Abstract
Background and objectives
The erector spinae plane block (ESPB) and classical thoracolumbar interfascial plane (TLIP) block can reduce postoperative pain in lumbar surgery. In this study, we compared the efficacy of ESPB and classical TLIP block in providing perioperative analgesia in patients undergoing lumbar posterior decompression and stabilization by comparing postoperative pain, opioid consumption, and IL-6 and IL-10 serum concentrations between ESPB and classical TLIP block.
Method
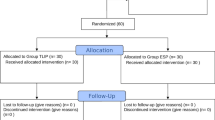
This was a prospective, double-blinded, randomized controlled trial in tertiary referral hospitals. Forty patients were randomized into two equal groups, each receiving either ESPB or classical TLIP block. The primary outcome was the difference in IL-6 and IL-10 serum concentrations at baseline and 6 h after lumbar posterior decompression and stabilization. The secondary outcome was total opioid consumption and pain score 24 h post-operatively.
Result
There were no significant differences between the ESPB and classical TLIP block groups in pain score, IL-6 and IL-10 concentration change, and total opioid consumption post-operatively. There was a significant difference in the time until the first dose of morphine was needed between the ESPB and classical TLIP block groups (300 min vs. 547.5 min; p = 0.002).
Conclusion
ESPB and classical TLIP block performance during lumbar surgery have comparable pain scores, IL-6 and IL-10 concentration differences pre- and post-operation, and total opioid consumption post-operatively. However, classical TLIP block provides a prolonged duration of analgesia.
Trial registration
ClinicalTrials.gov NCT04951024.
Similar content being viewed by others
Introduction
Posterior lumbar decompression and stabilization are surgical procedures that alter spinal instability and deformity [1, 2]. Spinal surgery is a procedure that results in severe pain on the first postoperative day [3]. Inadequate perioperative pain management will impact patient recovery, prevent mobilization and rehabilitation, and increase the risk of chronic pain [4].
Postoperative pain during lumbar decompression and posterior stabilization procedures accounts for the management of nociceptive, neuropathic, and inflammatory pain [5, 6] and is related to the surgical stress response [7,8,9,10]. It involves the release of proinflammatory cytokines such as interleukins (IL-1, IL-6), tumour necrosis factor-α (TNFα), and anti-inflammatory cytokines (IL-4, IL-10, transforming growth factor (TGF)). Interleukin-6 (IL-6) is the primary and first mediator involved in the induction and regulation of acute-phase protein synthesis and is released by hepatocytes after surgery or trauma [11]. IL-6 is the most relevant marker of tissue damage during surgical procedures and an important and accurate biomarker for pain [11,12,13]. The balance between proinflammatory and anti-inflammatory cytokines determines the postsurgical immune response, infection, and wound healing through local and systemic effects [14].
Erector spinae plane block (ESPB) and classical thoracolumbar interfascial plane (TLIP) block have been used recently to provide good pain control after posterior decompression and stabilization [15,16,17,18].
ESPB inhibits pain transmission in the dorsal of the thoracic and abdominal spinal nerves [19]. ESPB has been reported as part of multimodal analgesia that could significantly reduce opioid consumption and postoperative pain in lumbar spinal decompression surgery [16, 20]. The thoracolumbar interfascial plane (TLIP) block has also been reported as an effective regional anaesthetic technique for lumbar surgery [21]. TLIP blocks inhibit pain transmission on the dorsal ramus of the lumbar nerve [22,23,24].
The study was conducted to compare the efficacy of ESPB and classical TLIP block in providing perioperative analgesia among patients undergoing lumbar posterior decompression and stabilization. The primary outcome was the difference in IL-6 and IL-10 serum concentrations at baseline and 6 h after lumbar posterior decompression and stabilization, and the secondary outcomes were total opioid consumption and pain score at 24 h post-operatively.
Materials and methods
This was a prospective, double-blinded randomized controlled trial in two parallel groups conducted in two tertiary referral hospitals. The study protocol was carried out in accordance with relevant guidelines and regulations and was approved by the Ethics Committee of Medical Faculty Universitas Indonesia (KET-99/UN2.F1/ETIK/PPM.00.02/2021) and Universitas Syiah Kuala – Zainoel Abidin Hospital (122/EA/FK-RSUDZA/2021) prior to the study. The study was also registered at ClinicalTrial.gov (NCT04951024; 06/07/2021). Informed consent for study participation was obtained from all patients and/or their legal guardian(s). No violation of the Helsinki Declaration occurred during the informed consent and data acquisition period.
