Abstract
Background
In Uganda, few children with congenital heart diseases (CHD) benefit from early corrective cardiac surgery. These children are at high risk of developing heart failure and electrolyte imbalances; factors which increase their risk of developing arrhythmias. This study aimed to determine the prevalence and factors associated with arrhythmias among children with congenital heart diseases receiving care at Mulago Hospital.
Methods
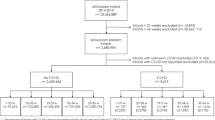
This was a cross-sectional study carried out from August 2013 to March 2014 at Mulago Hospital. Children were consecutively enrolled into the study. Standard 12-lead electrocardiograms (ECGs) were performed on 194 children with CHD (age range 10 days–15 years). Data was analysed using SPSS 16.0.
Results
Out of 194 children studied, 53/194 (27.3 %, 95 % CI 21.0 – 33.6) children had arrhythmias. Of the CHD children, 44/194 (22.7 %, 95 % CI 16.8 – 28.6) had first degree AV block while 9/194 (4.6 %, 95 % CI 1.7 – 7.6) children had either ectopic atrial rhythm, premature atrial contractions, junctional rhythm, complete atrioventricular (AV) dissociation or premature ventricular contractions. Children using digoxin were more likely to have first degree AV block (OR 3.75, 95 % CI 1.60–8.86) while those aged 5 years and below were less likely to have first degree AV block (OR 0.16, 95 % CI 0.07–0.37).
Conclusion
Arrhythmias are common among children with CHD receiving care from Mulago Hospital. These are associated with digoxin use, child’s age and electrolyte imbalances; factors which can easily be assessed, managed and where possible modified in these children during their care.
Similar content being viewed by others
Background
Children with congenital heart diseases (CHD) commonly develop arrhythmias. If they are not identified early and managed appropriately, the arrhythmias contribute to morbidity and mortality among these children [1]. The arrhythmias are a result of either co-existing congenital abnormalities of the specialized conduction system or in response to hemodynamic influences on chamber dimensions, muscle mass and metabolism of myocardial tissue [2].
In low resource countries, very few children with CHD get early corrective heart surgery [3]. Due to delayed surgery, these children develop many complications such as heart failure, severe cyanosis and other long-term sequelae which increase their risk of developing arrhythmias [4]. In addition, children in low resource settings are at an increased risk of malnutrition, HIV and electrolyte imbalances; factors which are known to increase the risk of developing arrhythmias [5–7].
There is currently limited data on the magnitude of arrhythmias among children with congenital heart diseases in low resource countries due to limited access to electrocardiography services in these countries. In Uganda, electrocardiography is not offered as part of the routine care of children with congenital heart diseases because of its limited availability and high cost. We therefore conducted a cross-sectional study to determine the prevalence and factors associated with arrhythmias among children with congenital heart diseases receiving care at Mulago National Referral Hospital, Kampala.
Methods
Study site and population
Mulago National Referral Hospital is located in Kampala, the capital city of Uganda. The hospital has the Uganda Heart Institute which employed the only two paediatric cardiologists in the country at the time when the study was carried out. Children with congenital heart diseases from different parts of the country receive care from this hospital.
Children with congenital heart diseases who presented to the hospital between the period of August 2013 and March 2014 were consecutively enrolled into the study. We included all children aged 0–15years with congenital heart disease confirmed on echocardiography by a qualified paediatric cardiologist.
Sample size calculation
The number of participants was generated using the Kish Leslie (1965) formula for cross-sectional studies [8]. Prevalence of arrhythmias among children with congenital heart disease in other studies ranges from 6.3 % (before surgery) to 12 % (in the late post-operative follow up period) [9]. The sample size required, n, was calculated using the formula n = pqz2/d2, where p is the prevalence of arrhythmias among children with congenital heart defects (p = 0.12); q = 1-p; z is 1.96 (for 5 % alpha error); and d is precision which is 0.05 (permissible margin of error at 5 % level of statistical significance). This gave a total of 162 children with congenital heart defects. We incorporated a non-response rate/missing data of 20 % [10] and this gave a total required study population of 194 children.
