Abstract
Background
To evaluate the postoperative morbidity and mortality of patients undergoing cardiovascular surgery during the 2022 nationwide Omicron variant infection wave in China.
Methods
This retrospective cohort study included 403 patients who underwent cardiovascular surgery for the first time during the 2022 wave of the pandemic within 1 month. Among them, 328 patients were preoperatively diagnosed with COVID-19 Omicron variant infection during the pandemic, and 75 patients were negative. The association between Omicron variant exposure and postoperative prognosis was explored by comparing patients with and without COVID-19 exposure. The primary outcome was in-hospital death after cardiovascular surgery. The secondary outcomes were major postoperative morbidity, including myocardial infarction (MI), acute kidney injury (AKI), postoperative mechanical ventilation hours, ICU stay hours, and postoperative length of stay. The data were analyzed using inverse probability of treatment weighting (IPTW) to minimize bias.
Results
We identified 403 patients who underwent cardiovascular surgery, 328 (81.39%) had Omicron variant infections. In total, 10 patients died in the hospital. Omicron variant infection was associated with a much greater risk of death during cardiovascular surgery after adjustment for IPTW (2.8% vs. 1.3%, adjusted OR 2.185, 95%CI = 1.193 to 10.251, P = 0.041). For major postoperative morbidity, there were no significant differences in terms of myocardial infarction between the two groups (adjusted OR = 0.861, 95%CI = 0.444 to 1.657, P = 0.653), acute kidney injury (adjusted OR = 1.157, 95%CI = 0.287 to 5.155, P = 0.820), postoperative mechanical ventilation hours (B -0.375, 95%CI=-8.438 to 7.808, P = 0.939), ICU stay hours (B 2.452, 95%CI=-13.269 to 8.419, P = 0.660) or postoperative stay (B -1.118, 95%CI=-2.237 to 1.154, P = 0.259) between the two groups.
Conclusion
Perioperative COVID-19 infection was associated with an increased risk of in-hospital death among patients who underwent cardiovascular surgery during the Omicron variant wave of the pandemic.
Similar content being viewed by others
Introduction
Since the outbreak of COVID-19, more than 160 countries have the disease a pandemic, which has had an enormous impact on the global medical system and economic losses [1, 2]. On December 6th ,2022, the Notice on Further Optimizing the Implementation of COVID-19 Prevention and Control Measures (referred to as the “Ten New Guidelines”) [3] announced the beginning of the Omicron wave and that all levels of medical institutions should ensure normal medical services and medical convenience for patients in China. Compared with the Delta variant or the original strain, Omicron variant exhibited considerable transmissibility but decreased disease severity [4]. . Additionally, the majority of the population had received the COVID-19 vaccine. Accordingly, the focus on perioperative management of surgical patients with a history of Omicron infection changed from early nosocomial infection control and disease prevention to postoperative prognosis improvement.
Guidelines for the management of surgical patients were issued during the pandemic [5, 6]. However, the available information was not up-to-date and did not involve the Chinese population regarding the less virulent Omicron variant that caused a nationwide wave in China. Owing to a lack of evidence, the perioperative management of surgical patients with Omicron infection in China is currently challenging for surgeons and anesthesiologists.
Cardiovascular surgery patients are a particularly vulnerable population because perioperative concomitant infection is a burden associated with adverse outcomes [7]. The impact of COVID-19 infection on postoperative morbidity and mortality during cardiovascular surgery needs to be identified to enable surgeons and patients to make evidence-based decisions during pandemics.
The aim of this study was to assess the outcomes of cardiovascular surgery among patients who were positive for COVID-19and negative for COVID-19 during the first month of the Omicron wave in China. The information in this study has important implications for patients considering cardiovascular surgery during the COVID-19 pandemic.
Materials and methods
Patients and study design
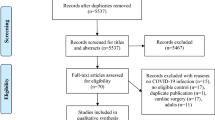
This was a retrospective analysis of data collected from the largest volume of cardiac surgery hospital data in China. In total, 567 consecutive patients were examined from December 6, 2022, to January 6, 2023, for the first time during the Omicron wave.
The patients underwent one of five surgical procedures: coronary artery bypass graft (CABG), valvular surgery, CABG and valvular combined surgery, aortic dissection surgery or congenital surgery. All surgeries were open cardiothoracic surgeries. All patients were 18 + years of age. The exclusion criteria were reoperation, emergency surgery or minimally invasive surgery. A total of 403 patients met the inclusion criteria. Patients were classified as COVID-19 positive if they had a record of a positive COVID-19 test 14 days before surgery. We compared the postoperative outcomes between COVID-19 positive patients and COVID-19 negative patients during the pandemic. All the extracted patients were from Chinese ethnic population. Dedicated staff were responsible for the collection, completeness and submission of the hospitalization materials. This study was approved by the Ethics Committee of Beijing Anzhen Hospital (No. 2023164X).
