Abstract
Background
Previous studies have suggested that the gender and/or age of a patient may influence the clinical outcomes of critically ill patients. Our aim was to determine whether there are gender- and age-based differences in clinical outcomes for mechanically ventilated patients in intensive care units (ICUs).
Methods
We performed a multicentre retrospective study involving adult patients who were admitted to the ICU and received at least 24 h of mechanical ventilation (MV). The patients were divided into two groups based on gender and, subsequently, further grouped based on gender and age < or ≥ 65 years. The primary outcome measure was hospital mortality.
Results
A total of 853 mechanically ventilated patients were evaluated. Of these patients, 63.2% were men and 61.5% were ≥ 65 years of age. The hospital mortality rate for men was significantly higher than that for women in the overall study population (P = 0.042), and this difference was most pronounced among elderly patients (age ≥ 65 years; P = 0.006). The durations of MV, ICU lengths of stay (LOS), and hospital LOS were significantly longer for men than for women among younger patients (P ≤ 0.013) but not among elderly patients. Multivariate logistic regression analysis revealed that male gender was independently associated with hospital mortality among elderly patients but not among younger patients.
Conclusions
There were important gender- and age-based differences in the outcomes among mechanically ventilated ICU patients. The combination of male gender and advanced age is strongly associated with hospital mortality.
Similar content being viewed by others
Introduction
Mechanical ventilation (MV) is one of the most commonly used treatment techniques in the intensive care unit (ICU). The proportion of patients receiving MV out of total ICU admissions has reached between 50 and 70% [1,2,3,4,5]. With our ageing population, the number of patients with MV will steadily increase, with a projected increase of 80% by 2026 when compared to 2000 [6]. Additionally, many studies have also shown that men account for more than half of the patients receiving MV in the ICU [2, 3, 7,8,9,10,11], and in the very elderly patients (aged ≥80 years), this proportion can reach more than 80% [12].
However, there have been few studies on the effect of gender on clinical outcomes of mechanically ventilated patients, and the results are inconsistent. Kollef et al. [13] used multivariate analysis to show that women requiring MV were at greater risk for hospital mortality than men. In contrast, two other prospective studies showed that gender was not independently associated with hospital mortality [7, 10]. It is not known whether these findings apply to other regions and patient populations. Our hypothesis was that there are significant differences in clinical outcomes between mechanically ventilated men and women, and that such gender-related differences may depend on age. To further investigate this hypothesis, we conducted a multicentre retrospective study of ICUs in Beijing.
Materials and methods
Study setting and design
This retrospective observational cohort study was carried out in fourteen ICUs of thirteen tertiary teaching hospitals in Beijing between January 2012 and June 2013.
Among the fourteen participating ICUs, ten were medical-surgical ICUs, two were surgical ICUs, one was a respiratory ICU, and one was a medical ICU. The number of ICU beds ranged from eight to twenty during the study period. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This retrospective study was approved by the Institutional Review Board of Fu Xing Hospital, Capital Medical University (Approval number: 2019FXHEC-KY167), and a waiver of informed consent was granted.
Study population
Patients who were admitted to the ICU and received at least 24 h of invasive MV within the first 48 h of their ICU stay were eligible. Patients were excluded if they were younger than 18 years old, had incomplete datasets, were diagnosed with a neuromuscular disease, required chronic MV prior to hospital admission, or were transferred from other facilities and had already been intubated or tracheotomised. A patient was considered one case if they were admitted to the ICU several times during the study period, and only data from the first ICU admission were analysed.
In our study, older patients were defined as those ≥65 years of age at the time of hospital admission and the cohort was divided on the basis of gender and age (< or ≥ 65 years).
Data collection
For every enrolled patient, the following data were recorded: demographic and epidemiological characteristics; the source of ICU admission; comorbidities; the severity of the illness; the primary indication for MV; arterial blood gas measurements; MV parameters and settings; the sedatives, analgesics, and neuromuscular blockers (NMBs) used during MV; the total duration of MV; the number of ventilator-free days; the occurrence of successful weaning within 30 days; the ICU and hospital lengths of stay (LOS); ICU and hospital costs; events occurring over the course of MV; the occurrence of withholding or withdrawing life-sustaining treatments; and the discharge destination. The severity of illness was assessed using the Acute Physiology and Chronic Health Evaluation (APACHE) II scoring system [14]. In this study, we adopted the acute respiratory distress syndrome (ARDS) Network predicted body weight (PBW) equation [15] to standardize mechanical ventilation tidal volumes setting.
