated with higher all-cause mortality (Additional file 1: Table S1).
Aggregation and pair-wise combinations of cardiovascular risk factors and 10-year all-cause mortality
The population characteristics according to vital status are shown in Additional file 1: Table S1). In the multivariate models adjusting for sociodemographic and lifestyle variables, participants with two cardiovascular risk factors had more than twice all-cause mortality risk compared to those without cardiovascular risk factors. Similarly, people with three or more cardiovascular risk factors had almost four times higher all-cause mortality risk than those without any cardiovascular risk factors (Table 2 & Additional file 1: Table S2).
When pair-wise combinations were assessed, subjects with hypertension and type 2 diabetes had a 12-fold increase in the risk of all-cause mortality compared to those without any of these conditions. In the same model, hypertension alone doubled such risk. On the other hand, subjects with hypertension and overweight/obesity together had almost three times the risk of all-cause mortality, whereas hypertension alone increased such risk on 3.2 times (Table 3 & Additional file 1: Table S3).
Discussion
In our study conducted in a low-resource LMIC setting, we found that several aggregation or combination patterns of cardiovascular risk factors were strongly associated with an increased 10-year all-cause mortality risk. Of note, the combination of hypertension and type 2 diabetes mellitus had a tenfold higher risk of mortality, whereas hypertension and overweight/obesity increased the 10-year all-cause mortality risk up to nearly four-fold. Additionally, having two or more cardiovascular risk factors was associated with a greater risk of mortality.
Previous studies have examined the risk of mortality among individuals with two or more chronic conditions compared to those who were free of disease. Three independent conditions, i.e., diabetes mellitus, stroke, and myocardial infarction, have been associated with a similar increase in the risk of mortality, but their aggregation had a multiplicative effect on the risk of death [12]. Another recent study found that the risk of mortality associated with more than four chronic conditions was the same for each condition evaluated individually [13]. Our study, despite having evaluated a limited number of cardiovascular conditions, shows an additive effect for each additional cardiovascular risk factor as well as varying additive effects with different conditions. The effect of the aggregation of cardiovascular factors risk on mortality risk may be explained by the duration and severity of each additional risk factor [14].
We found that the co-occurrence of several pairs of diseases had a multiplicative effect on the all-cause mortality risk. Hypertension-type 2 diabetes mellitus was associated with a twelve-fold higher all-cause mortality risk compared to a nearly three-fold risk in the case of hypertension and overweight/obesity. Our estimates were similar to those reported by other studies, in which cardiovascular mortality was elevated among individuals with type 2 diabetes mellitus and hypertension [15,16,17]. However, our findings differ with those reported by a meta-analysis, which demonstrated that high systolic blood pressure plus high serum cholesterol substantially increased cardiovascular mortality risk [18]. In this study, hypercholesterolemia, and its co-occurrence with type 2 diabetes mellitus, overweight/obesity and hypertension had a minimal effect. Perhaps these comorbidities attenuated the proportional effects of hypercholesterolemia on the risk of mortality. Our results also showed a non-significant association between overweight/obesity and type 2 diabetes mellitus and mortality risk. Additionally, hypertension was associated with a higher mortality risk alone compared to when it co-occurred with certain cardiovascular risk factors (e.g., hypertension with overweight/obesity and hypertension with hypercholesterolemia). However, when hypertension was combined with type 2 diabetes mellitus, it resulted in a multiplicative mortality risk. The consistency of our findings has been reported in other studies [19, 20]. A possible explanation for this finding is that inadequate control of hypertension and diabetes increases the likelihood of life-threatening complications and mortality. Therefore, the data presented highlights the need for primary prevention of both hypertension and the combination of hypertension with other cardiovascular risk factors.
The results of the prevalence of multiple conditions in LMICs vary. In this study, we evaluated the four most common chronic conditions in LMICs. Despite the limited number of chronic conditions chosen, the overall proportion of people with multimorbidity was high (25%), especially among urban dwellers. Our estimates of multimorbidity were similar to those reported in a study conducted in six LMICs [21], as well as others carried out in Scotland [22], and the Netherlands [23, 24]. However, the prevalence of multimorbidity was lower compared to a recent study that included nine HICs. In this study, the authors used 12 of the most prevalent chronic conditions, and the data collection was performed between 2007 and 2012. The highest frequency of multimorbidity was observed in Russia (71.9%) and the lowest in China (45.1%) [25]. The variability in multimorbidity between studies can be attributed in part to the definition of multimorbidity used in each study, as there is a lack of consensus regarding it. The Academy of Medical Sciences has suggested using “the presence of two or more chronic conditions without any one disease taking priority over the other” [3], and our analysis has applied that definition, but only for four conditions. Differences could also be due to the number of conditions included in that definition; socioeconomic differences resulting in lifestyle changes (e.g. improved transit that leads to less physical activity), sociodemographic differences between countries such as age and sex distribution, and the country’s phase of epidemiological and nutritional transition (e.g., greater exposure to fast foods) [25,26,27,28]. Due to this, it is necessary to conduct country-specific studies to better characterize and understand the epidemiology of multimorbidity. Currently, the provision of medical care in many LMIC settings is largely based on the treatment of individual diseases. Additionally, although there are available guidelines for the treatment of people with multiple morbidities [29], it is necessary that these guidelines include care and treatment for people with LMIC-specific multimorbidity [30].
