Abstract
Background
ICU survivors often suffer from prolonged physical and mental impairments resulting in the so called “Post-Intensive Care Syndrome” (PICS). The aftercare of former ICU patients affected by PICS in particular has not been addressed sufficiently in Germany so far. The aim of this study was to evaluate the feasibility of a pragmatic randomised trial (RCT) comparing an intensive care unit (ICU) follow-up clinic intervention to usual care.
Methods
This pilot study in a German university hospital evaluated the feasibility of a pragmatic RCT. Patients were assigned in a 1:1 ratio to an ICU follow-up clinic intervention or to usual care. The concept of this follow-up clinic was previously developed in a participatory process with patients, next of kin, health care professionals and researchers. We performed a process evaluation and determined acceptability, fidelity, completeness of measurement instruments and practicality as feasibility outcomes. The RCT’s primary outcome (health-related quality of life) was assessed six months after ICU discharge by means of the physical component scale of the Short-Form-12 self-report questionnaire.
Results
The pilot study was conducted from June 2020 to May 2021 with 21 and 20 participants in the intervention and control group. Principal findings related to feasibility were 85% consent rate (N = 48), 62% fidelity rate, 34% attrition rate (N = 41) and 77% completeness of outcome measurements. The primary effectiveness outcome (health-related quality of life) could be measured in 93% of participants who completed the study (N = 27). The majority of participants (85%) needed assistance with follow-up questionnaires (practicality). Median length of ICU stay was 13 days and 85% (N = 41) received mechanical ventilation, median Sequential Organ Failure Assessment Score was nine. Six-month follow-up assessment was planned for all study participants and performed for 66% (N = 41) of the participants after 197 days (median).
Conclusion
The participatory developed intervention of an ICU follow-up clinic and the pragmatic pilot RCT both seem to be feasible. We recommend to start a pragmatic RCT on the effectiveness of the ICU follow-up clinic.
Trial registration
ClinicalTrials.gov US NLM, NCT04186468, Submission: 02/12/2019, Registration: 04/12/2019, https://clinicaltrials.gov/ct2/show/NCT04186468
Similar content being viewed by others
Background
Survivors of ICU (intensive care unit) treatment often suffer from a wide range of physical, cognitive and mental health difficulties, referred to as post-intensive care syndrome (PICS) [1,2,3]. Available studies and data differ with respect to the prevalence and characteristics of PICS in ICU survivors [4,5,6,7]. For example, 25–80% of ICU survivors experience intensive care unit-acquired weakness (ICUAW) [8, 9], 30–80% cognitive impairments [4, 10, 11] and about 50% depression, anxiety or posttraumatic stress disorder (PTSD) [4, 6, 7]. Physical, cognitive and mental impairments have negative effects on patients’ health-related quality of life (HRQOL) [7, 12, 13]. A lower HRQOL compared to the general population is still present one year after discharge from ICU [12, 14, 15]. In addition, several studies show evidence for complications including depressive, anxiety and posttraumatic stress disorder also in family members, which is conceptualized as post-intensive care syndrome family (PICS-F) [9].
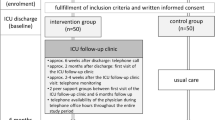
To address adverse sequelae of former critically ill patients as well as of their next of kin, several aftercare programs such as ICU follow-up clinics were developed. A recent systematic review on effects of ICU follow-up clinics concluded that symptoms of depression and mental HRQOL may be improved by this kind of intervention [16] but the quality of evidence regarding the effectiveness of those clinics is low [17,18,19]. Existing concepts of ICU follow-up clinics differ in the management (e.g. led by nurses, physicians or a multidisciplinary team), the focus of the intervention (e.g. physical and/or mental), the administration of consultation and counselling (direct contact or by phone), the frequency/dose of follow-up (e.g. weekly or monthly) or the eligible patient group (e.g. duration of ICU stay or specific diagnosis). This makes comparisons regarding effectiveness of interventions challenging [17,18,19,20,21,22]. While some European countries already have integrated ICU follow-up clinics in several hospitals [18, 20], no follow-up services are available for critically ill patients after discharge from ICU in Germany until now and the internationally implemented concepts have not been developed with intense involvement of all relevant stakeholder groups. Rehabilitation in Germany is rather specialized to disciplines and specific organ failures, than to general ICU population [23]. In general, ICU patients with severe underlying diseases are transferred to specialized rehabilitation facilities for early rehabilitation according to the level of support they require. In contrast to early rehabilitation, follow-up rehabilitation is part of medical rehabilitation that takes place when there is no (longer) need for acute medical treatment. The patients are already early mobilised and capable of self-help. The follow-up rehabilitation can be either conducted ambulatory, in a specialized rehabilitation centre or home-based [24]. However, after rehabilitation the support for further treatment is left to the treating physician without special experience for those patients with severe underlying diseases. Therefore, specialized follow-up services for those patients are necessary to provide the best-possible care [25]. Against this background, a multidisciplinary stakeholder group composed of health care professionals, researchers, patients and next of kin conceptualized an ICU follow-up clinic intervention in a German university hospital. The intervention was developed in a participatory process as previously reported [26,27,28] and consists of three main components: information, consultation and networking (Fig. 1). In brief, the development included face-to-face interviews with former ICU patients, next of kin of former ICU patients, six focus group discussions and six expert interviews to capture all relevant stakeholders’ perspectives (in total, nine different professions). Results of interviews, discussions, evidence from the literature and evidence from claims data analysis were assessed and synthesised to create a first draft of the intervention. This draft was discussed and refined in two workshops with stakeholders and finalised by the interdisciplinary project team.
Main components of the ICU follow-up clinic adapted from our study protocol [28]
Methods/Study design
Trial design
The methodology of the study has been outlined previously [28]. Briefly, our study was a pragmatic, single-centre, superiority, two-armed pilot randomised controlled trial with 1:1 allocation ratio, conducted between December 2019 and June 2021. To explore feasibility and acceptability of the trial and the intervention, it was accompanied it by a mixed-methods process evaluation according to the Medical Research Council (MRC) framework [29, 30] performed by a scientific study team not involved in the clinical study. Quantitative as well as qualitative data were collected and analysed alongside the pilot RCT. The institutional Ethics Committee of the University of Regensburg approved the study on 26/09/2019 (19–1522-101). Every participant actively agreed to be part of the study and informed consent was obtained according to the Helsinki Declaration [31]. We registered the study at a trials registry (clinicaltials.gov, NCT04186468) on 04/12/2019 before inclusion of the first participant.
Participants and randomisation
The clinical study team (two physicians and two nurses) screened eligible patients on a daily basis at three ICUs (two medical and one surgical ICU) of Regensburg University Hospital. Inclusion criteria were: Length of ICU stay > 120 h (5 days), Sequential Organ Failure Assessment (SOFA) score [32] during ICU stay > 5, age ≥ 18 years and estimated life expectancy > 6 months. At the end of the ICU stay patients were approached if they were responsive (i.e. no sedation, fully conscious, no medical interventions). Patients were excluded if they were less than 18 years old, gave no written informed consent (unable or unwilling), were not expected to survive more than 6 months after hospital discharge, had an ICU stay equal or shorter than 120 h, had a SOFA score of 5 or less, were unable to complete questionnaires or had insufficient German language skills. The study physician explained the trial and handed out the study information brochure. Informed consent was obtained during the ICU stay from participants or their legal representatives. Participants were randomised to intervention or control group. They did not receive any incentives. The scientific study team prepared computer-generated permuted block randomisation with blocks of size 10 to ensure balance between groups over short time spans [33]. The responsible study physician received an opaque, sequentially numbered envelope supplied by the study team. The study physician opened the envelope after the participant's consent to take part in the study and explained the result of the randomisation. Blinding of the study personnel or the participants after randomisation was not possible due to the nature of our study. Nevertheless, the trust centre masked group allocation for the outcomes assessor during analysis of the primary outcome.