Data collection
Standardized pretested and pre – coded interviewer – administered data collection tools were used in data collection. Data collection was done by the principal investigator (AB) and a research assistant who was a medical officer with two years of experience in management of children with heart diseases.
Clinical history
Information collected included child’s social demographic characteristics and information concerning the medication the child was using in the period one week prior to the interview (heart failure medication). All children who were enrolled into the study were assessed for features of heart failure by the principal investigator or research assistant. The severity of heart failure was graded using the modified Ross score. Patients with a score of 0 to 6 were classified as no or mild heart failure while those with a score of above 6 were classified as having moderate or severe heart failure [11, 12].
Laboratory investigations
A complete blood count was done for each child using a Celltac E MEK-7222 automatic hematology analyzer. The World Health Organization age specific values for hemoglobin levels were used to classify children as having mild, moderate or severe anaemia [13]. We analysed serum electrolytes using automated clinical chemistry analyzer (Cobas® Integra 400 plus model Roche, Germany). Interpretation of serum electrolyte values was made with reference to age specific reference values described by Pesce 2007 [14].
We tested all children for HIV using standard rapid testing kits. The procedure involved an initial screen Alere™ HIV-1/2 Determine® followed by STAT-PAK® HIV-1/2; the third rapid test Uni-Gold™ Recombigen® HIV was used as a tie breaker. For children under 18 months with a positive HIV serology test and of unknown HIV status (children without an HIV DNA PCR report done in the past 3 months), blood was sent for DNA PCR to confirm presence or absence of HIV.
Electrocardiography procedure
The electrocardiography was conducted using ECG machines (Mortara ELI 350 model, USA and MCA 1200 model, USA). Standard 12-lead electrocardiography was performed in supine position (at 25 mm/s. and voltage of 10 mm/mV). ECGs were carried out by a technician who is a professional nurse working with the Uganda Heart Institute; she was trained in the study methodologies before the start of the study. The electrocardiograms were interpreted by two paediatric cardiologists (PL and SL). Each electrocardiograph was read and interpreted by any one of the cardiologists who was available on duty on a given day during the study period; and the cardiologist’s interpretation was taken as the final interpretation for a given ECG.
Statistics
Data was entered using Epi data version 2.1b and then exported to SPSS 16.0 for analysis. Descriptive statistics were generated as frequencies and distributions. Associations were derived between the independent and the outcome variables (arrhythmias). At bivariate analysis, factors with a p value less than 0.2 were entered into the final logistic regression model using a model of 7 events per variable [15] and analysed using the backward likelihood ratio approach. Variables with p values less than 0.05 were considered significant.
Results
Baseline characteristics
A total of 194 children aged 10 days to 15 years were recruited (median age 2.4 years, IQR 1- 5.3). Only 2 children (1 %) were HIV positive and none of them was on antiretroviral therapy. Majority of the children 111 (57.2 %) were female. A large number of the children presented with ventricular septal defects 48/194 (24.7 %), patent ductus arteriosus 38/194 (19.6 %) and tetralogy of Fallot 25/194 (12.9 %) as shown in Table 1. In total, these three diagnoses constituted 57.2 % of the congenital heart diseases among the children. Majority of the children had a single heart anomaly 163/194 (84 %) while fewer children 31/194 (16 %) had multiple structural heart anomalies as shown in Tables 1 and 2.
Arrhythmias among the children with congenital heart disease
Arrhythmias were found in 53/194 (27.3 %, 95 % CI 21.0 – 33.6) children as shown in Table 3. Of these children, 44/194 (22.7 %, 95 % CI 16.8 – 28.6) had first degree AV block while 9/194 (4.6 %, 95 % CI 1.7 – 7.6) had either ectopic atrial rhythm, premature atrial contractions, junctional rhythm, complete atrioventricular (AV) dissociation or premature ventricular contractions; the clinical and laboratory characteristics of these children are shown in Table 4.