One of the main strengths of this study is the 10-year follow-up in a LMIC setting and the use of a national records (RENIEC) database to obtain information about the number and date of deaths, thereby decreasing the differential classification bias. Additionally, participants were evaluated with standardized instruments and procedures. Also, lost to follow up rates were very low (i.e., 1·2% of the total study population). Finally, we reduced misclassification bias by using four categories for each pair-wise combination instead of using only two (having or nor having the two conditions).
This study also has limitations. The limited number of deaths, despite the 10 years of follow-up, provides point estimates with wide confidence intervals. In addition, only four chronic cardiovascular conditions (hypertension, type 2 diabetes, hypercholesterolemia, and overweight/obesity) were evaluated at baseline, which limits a more detailed exploration of the potential effect of other conditions on mortality. Moreover, new cases of hypertension, type 2 diabetes or hypercholesterolemia, or the variation of BMI over time was not considered. Besides, cardiovascular death should have been ideally the outcome of interest. However, specific cause of death was not available. Finally, our biostatistical models only adjusted for main sociodemographic and lifestyle factors as confounding variables. We did not include other factors, such as race, in our baseline analysis.
Conclusion
After a 10-year follow-up period, we observed a higher risk of all-cause mortality when more cardiovascular risk factors were present. Additionally, the pair-wise combinations of hypertension and type 2 diabetes mellitus and hypertension and overweight/obesity had the highest risks of death. These results suggest the need for better interventions targeted at people with multiple chronic conditions in LMIC settings.
Availability of data and materials
The datasets used for this study are available from the corresponding author.
References
World Health Organization. Cardiovascular diseases [Internet]. Geneva: World Health Organization: World Health Organization; 2015 [cited 2017 Apr 24]. http://www.who.int/mediacentre/factsheets/fs317/es/.
World Health Organization. Global Health Risks: Mortality and burden of disease attributable to selected major risks [Internet]. Switzerland: World Health Organization; 2009 [cited 2019 Jul 8]. https://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf.
Singh-Manoux A, Fayosse A, Sabia S, Tabak A, Shipley M, Dugravot A, et al. Clinical, socioeconomic, and behavioural factors at age 50 years and risk of cardiometabolic multimorbidity and mortality: a cohort study. PLoS Med. 2018;15(5):e1002571.
Zhang D, Tang X, Shen P, Si Y, Liu X, Xu Z, et al. Multimorbidity of cardiometabolic diseases: prevalence and risk for mortality from one million Chinese adults in a longitudinal cohort study. BMJ Open. 2019;9(3):e024476.
Academy of Medical Sciences. Multimorbidity: a priority for global health research [Internet]. London: Academy of Medical Sciences; 2018 [cited 2019 Jul 14]. https://acmedsci.ac.uk/file-download/99630838.
Villarreal-Zegarra D, Carrillo-Larco RM, Bernabe-Ortiz A. Short-term trends in the prevalence, awareness, treatment, and control of arterial hypertension in Peru. J Hum Hypertens. 2020;28(12):1462–536.
Carrillo-Larco RM, Bernabé-Ortiz A. Diabetes mellitus tipo 2 en Perú: una revisión sistemática sobre la prevalencia e incidencia en población general. Rev Peru Med Exp Salud Publica. 2019;36(1):26–36.
Caughey GE, Ramsay EN, Vitry AI, Gilbert AL, Luszcz MA, Ryan P, et al. Comorbid chronic diseases, discordant impact on mortality in older people: a 14-year longitudinal population study. J Epidemiol Community Health. 2010;64(12):1036–42.
Ferrer A, Formiga F, Sanz H, Almeda J, Padrós G. Multimorbidity as specific disease combinations, an important predictor factor for mortality in octogenarians: the Octabaix study. Clin Interv Aging. 2017;27(12):223–31.
Patil RR. Urbanization as a determinant of health: a socioepidemiological perspective. Soc Work Public Health. 2014;29(4):335–41.
Miranda JJ, Gilman RH, García HH, Smeeth L. The effect on cardiovascular risk factors of migration from rural to urban areas in Peru: PERU MIGRANT Study. BMC Cardiovasc Disord. 2009;9(1):23.