Outcomes of interest
The primary outcome of interest was hospital mortality. The secondary outcomes included the duration of MV, the hospital and ICU LOS, and ICU mortality.
Statistical analysis
Statistical analyses were carried out using SPSS 21.0 (SPSS Inc., Chicago, Illinois, USA). Data are expressed as the mean ± standard deviation for normally distributed continuous variables, the median (interquartile range) for nonnormally distributed variables, and the number (percentage) for categorical variables. Continuous variables were compared using the Mann–Whitney U test. Categorical variables were compared using the chi-square test or Fisher’s exact test. Multiple logistic regression with forwards stepwise selection was used to determine the risk factors for hospital mortality. Variables with a P value < 0.20 during univariate analysis as well as the variable of gender were entered into the multivariate analysis. To investigate how gender-related differences might depend on age, we prospectively chose 65 years of age as the cut-off and performed two separate multivariate analyses. A two-sided P value < 0.05 was considered statistically significant.
Results
Baseline characteristics
During the study period, we evaluated 875 patients who were admitted to the ICUs and received mechanical ventilation for at least 24 h. Twenty-two patients were excluded from the study for reasons including an age < 18 years (n = 2), readmission to the ICU (n = 4), and incomplete clinical data (n = 16). Therefore, 853 patients were enrolled in this study. Of these, 539 (63.2%) were men and 314 (36.8%) were women. There were 328 patients under the age of 65 years (38.5%) and 525 patients aged 65 years and older (61.5%). The baseline characteristics of the study population are shown in Table 1.
Overall, there were no significant differences between the genders in age, body mass index (BMI), the need for noninvasive mechanical ventilation (NIMV) before ICU admission, the source of ICU admission, APACHE II scores, or the number of comorbidities. There was also no significant difference in the primary indication for MV between the genders, except for reasons due to trauma and coma. However, we found a significant difference in the proportion of men and women who had a history of smoking (50.3% vs. 9.6%, respectively; P < 0.001). Before the onset of MV, men tended to have a lower pulse oxygen saturation (Spo2; P = 0.032).
However, both in the overall study population and in the older age group, when we compared the APACHE II scores according to the indication for mechanical ventilation, we found that patients had significantly higher APACHE II scores, as was the case for men in the ARDS category (P = 0.032 and P = 0.036, respectively) and women in the cardiac arrest category (P = 0.035 and P = 0.026, respectively; see Additional file 1).
Management of mechanically ventilated ICU patients
Table 2 shows the data related to mechanically ventilated patient management, which was stratified by age and gender. There was a significant difference in the tidal volumes setting between men and women (P < 0.001), which remained significant even after stratification by age (P < 0.001). The incidence rates of ventilator-associated pneumonia (VAP) and tracheostomy in both men and women were high, but the incidence rate of self-extubation was low. Among the younger age group (< 65 years), we found that the incidence rates of VAP and tracheostomy were significantly higher among men than among women. However, there was no significant difference in these rates among the older age group (≥ 65 years). No differences were found between men and women in the choice of MV mode, the use of positive end-expiratory pressure (PEEP), or the use of sedatives, analgesics and NMBs.
Clinical outcomes
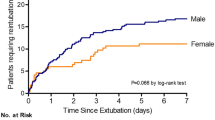
As shown in Table 3, the duration of MV, ICU LOS, and hospital LOS were significantly longer for men than for women among the younger age group (P ≤ 0.013), but no significant differences were observed in these times among the older age group.
Despite the observation that men and women aged 65 years or older had similar severities upon ICU admission, mortality was higher among men than among women in the ICU (42.6% vs. 31.4%, respectively; P = 0.011) and in the hospital (45.6% vs. 33.5%, respectively; P = 0.006) (Table 3). Mortality rates did not differ significantly between younger men and women.