Of the children who had first degree AV block, all had never had corrective heart surgery, none of them had hypercalcemia and all were HIV negative. At bivariate analysis, factors that were associated with first degree AV block included age 5 years and below, use of digoxin and hypokalemia as shown in Tables 5 and 6. At adjusted analysis, factors that were associated with first degree AV block were digoxin use (OR 3.75, 95 % CI 1.60–8.86) and age 5 years and below (OR 0.16, 95 % CI 0.07–0.37) as shown in Table 7.
Discussion
In this study, arrhythmias were found in 27.3 % of children; with 22.7 % having first degree AV block while 4.6 % had either ectopic atrial rhythm, premature atrial contractions, junctional rhythm, complete atrioventricular (AV) dissociation or premature ventricular contractions (PVCs). This prevalence of arrhythmias with the exception of first degree AV block is comparable to a study by Ringel and colleagues 1984 who detected arrhythmias in 4/64 (6.3 %) children (age one week to 16 years) with congenital heart disease attending University of Merryland hospital [9]. However, this prevalence is lower than the prevalence of arrhythmias detected by holter ECGs, which show a prevalence of up to 41.2 % in infants and children with congenital heart diseases before surgical correction of the heart defects [16]. Holter ECGs are not readily available in Uganda and other developing countries and thus the use of standard 12 lead ECG is employed.
Complete AV dissociation, a life threatening arrhythmia was detected in one child (0.5 %). This arrhythmia in association with structural heart disease has a case fatality rate of 29 % in infancy and 10 % in childhood [17]. Complete AV dissociation has been described in children with L-TGA and in children with CAVC [18, 19]. However, in our study this arrhythmia was found in a child with TOF. There is limited literature on occurrence of complete AV dissociation in children with TOF although studies have describe this arrhythmia among fetuses with TOF [20, 21]. This child with complete AV dissociation had normal serum electrolytes (sodium, potassium, magnesium and total serum calcium) implying that imbalances of these serum electrolytes had no role in predisposing the child to complete AV dissociation.
In our study, prevalence of ectopic atrial rhythm was 1.5 %, PACs 1.5 %, junctional rhythm 0.5 % and that of PVCs was 0.5 %. Similar studies among children with congenital heart diseases detected comparable prevalence of these arrhythmias. Prevalence of PVCs being at 1.5 % among children with congenital heart diseases [9]. Ectopic atrial rhythm has been reported in children with TOF at a prevalence of 1/15 (6.7 %) [22]. PVCs have been described in children with VSD and CAVC while PACs and junctional rhythm have been reported in individuals with TGA [19, 23].
The three children with PACs in our study had either normal or mild electrolyte imbalances (one had mild hypernatraemia for age while the second child mild hypernatraemia and mild hypermagnesaemia) which may not have predisposed these children to having PACs.
Significant electrolyte imbalances were seen in a child with ectopic atrial rhythm (hypermagnesaemia, severe hypokalemia and severe hypocalcemia) and the child with PVCs (severe hyponatraemia and severe hypocalcemia). Hypermagnesemia is rare in children and it is often iatrogenic following excessive intake of magnesium. There is limited data on association of hypermagnesimia with ectopic atrial rhythms although some reports have associated hypermagnesemia with first degree AV block [24]. Arrhythmias associated with hypokalemia include a prolonged QT interval, ventricular extrasystoles, and malignant ventricular arrhythmias such as ventricular tachycardia, torsades de pointes and ventricular fibrillation [25]. There are no previous reports associating ectopic atrial rhythm with hypokalemia. However, in patients with underlying heart disease, even mild-to-moderate hypokalemia increases their likelihood of cardiac arrhythmias [26], and this could therefore have predisposed this child to development of an atrial rhythm. Hypocalcaemia causes prolongation of QTc interval and this is directly proportional to the degree of hypocalcaemia [27], there are no reports which associate hypocalcemia with ectopic atrial rhythm or PVCs. This may thus mean that hypocalceamia may not have had any role in predisposing these children to ectopic atrial rhythm and PVCs. The child with PVCs had severe severe hyponatraemia in addition to severe hypocalcemia. Patients with hyponatremia are more prone to cardiac arrhythmias [28] and thus this might have increased the risk of this child developing PVCs.
