Abstract
Introduction
Previous studies in western countries have observed that women are less likely than men to receive intensive care and mechanical ventilation (MV). We aimed to investigate whether the gender difference also exists in Asian populations and in the provision of different types of MV including invasive (INV) and noninvasive ventilation (NIV).
Methods
We analyzed all adult hospital patients between 2005 and 2007 in the claims data from 1,000,000 randomly selected people in the Taiwan National Health Insurance Research Database. NIV-only was defined as patients receiving NIV as the only ventilator treatment during hospitalization. Gender difference was assessed using multivariable analyses with/without considering a hospital cluster effect by generalized estimating equations models. Subgroup analyses for gender difference in NIV use were performed using propensity score matching method.
Results
Of the 128,327 patients enrolled, 53.8% were men, 9.2% received intensive care and 5.2% used MV. After adjusting for potential confounders, women were less likely than men to receive intensive care (adjusted odds ratio [aOR] 0.77, 95% confidence interval [CI] 0.73-0.82) and MV (aOR 0.84, 95% CI 0.78-0.91). Among MV patients, 6.8% received NIV-only; the proportion of which was higher in women than in men (8.6% vs. 5.7%, P < 0.001). After controlling for confounders and a cluster effect, women remained more likely to receive NIV-only (aOR 1.61, 95% CI 1.32-1.96). Subgroup analyses showed that patients with underlying congestive heart failure (CHF) had the highest difference in the provision of NIV-only (female-to-male aOR 2.76, 95% CI 1.38-5.53). A hospital cluster effect on the gender difference in NIV use was found in patients with diseases other than chronic obstructive pulmonary disease and CHF.
Conclusions
Gender differences existed not only in the provision but also in the types of MV. Further studies are needed to understand why gender differences occur.
Similar content being viewed by others
Introduction
Studies in western countries have shown that gender differences exist in the process of care for critically ill patients [1–3]. For example, women are found to be less likely than men to receive intensive care [1, 2] and invasive treatments including mechanical ventilation (MV) [1–3]. The suboptimal care might contribute to an observed excess mortality in women [2]. Whether these differences exist in Asian populations remains unknown. Besides, the influence of gender on the provision of different types of MV, that is, invasive ventilation (INV) and noninvasive ventilation (NIV), has not been investigated.
NIV provides ventilator support via a nose/face mask without using an invasive artificial airway for patients with acute respiratory failure (ARF). The use of NIV has been shown to reduce intubation and mortality in ARF patients with acute pulmonary edema and underlying chronic obstructive pulmonary disease (COPD) [4–7]. In diseases other than COPD and acute pulmonary edema, NIV is also increasingly used with variable success rates [8–12]. The utilization rates of NIV in patients with ARF range from 16% to 24% in developed countries [12–14]. But these data are underestimated because NIV is increasingly initiated outside the ICU setting [14, 15].
Women may be more likely to receive NIV if they are less likely than men to receive invasive treatments such as INV [1–3]. In addition, a higher perception of breathlessness in women [16, 17] may increase the chance of receiving an NIV trial for "shortness of breath" because strict criteria are usually lacking in clinical practices [9]. In Taiwan, the National Health Insurance Research Database (NHIRD) covers nearly all (99%) claims for its population of more than 22 million. It has been used extensively in various studies [18–20] and can provide real world experiences of NIV use both outside and inside the ICU. Therefore, we conducted this study, based on the NHIRD, to analyze the nationwide utilization of NIV in Taiwan and to assess whether gender differences exist not only in the provision of intensive care and MV but also in the provision of different types of MV for patients with ARF. We hypothesized that women are less likely than men to receive intensive care and MV during hospitalization but receive more trials of NIV for ARF and that the gender difference in NIV use varies among subgroups of patients with underlying COPD, congestive heart failure (CHF) and other diseases.
Materials and methods
Database
In Taiwan, a compulsory and universal National Health Insurance (NHI) program was initiated by the government in 1995 [18]. With the exception of prison inmates, all citizens are enrolled in the program. Patients were drawn from the NHIRD, released for research purposes by the National Health Research Institute, Taipei, Taiwan. The NHIRD provided encrypted patient identification numbers, sex, birthday, dates of admission and discharge, medical institutions providing the services, the ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) codes of diagnoses (up to five) and procedures (up to five), outcome at hospital discharge (recovered, died or transferred out), order codes, and the fees charged to patients.