When we compared the duration of mechanical ventilation, ICU mortality and hospital mortality according to the indication for mechanical ventilation, gender, and age, we found that there were no differences in the duration of mechanical ventilation between mechanically ventilated men and women in the overall study population or in both age groups. We found that the ICU mortality and hospital mortality rates for men were significantly higher than those for women postoperatively in the overall study population (11.8% vs. 4.7%, P = 0.030 and 14.9% vs. 5.5%, P = 0.009, respectively), although there was no significant difference in the APACHE II scores between the men and women (P = 0.749). Similarly, this trend was also shown in the older age group (P = 0.071 and P = 0.033, respectively). No differences in ICU mortality and hospital mortality were found between the men and women after stratification based on other categories and age (see Additional files 1-3).
In the overall study population, as well as in both age groups, men had higher hospital and ICU costs than women. There was no significant difference in the occurrence of withholding or withdrawing life-sustaining treatments between men and women in the overall study population or in either age group. Overall, the proportion of women who were discharged directly home was higher than that of men.
Multivariate logistic regression analyses
Using multivariate logistic regression analysis, we found that age, gender, the source of ICU admission (medical ward), APACHE II scores, hospital LOS, events occurring over the course of MV, and the decision to withhold or withdraw life-sustaining treatments were independently associated with hospital mortality in the overall study population (Table 4).
To study whether gender-related differences might depend on age, we prospectively chose a cut-off value of 65 years of age. Therefore, we used separate models for patients younger than 65 years old and for those 65 years or older. We found that male gender was not independently associated with hospital mortality among patients younger than 65 years of age. However, after adjusting for all other factors, we found that male gender was independently associated with hospital mortality among older patients (adjusted odds ratio [AOR] = 2.074; 95% confidence interval [CI] = 1.315 to 3.269; P = 0.002), as shown in Table 4. The multiple logistic regression analysis also demonstrated that patient age was independently associated with hospital mortality among elderly patients.
Discussion
The main finding of this study was that there were gender and age-related differences in the clinical outcomes of mechanically ventilated ICU patients. Specifically, we found that male gender was independently associated with hospital mortality in the overall study population as well as among elderly patients, but not among younger patients.
As reported in other studies [2, 3, 7,8,9,10,11], we found that men account for more than half of the patients (63.2%) receiving MV in the ICU. These findings are even more surprising when we consider the gender distribution of the Chinese urban adult population. For example, in 2010, women accounted for nearly 50% of the Chinese urban adult population, and this proportion increased with age [16]. It is not clear why the proportion of women receiving MV in the ICU is generally lower than that of men, but this may be due to differences in treatment preferences or gender bias. Women were less likely than men to be admitted to an ICU and to receive care and life-supporting treatments such as MV, although the severity of illness was similar in men and women or even higher in women [3, 17,18,19,20]. This difference in care may stem from less aggressive treatment preferences by women (or their surrogates) [18, 21, 22]. Furthermore, Sagy et al. [23] reported that both the physician and the patient being female was associated with a decreased ICU admission rate of critically ill patients. Their findings indicated the existence of possible gender bias where the patient and the treating physician both being female diminish the likelihood of restricted health resource use.