Participants
Eligible patients were adults aged 18–65 years old, ASA I-III, with body mass index 18.5–27.0 kg/m2 who were undergoing elective posterior lumbar decompression and stabilization surgery. Patients who had a history of chronic opioid consumption, coagulation disorder, cognitive disorder, or infection at the injection site were excluded from this study.
Sample size calculation
The sample size was calculated based on the unpaired numerical analytical research formula. The standard deviation in the unpaired group was the combined standard deviation of the two groups. Type I error was set at 5%, one-way hypothesis so that Za = 1.64. The type II error was set at 10%, and Zb = 1.28. Based on IL-6 (S = 13.1; X1-X2 = 13) and IL-10 (S = 8.6; X1-X2 = 9) concentrations [14] in a previous study, the calculated sample size was as follows:
Za = standard derivative alpha.
Zb = standard derivative beta.
S = the combined standard deviation of the compared groups.
X1 – X2 = the minimum difference in the mean that is considered significant.
There are a limited number of studies that utilize IL-6 and IL-10 as markers of inflammation, especially in patients undergoing spinal surgery. In this study, we used Amin et al.’s study [14], which has the most similar population, to determine the S value in a study of pro- and anti-inflammatory cytokines in surgery.
This study would require a sample size of 18 for each group. We included 18 participants in each group. A total of 40 participants enrolled in this study, with comparable allocation to two arms, allowing for a drop-out of 10%.
Procedures
Patients were randomized by computer-generated block randomization (www.randomizer.org) in a 1:1 ratio to the ESPB or classical TLIP block groups with stratification according to centre. Random allocation was performed by a research assistant who was not directly involved in the research. Randomization results were put into opaque sealed envelopes. The patients, anaesthesiologists who performed intraoperative monitoring, and the Acute Pain Service personnel were blinded to the intervention.
The first blood sample for measuring IL-6 and IL-10 levels was taken when the patient arrived in the operating room. An anaesthesiologist who was not aware of the size of the randomization blocks opened the sealed envelope. ESPB or TLIP block was performed according to the subject allocation.
ESPB or classical TLIP blocks were performed at the L3 level in a prone position after the induction of general anaesthesia (Fig. 1). Since both ESPB and TLIP block could extend 2–3 levels cranially and caudally, we provided analgesia for the whole lumbar segment by performing the blocks on L3. ESPB was conducted by local anaesthetic injection into the interfascial space between m. Erector spinae and the transverse processes with ultrasound guidance. A low-frequency curved array transducer (Hitachi Arietta® 850 5–1 MHz) was placed longitudinally in a cephalocaudal orientation 2–3 cm lateral to the midline of the L3 vertebral column. After identifying m. Erector spinae superficial to the transverse process, an insulated 100 mm 22G nerve block needle was inserted in-plane in the cranial caudal direction until the needle tip contacted the transverse process. Two millilitres of local anaesthetic was injected to confirm proper needle placement deep into the erector spinae. Twenty millilitres of 0.25% bupivacaine was injected bilaterally in 5 ml increments, with aspiration after every 5 ml.
In the classical TLIP block group, the low-frequency curved array transducer was placed in the transverse position at the level of the L3 vertebrae. After the identification of the spinous process, the probe was moved laterally to identify m. multifidus and m. longissimus. An insulated 100-mm 22G nerve block needle was inserted in-plane in the latero-medial direction towards m. multifidus. Two millilitres of local anaesthetic was injected to confirm proper needle placement in the interfascial space between m. multifidus and m. longissimus. Twenty millilitres of 0.25% bupivacaine was injected bilaterally in 5 ml increments, and aspiration was performed every 5 ml.
Another anaesthesiologist, who was blinded to the type of block, entered the operating room after the draping process was completed and performed the intraoperative monitoring. An additional 50 mcg intraoperative fentanyl was given if there was a sudden increase in pulse rate and blood pressure to more than 20% of the basal value. Another 25 mcg of fentanyl was given 5 min later if the pulse rate and blood pressure still escalated.