Intervention
The intervention was a complex intervention including three components mentioned above. An intervention manual was compiled that specifies all procedures and contained the necessary instructions for action.
Shortly before ICU discharge, a first consultation took place. Participants were informed about the next steps: transfer to a regular ward, appointment to visit the follow-up clinic, telephone availability and monitoring by the study team, distribution of information material, e.g. ICU Steps brochure [34].
The ICU follow-up clinic visit was scheduled three months after ICU discharge. Three weeks before the visit the study nurse called the participants and reminded them of the upcoming appointment. The participants’ relatives were also invited to the appointment.
First, a brief assessment of the health condition and a screening of mobility was performed by the study nurse before the physician's consultation, including a blood pressure, oxygen saturation and heart rate measurement, and short current medical history. A standardised checklist based on questionnaires (Mini-Cog [35], PHQ-8 [36], GAD-7 [37], PTSS-10 [38], structured questions on symptoms of dysphagia and neuropathy [39]), were completed. Participants were motivated to self-complete the screening instruments and only received support by the study nurses, if they needed it (which was often the case). After completion, the study nurses evaluated the screening questionnaires. In case of strong deviations, irregularities in the preparation and peculiarities concerning the patient, they made memos in preparation for the consultation with the physician. The results of the questionnaires together with the memos then formed the indications for further questions from the physician. Thus, possible actions (e.g. further diagnostics, revision of medication, referrals) could be initiated immediately. During the consultation, participants and – if present – their next of kin were able to talk about the experiences at ICU and to ask questions. In the further medical examination, all areas (cognition, psyche, body, social, well-being) were examined. All participants were offered a visit to the ICU facilities and participation in a self-help group. The study physician wrote a physician's letter summarising the most important information about patient's health condition. In addition, the letter contained recommendations on further therapy measures, a description of the referrals issued and notes for the general practitioner. Information on e.g. social security issues, sleep hygiene or stockings were given to almost all participants. This letter was discussed intensively with the participant and if present next of kin and there was again room for questions. Referrals to therapists or specialists were organised.
At the latest four weeks after the ICU follow-up clinic visit, the study physician called the participants. During the telephone call, the state of health and, if applicable, the progress of the referrals were queried. If new impairments were detected, a referral to a GP visit was made or an additional ICU follow-up clinic visit was offered (case-by-case decision). The telephone monitoring also served as a monitoring tool for the implementation of the recommendations made. Furthermore, participants and relatives had the opportunity to call the ICU follow-up clinic during office hours to speak with the staff.
Control treatment
Participants enrolled in the control group received usual care without any additional information or consultation or monitoring until the follow-up assessment six months after discharge. Usual care in this context means that patients receive rehabilitation during and after a longer stay in hospital. The aim of rehabilitation in Germany is to strengthen physical, mental, social and vocational skills as well as self-determination and equal participation in all areas of life [40]. Rehabilitation in Germany is subdivided in different phases [41]. Early rehabilitation takes place in phases B and C in particular (phase A comprises the acute treatment). In phase B, patients usually still require intensive medical treatment, e.g. need to be ventilated. In phase C, they can already cooperate in therapy, but must continue to receive medical care and nursing [41]. Early rehabilitation is part of (usual) hospital treatment and is covered by health insurance if medically necessary [42]. It is started during acute inpatient treatment and can be continued in specialized facilities. The goals are, in particular, early mobilization, avoidance of later complications, and clarification and planning of further rehabilitation and care measures. A multidisciplinary team of physiotherapists, occupational therapists, speech therapists, neuropsychologists, social workers, specialized nursing and physicians work in these early rehabilitation facilities [43]. Depending on the severity of the permanent restrictions, those affected can then be reintegrated into working life, e.g., through follow-up rehabilitation and occupational rehabilitation measures, or receive benefits from long-term care insurance (e.g., long-term care allowance, day and night care) if the need for long-term care persists [24]. However, these efforts are not targeted to patients after ICU stay.
Feasibility outcomes
A quantitative process evaluation was conducted using a logic model [28] to frame our evaluation questions [30]. The overarching questions were:
-
Is a pragmatic RCT on the effects of the participatory developed ICU follow-up clinic feasible in terms of recruitment, randomisation, intervention delivery and follow-up?
-
Is it feasible to care for patients in terms of improving physical functioning and mental health in a participatory developed ICU follow-up clinic?
To answer those questions, the following key domains of feasibility were assessed:
-
Acceptability
-
◦ Number of study participants divided by number of possibly eligible patients (consent rate)
-
◦ Proportion of study participants who accepted their random group allocation (acceptance of randomisation)
-
-
Fidelity
-
◦ Number of study participants to whom all components of the intervention were delivered divided by all included study participants
-
-
Completeness
-
◦ Number of study participants lost to follow-up divided by all included participants (attrition rate)
-
◦ Mean completeness of baseline measurements (on instrument level)
-
◦ Mean completeness of follow-up measurements (on instrument level)
-
-
Practicality
-
◦ Proportion of participants needing assistance with questionnaires.
-
We predefined those domains and respective outcomes according to literature [44, 45]. We decided against certain thresholds because there will not be a single threshold above which the RCT is not feasible anymore.
Effectiveness outcomes (targeted results of the intervention)
Primary outcome
Primary effectiveness outcome was physical HRQOL at six months after informed consent/ICU discharge assessed by the physical component scale (PCS) of the Short Form-12 self-report questionnaire (SF-12) [46] with a four-week recall period. Items were scored according to published algorithms (German norm values; resulting in a standard score with mean = 50 and standard deviation = 10) [47]. Scores range between 0–100, with higher values indicating higher HRQOL.
Secondary outcomes
The secondary outcomes encompassed physical functioning, mental and social impairments as well as the extent of ambulatory and stationary health care use after ICU discharge. In addition, HRQOL of next of kin was assessed using the SF-12 questionnaire (PCS and MCS). Primary and secondary outcomes are shown in Table 1.
Data collection and analysis
To keep the participant's strain to a minimum, we collected as much information as possible from the clinical information systems (CIS) and next of kin (e.g. contact information, disease- and therapy-related characteristics). At inclusion in the study, we recorded their baseline measurements (e.g. sociodemographic characteristics not available from CIS) and quality of life assessed in form of the EQ-5D Visual Analogue Scale (VAS) [58]. The study team considered EQ-5 D VAS as the most feasible measurement instrument to assess health-related quality of life due to its brevity to keep the burden on the participants as low as possible at this very moment. At the follow-up assessment six months after discharge from ICU, we collected outcomes mentioned in Table 1. Trained study personnel handed out self-report questionnaires, provided standardized instructions and performed physical measurements. Missing data were minimized by having study personnel available at all times to check the completeness of the questionnaires or to answer participants´ questions. If participants were not able to visit the study centre, home visits were offered. If a home visit was not feasible, paper-based assessment with telephone support was considered. If a participant discontinued the trial before outcome assessment, only baseline data (e.g. sociodemographics, characteristics of the ICU stay and more details in Table 3) and the reasons for discontinuation were included in the analysis. All data were entered by the study team on site twice into a centralised database and checked for plausibility.