In our study, prevalence of first degree AV block was 22.7 %. A higher prevalence of first degree AV block (44.4 %) among children and young adults with congenital heart diseases was described by Waldo and colleagues, 1974 in New York [29]. Waldo and colleagues studied 30 children and young adults of ages 2 years to 25 years with various congenital heart diseases. The higher prevalence of first degree AV block in their study compared to the prevalence we have found in our study could be due to the difference in the age groups since Waldo and colleagues included individuals above age 15 years and also because they had a smaller sample size.
There is generally paucity of data on the prevalence of first degree AV block among children with congenital heart diseases. This is because in the past, first degree AV block was considered a benign condition. However, recently first degree AV block has been reported to be associated with increased risk of atrial fibrillation, pacemaker implantation and all-cause mortality especially in adults [30]. Patients with a borderline first-degree AV block during normal sinus rhythm may also have dual AV node physiology and may be at higher risk for clinical atrioventricular nodal re-entry tachycardia (AVNRT) [31]. In Uganda many children with congenital heart diseases grow into adulthood without corrective surgery. Our study does not provide information on how first degree AV block affects these children as they grow with congenital heart diseases. However, these results mean that electrocardiography should be done regularly for these children and there is need for further research to assess the impact of first degree AV block on these children as they grow into adulthood.
In this study, use of digoxin and age were independently associated with first degree AV block. One of the possible explanations for the association between digoxin use and first degree AV block in this study could be that first degree AV block was a manifestation of digoxin toxicity in these children. In this study, we did not measure serum digoxin levels for children who had first degree AV block, which was a limitation. However, digoxin toxicity is known to cause first degree AV block [32].
In this study, children aged 5 years and below were less likely to have first degree AV block compared to children above 5 years. This could be because young children are less likely to have digoxin toxicity. The younger the child, the higher the serum levels of digoxin which can be tolerated before manifestations of digoxin toxicity occurs [32]. The other reason why older children have a higher prevalence of first degree AV block may also be because these children have lived longer with un-operated congenital heart disease and are more likely to present with arrhythmias as a complication of the congenital heart defects.
This study was carried out among children in Mulago Hospital; a setting where children with congenital heart diseases rarely have ECGs done during their care. These results therefore provide an understanding of the prevalence of arrhythmias among the children who are managed in the hospital. The study also shows some of the factors associated with these arrhythmias such as age of the child, digoxin use and electrolyte imbalances. These are factors that can easily be assessed among the children who receive care at Mulago Hospital and in other similar resource limited settings.
Study limitations
This study was carried out using a standard 12 lead ECG and not a holter ECG thus the prevalence of arrhythmias reported may be lower than the actual prevalence which would be detected using holter ECGs.
In this study we did not determine serum digoxin levels to assess for digoxin toxicity. This limited our ability to determine whether the prevalence of first degree AV block was a feature of digoxin toxicity.
This study was unable to assess other factors which could predispose these children to arrhythmias such as genetic factors, infections and in cases of neonates factors such as congenital infections, maternal diabetes and prematurity.
Conclusion
Arrhythmias are relatively common among children with congenital heart diseases presenting at Mulago hospital; occurring in approximately one in four children with congenital heart diseases. Factors associated with these arrhythmias include age of the child, digoxin use and electrolyte imbalances. This study therefore provides an understanding of the need to routinely assess children with congenital heart disease for arrhythmias and the various factors associated with these arrhythmias as the children receive routine care at the hospital. Future research can be done using a holter ECG to provide a more comprehensive analysis of the arrhythmias among children with congenital heart diseases in similar resource limited settings.
Ethical approval and consent
This study was approved by the Makerere University School of Medicine Research and Ethics Committee (SOMREC) and the Uganda National Council for Science and Technology. All caretakers of children provided informed consent for the children before recruitment into the study. In addition, children aged 8 years and above provided assent before participating in the study.
Availability of data and materials
All relevant data supporting the conclusions of this article is included within the article.