Study outcomes
The primary outcome of this study was in-hospital death after surgery which was determined based on hospital medical records.
The secondary outcomes included the incidence of major postoperative morbidity, including myocardial infarction (MI); and acute kidney injury (AKI); the duration of mechanical ventilation time, the length of intensive care unit (ICU) stay; and the length of postoperative stay.
Myocardial infarction was defined as an absolute increase in cardiac troponin levels (from baseline) ≥ 75 times the upper reference limit plus 1 of the following criteria: ①ischemic ST-T changes; ②New significant Q waves ③Imaging evidence showed loss of myocardium or abnormal local wall motion [8]. . Acute kidney injury was defined by the Kidney Disease: Improving Global Outcomes (KDIGO) criterria [9] as plasma creatinine levels ≥ 1.5 times greater than baseline plasma creatinine levels or a 26.5umol/L increase in plasma creatinine levels within 48 h after surgery compared with baseline levels.
Statistical analysis
Descriptive variables are presented as the means ± standard deviations; the t test was used to assess differences. Categorical variables are shown as frequencies (percentages), and comparisons were made with chi-square tests. Two-tailed P values ≤ 0.05 were considered to indicate statistical significance. All the statistical analyses were performed using SAS 4.2.0 (SAS Institute Inc., Cary, NC, USA).
To adjust for the impact of treatment selection bias and potential confounders in this study, propensity scores were calculated via multiple logistic-regression analysis, and inverse probability of treatment weighting was employed. We applied probability weights equal to the inverse propensity score for positive patients, and probability weights were calculated as the inverse of 1 minus the propensity score for negative patients. A separate propensity score for positive versus negative patients was derived for each comparison. The odds ratios (ORs) and estimated coefficients (B) for postoperative outcomes were calculated, and 95% confidence intervals were used to show the effect sizes of comparisons.
Results
A total of 403 patients were ultimately included in this original study. Among them, 328 were positive for COVID-19 during the preoperative period, and 75 patients were negative. The two groups had similar baseline characteristics with respect to age, sex, BMI, hypertension, diabetes mellitus, myocardial infarction, chronic heart failure, creatinine, ejection fraction and NYHA class. However, more people in the positive group had higher hyperlipidemia (35.1% vs. 17.3%, P = 0.005) and diabetes mellitus (29.3% vs. 17.3%, P = 0.036) (Table 1).
Primary outcomes
In total, the overall in-hospital mortality rate was 2.48% (10/403). In the negative group, only one patient who underwent CABG died from postoperative acute myocardial infarction. In the positive group, 9 patients died- 3 patients who underwent CABG ,2 patients who underwent CABG and valvular surgery, 2 patients who underwent valvular surgery only and 2 patients who underwent aortic dissection surgery. In-hospital deaths associated with Omicron infections were caused mainly by direct life-threatening respiratory failure and toxic shock.
Secondary outcomes
The major postoperative morbidities during the Omicron wave were compared between COVID-19 positive patients who underwent cardiovascular surgery and negative patients using inverse probability weighting. Tables 2 and 3 show the contingency tables for each major complication with p values.
There was no significant difference in terms of myocardial infarction (adjusted OR = 0.861, 95%CI = 0.444 to 1.657, P = 0.653); acute kidney injury (adjusted OR = 1.157, 95%CI = 0.287 to 5.155, P = 0.820); postoperative mechanical ventilation hours (B -0.375, 95%CI=-8.438 to 7.808, P = 0.939); ICU stay hours (B 2.452, 95%CI=-13.269 to 8.419, P = 0.660) or postoperative length of stay (B -1.118, 95%CI=-2.237 to 1.154, P = 0.259) between the two groups.
Even though there was no significant difference in postoperative morbidity between the two groups, the tendency was greater in the positive group.
Discussion
This is the first and largest study to estimate the effect of the Omicron wave on patients undergoing cardiovascular surgery in China. We sought to confirm that the outcomes of COVID-19 positive patients were comparable to those negative patients and to determine the best result for cardiovascular surgery during the pandemic. In this study, the incidence rates of postoperative morbidity and mortality were high among patients with a history of Omicron infection.
Preoperative COVID-19 was previously shown to be associated with significantly increased risks of morbidity and mortality, and consensus recommendations were made to delay elective surgery for 7 weeks after SARS-CoV-2 infection [10, 11]. However, such evidence represents the early wave of the COVID-19 pandemic, which was triggered by the ancestral variant, as opposed to the less virulent Omicron variant that caused the 2022 nationwide wave of infections in China [12]. Consequently, earlier evidence may not be applicable for guiding current practices during this pandemic wave in China [13].