Although previous studies have explored the effects of gender on the outcomes of mechanically ventilated ICU patients, the findings across these studies are often inconsistent [7, 10, 13]. Our results are also inconsistent with or even contrary to these previous studies. The possible reasons for this inconsistency are as follows: (I) Age has been shown to be independently associated with mortality in mechanically ventilated ICU patients, and this correlation increases with age [5, 7, 13]. The mean age of the patients included in the three studies was significantly different, and all patients were younger than 65 years old. In our study, the mean age of the patients was 66 years old, and 61.5% of the patients were 65 years or older. (II) Two of the three studies did not further explore the effect of the interaction between age and gender on the outcomes of mechanically ventilated patients. Fowler et al. [3] found that sex- and age-related differences exist among ICU admissions, treatment with specific life-supporting interventions, and short- and long-term outcomes. Mahmood et al. [19] also found that there was a statistically significant interaction between gender and age among critically ill patients. In this study, we also demonstrated that there were gender- and age-related differences in clinical outcomes among mechanically ventilated ICU patients. Male gender was found to be independently associated with hospital mortality among elderly patients but not among younger patients. Therefore, when evaluating the effect of gender on the outcomes of mechanically ventilated patients, we should not ignore the age-related effect. (III) In previous studies, mechanically ventilated patients were either all medical patients [10], mainly medical patients [7], or half medical and half surgical patients [13]. In this study, among the younger age group, more than half of the mechanically ventilated patients came from the surgical ward, while in the older age group, this proportion decreased significantly. Reinikainen et al. [24] found that male gender was independently associated with increased hospital mortality among postoperative patients and among patients aged 75 years or older, but not among medical patients. Women had a higher mortality than men after coronary artery bypass graft surgery and a lower mortality with COPD exacerbation. There was no difference in mortality for acute coronary syndrome, sepsis, or trauma among the critically ill patients [19]. Therefore, referral bias or differences in the composition of ICU admission diagnoses may also contribute to inconsistencies in the study results.
When investigating the reasons for the gender differences in the clinical outcomes of mechanically ventilated ICU patients, in addition to considering age, hormonal status should also be an important factor. In numerous clinical and experimental studies, sex hormones have been shown to affect gender-specific immune responses and organ functions after shock, trauma, and sepsis. Specifically, studies have indicated that female hormones are protective in both immune responses and organ functions, whereas male sex hormones are deleterious [25,26,27,28]. In fact, the inflammatory response to infection seems to be exacerbated in males compared with females [29]. The available information indicates that sex hormones play a key role in regulating the immune response and organ function. In addition, there were gender differences in neuroendocrine and endothelial responses in critically ill patients, possibly mediated or regulated by sex hormones [28]. Thus, differences in the hormonal status of critically ill patients may partly explain the gender-related differences in the rate of disease progression and response to treatment in ICU patients. In our study, we found that the duration of MV, ICU LOS and hospital LOS were significantly longer for men than for women both in the overall study population and in the different age subgroups. These results imply that women may be more capable of recovering from critical illness or surgery than men.
In an international multicentre prospective study, Esteban et al. [7] reported that the main conditions independently associated with increased mortality in mechanically ventilated ICU patients not only included the factors present at the start of MV but also factors related to patient management and factors that developed during MV. Esteban et al. [9] also found that factors associated with the highest risk of mortality in patients older than 70 years were the development of complications during the course of mechanical ventilation, such as acute renal failure and shock. In our study, we also found that in the overall study population, the source of ICU admission, APACHE II scores, hospital LOS, events occurring over the course of MV, and the withholding or withdrawing of life-sustaining treatments were also independently associated with hospital mortality. Therefore, three types of variables, including the baseline characteristics of the patients at the beginning of MV, factors related to patient management, and events that occurred during MV, may also have accounted for the differences in the outcomes of mechanically ventilated ICU patients based on age and gender. For example, differences in the process of care or gender-based treatment bias may explain gender-based differences in the outcomes of mechanically ventilated ICU patients [10, 13].
To the best of our knowledge, this is the first multicentre retrospective study in China providing data that indicate gender- and age-related differences in clinical outcomes among mechanically ventilated ICU patients. However, we are also aware of several limitations of our study. First, this study was a retrospective study, and the data were obtained from 2012 to 2013, which may impose temporal limitations on the applicability of this dataset. Second, the 14 ICUs included in our study population were all in Beijing, and these ICUs may not be representative of a random sample of Chinese ICUs. Thus, our research results may not be applicable to other regions or countries. Third, our study did not include other important variables, including nutritional status, the degree of organ dysfunction, and other invasive procedures, which may also account for gender differences in outcomes. Finally, our study only collected the ventilator parameters at the beginning of mechanical ventilation, such as initial tidal volumes, PEEP, etc., but did not record the changes in ventilator parameters over the course of mechanical ventilation. As a result, we were unable to investigate the effects of ventilator modes and settings on clinical outcomes in mechanically ventilated women and men. Therefore, it is necessary to conduct more prospective studies specifically designed to address age and gender differences in outcomes of mechanically ventilated ICU patients.