Study sample
The study cohort was drawn from a subset of the NHIRD, the Longitudinal Health Insurance Database of 2005 (LHID-2005) [18]. One million beneficiaries, representing about 5% of the Taiwanese population enrolled in 2005, were selected using a simple random sampling method from the NHIRD and included in the LHID-2005 that contained all linked claims data of the cohort from 2005 to 2007. There were no significant differences in age and sex between the study cohort and the general population [18]. The study period spanned from 1 January, 2005 to 31 December, 2007. All adult (≥ 18 years old) patients were identified by linking through the hospitalization claims data. Patients were excluded if they were hospitalized for mental disorders (ICD-9-CM codes 290-319) or had diagnoses related to complications of pregnancy, childbirth or the puerperium (ICD-9-CM codes 630-679); the reasons for exclusion were reduced likeliness of receiving non-psychiatric acute medical treatment for the former and a lack of relevant male-related codes for the latter. Patients were also excluded if they were ventilator dependent in the respiratory wards or received negative pressure or high frequency oscillatory ventilation due to their chronic respiratory failure and/or receipt of uncommon mode of ventilation. To ensure the independence of observations, only the first-episode admissions were included in the analyses. Human Subjects Institutional Review Board Approval and informed consent were not needed because the study used an encrypted administrative database.
Definition
Patients who received MV during acute care hospitalizations were designated as ARF [21]. INV-only was used to define those receiving INV as the only ventilator treatment and NIV-only was for those receiving only NIV during the same hospitalization. Because we could not verify the sequence, NIV/INV described those who received both NIV and INV during the same hospitalization. NIV was delivered using continuous positive airway pressure and/or bilevel positive airway pressure ventilation. The specific indications for MV or use of NIV could not be determined because the database did not provide such information. As claims reimbursement for use of MV was based on a per day basis, not per hour use, and only one claim can be filed for those receiving both INV and NIV on the same day, only the claim for the higher-cost INV was made. For example, if one ARF patient received NIV on day one but, due to NIV failure, required INV from day two to five, and then when the patient was weaned from INV, received NIV again on day six for post-extubation respiratory distress, it would show "NIV for two days" (i.e., day one and six) and "INV for four days" (i.e., day two to five) on claims data. The use of NIV on day two would not be eligible for reimbursement.
Definitions of readmission, surgical conditions, and hospital mortality have been described previously [19].
Measurements
Baseline characteristics of study subjects were examined, including age, gender, medical/surgical conditions, hospital levels (medical centers with > 500 beds, regional hospitals with 250 to 500 beds, and district hospitals with 20 to 249 beds), prevalence of selected comorbid conditions (including COPD, CHF, cerebrovascular disease, and cancer), Charlson Comorbidity Index [22, 23], principal diagnoses, and occurrence of acute organ dysfunction (as a measure of disease severity) [19]. Outcome measures included use and types of MV (including INV-only, NIV-only, and NIV/INV), ICU admission, duration of MV, length of stays, and hospital mortality [19]. COPD was defined as ICD-9-CM codes 490 to 496 (excluding 493 for asthma). Definitions of CHF, cerebrovascular disease, and cancer were based on the Charlson Comorbidity Index [22, 23], which is a weighted summary measure of clinically important concomitant diseases that has been adapted for use with ICD-9-CM coded administrative databases.
Statistics
Continuous variables were described as median (interquartile range (IQR)) and compared by the Mann-Whitney U test; discrete ones were expressed as counts or percentages and analyzed by the chi-square test. To examine the effects of gender on various outcomes, we conducted multivariable logistic regression analyses adjusting for the baseline covariates, including age, surgical and selected comorbid conditions, Charlson Comorbidity Index, hospital levels, principal diagnoses and number of acute organ dysfunction. Additional covariates such as status of MV or intensive care were included as appropriate. Specifically, MV was included as an additional covariate when modeling the gender effect on the provision of intensive care and on hospital mortality of patients requiring intensive care. Conversely, intensive care status was included as an additional covariate when modeling the gender effect on the provision of MV for all patients and that of different types of MV for ARF patients as well as on hospital mortality of ARF patients. Resource uses (including duration of MV and length of stays) were compared using multivariable linear regression models adjusting for the baseline covariates, with the inclusion of MV and intensive care status as additional covariates when appropriate. Tolerance level was calculated to assess multicollinearity, which was defined as existing when the level was less than 0.1.