Miranda JJ, Gilman RH, Smeeth L. Differences in cardiovascular risk factors in rural, urban and rural-to-urban migrants in Peru. Heart. 2011;97(10):787–96.
Carrillo-Larco RM, Ruiz-Alejos A, Bernabé-Ortiz A, Gilman RH, Smeeth L, Miranda JJ. Cohort Profile: the PERU MIGRANT Study—a prospective cohort study of rural dwellers, urban dwellers and rural-to-urban migrants in Peru. Int J Epidemiol. 2017;46(6):1752–1752f.
O’Brien E, Waeber B, Parati G, Staessen J, Myers MG. Blood pressure measuring devices: recommendations of the European Society of Hypertension. BMJ. 2001;322(7285):531–6.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2011;34(Suppl 1):S62-9.
National Institutes of Health. The Practical Guide Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Heart, Lung and Blood Institute: NIH Publication No. 00-4084; 2000.
Grundy S, Becker D, Clark LT, Cooper RS, Denke MA, Howard J, et al. Third Report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) Final Report [Internet]. Washington: American Heart Association; 2002. http://www.cverdad.org.pe/ingles/ifinal/conclusiones.php.
World Health Organization. Waist circumference and waist-hip ratio: report of a WHO expert consultation [Internet]. Geneva: World Health Organization; 2008 [cited 2019 Mar 14]. 47 p. www.who.int.
Emerging Risk Factors Collaboration TERF, Di Angelantonio E, Kaptoge S, Wormser D, Willeit P, Butterworth AS, et al. Association of cardiometabolic multimorbidity with mortality. JAMA. 2015;314(1):52–60.
Marengoni A, von Strauss E, Rizzuto D, Winblad B, Fratiglioni L. The impact of chronic multimorbidity and disability on functional decline and survival in elderly persons. A community-based, longitudinal study. J Intern Med. 2009;265(2):288–95.
Cornoni-Huntley JC, Foley DJ, Guralnik JM. Co-morbidity analysis: a strategy for understanding mortality, disability and use of health care facilities of older people. Int J Epidemiol. 1991;20(Suppl 1):S8-17.
Afsharian S, Akbarpour S, Abdi H, Sheikholeslami F, Moeini AS, Khalili D, et al. Risk factors for cardiovascular disease and mortality events in adults with type 2 diabetes—a 10-year follow-up: Tehran Lipid and Glucose Study. Diabetes Metab Res Rev. 2016;32(6):596–606.
Bozorgmanesh M, Hadaegh F, Mohebi R, Ghanbarian A, Eskandari F, Azizi F. Diabetic population mortality and cardiovascular risk attributable to hypertension: a decade follow-up from the Tehran Lipid and Glucose Study. Blood Press. 2013;22(5):317–24.
Sehestedt T, Hansen TW, Li Y, Richart T, Boggia J, Kikuya M, et al. Are blood pressure and diabetes additive or synergistic risk factors? Outcome in 8494 subjects randomly recruited from 10 populations. Hypertens Res. 2011;34(6):714–21.
Asia Pacific Cohort Studies Collaboration. Joint effects of systolic blood pressure and serum cholesterol on cardiovascular disease in the Asia Pacific region. Circulation. 2005;112(22):3384–90.
Zafari N, Asgari S, Lotfaliany M, Hadaegh A, Azizi F, Hadaegh F. Impact of hypertension versus diabetes on cardiovascular and all-cause mortality in Iranian older adults: results of 14 years of follow-up. Sci Rep. 2017;7(1):1–8.
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–13.
Lee JT, Hamid F, Pati S, Atun R, Millett C. Impact of noncommunicable disease multimorbidity on healthcare utilisation and out-of-pocket expenditures in middle-income countries: cross sectional analysis. PLoS ONE. 2015;10(7):e0127199.
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43.
Schellevis FG, van der Velden J, van de Lisdonk E, van Eijk JT, van Weel C. Comorbidity of chronic diseases in general practice. J Clin Epidemiol. 1993;46(5):469–73.
Uijen AA, van de Lisdonk EH. Multimorbidity in primary care: prevalence and trend over the last 20 years. Eur J Gen Pract. 2008;14(sup1):28–32.
Garin N, Koyanagi A, Chatterji S, Tyrovolas S, Olaya B, Leonardi M, et al. Global multimorbidity patterns: a cross-sectional, population-based, multi-country study. J Gerontol Ser A Biol Sci Med Sci. 2016;71(2):205–14.
Carvalho J, Roncalli Â, Cancela M, Souza D. Prevalence of multimorbidity in the Brazilian adult population according to socioeconomic and demographic characteristics. PLoS ONE. 2017;12(4):e0174322.
Nimako BA, Baiden F, Sackey SO, Binka F. Multimorbidity of chronic diseases among adult patients presenting to an inner-city clinic in Ghana. Global Health. 2013;9:61.