Postoperatively, paracetamol 1 g/8 h and PCA morphine, with a demand dose of 1 mg, lockout interval of 10 min, and maximum dose of 10 mg/4 h, were given.
In the ward, Acute Pain Service personnel assessed patients’ pain scales and performed blood sample collection. NRS pain scale at 1, 6, 12, and 24 h post-operatively and the first 24 h total morphine consumption were recorded. The second collection for serum IL-6 and IL-10 measurement was taken 6 h post-operatively.
Statistical analysis
Participants' baseline characteristics were analysed descriptively. Numerical variables are presented as the mean ± SD or median (IQR), while categorical variables are presented as frequency distributions. The data were tested for normality and homogeneity. Data were normally distributed and had a variance of homogeneity if the p value > 0.05 in the Shapiro‒Wilk test and Levene’s test, respectively. The difference between the two groups was analysed using an independent t test or Mann‒Whitney test. Two-sided p values were applied with a significance level of 5% for all tests.
Results
There were 40 eligible subjects recruited, with 20 subjects in each group (Fig. 2). The two groups were comparable regarding age, sex, duration of surgery, and the number of segments involved (Table 1).
There was no significant difference in intraoperative fentanyl consumption (p > 0.05), postoperative NRS score, and first 24 h of total morphine consumption (p > 0.05) between the two groups. However, the time to first morphine consumption post-operatively in the classical TLIP block group was significantly longer than that in the ESPB group (Table 2).
Before induction, the levels of the proinflammatory cytokine IL-6 and the anti-inflammatory cytokine IL-10 were not significantly different between the groups (Table 3). Likewise, 6 h after surgery, the levels of IL-6 and IL-10 were not significantly different (Table 3).
Discussion
This double-blind, randomized controlled trial (RCT) compares ESPB and classical TLIP block in lumbar posterior decompression and stabilization procedures in terms of stress response cytokines (IL-6 and IL-10), pain scale, and total perioperative opioid consumption. ESPB is effective as analgesia in lumbar spine surgery because it will consistently block the dorsal rami of the lumbar spinal nerves that innervate the back of the vertebra. ESPB also has extensive cranial and caudal spread through the paraspinal muscles from a single injection point, which aids ESPB in covering multiple vertebral levels [25,26,27,28,29,30,31]. Meanwhile, TLIP blocks the site of injection, which is located more superficially and further away from the lumbar nerve roots and plexus compared to ESPB. TLIP blocks the dorsal ramus and its branches exclusively in the lumbar distribution.
The local anaesthetic in ESPB was injected deep into the ESP muscle, protecting the solution from being washed out during the surgical procedure and focusing it on post-lumbar surgery pain [27]. Wang et al. found that ESPB provides a better postlumbar spine analgesia profile than TLIP block [27]. ESPB might be better than TLIP block in suppressing the formation of proinflammatory cytokines related to the stress response. ESPB might also provide a better sympathetic and inflammatory response that occurs perioperatively, such as an increase in blood flow, vascular permeability, and leukocyte accumulation.
For decades, cytokines have received more attention for physiological changes after trauma or surgery and acute and chronic inflammation. Under physiological conditions, pro- and anti-inflammatory cytokines act as immunomodulatory elements that prevent excessive damage caused by an inflammatory reaction. A dynamic balance relationship between pro- and anti-inflammatory cytokine changes affects organ dysfunction, immunity, infection, wound healing, and postoperative pain [32].
However, our results differed from those of previous research that hypothesized that a deeper injection of ESPB might provide better analgesia. At six hours, postoperative IL-6 and IL-10 levels were not significantly different between the ESPB and classical TLIP block groups (Table 3). ESPB did not have significantly better perioperative suppression of IL-6 levels compared with TLIP block.
These results may be attributed to pain pathways that were mainly involved in the posterior decompression and stabilization procedure. Pain in lumbar spine surgery mainly involves the dorsal rami of the vertebral nerve, which is covered by both blocks [16, 25], and both blocks work well on the dorsal rami of the vertebral nerve.
Our research results corroborate the previous statement that unlike thoracic ESPB, lumbar ESPB has limited spread to the ventral area. The deep back muscles in the lumbar spine, longissimus, and multifidus are more substantial and prominent in the lumbar region than in the thoracic region. In the lumbar region, local anaesthetic is concentrated within the thick musculature adjacent to the spine [31]. It was postulated that the complex attachments of the deep back musculature to the transverse processes may limit local anaesthetic spread in thoracic ESP injections [33].