To further explore the effect of gender on the provision of different types of MV, we also applied the propensity score method [24–26] for ARF patients and for subgroups with underlying COPD, CHF, and others. Patients with COPD or CHF were selected because they were associated with increased use of NIV [4, 5]. The propensity score method has been used to reduce bias and increase precision of estimates in observational research [24–26]. The propensity score, that is the probability of being a female patient, was estimated by a logistic regression model conditional on the baseline covariates and intensive care status. For all ARF patients and subgroups, men and women were matched one-to-one by the propensity score using the greedy-matching algorithm [26] and then analyzed in the logistic regression models to estimate the gender effect on the provision of NIV. Because hospitals tended to behave differently and outcomes of patients within the same hospitals were correlated, a hospital cluster effect might be present [27]. Therefore, the gender effect on the provision of NIV was reanalyzed using logistic Generalized Estimating Equations (GEE) models [27], specifying an exchangeable structure of a working correlation matrix to regress the correlated binary outcomes. The performance of the propensity score model was assessed by examining whether the baseline covariates of men and women were balanced after matching. Data analysis was performed using SPSS for Windows, version 17.0. (SPSS Inc., Chicago, IL, USA) and SAS software, version 9.1 (SAS Institute, Inc., Cary, NC, USA). Statistical significance was set at P < 0.05 (two-tailed).
Results
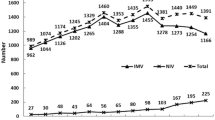
During the three-year study period, we identified 128,327 patients. Of them, 53.8% were men, 9.2% had an ICU stay and 5.2% received MV (Figure 1). Characteristics of the study population are shown in Table 1. Women were less likely than men to receive intensive care (P < 0.001) and MV (P < 0.001). The differences were consistent across all age groups except those aged 85 years or older (Figures 2a and 2b). After adjusting for potential confounders (i.e., baseline and additional covariates as described in the Methods section), women remained less likely than men to receive intensive care (adjusted odds ratio (aOR) 0.77, 95% confidence interval (CI) 0.73-0.82) and MV (aOR 0.84, 95% CI 0.78-0.91).
Age-and-gender-specific proportional distributions of patients receiving (a) intensive care, (b) mechanical ventilation (MV), (c) noninvasive and invasive ventilation (NIV/INV) and (d) NIV-only. Note: NIV-only was used to define those receiving NIV as the only ventilator treatment and NIV/INV was for those receiving both NIV and INV during the same hospitalization. ARF, acute respiratory failure.
Distributions of different types of MV in ARF patients are shown in Table 2. The age-and-gender-specific distribution of ARF patients receiving NIV is shown in Figures 2c and 2d. Among ARF patients, 6.8% received NIV-only, of which a higher proportion was in women than in men (Table 2).
Characteristics, resource use, and outcomes of ARF patients stratified by gender and intensive care status are shown in Table 3. Among ARF patients, women were older than men inside or outside the ICU, and women being cared for inside the ICU had fewer surgical conditions. The distribution patterns of selected comorbid conditions were different in ICU patients of both genders but similar in those being cared for outside the ICU. But the distribution of principal diagnoses, number of organ dysfunction, and hospital-level patterns were comparable in both genders. Outcomes including the proportion of ICU admission (88.9% vs. 88.7%, P = 0.858), duration of MV, length of stays, and hospital mortality were similar between men and women. Among ARF patients receiving NIV (including NIV-only and NIV/INV), duration of NIV was significantly longer in women than in men (median three days, IQR one to five days vs. two days, IQR one to four days, respectively: crude and adjusted P = 0.025 and 0.043, respectively). The differences became insignificant when durations of NIV in patients receiving NIV-only and NIV/INV were calculated separately.