We compiled a statistical analysis plan (SAP) a priori that was already geared towards a large-scale study. Descriptive statistics were used to determine participant characteristics and to check their distribution at baseline in the intervention and control group. We calculated point and interval estimates where appropriate. Continuous data are presented as mean and standard deviation or median and interquartile range, depending on whether the values were normally distributed; normal distribution was tested with Shapiro–Wilk test. Categorical data are reported as counts and percentages. The primary outcome physical HRQOL was compared six months post randomisation between intervention and control group. As our overarching goal was to evaluate the feasibility of delivering an RCT comparing usual care with an ICU follow-up clinic, the study was not designed to measure differences between treatment groups (e.g. no power calculation). Therefore, no formal hypothesis testing was performed. Nevertheless, we undertook descriptive analyses on the outcome measures of interest. Data management was done with Microsoft© Access© 2016. Analyses were performed with IBM® SPSS© Statistics version 26.0 and 28.0.
Deviations from the initial study protocol
We initially started our study in December 2019. Due to the COVID-19 pandemic and related restrictions imposed by the German authorities also on clinical research, we had to discontinue all our activities (e.g. recruitment, inclusion of participants, the follow-up clinic) on March 20, 2020. Consequently, we needed to restart the RCT, since the duration of the interruption was not foreseeable at this time. Intensive discussions among the study team and with the funding agency led to a reduction of planned participants to 40. We chose this number primarily for economic reasons, as limited duration of the project and limited budget did not allow a further extension to achieve a number of 100 participants. We were able to resume activities on June 15, 2020.
Results
Patient flow and feasibility outcomes
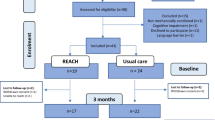
Participants were recruited from three ICUs (two medical and one surgical) at Regensburg University Hospital, Germany from June until September 2020. Based on a daily screening (60–90 min workload per day) two study nurses identified 169 eligible patients. 121 were excluded according to our exclusion criteria. A number of 48 potential participants were approached and informed about the study, of which 41 (85.4%) consented to take part in the study. Six suitable patients or their next of kin declined study participation with the following reasons: feeling too sick to participate, no interest in the study, not able to understand the language (n = 2, respectively). One patient withdrew his consent to participate after randomisation and was excluded for further proceedings and data analysis. The informed consent interviews lasted 20 min on average. All participants were randomised. All participants accepted the randomisation. Details on enrolment, allocation and follow-up can be found in Fig. 2.
For our predefined feasibility domains acceptability, fidelity, completeness and practicality, quantitative feasibility outcomes were measured alongside the RCT. All feasibility domains and the results for quantitative feasibility outcomes are shown in Table 2.
We were able to collect baseline values for all participants. Considering HRQOL measured by the EQ-5D VAS at baseline, 26.8% participants (N = 41) needed assistance in writing their value on the case report form. Approximately eight weeks after ICU discharge, 71% participants in the intervention group (N = 21) were reached out by phone to confirm the appointment for the ICU follow-up clinic visit. Two participants died in the meantime, three cancelled the further study participation actively. Two participants could not be reached, one was still treated at a hospital. The ICU follow-up clinic visit took place 11–12 weeks after discharge from hospital (mean/median 83/75 days after randomisation). There were some postponements due to a longer stay in rehabilitation. One participant’s hospital stay took so long that the ICU follow-up clinic visit had to be combined with the six-month follow-up assessment. The ICU follow-up clinic visit took 45–90 min (mean/median: 60 min), of which 15–60 min (median 30 min) were attended by the physician. Most participants were assisted from study personnel for completing the questionnaires. After the short evaluation by the study nurse, the results were discussed and recommendations for action assessed: Referrals to specialists (e.g. neurology, diabetology, gastroscopy) were issued eight times, referrals to therapy (e.g. physical therapy, counselling, podiatry) 21 times. For all participants, drug therapy was reviewed. The self-help groups were offered twice and due to no participants, the third meeting was cancelled in advance. Reasons for non-utilisation were a too great distance from home, no need due to improved health status or the effects of the COVID-19 pandemic (travel restrictions, fear of infection in the hospital). None of the participants took advantage of the offer to visit the ICU facilities.
Approximately three weeks after the ICU follow-up clinic visit, the study physicians conducted a telephone monitoring to discuss the current state of health and further therapy. Due to the COVID-19 pandemic, additional network meetings and events could no longer take place after the initial networking event in September 2019. The newsletter for health care providers envisaged in the original concept was not implemented. Moreover, the conceived referral list (i.e. information on therapists or physicians specialized in after ICU treatment) was not feasible because the catchment area of the study participants was too large (participants’ distance from home to follow-up clinic 6–310 km, mean 79 km).
Out of 41 participants with data from baseline assessment, we were able to re-assess 27 participants (66%) at the six-month follow-up. Attrition rate was 8/21 (38%) in the intervention group and 6/21 (29%) in the control group. In total, three participants died in between the six months after ICU discharge, ten participants did not respond or had no interest in the study anymore. No participant in the intervention group died in between the intervention and six-month follow-up. More details can be seen in Fig. 2. Thirteen participants were followed-up in the ICU follow-up clinic. Most of them needed assistance for completing the follow-up questionnaires. Six participants were visited at home. If even home visits were not feasible due to health status of the participant or the distance to the hospital, paper-based assessments with telephone support were conducted and thus the physical tests (grip strength and chair rising) could not be performed. Detailed completeness of the outcome measurement instruments are shown in Table 2 of the supplement S1. In particular, physical assessments and data collection from next of kin resulted in decreased completeness. The pilot RCT was duly concluded on 31/05/2021.
Participant characteristics
The study sample consisted of 15 women (37%) and 26 men (63%). Male participants were overrepresented in both the intervention (n = 12) and the control group (n = 14) at baseline. Two out of 13 participants without long-term nursing care gradeFootnote 1 upon baseline assessment had a long-term care grade at follow-up, four participants had a long-term care grade both at baseline and at follow-up. The majority of participants (64%) graduated from middle school. Only 17% percent had a higher education such as college or university degrees. Twenty-two participants (54%) were not employed prior to the ICU stay, fifteen (37%) were full-time employed. An imbalance existed between the intervention and control group in terms of employment (33% vs. 60%). Median duration of ICU stay was almost similar in the intervention and control group as well as the SOFA Score, Barthel-index, number of participants with mechanical ventilation and mean HRQOL score. Duration of mechanical ventilation was longer in the control group than in the intervention group (median 271 h compared to 184 h). Further, extracorporeal life support measures (ECMO, dialysis) were applied more often in the control group. Considering the baseline characteristics, there was an imbalance between the intervention and control group. Further imbalances in baseline characteristics were seen for gender and primary diagnosis. More details of baseline characteristics stratified for intervention and control group (usual care) are shown in Table 3.