Abbreviations
- ASD:
-
atrial septal defect
- AV:
-
atrial ventricular
- AVNRT:
-
atrioventricular nodal re-entry
- CAVC:
-
common atrial- ventricular canal defect
- CHD:
-
congenital heart disease
- ECG:
-
electrocardiography
- HIV:
-
human immune-deficiency virus
- L-TGA:
-
L transposition of great arteries
- PACs:
-
premature atrial contractions
- PVCs:
-
premature ventricular contractions
- TOF:
-
Tetralogy of Fallot
- VSD:
-
ventricular septal defect
- VT:
-
ventricular tachycardia
References
Liberthson RR. Sudden death from cardiac causes in children and young adults. N Engl J Med. 1996;334(16):1039–44.
Szili-Torok T, Kornyei L, Jordaens LJ. Transcatheter ablation of arrhythmias associated with congenital heart disease. J Interv Card Electrophysiol. 2008;22(2):161–6.
Yacoub MH. Establishing pediatric cardiovascular services in the developing world. Circulation. 2007;116(17):1876–8.
Mocumbi AO, Lameira E, Yaksh A, Paul L, Ferreira MB, Sidi D. Challenges on the management of congenital heart disease in developing countries. Int J Cardiol. 2011;148(3):285–8.
Olivares JL, Vázquez M, Rodríguez G, Samper P, Fleta J. Electrocardiographic and echocardiographic findings in malnourished children. J Am Coll Nutr. 2005;24(1):38–43.
Dei Cas L, Metra M, Leier CV. Electrolyte disturbances in chronic heart failure: metabolic and clinical aspects. Clin Cardiol. 1995;18(7):370–6.
Lubega S, Zirembuzi G, Lwabi P. Heart disease among children with HIV/AIDS attending the paediatric infectious disease clinic at Mulago Hospital. Afr Health Sci. 2007;5(3):219–26.
Kish L. Survey Sampling. New York: John Wiley & Sons, Inc; 1965. p. 41.
Ringel RE, Kennedy HL, Brenner JI, Roberts GS, Berman MA. Detection of cardiac dysrhythmias by continuous electrocardiographic recording in children undergoing cardiac surgery. J Electrocardiol. 1984;17(1):1–6.
Naing L, Winn T, Rusli B. Practical issues in calculating the sample size for prevalence studies. Arch Orofac Sci. 2006;1(1):9–14.
Ross RD, Bollinger RO, Pinsky WW. Grading the severity of congestive heart failure in infants. Pediatr Cardiol. 1992;13(2):72–5.
Reithmann C, Reber D, Kozlik-Feldmann R, Netz H, Pilz G, Welz A, Werdan K. A post-receptor defect of adenylyl cyclase in severely failing myocardium from children with congenital heart disease. Eur J Pharmacol. 1997;330(1):79–86.
World Health Organization: Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System. Geneva 2011.
Pesce M. Reference ranges for laboratory tests and procedures. In Stanton B, Berhman K, Stanton J (Eds). Nelson textbook of Paediatrics. 18th Edition, Chapter 715. Elsevier 2007.
Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol. 2007;165(6):710–8.
Grosse-Wortmann L, Kreitz S, Grabitz RG, Vazquez-Jimenez JF, Messmer BJ, von Bernuth G, Seghaye M-C. Prevalence of and risk factors for perioperative arrhythmias in neonates and children after cardiopulmonary bypass: continuous holter monitoring before and for three days after surgery. J Cardiothorac Surg. 2010;5(1):85.
Michaëlsson M, Riesenfeld T, Jonzon A. Natural history of congenital complete atrioventricular block. Pacing Clin Electrophysiol. 1997;20(8):2098–101.
Walsh EP. Interventional electrophysiology in patients with congenital heart disease. Circulation. 2007;115(25):3224–34.
Khairy P, Balaji S. Cardiac arrhythmias in congenital heart diseases. Indian pacing and electrophysiology journal. 2009;9(6):299.
Stewart P, Tonge H, Wladimiroff J. Arrhythmia and structural abnormalities of the fetal heart. Br Heart J. 1983;50(6):550–4.