Among ARF patients, women were 63% more likely than men to receive NIV-only after controlling for all potential confounders (Table 4). These differences changed little after using logistic GEE models, suggesting a low cluster effect. The results based on analyses of the propensity score matched pairs were similar (Table 4). The baseline characteristics of men and women were balanced after matching (Table 5). In subgroup analyses, the gender difference in the use of NIV-only was the highest for ARF patients with CHF, followed by those without COPD or CHF, but was insignificant for those with COPD (Table 4). The cluster effect on the use of NIV-only was unremarkable except in ARF patients without COPD or CHF because the gender difference became insignificant after using a logistic GEE model.
Discussion
In this study, we found that women were more likely than men to receive NIV-only for ARF, especially those with underlying CHF or diseases other than COPD. We also confirmed the reports from western countries that women were less likely than men to receive intensive care and MV [1–3]. Despite these differences, hospital mortality in patients requiring MV or intensive care was similar between men and women.
The finding that women were more likely to receive NIV-only for ARF is consistent with prior reports [1–3]. Studies in Austria, Canada, Brazil, and the USA have shown that women are less likely than men to receive invasive treatments [1–3]. These findings suggest that ethnic, cultural, and geographical factors do not seem to contribute to the gender difference in the delivery of NIV for ARF. However, the social context of gender differences may influence the decision for initiating life-supporting treatment [1, 2], which could possibly lead to a differential use of NIV. And there may be a mix of biological and clinical explanations for it. For example, a higher use of NIV in women may reflect their increased perception of breathlessness [16, 17] and a lack of strict criteria for NIV use in clinical practices [9]. Therefore, women may receive NIV earlier, for longer, and perhaps more frequently because they may report more symptoms of dyspnea even under similar respiratory conditions [16, 17]. Finally, the results of this study might also imply that women could be more likely to succeed in NIV treatment than men because the NIV-only group was mostly made of patients with NIV success (plus do-not-resuscitate patients who failed NIV without being intubated) and the NIV/INV group was mostly those with NIV failure (plus those who received a post-extubation NIV). Nevertheless, because gender is not shown to be associated with NIV failure [28], it might be more likely that a higher rate of NIV use in women simply reflects a gender bias in decision-making on NIV use instead of a higher rate of NIV success.
There are other reasons that might also explain some of the observed gender difference in NIV. First, misclassification between INV-only and NIV/INV was likely. In unselected patients with ARF receiving NIV, the reported intubation rates after a failed trial range from 10% to 60%; among them, 60% to 100% occur within 24 hours [8–10, 13, 29–33]. Therefore, the utilization rate of NIV in this study is likely to be underestimated. Because of the limitation in the Taiwan's NHI reimbursement policy (see methods section), the NHIRD tended to capture claims of patients receiving longer-duration NIV and misclassify those using INV-only and NIV/INV (i.e., to overestimate INV-only and underestimate NIV/INV). Since duration of NIV did not differ significantly between men and women receiving NIV/INV, misclassification would be similar for both genders and hence less likely to cause the observed difference. Besides, this bias cannot explain the difference observed in the provision of NIV-only. Second, some potential confounders could not be controlled in this study. For example, differential sex distributions have been reported in many aspects including the severity of acute illnesses [1], the occurrence of post-extubation stridor [34], the preference of advance directives (such as do-not-resuscitate or do-not-intubate orders) [35] and the population prevalence and incidence of some acute illnesses [36, 37] or chronic comorbidities [38, 39]; all of which have been shown to influence the outcome of, and hence the decision-making for, an NIV trial [28, 39]. For this reason, we did a sub-analysis in propensity-score-matched pairs with underlying CHF and found that women were still more than twice as likely as men to receive NIV-only. And finally, a hospital cluster effect may also explain some of the observed difference in subgroups such as ARF patients with diseases other than COPD or CHF.