China deployed successful multilayer nonpharmaceutical interventions (NPIs), and the majority of the population experienced an Omicron infection for the first time during the 2022 wave of the pandemic within 1 month [14]. The likely cause of this was the absence of previous epidemics, with the majority of infected patients experiencing the first course of the disease. This necessitated a prompt response in terms of perioperative management, particularly in the Chinese population. Therefore, we explored the feasibility of this mitigation strategy during the Omicron wave for perioperative patient management to facilitate decision-making while minimizing the disease burden.
At one month after the onset of the Omicron wave, a cohort of 403 individuals who underwent cardiovascular surgery procedures was collected, which represented a substantially decreased number of cardiac surgeries during the pandemic, with a 54% decrease in surgical volume compared with the previous year at our hospital. This means that most elective surgical interventions were deferred during the pandemic. Our research showed that the outcomes of cardiovascular surgery among patients who had COVID-19 during the perioperative period were significantly poor outcomes of increased mortality during hospitalization. The mortality rates for the positive and negative patients were 2.8% and 1.3%, respectively, which were statistically significant. For postoperative major morbidity, the positive group had a high rate, even though the difference was not statistically significant.
CABG surgeries and vascular surgeries were still the most common procedures performed during the pandemic [15]. In our research, the in-hospital mortality rate of CABG in the positive group was 1.57% (3/191), which was higher than that of 1.32% in the pre-COVID-19 era in our hospital [16]. Life-threatening disease during surgical repair of aortic dissection in patients with confirmed COVID-19 may result in fatal outcomes. In-hospital mortality was 8.16% (4/49) higher than that in the pre-COVID-19 era(6.1%) in our hospital [17]. Aortic dissection repair is an enormous challenge given the technical difficulty and complexity of this procedure as well as the cardiopulmonary damage caused by COVID‐19 during the pandemic.
The Omicron variant had lower pathogenicity, resulting in considerable lower rates of severe illness and death due to less severe disease and an improved clinical profile compared to those of the original strain. Additionally, the majority of the population was completely vaccinated. On the other hand, Omicron’s increased transmissibility is due to its rapid replication in the upper airways and increased attachment of the surface spike protein to angiotensin-converting enzyme 2 (ACE-2) receptors [18, 19]. There is abundant evidence suggesting that ACE-2 receptor-mediated endothelial dysfunction can cause severe myocardial injury [20,21,22]. Therefore, despite the decreased disease severity experienced with the Omicron variant, it continues to pose a major threat to cardiometabolic demand with resultant pressure on the health care system, as illustrated by the patients’ high incidence of in-hospital death. An updated guideline from the United Kingdom recommended that patients avoid elective surgery within 2 weeks after SARS-CoV-2 infection [23].
This study explored the influence of the Omicron variant on the postoperative prognosis of patients who underwent cardiovascular surgery. The risk of in-hospital death was higher among COVID-19-positive patients.
Conclusion
Aa many regions worldwide continue to experience the spread of COVID-19, it is necessary to estimate the risk associated with cardiac surgery during a pandemic. Preoperative COVID-19 positivity during thepandemic was associated with an increased risk of in-hospital death among patients undergoing cardiac surgery. However, for patients with severe multivessel coronary or aortic dissection requiring emergency procedures, even though there is an increased likelihood of mortality compared with the pre-COVID-19 era, delay would more likely result in patient harm.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Deng SQ, Peng HJ. Characteristics of and Public Health Responses to the Coronavirus Disease 2019 Outbreak in China. J Clin Med 2020;9(2).
Han Q, Lin Q, Jin S, You L. Coronavirus 2019-nCoV: a brief perspective from the front line. J Infect. 2020;80(4):373–7.
Cheng ZJ, Zhan Z, Xue M, Zheng P, Lyu J, Ma J, Zhang XD, Luo W, Huang H, Zhang Y, et al. Public Health Measures and the control of COVID-19 in China. Clin Rev Allergy Immunol. 2023;64(1):1–16.
Chinese Center For Disease C, Prevention. Guidelines for Investigation and Management of Close contacts of COVID-19 cases. China CDC Wkly. 2020;2(19):329–31.
Hassan A, Arora RC, Adams C, Bouchard D, Cook R, Gunning D, Lamarche Y, Malas T, Moon M, Ouzounian M, et al. Cardiac surgery in Canada during the COVID-19 pandemic: a Guidance Statement from the Canadian society of Cardiac surgeons. Can J Cardiol. 2020;36(6):952–5.
Global guidance for surgical care during the COVID-19 pandemic. Br J Surg 2020, 107(9):1097–103.
Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, Bi Z, Zhao Y. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531–8.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD. Fourth Universal Definition of Myocardial Infarction (2018). J Am Coll Cardiol. 2018;72(18):2231–64.