Opioid doses that were given during the induction and maintenance of general anaesthesia might also contribute to these results. Opioids might have reduced the degree of perioperative pain in both groups, so the differences were not significant.
Likewise, we also found no significant difference in pain scales at 1, 6, 12, and 24 h post-operatively between ESPB and classical TLIP block (Table 2). The first 24 h of morphine consumption did not differ significantly between the two groups. An additional paracetamol dose of 1 g/8 h that was given as part of postoperative multimodal analgesia might also contribute to these results since the postoperative pain scale might be lowered.
However, we found that the time until first postoperative opioid administration was significantly longer in the classical TLIP block group than in the ESPB group (Table 2). Absorption of local anaesthetics from the injection site depends on the local anaesthetic’s concentration at the site of injection, total dose, vascularization, and concomitant vasoactive that was administered [34,35,36]. In this study, both groups were injected with identical local anaesthetic doses. In the lumbar region, a median of 5 mL of local anaesthetic is needed to cover one vertebral level by ESPB, which showed that lumbar ESPB has a wider compartment than other blocks. This may be in accordance with the different anatomy of vertebrae and the different spinal curves [25].
The wider compartment of ESPB and more homogeneous distribution of local anaesthetic on the injection plane in the lumbar region led to a rapid and extensive rate of local anaesthetic absorption in ESPB in comparison with other blocks. Cassai et al. reported that peak lidocaine concentration in blood was achieved 5 min after ESPB injection [37]. There have been no papers about local anaesthetic absorption in classical TLIP block yet. In our study, we found that classical TLIP block provides a longer duration of analgesia. Nonetheless, the duration of analgesia of classic TLIP block and ESPB remains inconclusive [27, 38, 39]. Both ESPB and classical TLIP block could provide analgesia 12–24 h after lumbar surgery. Further research regarding the local anaesthetic absorption rate in classic TLIP block is needed.
The limitations of this study included, first, the type of stress response biomarker that had been examined. This study only examined IL-6 and IL-10 cytokine levels to predict the stress response related to the posterior decompression and stabilization procedure. Further research with other mediators and biomarkers could provide more information to make our obtained data more robust. Second, the sample size was calculated using a study in a different setting, which could lead to our study being underpowered.
Conclusions
There was no significant difference in IL-6 and Il-10 levels and opioid consumption perioperatively between classical TLIP block and ESPB. However, classical TLIP block can provide the same analgesia as ESPB with a longer duration. Both blocks can be used as perioperative analgesia in decompression and posterior stabilization procedures.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Kalyvas J, Theodore N. Lumbar spine stabilization. Encyclopedia Neurol Sci. 2014;2:934–7.
Avis G, Gricourt Y, Vialatte P, Meunier V, Perin M, Simon N, et al. Analgesic efficacy of erector spinae plane blocks for lumbar spine surgery: a randomized double-blind controlled clinical trial. Reg Anesth Pain Med. 2022;47:610–6.
Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. 2013;118(4):934–44.
Bajwa SJS, Haldar R. Pain relief following spinal surgeries: a challenging task. J Spine. 2015;4(3):233.
Bajwa SJ, Haldar R. Pain management following spinal surgeries: an appraisal of the available options. J Craniovertebr Junction Spine. 2015;6(3):105–10.
Dunn LK, Durieux ME, Nemergut EC. Non-opioid analgesics: Novel approaches to perioperative analgesia for major spine surgery. Best Pract Res Clin Anaesthesiol. 2016;30(1):79–89.
Lotfinia I. A review: treatment of acute pain after lumbar discectomy. Orthop Surg Traumatol. 2017;1(5):174–81.
Moor D, Aggarwal G, Quiney N. Systemic response to surgery. Elsevier Ltd. 2017;35(4):220–3.
Gutierrez T, Hornigold R, Pearce A. The systemic response to surgery. Elsevier Ltd. 2014;32(3):149–52.