Effectiveness outcomes (targeted results of the intervention)
Primary outcome
Our primary outcome (physical health-related quality of life) was lower in the intervention (mean 34.3 ± 10.8, min. 20.6, max. 53.6) than in the control group (mean 39.3 ± 11.0, min. 26.3, max. 56.0).
Secondary outcomes
Participants in the intervention group had more favourable outcomes in HRQOL (SF-12, mental health, MCS), activities of daily living (Barthel index) or indication for depressive disorders than the control group. The mean values for hand grip strength as an indicator of overall muscular strength were 28 kg and did not differ between intervention and control group. There was almost no difference for mental symptom-related difficulties in daily and working life (short form PHQ-D). Physical functioning (chair rising test) was better in the control group than in the intervention group (16 vs. 24 s for getting up five times from a chair without support). HRQOL of the relatives of the former ICU patients was better in the intervention group than in the control group (54 vs. 49). More details on secondary outcomes are presented in Table 4.
Discussion
To the best of our knowledge, this is the first study investigating the feasibility and potential effects of a complex intervention in form of an ICU follow-up clinic for ICU survivors in Germany.
Feasibility
Principal findings of this study were a consent rate of 85%, a fidelity rate of 62% and an attrition rate of 34%. Within 12 weeks, we recruited and successfully randomised 42 participants for the pilot study, i.e. 21 per arm. The participants accepted randomisation. One participant revoked his consent to participate in the study after assignment to the control group; the designated procedures to remove participant’s data worked. Some components of the intervention (e.g. self-help groups) could not be carried out largely due to COVID-19, which resulted in the 62% fidelity rate. Loss to follow-up mainly resulted from the fact that the participants were not (any longer) reachable. We know of three deceased participants during our study period. Data from other studies on ICU aftercare indicate that e.g. one-year-mortality is between 16–77% [64]. Further, the expected mortality among critically ill patients should be considered in the sample size calculation for a large-scale trial. Regarding the inclusion criteria and target group for an ICU follow-up clinic, patient groups for which dedicated follow-up programmes already exist (e.g. after organ transplantation, after a stroke or with cancer treatment) might not be included in a large-scale trial assessing the effects of the ICU follow-up clinic. Baseline data collection was successful and complete. The imbalance of baseline characteristics of the study sample might be due to the small sample size. Completeness of assessment of the primary outcome among all participants with completed follow-up was very good (93%); however, data which were assessed through physical examinations or data collected from next of kin was not complete in about 45% and 48% of cases due to logistic reasons. It is interesting to note that the relatives of the study participants often did not answer the questions on health-related quality of life (SF-12 MCS, ca. 50% completeness). The respondents might have felt under pressure at this moment or did not want to give "wrong" statements (social desirability). This could be addressed by better informing the patients’ relatives about the study already in advance, by explaining why their health is also important.
We were able to deliver the intervention to 14/21 study participants in the ICU follow-up clinic (see Fig. 2). The ICU follow-up visit took 60–90 min. In the context of a large-scale study (or as part of routine care), adjustments would have to be made in time management. One suggestion would be that patients could fill in the questionnaires before the ICU clinic follow-up visit in order to make this time window (20— 30 min) more effective. Regarding the six-month follow-up assessment, one should consider that particularly participants from the control group might have no incentive to travel to the study centre, especially if they live at a distance. Home visits took up a lot of resources that may not be available in everyday care and should be reconsidered for the effectiveness study. Of course, this could reduce the number of participants assessed in-person in a large-scale trial.
At baseline, 27% study participants needed support to point their value on the EQ-5D-VAS at that time. Further, 85% of the participants needed help in filling out the follow-up questionnaires, which would mean high effort for a larger study. Those consisted of five measurement instruments (SF-12, PHQ, PTSS-10, Barthel index, health care use), which may explain the high amount of assistance needed. We did not carry out a detailed analysis of the feasibility or acceptance of the single measurement instruments used. However, in the interest of data economy, minimising the amount of missing values and reducing the burden on patients, we suggest that the selection and composition of the measurement instruments in the large-scale study should be chosen even more carefully. Choice of outcome measurement instruments for a future trial should consider recent developments, in particular regarding core outcome sets [65,66,67], and should also take into account that the MCS and PCS of the SF-12 may not be independent components and therefore need to be interpreted with caution [68].
Signals for effectiveness of the intervention
With regard to the effectiveness of our intervention, the pilot trial with 41 participants showed lower physical HRQOL (primary outcome) in the intervention group compared to the control group (mean 34.3 vs. 39.3). However, the mental HRQOL of the participants in the intervention group (mean 49.0) was higher than that of the control group (mean 44.4). It can be hypothesised that the intervention had a greater impact on the participants’ mental health than on their physical health. This is in line with previous findings from the PRacTICaL study [22]. However, as mentioned above those component scale values need to be interpreted with caution. A recent systematic review synthesised subject-related outcomes of post-ICU follow-up clinics: Rosa et al. [16] indicated also that ICU follow-up clinics are associated with improved mental HRQOL outcomes. In our study, we also explored patients’ perceived benefits of the intervention using qualitative interviews. The results will be published elsewhere.
Deviations from the initial study protocol and its implications
The initially planned sample size of 100 participants had to be reduced due to the impacts of the COVID-19 pandemic. However, the final sample size followed recommendations for pilot trials if the effect size is unknown but expected to be small [69]. The reduced sample size although might have led to the imbalance between intervention and control group, so outliers might influence outcome evaluation. Therefore, we could not assess whether the ICU stay or an underlying disease (as the reason for the treatment) of the respective participant caused the recorded impairments.
Second, participants did not attend the planned self-help groups, so we were not able to actively assess acceptability or feasibility of this intervention component. Perhaps not attending the groups reflects a form of non-acceptance of this component.
Third, a network of health care professionals could not be implemented due to the impact of the pandemic; cross-sector collaboration for follow-up care could not be assessed.
Fourth, our SAP was already geared towards a large-scale study. Therefore, parts of it could not be implemented e.g., regarding the data analysis no intention-to-treat approach could be followed to analyse the effect of the ICU follow-up clinic on HRQOL as primary outcome and the secondary outcomes due to the small sample size and the nature of the conducted feasibility study. In addition, a sensitivity analysis was not suitable with regard to this data basis.
Strengths and limitations
Our complex intervention (ICU follow-up clinic) was developed in a participatory multi-stakeholder process. This enabled us to consider as many different perspectives as possible. The intervention was subsequently implemented in an RCT and the entire concept was tested for feasibility. The external evaluation as well as the (initially blinded) outcomes assessment further improved the quality of the here presented concept and study. This should be also considered in the large-scale trial in order to evaluate the effectiveness of the ICU follow-up clinic. In this study, we were not able to identify the exact healthcare trajectories of each participant after the ICU stay and we did not gather data on healthcare use before their critical illness. Therefore, no comparison on healthcare use before/after critical illness was possible. Even in light of COVID-19, we were able to restart and manage the study, however with a reduced number of participants. Statistical testing regarding the RCT’s primary outcome was not intended per our study protocol [28]. The low number of feasibility studies of ICU follow-up clinics is remarkable. We contribute to this body of research by providing a pilot study that went through all the stages of a proper RCT, including an extensive feasibility analysis of the procedures. We have collected and reported on the decisive parameters that are mentioned in the literature on pilot studies [44, 45, 70, 71]. It seems essential to define clear feasibility criteria, measure relevant outcomes and evaluate the respective pilot study before a definitive trial on complex health care intervention in order to avoid “ineffective” effectiveness trials.