Ostermann M, Bellomo R, Burdmann EA, Doi K, Endre ZH, Goldstein SL, Kane-Gill SL, Liu KD, Prowle JR, Shaw AD et al. Controversies in acute kidney injury: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Conference. Kidney Int 2020;98(2):294–309.
Rohatgi N, Smilowitz NR, Reejhsinghani R. Perioperative Cardiovascular considerations prior to elective noncardiac surgery in patients with a history of COVID-19. JAMA Surg. 2022;157(3):187–8.
El-Boghdadly K, Cook TM, Goodacre T, Kua J, Blake L, Denmark S, McNally S, Mercer N, Moonesinghe SR, Summerton DJ. SARS-CoV-2 infection, COVID-19 and timing of elective surgery: a multidisciplinary consensus statement on behalf of the Association of Anaesthetists, the Centre for Peri-operative Care, the Federation of Surgical Specialty Associations, the Royal College of Anaesthetists and the Royal College of Surgeons of England. Anaesthesia. 2021;76(7):940–6.
Wang L, Zheng Z, Zhu S, Luo G, Gao B, Ma Y, Xu S, Dong H, Lei C. Changes in early postoperative outcomes and complications observed in a single center during the 2022 COVID-19 pandemic wave in China: a single-center ambispective cohort study. Chin Med J (Engl). 2023;136(14):1708–18.
Glasbey JC, Dobbs TD, Abbott TEF. Can patients with asymptomatic SARS-CoV-2 infection safely undergo elective surgery? Br J Anaesth. 2022;128(6):909–11.
Cai J, Deng X, Yang J, Sun K, Liu H, Chen Z, Peng C, Chen X, Wu Q, Zou J, et al. Modeling transmission of SARS-CoV-2 Omicron in China. Nat Med. 2022;28(7):1468–75.
Ayati A, Hosseini K, Hadizadeh A, Jalali A, Lotfi-Tokaldany M, Milan N, Bagheri J, Ahmadi Tafti SH. Surgical coronary revascularization in patients with COVID-19; complications and outcomes: a retrospective cohort study. Health Sci Rep. 2022;5(5):e751.
Li Y, Hou XJ, Liu TS, Xu SJ, Huang ZH, Yan PY, Xu XY, Dong R. Risk factors for acute kidney injury following coronary artery bypass graft surgery in a Chinese population and development of a prediction model. J Geriatr Cardiol. 2021;18(9):711–9.
Zhang CH, Ma WG, Zhong YL, Ge YP, Li CN, Qiao ZY, Liu YM, Zhu JM, Sun LZ. Management of acute type a aortic dissection during COVID-19 outbreak: experience from Anzhen. J Card Surg. 2021;36(5):1659–64.
Hui KPY, Ho JCW, Cheung MC, Ng KC, Ching RHH, Lai KL, Kam TT, Gu H, Sit KY, Hsin MKY, et al. SARS-CoV-2 Omicron variant replication in human bronchus and lung ex vivo. Nature. 2022;603(7902):715–20.
Meng B, Abdullahi A, Ferreira I, Goonawardane N, Saito A, Kimura I, Yamasoba D, Gerber PP, Fatihi S, Rathore S, et al. Altered TMPRSS2 usage by SARS-CoV-2 omicron impacts infectivity and fusogenicity. Nature. 2022;603(7902):706–14.
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, et al. Clinical characteristics of 138 hospitalized patients with 2019 Novel Coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–9.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506.
Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271–280e278.
El-Boghdadly K, Cook TM, Goodacre T, Kua J, Denmark S, Mercer N, Moonesinghe SR, Summerton DJ. Timing of elective surgery and risk assessment after SARS-CoV-2 infection: 2023 update: a multidisciplinary consensus statement on behalf of the Association of Anaesthetists, Federation of Surgical Specialty Associations, Royal College of Anaesthetists and Royal College of Surgeons of England. Anaesthesia. 2023;78(9):1147–52.
Acknowledgements
Not applicable.
Funding
This work was supported by a grant from the National Natural Science Foundation of China (No. 8216030718).
Author information
Authors and Affiliations
Contributions
FX wrote the manuscriptYB and FX performed the statistical analysisDL and ZW prepared the tables and figuresSW designed the studyAll authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Beijing Anzhen Hospital (No. 2023164X), and informed consent was obtained from all the subjects and/or their legal guardian(s).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, F., Bai, Y., Xie, F. et al. Postoperative morbidity and mortality of patients with COVID-19 undergoing cardiovascular surgery: an inverse propensity-weighted study. BMC Anesthesiol 24, 98 (2024). https://doi.org/10.1186/s12871-024-02445-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-024-02445-5