The reasons that the gender difference in the provision of NIV was not found in patients with COPD are unclear. As COPD is the most well-established disease benefited from NIV [4, 5], the gender difference may be less likely to occur. However, because women are at risk of under-diagnosis, and hence being under-coded, of COPD [40], the results could be either over- or under-estimated. For example, failure to code for COPD would hinder the adjustment for women and thereby bias the observed association between women and NIV away from the null. On the other hand, failure to diagnose COPD could theoretically result in under-utilization of NIV in women. This may also explain the null finding in ARF patients with COPD.
Our study provides the first nationwide population-based data on the utilization rate of NIV (including NIV-only and NIV/INV) both outside and inside the ICU in Taiwan. The utilization rate was slightly lower than that in developed countries (15.4% vs. 16% to 24%, respectively) [12–14, 29, 41]. The reported rates in developed countries are also likely to be under-estimated by including only ICU patients [12–14, 30, 41]; and the under-estimation may become more significant over time due to increased successful use of NIV outside the ICU [14, 42, 43]. For example, in a regional survey of 82 acute care hospitals in the USA, 20% of ARF patients received NIV, of which 45% of the treatment was initiated outside the ICU [42]. In this study, 27.7% of patients receiving NIV were cared for only outside the ICU.
The effect of gender on the outcome of patients requiring intensive care or MV remains debatable [1, 2, 31, 44–46]. Although a higher risk of death in women requiring intensive care or MV has been found in some studies [2, 44, 45], it is not confirmed by others [1, 31, 46]. Our study did not find the gender effect on the outcomes of these patients despite the observed difference in the process of care. This finding is consistent with a prior report [1] showing that a more invasive therapeutic approach in men does not translate to a better outcome.
The finding of a hospital cluster effect on the gender difference in NIV use may provide policy implications for best practice provision across hospitals. The cluster effect implies that clinicians are not using standard criteria to start NIV based on evidence from guidelines [5, 12]. Non-adherence to guidelines is also present in situations eligible for NIV, leading to its underuse [12, 47]. For example, one retrospective study showed that nearly two thirds of ICU patients with exacerbation of COPD or CHF did not receive an NIV trial despite meeting eligibility criteria [47]. However, because the indication for NIV could not be determined in this study, we do not know whether the use of NIV for ARF is appropriate to the guidelines.
Several other limitations deserve comments. First, the administrative databases are subject to possible under-coding and over-coding errors. The definitions of diagnoses relied solely on diagnostic codes, but the accuracy of which could not be verified. Second, information on primary causes of ARF, indications/mode/settings and effectiveness of NIV use, and types of ventilators was not available. Third, hospital mortality might be under-estimated for the inability to verify through linkage to death certificate. And finally, since only five diagnostic codes were available, some related diagnoses could have been missed. But these biases are toward the null. Nevertheless, our study is strengthened by the large number of patients retrieved from a nationwide population-based dataset, which can provide an unbiased selection and enhance its generalizability.
Conclusions
This study suggests that gender difference not only existed in the provision of intensive care and MV, but also in the use of NIV in Taiwan. The subgroup analyses indicate that the gender differences in NIV use were heterogeneous and related to the underlying diseases. Further research is needed to explore why gender differences exist, especially whether and how gender-biased decision-making affects the use of NIV.
Key messages
-
Studies in western countries have shown that gender differences exist in the process of care for critically ill patients.
-
Our findings confirm the reports from western countries that women were less likely than men to receive intensive care and mechanical ventilation.
-
Moreover, we found that women were more likely than men to receive NIV-only for acute respiratory failure, especially those with underlying heart failure.
-
The finding of a higher NIV use in women may reflect a higher perception for dyspnea and their lower tendency to receive invasive treatments than men as well as a lack of strict criteria for NIV use in clinical practices.
-
Further research is needed to understand why the gender difference occurs, especially whether and how gender-biased decision-making affects the use of NIV.
Abbreviations
- aOR:
-
adjusted odds ratio
- ARF:
-
acute respiratory failure
- CHF:
-
congestive heart failure
- CI:
-
confidence interval
- COPD:
-
chronic obstructive pulmonary disease
- GEE:
-
generalized estimating equations
- ICD-9-CM International Classification of Diseases:
-
: Ninth Revision: Clinical Modification
- INV:
-
invasive ventilation
- IQR:
-
interquartile range
- LHID:
-
Longitudinal Health Insurance Database
- MV:
-
mechanical ventilation
- NHIRD:
-
National Health Insurance Research Database
- NIV:
-
noninvasive ventilation.