Comparison to other ICU follow-up services feasibility studies
Previous studies on ICU follow-up clinics have mainly been conducted as full RCTs. Teixeira et al. [72] compiled an overview on effectiveness and feasibility of 30 studies on ICU follow-up clinics and did not find statistically significant effects in patients or their next of kin. They concluded that only individualized aftercare might be the right model for post-ICU patients. Six of the included studies were RCTs. However, none of these studies was a feasibility trial. In a systematic review of Schofield-Robinson et al. [73] on the effectiveness of ICU follow‐up services, the authors included five studies (four RCTs, one non‐randomised study) and concluded that there was only low-certainty of evidence that ICU follow-up services may make little or no improvements regarding HRQOL or PTSD at 12 months after ICU discharge. The systematic review of Geense et al. [74] on non-pharmacologic interventions to prevent PICS included ten pilot studies and five studies on ICU follow-up services but without overlap between those two groups. The four included studies on follow-up services are the same as in the systematic review of Schofield-Robinson et al. [22, 75,76,77]. One reason for the limited possibility to show effects of an ICU follow-up clinic on e.g. HRQOL or psychosocial wellbeing might be that only little effort has been dedicated to evaluate the feasibility of the proposed intervention and to perform a pilot study in advance. We identified three pilot studies [78,79,80] on ICU follow-up clinics (two RCTs, one cohort study, details in Table 5).
Henderson et al. [79] performed a single-centre feasibility cohort trial on a five-week multidisciplinary peer support rehabilitation programme for ICU survivors (complex intervention) and measured its impact on HRQOL, anxiety, depression, pain and caregiver strain through surveys. The intervention [81] contained a de-brief of the ICU stay, physical assessment and dedicated physiotherapy, review of medication, advice on social care support and peer support groups. Inclusion criteria were a minimum duration of mechanical ventilation of 48 h and a prolonged ICU stay (no further details provided). 27 participants (67% male, median age 66 years) were followed-up 12 weeks, three and 12 months after ICU discharge. The intervention showed to be feasible and safe in the clinical environment with a participation rate of 24% and an attrition rate of 4%. The initial visit at the clinic was 12 weeks after discharge compared to 20 weeks in our study. In contrast to our study, HRQOL was measured at three points (baseline, after 3 and 12 months) with the EuroQol Visual Analogue Scale (EQ-VAS). The mean baseline value was 70 (52 in our study) and improved to 78.
The feasibility study on a paediatric ICU follow-up clinic from Samuel et al. [80] measured the risk for posttraumatic stress, anxiety, and depression of parents whose children stayed on ICU for at least 12 h and evaluated if a follow-up clinic appointment two months after discharge decreased this risk. Half of the approached parents (52%) participated in their study. Randomisation worked and they did not observe significant differences between intervention and control group. The authors report a similar completeness of outcome measurement instruments to our study (75% vs. 77%). Uniquely, the study group included a low-risk group of parents (n = 131) which was not involved into the randomised trial but assessed in lights of acceptability measures. E.g. they were asked if the lack of invitation to the follow-up clinic was upsetting, which they denied. Further, 56% parents in the control group would have liked to visit the follow-up clinic. Identified barriers to visit the follow-up clinic were e.g. difficulties arranging time off work, travel costs or distance from hospital. In lights of signals for effectiveness, no significant differences were found between the intervention group and the control group six months after discharge.
Bloom et al. [78] performed a single-centre pilot RCT (“Vanderbilt study”) comparing an ICU recovery program to usual care. The program consisted of ten components (see Table 5) and were applied in between ICU discharge and 30 days after. Main feasibility outcome was the number of intervention components received. Further, readmission rate, death rate and health care utilisation were measured. Regarding the outpatient intervention components (the latter could be equivalent to an ICU follow-up clinic), only 8.1% attended an ICU recovery clinic appointment.
Conclusions
Our participatory designed ICU follow-up clinic and a pilot RCT assessing its effectiveness were feasible in terms of acceptability, fidelity, completeness and practicality. Regarding the primary outcome physical HRQOL, there were no signals for improvement six months after discharge from the ICU. We recommend planning and conducting a multicentre study to evaluate the effects of our proposed ICU follow-up clinic, subject to aforementioned adjustments.
Availability of data and materials
Data can be requested from the principal investigator (CA) upon reasonable request.
Notes
In the German health care system 5 grades of nursing care (until 2016 known as levels of care) are assigned to persons, who cannot manage their daily lives independently and are dependent on the help of relatives or professional staff. The guidelines are anchored in the Eleventh Book of the Social Code Book (SGB XI). Further information on long-term care in Germany can be obtained elsewhere [59].
Abbreviations
- h:
-
hours
- HRQOL:
-
Health related quality of life
- ICU:
-
Intensive Care Unit
- Kg:
-
Kilogram
- Km:
-
Kilometre
- min:
-
minutes
- PICS:
-
Post-intensive care syndrome
- PTSD:
-
Posttraumatic stress disorder
- QoL:
-
Quality of life
- s:
-
seconds
- SAPS:
-
Simplified Acute Physiology Score
- SD:
-
Standard deviation
- SOFA-Score:
-
Sepsis-related organ failure score
References
Inoue S, Hatakeyama J, Kondo Y, Hifumi T, Sakuramoto H, Kawasaki T, et al. Post-intensive care syndrome: its pathophysiology, prevention, and future directions. Acute Med Surg. 2019;6:233–46. https://doi.org/10.1002/ams2.415.
Fernandes A, Jaeger MS, Chudow M. Post-intensive care syndrome: A review of preventive strategies and follow-up care. Am J Health Syst Pharm. 2019;76:119–22. https://doi.org/10.1093/ajhp/zxy009.
LaBuzetta JN, Rosand J, Vranceanu A-M. Review: Post-Intensive Care Syndrome: Unique Challenges in the Neurointensive Care Unit. Neurocrit Care. 2019;31:534–45. https://doi.org/10.1007/s12028-019-00826-0.
Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012;40:502–9. https://doi.org/10.1097/CCM.0b013e318232da75.
Davydow DS, Gifford JM, Desai SV, Needham DM, Bienvenu OJ. Posttraumatic stress disorder in general intensive care unit survivors: a systematic review. Gen Hosp Psychiatry. 2008;30:421–34. https://doi.org/10.1016/j.genhosppsych.2008.05.006.
Nikayin S, Rabiee A, Hashem MD, Huang M, Bienvenu OJ, Turnbull AE, Needham DM. Anxiety symptoms in survivors of critical illness: a systematic review and meta-analysis. Gen Hosp Psychiatry. 2016;43:23–9. https://doi.org/10.1016/j.genhosppsych.2016.08.005.