Conclusion
In this study, we demonstrated the existence of gender- and age-related differences in clinical outcomes among mechanically ventilated ICU patients. The combination of male gender and advanced age is strongly associated with hospital mortality. Our findings merit consideration when designing future clinical trials involving mechanically ventilated patients.
Availability of data and materials
The datasets used and/or analysed in the current study are available from the corresponding author on reasonable request.
Abbreviations
- MV:
-
Mechanical ventilation
- ICU:
-
Intensive care unit
- NMB:
-
Neuromuscular blocker
- LOS:
-
Length of stay
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- ARDS:
-
Acute respiratory distress syndrome
- PBW:
-
Predicted body weight
- BMI:
-
Body mass index
- NIMV:
-
Noninvasive mechanical ventilation
- COPD:
-
Chronic obstructive pulmonary disease
- Pao2 :
-
Partial pressure of oxygen in arterial blood
- FIo2 :
-
Fraction of inspired oxygen
- Paco2 :
-
Partial pressure of carbon dioxide in arterial blood
- Spo2 :
-
Pulse oxygen saturation
- VCV:
-
Volume-controlled ventilation
- PCV:
-
Pressure-controlled ventilation
- PSV:
-
Pressure support ventilation
- SIMV:
-
Synchronized intermittent mandatory ventilation
- PEEP:
-
Positive end-expiratory pressure
- VAP:
-
Ventilator-associated pneumonia
- PMV:
-
Prolonged mechanical ventilation
- CNY:
-
Chinese Yuan
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
References
Du B, An Y, Kang Y, Yu X, Zhao M, Ma X, et al. Characteristics of critically ill patients in ICUs in mainland China. Crit Care Med. 2013;41(1):84–92.
Metnitz PG, Metnitz B, Moreno RP, Bauer P, Del Sorbo L, Hoermann C, et al. Epidemiology of mechanical ventilation: analysis of the SAPS 3 database. Intensive Care Med. 2009;35(5):816–25.
Fowler RA, Sabur N, Li P, Juurlink DN, Pinto R, Hladunewich MA, et al. Sex-and age-based differences in the delivery and outcomes of critical care. CMAJ. 2007;177(12):1513–9.
Sacanella E, Pérez-Castejón JM, Nicolás JM, Masanés F, Navarro M, Castro P, et al. Mortality in healthy elderly patients after ICU admission. Intensive Care Med. 2009;35(3):550–5.
Farfel JM, Franca SA, Sitta Mdo C, Filho WJ, Carvalho CR. Age, invasive ventilatory support and outcomes in elderly patients admitted to intensive care units. Age Ageing. 2009;38(5):515–20.
Needham DM, Bronskill SE, Calinawan JR, Sibbald WJ, Pronovost PJ, Laupacis A. Projected incidence of mechanical ventilation in Ontario to 2026: preparing for the aging baby boomers. Crit Care Med. 2005;33(3):574–9.
Esteban A, Anzueto A, Frutos F, Alía I, Brochard L, Stewart TE, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002;287(3):345–55.
Ye Y, Zhu B, Jiang L, Jiang Q, Wang M, Hua L, et al. A contemporary assessment of acute mechanical ventilation in Beijing: description, costs, and outcomes. Crit Care Med. 2017;45(7):1160–7.
Esteban A, Anzueto A, Frutos-Vivar F, Alía I, Ely EW, Brochard L, et al. Outcome of older patients receiving mechanical ventilation. Intensive Care Med. 2004;30(4):639–46.
Epstein SK, Vuong V. Lack of influence of gender on outcomes of mechanically ventilated medical ICU patients. Chest. 1999;116(3):732–9.
Esteban A, Anzueto A, Alía I, Gordo F, Apezteguía C, Pálizas F, et al. How is mechanical ventilation employed in the intensive care unit? An international utilization review. Am J Respir Crit Care Med. 2000;161(5):1450–8.
Xu Y, Lai C, Xu G, Meng W, Zhang J, Hou H, et al. Risk factors of ventilator-associated pneumonia in elderly patients receiving mechanical ventilation. Clin Interv Aging. 2019;14:1027–38.