References
Valentin A, Jordan B, Lang T, Hiesmayr M, Metnitz PG: Gender-related differences in intensive care: a multiple-center cohort study of therapeutic interventions and outcome in critically ill patients. Crit Care Med 2003, 31: 1901-1907. 10.1097/01.CCM.0000069347.78151.50
Fowler RA, Sabur N, Li P, Juurlink DN, Pinto R, Hladunewich MA, Adhikari NK, Sibbald WJ, Martin CM: Sex-and age-based differences in the delivery and outcomes of critical care. CMAJ 2007, 177: 1513-1519. 10.1503/cmaj.071112
Pietropaoli AP, Glance LG, Oakes D, Fisher SG: Gender differences in mortality in patients with severe sepsis or septic shock. Gend Med 2010, 7: 422-437. 10.1016/j.genm.2010.09.005
Brochard L, Mancebo J, Wysocki M, Lofaso F, Conti G, Rauss A, Simonneau G, Benito S, Gasparetto A, Lemaire F, Isabey D, Harf A: Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med 1995, 333: 817-822. 10.1056/NEJM199509283331301
International Consensus Conferences in Intensive Care Medicine: noninvasive positive pressure ventilation in acute respiratory failure Am J Respir Crit Care Med 2001, 163: 283-291.
Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, Fukuchi Y, Jenkins C, Rodriguez-Roisin R, van Weel C, Zielinski J, Global Initiative for Chronic Obstructive Lung Disease: Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2007, 176: 532-555. 10.1164/rccm.200703-456SO
Masip J, Roque M, Sánchez B, Fernández R, Subirana M, Expósito JA: Noninvasive ventilation in acute cardiogenic pulmonary edema: systematic review and meta-analysis. JAMA 2005, 294: 3124-3130. 10.1001/jama.294.24.3124
Sinuff T, Cook D, Randall J, Allen C: Noninvasive positive-pressure ventilation: a utilization review of use in a teaching hospital. CMAJ 2000, 163: 969-973.
Paus-Jenssen ES, Reid JK, Cockcroft DW, Laframboise K, Ward HA: The use of noninvasive ventilation in acute respiratory failure at a tertiary care center. Chest 2004, 126: 165-172. 10.1378/chest.126.1.165
Schettino G, Altobelli N, Kacmarek RM: Noninvasive positive-pressure ventilation in acute respiratory failure outside clinical trials: experience at the Massachusetts General Hospital. Crit Care Med 2008, 36: 441-447. 10.1097/01.CCM.0000300084.67277.90
Keenan SP, Mehta S: Noninvasive ventilation for patients presenting with acute respiratory failure: the randomized controlled trials. Respir Care 2009, 54: 116-126.
Chiumello D: Is noninvasive ventilation still underused by physicians? Respir Care 2009, 54: 1302-1303.
Esteban A, Ferguson ND, Meade MO, Frutos-Vivar F, Apezteguia C, Brochard L, Raymondos K, Nin N, Hurtado J, Tomicic V, González M, Elizalde J, Nightingale P, Abroug F, Pelosi P, Arabi Y, Moreno R, Jibaja M, D'Empaire G, Sandi F, Matamis D, Montañez AM, Anzueto A, VENTILA Group: Evolution of mechanical ventilation in response to clinical research. Am J Respir Crit Care Med 2008, 177: 170-177.
Frutos-Vivar F, Ferguson ND, Esteban A: Mechanical ventilation: quo vadis? Intensive Care Med 2009, 35: 775-778. 10.1007/s00134-009-1450-3
Carlucci A, Delmastro M, Rubini F, Fracchia C, Nava S: Changes in the practice of non-invasive ventilation in treating COPD patients over 8 years. Intensive Care Med 2003, 29: 419-425.