Jaeggi E, Hornberger L, Smallhorn J, Fouron JC. Prenatal diagnosis of complete atrioventricular block associated with structural heart disease: combined experience of two tertiary care centers and review of the literature. Ultrasound Obstet Gynecol. 2005;26(1):16–21.
Paul O, MYERS GS, CAMPBELL JA. The electrocardiogram in congenital heart disease a preliminary report. Circulation. 1951;3(4):564–78.
Khairy P, Marelli AJ. Clinical use of electrocardiography in adults with congenital heart disease. Circulation. 2007;116(23):2734–46.
Harker HE, Majcher TA. Hypermagnesemia in a pediatric patient. Anesth Analg. 2000;91(5):1160–2.
Slovis C, Jenkins R. Conditions not primarily affecting the heart. In: Morris F, Edhouse J, Brady WJ, Camm J, editors. Abc of Clinical Electrocardiography. London: BMJ Publishing Group; 2003. p. 53–6.
Gennari FJ. Hypokalemia. N Engl J Med. 1998;339(7):451–8.
RuDusky BM. ECG abnormalities associated with hypocalcemia. CHEST Journal. 2001;119(2):668–9.
Epstein FH, Schrier RW, Abraham WT. Hormones and hemodynamics in heart failure. N Engl J Med. 1999;341(8):577–85.
Waldo AL, Kaiser GA, Bowman FO, Malm JR. Etiology of prolongation of the PR interval in patients with an endocardial cushion defect further observations on internodal conduction and the polarity of the retrograde P wave. Circulation. 1973;48(1):19–26.
Cheng S, Keyes MJ, Larson MG, McCabe EL, Newton-Cheh C, Levy D, Benjamin EJ, Vasan RS, Wang TJ. Long-term outcomes in individuals with prolonged PR interval or first-degree atrioventricular block. Jama. 2009;301(24):2571–7.
Schlechte EA, Boramanand N, Funk M. Supraventricular tachycardia in the pediatric primary care setting: Age-related presentation, diagnosis, and management. J Pediatr Health Care. 2008;22(5):289–99.
Hastreiter AR, van der Horst RL, Chow-Tung E. Digitalis toxicity in infants and children. Pediatr Cardiol. 1984;5(2):131–48.
Acknowledgements
We would like to thank Child Health and Development Centre and department of Paediatrics and Child Health Makerere University College of Health Sciences, and staff of Mulago National Referral Hospital for their different roles in the study.
Funding source
Research reported in this publication was supported by the Fogarty International Center, the National Heart Lung and Blood Institute, and the Common Fund of the National Institutes of Health under Award Number 5R24 TW008861. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
AB, CK, PL, SL, SK and VN contributed to the design of the study and participated in data analysis. AB coordinated the study and supervised the enrollment of patients. All authors contributed to the interpretation of data and writing of the manuscript. All authors read and approved the final manuscript.
Authors’ information
Anthony Batte - MBChB, M.med (Paediatrics). Lecturer Child Health and Development Centre Makerere University.
Charles Karamagi - MBChB, Mmed (Paediatrics), PhD. Associate Professor of Clinical Epidemiology Makerere University.
Peter Lwabi - MBChB, Mmed (Paediatrics), Dip Cardiology. Paediatric cardiologist at Uganda Heart Institute.
Sulaiman Lubega - MBChB, Mmed (Paediatrics), Dip Cardiology. Paediatric cardiologist at Uganda Heart Institute.
Sarah Kiguli - MBChB, Mmed (Paediatrics), MHPE. Professor of Paediatrics and Child Health Makerere University.
Violette Nabatte - MBChB, M.med (Paediatrics). Paediatrics and Child Health Makerere University
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Batte, A., Lwabi, P., Lubega, S. et al. Prevalence of arrhythmias among children below 15 years of age with congenital heart diseases attending Mulago National Referral Hospital, Uganda. BMC Cardiovasc Disord 16, 67 (2016). https://doi.org/10.1186/s12872-016-0243-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-016-0243-1