Parker AM, Sricharoenchai T, Raparla S, Schneck KW, Bienvenu OJ, Needham DM. Posttraumatic stress disorder in critical illness survivors: a metaanalysis. Crit Care Med. 2015;43:1121–9. https://doi.org/10.1097/ccm.0000000000000882.
Jolley SE, Bunnell AE, Hough CL. ICU-Acquired Weakness. Chest. 2016;150:1129–40. https://doi.org/10.1016/j.chest.2016.03.045.
Davidson JE, Harvey MA. Patient and Family Post-Intensive Care Syndrome. AACN Adv Crit Care. 2016;27:184–6. https://doi.org/10.4037/aacnacc2016132.
Harvey MA, Davidson JE. Postintensive Care Syndrome: Right Care, Right Now…and Later. Crit Care Med. 2016;44:381–5. https://doi.org/10.1097/CCM.0000000000001531.
Desai SV, Law TJ, Needham DM. Long-term complications of critical care. Crit Care Med. 2011;39:371–9. https://doi.org/10.1097/CCM.0b013e3181fd66e5.
Cuthbertson BH, Roughton S, Jenkinson D, Maclennan G, Vale L. Quality of life in the five years after intensive care: a cohort study. Crit Care. 2010;14:R6. https://doi.org/10.1186/cc8848.
Griffith DM, Salisbury LG, Lee RJ, Lone N, Merriweather JL, Walsh TS. Determinants of Health-Related Quality of Life After ICU: Importance of Patient Demographics, Previous Comorbidity, and Severity of Illness. Crit Care Med. 2018;46:594–601. https://doi.org/10.1097/CCM.0000000000002952.
Myhren H, Ekeberg Ø, Stokland O. Health-related quality of life and return to work after critical illness in general intensive care unit patients: a 1-year follow-up study. Crit Care Med. 2010;38:1554–61. https://doi.org/10.1097/CCM.0b013e3181e2c8b1.
Apfelbacher C, Brandstetter S, Blecha S, Dodoo-Schittko F, Brandl M, Karagiannidis C, et al. Influence of quality of intensive care on quality of life/return to work in survivors of the acute respiratory distress syndrome: prospective observational patient cohort study (DACAPO). BMC Public Health. 2020;20:861. https://doi.org/10.1186/s12889-020-08943-8.
Rosa RG, Ferreira GE, Viola TW, Robinson CC, Kochhann R, Berto PP, et al. Effects of post-ICU follow-up on subject outcomes: A systematic review and meta-analysis. J Crit Care. 2019;52:115–25. https://doi.org/10.1016/j.jcrc.2019.04.014.
Lasiter S, Oles SK, Mundell J, London S, Khan B. Critical Care Follow-up Clinics: A Scoping Review of Interventions and Outcomes. Clinical nurse specialist CNS. 2016;30:227–37. https://doi.org/10.1097/nur.0000000000000219.
Egerod I, Risom SS, Thomsen T, Storli SL, Eskerud RS, Holme AN, Samuelson KAM. ICU-recovery in Scandinavia: a comparative study of intensive care follow-up in Denmark, Norway and Sweden. Intensive Crit Care Nurs. 2013;29:103–11. https://doi.org/10.1016/j.iccn.2012.10.005.
Jensen JF, Thomsen T, Overgaard D, Bestle MH, Christensen D, Egerod I. Impact of follow-up consultations for ICU survivors on post-ICU syndrome: a systematic review and meta-analysis. Intensive Care Med. 2015;41:763–75. https://doi.org/10.1007/s00134-015-3689-1.
Griffiths JA, Barber VS, Cuthbertson BH, Young JD. A national survey of intensive care follow-up clinics. Anaesthesia. 2006;61:950–5. https://doi.org/10.1111/j.1365-2044.2006.04792.x.
Sevin CM, Jackson JC. Post-ICU Clinics Should Be Staffed by ICU Clinicians. Crit Care Med. 2019;47:268–72. https://doi.org/10.1097/CCM.0000000000003535.
Cuthbertson BH, Rattray J, Campbell MK, Gager M, Roughton S, Smith A, et al. The PRaCTICaL study of nurse led, intensive care follow-up programmes for improving long term outcomes from critical illness: a pragmatic randomised controlled trial. Bmj. 2009;339:b3723. https://doi.org/10.1136/bmj.b3723.
Mittag O, Welti F. Medizinische Rehabilitation im europäischen Vergleich und Auswirkungen des europäischen Rechts auf die deutsche Rehabilitation. [Comparison of medical rehabilitation in various European countries and the impact of European law on rehabilitation practice in Germany]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2017;60:378–85. https://doi.org/10.1007/s00103-017-2516-y.
Schmidt-Ohlemann M. Formen der Rehabilitation. In: Meyer T, Bengel J, Wirtz MA, editors. Lehrbuch Rehabilitationswissenschaften. 1st ed. Bern: Hogrefe; 2022. pp. 162-174. https://doi.org/10.1024/86067-000.
Stucki G, Stier-Jarmer M, Grill E, Melvin J. Rationale and principles of early rehabilitation care after an acute injury or illness. Disabil Rehabil. 2005;27:353–9. https://doi.org/10.1080/09638280400014105.
Bernardi C, Weiß A, Brandstetter S, Brandl M, Blecha S, Bein T, Apfelbacher C. Perspektiven von Patienten nach einem prolongierten Aufenthalt auf Intensivstation bezüglich einer Intensiv-Nachsorgeambulanz: eine qualitative Interviewstudie. Gesundheitswesen. 2018;80:94. https://doi.org/10.1055/s-0038-1667792.
Rohr M, Weiß A, Bein T, Bernardi C, Brandstetter S, Drewitz KP, et al. Experiences, opinions and expectations of health care providers towards an intensive care unit follow-up clinic: Qualitative study and online survey. Intensive Crit Care Nurs. 2021;67:103084. https://doi.org/10.1016/j.iccn.2021.103084.
Rohr M, Brandstetter S, Bernardi C, Fisser C, Drewitz KP, Brunnthaler V, et al. Piloting an ICU follow-up clinic to improve health-related quality of life in ICU survivors after a prolonged intensive care stay (PINA): study protocol for a pilot randomised controlled trial. Pilot Feasibility Studies. 2021;7:90. https://doi.org/10.1186/s40814-021-00796-1.
Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, Tyrer P. Framework for design and evaluation of complex interventions to improve health. BMJ. 2000;321:694–6. https://doi.org/10.1136/bmj.321.7262.694.
Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ. 2015;350:h1258. https://doi.org/10.1136/bmj.h1258.
World Medical Association. Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4. https://doi.org/10.1001/jama.2013.281053.
Vincent JL, Moreno R, Takala J, Willatts S, Mendonça A de, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–10. https://doi.org/10.1007/BF01709751.
Schulz KF, Grimes DA. Allocation concealment in randomised trials: defending against deciphering. Lancet. 2002;359:614–8. https://doi.org/10.1016/S0140-6736(02)07750-4.
Deutschen Sepsis-Hilfe e. V. Die Zeit der Intensivstation: Ein Leitfaden für Patienten und Angehörige. 2011. https://icusteps.org/assets/files/booklet/languages/Intensiv_Info_A5_Web.pdf. Accessed 22 Jan 2019.
Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The Mini-Cog: a cognitive “vital signs” measure for dementia screening in multi-lingual elderly. Int J Geriat Psychiatry. 2000;15:1021–7. https://doi.org/10.1002/1099-1166(200011)15:11%3c1021::aid-gps234%3e3.0.co;2-6.
Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1–3):163–73. https://doi.org/10.1016/j.jad.2008.06.026.
Löwe B, Spitzer R, Zipfel S, Herzog W. PHQ-D Gesundheitsfragebogen für Patienten: Autorisierte deutsche Version des "Prime MD Patient Health Questionnaire (PHQ)". 2nd ed. 2002.
Maercker A. Posttraumatische Stress Skala-10 (PTSS-10)-deutsche Version modifiziert nach Schüffel & Schade (unveröffentlicht). Manuskript: Technische Universität Dresden; 1998.
Feldman EL, Stevens MJ, Thomas PK, Brown MB, Canal N, Greene DA. A practical two-step quantitative clinical and electrophysiological assessment for the diagnosis and staging of diabetic neuropathy. Diabetes Care. 1994;17:1281–9. https://doi.org/10.2337/diacare.17.11.1281.
Meyer T, Bengel J, Wirtz MA. Definitionen der Rehabilitation und zentraler Begriffe. In: Meyer T, Bengel J, Wirtz MA, editors. Lehrbuch Rehabilitationswissenschaften. 1st ed. Bern: Hogrefe; 2022. pp. 28-41.
Bundesarbeitsgemeinschaft für Rehabilitation. Empfehlungen zur Neurologischen Rehabilitation von Patienten mit schweren und schwersten Hirnschädigungen in den Phasen B und C. 1999. https://www.bar-frankfurt.de/service/publikationen/produktdetails/produkt/35.html. Accessed 3 Jul 2023.
Steinke B. Leistungsträger der Rehabilitation und Einleitung von Leistungen zur Teilhabe und diagnostische Voraussetzungen. Akt Rheumatol. 2004;29:276–81. https://doi.org/10.1055/s-2004-813664.
Gutenbrunner C. Zielsetzungen der Rehabilitation bei rheumatischen Erkrankungen und Rehabilitationsformen. Akt Rheumatol. 2004;29:227–31. https://doi.org/10.1055/s-2004-813649.
Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, et al. How we design feasibility studies. Am J Prev Med. 2009;36:452–7. https://doi.org/10.1016/j.amepre.2009.02.002.
Orsmond GI, Cohn ES. The Distinctive Features of a Feasibility Study: Objectives and Guiding Questions. OTJR (Thorofare N J). 2015;35:169–77. https://doi.org/10.1177/1539449215578649.
Ware Jr JE, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996:220–33. https://doi.org/10.1097/00005650-199603000-00003.
Morfeld M, Kirchberger I, Bullinger M. SF-36 Fragebogen zum Gesundheitszustand: Deutsche Version des Short Form-36 Health Survey. 2nd ed. Göttingen: Hogrefe; 2011.
Mahoney FI, Barthel DW. Functional evaluation: The Barthel index: A simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Md State Med J. 1965;14:61–5.
Lübke N, Meinck M, Von Wolfgang RK. The Barthel Index in geriatrics A. context analysis for the Hamburg Classification Manual. Z Gerontol Geriatr. 2004;37:316–26. https://doi.org/10.1007/s00391-004-0233-2.
Fuchs J, Busch MA, Gößwald A, Hölling H, Kuhnert R, Scheidt-Nave C. Physical and cognitive capabilities among persons aged 65–79 years in Germany: results of the German Health Interview and Examination Survey for Adults (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56:723–32. https://doi.org/10.1007/s00103-013-1684-7.
Cooper R, Kuh D, Cooper C, Gale CR, Lawlor DA, Matthews F, Hardy R. Objective measures of physical capability and subsequent health: a systematic review. Age Ageing. 2011;40:14–23. https://doi.org/10.1093/ageing/afq117.
Bobos P, Nazari G, Lu Z, MacDermid JC. Measurement Properties of the Hand Grip Strength Assessment: A Systematic Review With Meta-analysis. Arch Phys Med Rehabil. 2020;101:553–65. https://doi.org/10.1016/j.apmr.2019.10.183.
Beaton DE, O’Driscoll SW, Richards RR. Grip strength testing using the BTE work simulator and the Jamar dynamometer: A comparative study. The Journal of hand surgery. 1995;20:293–8.
Stoll C, Kapfhammer HP, Rothenhäusler HB, Haller M, Briegel J, Schmidt M, et al. Sensitivity and specificity of a screening test to document traumatic experiences and to diagnose post-traumatic stress disorder in ARDS patients after intensive care treatment. Intensive Care Med. 1999;25:697–704. https://doi.org/10.1007/s001340050932.
Weisæth L. Torture of a Norwegian ship’s crew: The torture, stress reactions and psychiatric after-effects. Acta Psychiatr Scand. 1989;80:63–72.
Spitzer RL, Kroenke K, Williams JBW. Patient Health Questionnaire Primary Care Study Group. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA. 1999;282:1737–44.
Spitzer RL, Williams JBW, Kroenke K, Linzer M, Verloin de Gruy F, Hahn SR, et al. Utility of a New Procedure for Diagnosing Mental Disorders in Primary Care. JAMA. 1994;272:1749. https://doi.org/10.1001/jama.1994.03520220043029.
Greiner W. A European EQ-5D VAS valuation set. In: Brooks R, Rabin R, de Charro F, editors. The Measurement and Valuation of Health Status Using EQ-5D: A European Perspective. Dordrecht: Springer; 2003. p. 103–42.
Federal Ministry of Health. Long-Term Care Guide. 22nd ed. Berlin; 2020.
Rupp T, Butscheidt S, Jähn K, Simon MJ, Mussawy H, Oheim R, et al. Low physical performance determined by chair rising test muscle mechanography is associated with prevalent fragility fractures. Arch Osteoporos. 2018;13:71. https://doi.org/10.1007/s11657-018-0490-0.
Cooper R, Kuh D, Hardy R. Objectively measured physical capability levels and mortality: systematic review and meta-analysis. BMJ. 2010;341:c4467. https://doi.org/10.1136/bmj.c4467.
Dodds RM, Syddall HE, Cooper R, Benzeval M, Deary IJ, Dennison EM, et al. Grip strength across the life course: normative data from twelve British studies. PLoS ONE. 2014;9:e113637. https://doi.org/10.1371/journal.pone.0113637.
Kroenke K, Spitzer RL. The PHQ-9: A New Depression Diagnostic and Severity Measure. Psychiatr Ann. 2002;32:509–15. https://doi.org/10.3928/0048-5713-20020901-06.
Brinkman S, Bakhshi-Raiez F, Abu-Hanna A, de Jonge E, de Keizer NF. Determinants of mortality after hospital discharge in ICU patients: literature review and Dutch cohort study. Crit Care Med. 2013;41:1237–51. https://doi.org/10.1097/CCM.0b013e31827ca4f9.
Spies CD, Krampe H, Paul N, Denke C, Kiselev J, Piper SK, et al. Instruments to measure outcomes of post-intensive care syndrome in outpatient care settings – Results of an expert consensus and feasibility field test. J Intensive Care Soc. 2020:175114372092359. https://doi.org/10.1177/1751143720923597.