Scholl R, Bekker A, Babu R. Neuroendocrine and immune responses to surgery. Internet J Anesthesiol. 2012;30:1-8.
de Oliveira CM, Sakata RK, Issy AM, Gerola LR, Salomao R. Cytokines and pain. Rev Bras Anestesiol. 2011;61(2):255–9 60–5, 137–42.
Hashim S, Chin LY, Krishnasamy S, Sthaneswar P, Raja Mokhtar RA. Effect of sternal closure with biological bone adhesive on pain visual analogue score and serum cytokine. J Cardiothorac Surg. 2015;10:32.
Massel DH, Mayo BC, Long WW, Singh K. Multimodal analgesia in spine surgery: a commentary. J Pain Relief. 2015;4(6):218.
Amin OAI, Salah HE. The effect of general or spinal anaesthesia on pro- and anti-inflammatory intracellular cytokines in patients undergoing appendicectomy using flowcytometric method. Egypt J Anaesth. 2011;27:121–5.
Ekinci M, Ciftci B, Atalay YO. Ultrasound-guided modified thoracolumbar interfascial plane block is effective for pain management following multi-level lumbar spinal fusion surgery. Ain-Shams J Anesthesiol. 2019;11(24):1.
Yayik AM, Cesur S, Ozturk F, Ahiskalioglu A, Ay AN, Celik EC, et al. Postoperative analgesic efficacy of the ultrasound-guided erector spinae plane block in patients undergoing lumbar spinal decompression surgery: a randomized controlled study. World Neurosurg. 2019;126:e779–85.
Takahashi H, Suzuki T. Erector spinae plane block for low back pain in failed back surgery syndrome: a case report. JA Clin Rep. 2018;4(1):60.
Chin KJ, Lewis S. Opioid-free Analgesia for Posterior Spinal Fusion Surgery Using Erector Spinae Plane (ESP) Blocks in a Multimodal Anesthetic Regimen. Spine (Phila Pa 1976). 2019;44(6):E379-83.
Lopez MB, Cadorniga AG, Gonzales JML, Suarez ED, Carballo CL, Sobrino FP. Erector spinae block. A narrative review. Central Eur J Clin Res. 2018;1(1):28–39.
Singh S, Choudhary NK, Lalin D, Verma VK. Bilateral ultrasound-guided erector spinae plane block for postoperative analgesia in lumbar spine surgery: a randomized control trial. J Neurosurg Anesthesiol. 2019;32(4):330–4.
Chen K, Wang L, Ning M, Dou L, Li W, Li Y. Evaluation of ultrasound-guided lateral thoracolumbar interfascial plane block for postoperative analgesia in lumbar spine fusion surgery: a prospective, randomized, and controlled clinical trial. PeerJ. 2019;7: e7967.
Hand WR, Taylor JM, Harvey NR, Epperson TI, Gunselman RJ, Bolin ED, et al. Thoracolumbar interfascial plane (TLIP) block: a pilot study in volunteers. Can J Anaesth. 2015;62(11):1196–200.
Ciftci B, Ekinci M, Celik EC, Yayik AM, Aydin ME, Ahiskalioglu A. Ultrasound-guided erector spinae plane block versus modified-thoracolumbar interfascial plane block for lumbar discectomy surgery: a randomized. Controlled Study World Neurosurg. 2020;144:e849–55.
Ammar MA, Taeimah M. Evaluation of thoracolumbar interfascial plane block for postoperative analgesia after herniated lumbar disc surgery: a randomized clinical trial. Saudi J Anaesth. 2018;12(4):559–64.
De Cassai A, Andreatta G, Bonvicini D, Boscolo A, Munari M, Navalesi P. Injectate spread in ESP block: a review of anatomical investigations. J Clin Anesth. 2020;61: 109669.
Qiu Y, Zhang TJ, Hua Z. Erector spinae plane block for lumbar spinal surgery: a systematic review. J Pain Res. 2020;13:1611–9.
Wang L, Wu Y, Dou L, Chen K, Liu Y, Li Y. Comparison of two ultrasound-guided plane blocks for pain and postoperative opioid requirement in lumbar spine fusion surgery: a prospective, randomized, and controlled clinical trial. Pain Ther. 2021;10(2):1331–41.
Aponte A, Sala-Blanch X, Prats-Galino A, Masdeu J, Moreno LA, Sermeus LA. Anatomical evaluation of the extent of spread in the erector spinae plane block: a cadaveric study. Can J Anaesth. 2019;66(8):886–93.