Pati S, Swain S, Metsemakers J, Knottnerus JA, van den Akker M. Pattern and severity of multimorbidity among patients attending primary care settings in Odisha, India. PLoS ONE. 2017;12(9):e0183966.
National Institute for Health and Care Excellence. Multimorbidity: clinical assessment and management. London: National Institute for Health and Care Excellence; 2016. p. 23.
Hurst JR, Dickhaus J, Maulik PK, Miranda JJ, Pastakia SD, Soriano JB, et al. Global alliance for chronic disease researchers’ statement on multimorbidity. Lancet Global Health. 2018;6:e1270-1.
Acknowledgements
Our special thanks to several colleagues at the Universidad Peruana Cayetano Heredia and A.B. PRISMA in Lima, Peru, and several others in the United Kingdom, as well as the staff and team of field workers who contributed to different parts of this study. Most importantly, our sincere gratitude extends to the people who agreed to participate in the study, and to Candice Romero and Lilia Cabrera, who coordinated the fieldwork phase of this study. We also thank David Villarreal-Zegarra for collecting data on the vital status of the participants in the RENIEC offices.
Funding
The PERU MIGRANT Study was funded through a Wellcome Trust Master Research Training Fellowship and a Wellcome Trust PhD Studentship to J.J.M. (074833/Z/04/A). The first follow-up evaluation was funded by Universidad Peruana Cayetano Heredia (Competitive Fund 20205071009). The second follow-up evaluation was funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, through the GloCal Health Fellowship Program from the University of California Global Health Institute. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. All authors collectively had final responsibility for the decision to submit for publication. The authors alone are responsible for the opinions in the manuscript, which do not necessarily represent those of their institutions. In relation to the funding of the authors: JJM acknowledges having received support from the Alliance for Health Policy and Systems Research (HQHSR1206660), the Bernard Lown Scholars in Cardiovascular Health Program at Harvard T.H. Chan School of Public Health (BLSCHP-1902), Bloomberg Philanthropies, FONDECYT via CIENCIACTIVA/CONCYTEC, British Council, British Embassy and the Newton-Paulet Fund (223-2018, 224-2018), DFID/MRC/Wellcome Global Health Trials (MR/M007405/1), Fogarty International Center (R21TW009982, D71TW010877), Grand Challenges Canada (0335-04), International Development Research Center Canada (IDRC 106887, 108167), Inter-American Institute for Global Change Research (IAI CRN3036), Medical Research Council (MR/P008984/1, MR/P024408/1, MR/P02386X/1), National Cancer Institute (1P20CA217231), National Heart, Lung and Blood Institute (HHSN268200900033C, 5U01HL114180, 1UM1HL134590), National Institute of Mental Health (1U19MH098780), Swiss National Science Foundation (40P740-160366), Wellcome (074833/Z/04/Z, 093541/Z/10/Z, 107435/Z/15/Z, 103994/Z/14/Z, 205177/Z/16/Z, 214185/Z/18/Z) and the World Diabetes Foundation (WDF15-1224). Rodrigo M Carrillo-Larco has been supported by a Strategic Award, Wellcome Trust-Imperial College Centre for Global Health Research [100693/Z/12/Z], and Imperial College London Wellcome Trust Institutional Strategic Support Fund (Global Health Clinical Research Training Fellowship) [294834/Z/16/Z ISSF ICL]. Rodrigo M Carrillo-Larco is supported by a Wellcome Trust International Training Fellowship [214185/Z/18/Z].
Author information
Authors and Affiliations
Contributions
AB-O, RMC-L, RHG, LS and JJM conceived, designed and supervised the overall study. JB-P and AB-O developed the idea for this manuscript. JB-P and AB-O led the statistical analysis. JB-P drafted the first version of the paper. All authors participated in writing the manuscript, provided important intellectual content and gave their final approval of the submitted version. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The PERU MIGRANT Study was approved by the Institutional Review Board at Universidad Peruana Cayetano Heredia (UPCH) in Peru (approval number: 60014) and the London School of Hygiene and Tropical Medicine in the United Kingdom. This secondary analysis was approved by the ethics committee at UPCH (approval number: 101118). Data analyzed for this study were de-identified. Also, written informed consent was provided by all participants. This consent was previously approved by the Institutional Review Boards.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Aggregation and pair-wise combinations of cardiovascular risk factor and 10-year all-cause mortality.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bazalar-Palacios, J., Jaime Miranda, J., Carrillo-Larco, R.M. et al. Aggregation and combination of cardiovascular risk factors and their association with 10-year all-cause mortality: the PERU MIGRANT Study. BMC Cardiovasc Disord 21, 582 (2021). https://doi.org/10.1186/s12872-021-02405-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-021-02405-8