de Torres JP, Casanova C, Hernandez C, Abreu J, Aguirre-Jaime A, Celli BR: Gender and COPD in patients attending a pulmonary clinic. Chest 2005, 128: 2012-2016. 10.1378/chest.128.4.2012
Ofir D, Laveneziana P, Webb KA, Lam YM, O'Donnell DE: Sex differences in the perceived intensity of breathlessness during exercise with advancing age. J Appl Physiol 2008, 104: 1583-1593. 10.1152/japplphysiol.00079.2008
National Health Insurance Research Database[http://w3.nhri.org.tw/nhird//en/index.htm]
Shen HN, Lu CL, Yang HH: Epidemiologic trend of severe sepsis in Taiwan from 1997 through 2006. Chest 2010, 138: 298-304. 10.1378/chest.09-2205
Shen HN, Lu CL: Skin and soft tissue infections in hospitalized and critically ill patients: a nationwide population-based study. BMC Infect Dis 2010, 10: 151. 10.1186/1471-2334-10-151
Mayr FB, Yende S, Linde-Zwirble WT, Peck-Palmer OM, Barnato AE, Weissfeld LA, Angus DC: Infection rate and acute organ dysfunction risk as explanations for racial differences in severe sepsis. JAMA 2010, 303: 2495-2503. 10.1001/jama.2010.851
Charlson ME, Pompei P, Ales KL, MacKenzie CR: A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987, 40: 373-383. 10.1016/0021-9681(87)90171-8
Deyo RA, Cherkin DC, Ciol MA: Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992, 45: 613-619. 10.1016/0895-4356(92)90133-8
Rosenbaum PR, Rubin DB: The central role of the propensity score in observational studies for causal effects. Biometrika 1983, 70: 41-55. 10.1093/biomet/70.1.41
D'Agostino RB Jr: Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 1998, 17: 2265-2281. 10.1002/(SICI)1097-0258(19981015)17:19<2265::AID-SIM918>3.0.CO;2-B
Guru V, Fremes SE, Austin PC, Blackstone EH, Tu JV: Gender differences in outcomes after hospital discharge from coronary artery bypass grafting. Circulation 2006, 113: 507-516. 10.1161/CIRCULATIONAHA.105.576652
Hanley JA, Negassa A, Edwardes MD, Forrester JE: Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol 2003, 157: 364-375. 10.1093/aje/kwf215
Phua J, Kong K, Lee KH, Shen L, Lim TK: Noninvasive ventilation in hypercapnic acute respiratory failure due to chronic obstructive pulmonary disease vs. other conditions: effectiveness and predictors of failure. Intensive Care Med 2005, 31: 533-539. 10.1007/s00134-005-2582-8
Martin TJ, Hovis JD, Costantino JP, Bierman MI, Donahoe MP, Rogers RM, Kreit JW, Sciurba FC, Stiller RA, Sanders MH: A randomized, prospective evaluation of noninvasive ventilation for acute respiratory failure. Am J Respir Crit Care Med 2000, 161: 807-813.
Carlucci A, Richard JC, Wysocki M, Lepage E, Brochard L, SRLF Collaborative Group on Mechanical Ventilation: Noninvasive versus conventional mechanical ventilation. An epidemiologic survey. Am J Respir Crit Care Med 2001, 163: 874-880.