Kollef MH, O'Brien JD, Silver P. The impact of gender on outcome from mechanical ventilation. Chest. 1997;111(2):434–41.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–29.
Network ARDS, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301–8.
National Bureau of Statistics of China. The 2010 population census of the People’s Republic of China. http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm (in Chinese). Accessed April 10, 2020.
Valentin A, Jordan B, Lang T, Hiesmayr M, Metnitz PG. Gender-related differences in intensive care: a multiple-center cohort study of therapeutic interventions and outcome in critically ill patients. Crit Care Med. 2003;31(7):1901–7.
Sharma RK, Prigerson HG, Penedo FJ, Maciejewski PK. Male-female patient differences in the association between end-of-life discussions and receipt of intensive care near death. Cancer. 2015;121(16):2814–20.
Mahmood K, Eldeirawi K, Wahidi MM. Association of gender with outcomes in critically ill patients. Crit Care. 2012;16(3):R92.
Shen HN, Lu CL, Yang HH. Women receive more trials of noninvasive ventilation for acute respiratory failure than men: a nationwide population-based study. Crit Care. 2011;15(4):R174.
Bookwala J, Coppola KM, Fagerlin A, Ditto PH, Danks JH, Smucker WD. Gender differences in older adults' preferences for life-sustaining medical treatments and end-of-life values. Death Stud. 2001;25(2):127–49.
Nakamura K, Kinugasa Y, Sugihara S, Hirai M, Yanagihara K, Haruki N, et al. Sex differences in surrogate decision-maker preferences for life-sustaining treatments of Japanese patients with heart failure. ESC Heart Fail. 2018;5(6):1165–72.
Sagy I, Fuchs L, Mizrakli Y, Codish S, Politi L, Fink L, et al. The association between the patient and the physician genders and the likelihood of intensive care unit admission in hospital with restricted ICU bed capacity. QJM. 2018;111(5):287–94.
Reinikainen M, Niskanen M, Uusaro A, Ruokonen E. Impact of gender on treatment and outcome of ICU patients. Acta Anaesthesiol Scand. 2005;49(7):984–90.
Yu HP, Chaudry IH. The role of estrogen and receptor agonists in maintaining organ function after trauma-hemorrhage. Shock. 2009;31(3):227–37.
Angele MK, Schwacha MG, Ayala A, Chaudry IH. Effect of gender and sex hormones on immune responses following shock. Shock. 2000;14(2):81–90.
Angele MK, Pratschke S, Chaudry IH. Does gender influence outcomes in critically ill patients? Crit Care. 2012;16(3):129.
Papathanassoglou ED, Middleton N, Hegadoren K. Sex-dependent disparities in critical illness: methodological implications for critical care research. Nurs Crit Care. 2015;20(2):58–62.
Mathieu C, Leone M. Gender and sepsis: first step of personalized medicine? Minerva Anestesiol. 2018;84(4):434–6.
Acknowledgements
The authors are indebted to the study coordinators and the physicians who participated in the collection of data for this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
JM contributed to the study conception and design, data and statistical analysis, and manuscript preparation. BZ, LJ, and QJ contributed to the study design, data analysis, and manuscript revision. XX contributed to the study’s conception and design, data and statistical analysis, manuscript revision and supervision of the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective study was approved by the Institutional Review Board of Fu Xing Hospital, Capital Medical University (Approval number: 2019FXHEC-KY167) and a waiver of informed consent was granted.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Comparison of the duration of mechanical ventilation (hours) between mechanically ventilated women and men, based on stratification of indication for mechanical ventilation and age.
Additional file 2: Table S2.
Comparison of ICU mortality between mechanically ventilated women and men, based on stratification of indication for mechanical ventilation and age.
Additional file 3: Table S3.
Comparison of hospital mortality between mechanically ventilated women and men, based on stratification of indication for mechanical ventilation and age.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ma, JG., Zhu, B., Jiang, L. et al. Gender- and age-based differences in outcomes of mechanically ventilated ICU patients: a Chinese multicentre retrospective study. BMC Anesthesiol 22, 18 (2022). https://doi.org/10.1186/s12871-021-01555-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-021-01555-8