Choi YJ, Kwon HJ, O J, Cho TH, Won JY, Yang HM, et al. Influence of injectate volume on paravertebral spread in erector spinae plane block: An endoscopic and anatomical evaluation. PLoS One. 2019;14(10):e0224487.
Bonvicini D, Boscolo-Berto R, De Cassai A, Negrello M, Macchi V, Tiberio I, et al. Anatomical basis of erector spinae plane block: a dissection and histotopographic pilot study. J Anesth. 2021;35(1):102–11.
Harbell MW, Seamans D, Koyyalamudi V, Kraus MB, Craner RC, Langley NR. Evaluating the extent of lumbar erector spinae plane block: an anatomical study. Reg Anesth Pain Med. 2020;45(8):640–4.
Hsing CH, Wang JJ. Clinical implication of perioperative inflammatory cytokine alteration. Acta Anaesthesiol Taiwan. 2015;53(1):23–8.
Ivanusic J, Konishi Y, Barrington MJ. A cadaveric study investigating the mechanism of action of erector spinae blockade. Reg Anesth Pain Med. 2018;43:567–77.
Taylor A, McLeod G. Basic pharmacology of local anaesthetics. BJA Educ. 2020;20(2):34–41.
Ahiskalioglu A, Yayik AM, Doymus O, et al. Efficacy of ultrasound-guided modified thoracolumbar interfascial plane block for postoperative analgesia after spinal surgery. Can J Anaesth. 2018;65(5):603–4.
Ahiskalioglu A, Tulgar S, Celik M, Ozer Z, Alici HA, Aydin ME. Lumbar erector spinae plane block as a main anesthetic method for hip surgery in high risk elderly patients: initial experience with a magnetic resonance imaging. Eurasian J Med. 2020;52:16–20.
De Cassai A, Bonanno C, Padrini R, Geraldini F, Boscolo A, Navalesi P, Munari M. Pharmacokinetics of lidocaine after bilateral ESP block. Reg Anesth Pain Med. 2021;46(1):86–9.
Ammar MA, Taeimah M. Evaluation of thoracolumbar interfascial plane block for postoperative analgesia after herniated lumbar disc surgery: a randomized clinical trial. Saudi J Anaesth. 2018;12(4):559–64.
Pavithran P, Sudarshan PK, Eliyas S, Sekhar B, Kaniachallil K. Comparison of thoracolumbar interfascial plane block with local anaesthetic infiltration in lumbar spine surgeries – a prospective double-blinded randomised controlled trial. Indian J Anaesth. 2022;66(6):436–41.
Acknowledgements
N/A.
Funding
N/A.
Author information
Authors and Affiliations
Contributions
Contributors ART, RR, AHMM, DS, and RBS planned and conceived the study. RR and AJR conducted the study survey. ART, AJR and RR processed and analysed the study data. ART, AHMM, DS, and RBS supervised the study. RR and ART developed the theoretical framework. ART, RR, AHMM, DS, AJR, and RBS wrote the manuscript. All authors discussed the results and commented on the manuscript. All authors revised the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of Medical Faculty Universitas Indonesia (KET-99/UN2.F1/ETIK/PPM.00.02/2021) and Universitas Syiah Kuala – Zainoel Abidin Hospital (122/EA/FK-RSUDZA/2021) prior to the study. Informed consent for study participation was obtained from all patients and/or their legal guardian(s). All protocols were carried out in accordance with relevant guidelines and regulations and were approved by the Ethics Committee prior to the study. The patients were verbally informed about the data acquisition protocol, and written informed consent was obtained from all patients and/or their legal guardian(s). No violation of the Helsinki Declaration occurred during the informed consent and data acquisition period.
Consent for publication
N/A.
Competing interests
All authors have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tantri, A.R., Rahmi, R., Marsaban, A.H.M. et al. Comparison of postoperative IL-6 and IL-10 levels following Erector Spinae Plane Block (ESPB) and classical Thoracolumbar Interfascial Plane (TLIP) block in a posterior lumbar decompression and stabilization procedure: a randomized controlled trial. BMC Anesthesiol 23, 13 (2023). https://doi.org/10.1186/s12871-023-01973-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-023-01973-w