Needham DM, Sepulveda KA, Dinglas VD, Chessare CM, Friedman LA, Bingham CO, Turnbull AE. Core Outcome Measures for Clinical Research in Acute Respiratory Failure Survivors. An International Modified Delphi Consensus Study. Am J Respir Crit Care Med. 2017;196:1122–30. https://doi.org/10.1164/rccm.201702-0372OC.
Rose L, Burry L, Agar M, Blackwood B, Campbell NL, Clarke M, et al. A core outcome set for studies evaluating interventions to prevent and/or treat delirium for adults requiring an acute care hospital admission: an international key stakeholder informed consensus study. BMC Med. 2021;19:143. https://doi.org/10.1186/s12916-021-02015-3.
Taft C, Karlsson J, Sullivan M. Do SF-36 summary component scores accurately summarize subscale scores? Qual Life Res. 2001;10:395–404. https://doi.org/10.1023/a:1012552211996.
Whitehead AL, Julious SA, Cooper CL, Campbell MJ. Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat Methods Med Res. 2016;25:1057–73. https://doi.org/10.1177/0962280215588241.
Chan CL, Leyrat C, Eldridge SM. Quality of reporting of pilot and feasibility cluster randomised trials: a systematic review. BMJ Open. 2017;7:e016970. https://doi.org/10.1136/bmjopen-2017-016970.
Arnold DM, Burns KEA, Adhikari NKJ, Kho ME, Meade MO, Cook DJ. The design and interpretation of pilot trials in clinical research in critical care. Crit Care Med. 2009;37:S69-74. https://doi.org/10.1097/CCM.0b013e3181920e33.
Teixeira C, Rosa RG. Ambulatório pós-unidade de terapia intensiva: é viável e efetivo? Uma revisão da literature. [Post-intensive care outpatient clinic: is it feasible and effective? A literature review]. Rev Bras Ter Intensiva. 2018;30:98–111. https://doi.org/10.5935/0103-507X.20180016.
Schofield-Robinson OJ, Lewis SR, Smith AF, McPeake J, Alderson P. Follow-up services for improving long-term outcomes in intensive care unit (ICU) survivors. Cochrane Database Syst Rev. 2018;11:CD012701. https://doi.org/10.1002/14651858.CD012701.pub2.
Geense WW, van den Boogaard M, van der Hoeven JG, Vermeulen H, Hannink G, Zegers M. Nonpharmacologic Interventions to Prevent or Mitigate Adverse Long-Term Outcomes Among ICU Survivors: A Systematic Review and Meta-Analysis. Crit Care Med. 2019;47:1607–18. https://doi.org/10.1097/CCM.0000000000003974.
Schmidt K, Worrack S, von Korff M, Davydow D, Brunkhorst F, Ehlert U, et al. Effect of a Primary Care Management Intervention on Mental Health-Related Quality of Life Among Survivors of Sepsis: A Randomized Clinical Trial. JAMA. 2016;315:2703–11. https://doi.org/10.1001/jama.2016.7207.
Jensen JF, Egerod I, Bestle MH, Christensen DF, Elklit A, Hansen RL, et al. A recovery program to improve quality of life, sense of coherence and psychological health in ICU survivors: a multicenter randomized controlled trial, the RAPIT study. Intensive Care Med. 2016;42:1733–43. https://doi.org/10.1007/s00134-016-4522-1.
Douglas SL, Daly BJ, Kelley CG, O’Toole E, Montenegro H. Chronically critically ill patients: health-related quality of life and resource use after a disease management intervention. Am J Crit Care. 2007;16:447–57.
Bloom SL, Stollings JL, Kirkpatrick O, Wang L, Byrne DW, Sevin CM, Semler MW. Randomized Clinical Trial of an ICU Recovery Pilot Program for Survivors of Critical Illness. Crit Care Med. 2019;47:1337–45. https://doi.org/10.1097/CCM.0000000000003909.
Henderson P, Quasim T, Asher A, Campbell L, Daniel M, Davey L, et al. Post-intensive care syndrome following cardiothoracic critical care: Feasibility of a complex intervention. J Rehabil Med. 2021. https://doi.org/10.2340/16501977-2825.
Samuel VM, Colville GA, Goodwin S, Ryninks K, Dean S. The Value of Screening Parents for Their Risk of Developing Psychological Symptoms After PICU: A Feasibility Study Evaluating a Pediatric Intensive Care Follow-Up Clinic. Pediatr Crit Care Med. 2015;16:808–13. https://doi.org/10.1097/PCC.0000000000000488.
McPeake J, Shaw M, Iwashyna TJ, Daniel M, Devine H, Jarvie L, et al. Intensive Care Syndrome: Promoting Independence and Return to Employment (InS:PIRE). Early evaluation of a complex intervention. PLoS ONE. 2017;12:e0188028. https://doi.org/10.1371/journal.pone.0188028.
Acknowledgements
The authors would like to thank Thomas Bein, who, together with CA and SB was largely responsible for the project’s conceptualisation, the successful acquisition of the funding and the start of the project. We appreciate the commitment of Annette Weiß who supported the PINA study as a valuable colleague during the first year of study. We would like to thank Stefanie March and Christoph Stallmann for providing consulting advice regarding data protection issues. Further, we highly appreciate the commitment of our study nurse Christine Liebl who thoroughly performed the screening of eligible patients and took care of all study participants during intervention and follow-up assessment. Moreover, we would like to thank Philipp Schmidt, who assisted in data cleaning and analyses. Finally, we are grateful for the valuable shared experiences and the commitment of all our study participants both those in the concept development and those in the pilot study.
Funding
The study was funded by the Innovation Fund of the Federal Joint Committee (Innovationsfond G-BA), funding code 01VSF16056, which was neither involved in the study design, nor in the collection, analysis and interpretation of data, nor the writing of the article, nor the decision to submit the results for publication. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
CA and SB had the idea for the study and obtained funding for the study. CA, SB, MR, CB, CF and MVM developed the research design and methods with advice from KS. PD, MR and CA developed the data protection concept and finalized the study protocol. MR, VB and PD developed the study materials with input from CF and MVM. CF, MVM and KP collected clinical data. PD, CH, CB and KP managed and analysed data. CB, MR, VB and KP took field notes. PD wrote the article with input from CH, SB, CF, VB, PS, CB, CA, KS and MVM. All authors reviewed the article for important intellectual content.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The institutional Ethics Committee of the University of Regensburg (ref. 19–1522-101) approved the study protocol. The study was conducted in accordance with the declaration of Helsinki, the medical professional codex, the European General Data Protection Regulation (DS-GVO) and the Federal Data Protection Act (BDSG). Participants and their next of kin participated voluntarily and gave written informed consent. Participants were free to withdraw their participation at any time without negative consequences for their future medical care.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Drewitz, K.P., Hasenpusch, C., Bernardi, C. et al. Piloting an ICU follow-up clinic to improve health-related quality of life in ICU survivors after a prolonged intensive care stay (PINA): feasibility of a pragmatic randomised controlled trial. BMC Anesthesiol 23, 344 (2023). https://doi.org/10.1186/s12871-023-02255-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-023-02255-1