Esteban A, Anzueto A, Frutos F, Alía I, Brochard L, Stewart TE, Benito S, Epstein SK, Apezteguía C, Nightingale P, Arroliga AC, Tobin MJ, Mechanical Ventilation International Study Group: Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA 2002, 287: 345-355. 10.1001/jama.287.3.345
Honrubia T, Garcia Lopez FJ, Franco N, Mas M, Guevara M, Daguerre M, Alía I, Algora A, Galdos P: Noninvasive vs conventional mechanical ventilation in acute respiratory failure: a multicenter, randomized controlled trial. Chest 2005, 128: 3916-3924. 10.1378/chest.128.6.3916
Linko R, Okkonen M, Pettilä V, Perttilä J, Parviainen I, Ruokonen E, Tenhunen J, Ala-Kokko T, Varpula T, FINNALI-study group: Acute respiratory failure in intensive care units. FINNALI: a prospective cohort study. Intensive Care Med 2009, 35: 1352-1361. 10.1007/s00134-009-1519-z
Francois B, Bellissant E, Gissot V, Desachy A, Normand S, Boulain T, Brenet O, Preux PM, Vignon P, Association des Réanimateurs du Centre-Ouest (ARCO): 12-h pretreatment with methylprednisolone versus placebo for prevention of postextubation laryngeal oedema: a randomised double-blind trial. Lancet 2007, 369: 1083-1089. 10.1016/S0140-6736(07)60526-1
Wenger NS, Pearson ML, Desmond KA, Harrison ER, Rubenstein LV, Rogers WH, Kahn KL: Epidemiology of do-not-resuscitate orders. Disparity by age, diagnosis, gender, race, and functional impairment. Arch Intern Med 1995, 155: 2056-2062. 10.1001/archinte.155.19.2056
Gutierrez F, Masia M, Mirete C, Soldán B, Rodríguez JC, Padilla S, Hernández I, Royo G, Martin-Hidalgo A: The influence of age and gender on the population-based incidence of community-acquired pneumonia caused by different microbial pathogens. J Infect 2006, 53: 166-174. 10.1016/j.jinf.2005.11.006
Lundblad D, Holmgren L, Jansson JH, Näslund U, Eliasson M: Gender differences in trends of acute myocardial infarction events: the Northern Sweden MONICA study 1985 - 2004. BMC Cardiovasc Disord 2008, 8: 17. 10.1186/1471-2261-8-17
Punjabi NM: The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc 2008, 5: 136-143. 10.1513/pats.200709-155MG
Shen HN, Cheng KC, Hou CC, Tan CK, Huang WT: Clinical features and short-term outcome of critically ill patients with head and neck cancer in the medical intensive care unit. Am J Clin Oncol 2009, 32: 467-471. 10.1097/COC.0b013e3181931236
Chapman KR, Tashkin DP, Pye DJ: Gender bias in the diagnosis of COPD. Chest 2001, 119: 1691-1695. 10.1378/chest.119.6.1691
Demoule A, Girou E, Richard JC, Taillé S, Brochard L: Increased use of noninvasive ventilation in French intensive care units. Intensive Care Med 2006, 32: 1747-1755. 10.1007/s00134-006-0229-z
Maheshwari V, Paioli D, Rothaar R, Hill NS: Utilization of noninvasive ventilation in acute care hospitals: a regional survey. Chest 2006, 129: 1226-1233. 10.1378/chest.129.5.1226
Hess DR, Pang JM, Camargo CA Jr: A survey of the use of noninvasive ventilation in academic emergency departments in the United States. Respir Care 2009, 54: 1306-1312.
Kollef MH, O'Brien JD, Silver P: The impact of gender on outcome from mechanical ventilation. Chest 1997, 111: 434-441. 10.1378/chest.111.2.434
Romo H, Amaral AC, Vincent JL: Effect of patient sex on intensive care unit survival. Arch Intern Med 2004, 164: 61-65. 10.1001/archinte.164.1.61
Epstein SK, Vuong V: Lack of influence of gender on outcomes of mechanically ventilated medical ICU patients. Chest 1999, 116: 732-739. 10.1378/chest.116.3.732
Sweet DD, Naismith A, Keenan SP, Sinuff T, Dodek PM: Missed opportunities for noninvasive positive pressure ventilation: a utilization review. J Crit Care 2008, 23: 111-117. 10.1016/j.jcrc.2007.04.002
Acknowledgements
The study was performed in Chi Mei Medical Center and supported by grant CMFHR9855 from the hospital. The study was based in part on data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health and managed by National Health Research Institutes. The interpretation and conclusions contained herein do not represent those of Bureau of National Health Insurance, Department of Health or National Health Research Institutes. The authors thank Professor Chung-Yi Li for his assistance during the revision of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
HNS designed the study, obtained funding, performed data mining and processing, did statistical analyses, drafted the initial manuscript, and revised important content. CLL contributed to the study design, data mining and processing, analyses and interpretation of results, and revision for important content. HHY participated in the interpretation of results and revision for important content. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Shen, HN., Lu, CL. & Yang, HH. Women receive more trials of noninvasive ventilation for acute respiratory failure than men: a nationwide population-based study. Crit Care 15, R174 (2011). https://doi.org/10.1186/cc10323
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc10323