Abstract
Background
COVID-19 is a disease that caused a contagious respiratory ailment that killed and infected hundreds of millions. It is necessary to develop a computer-based tool that is fast, precise, and inexpensive to detect COVID-19 efficiently. Recent studies revealed that machine learning and deep learning models accurately detect COVID-19 using chest X-ray (CXR) images. However, they exhibit notable limitations, such as a large amount of data to train, larger feature vector sizes, enormous trainable parameters, expensive computational resources (GPUs), and longer run-time.
Results
In this study, we proposed a new approach to address some of the above-mentioned limitations. The proposed model involves the following steps: First, we use contrast limited adaptive histogram equalization (CLAHE) to enhance the contrast of CXR images. The resulting images are converted from CLAHE to YCrCb color space. We estimate reflectance from chrominance using the Illumination–Reflectance model. Finally, we use a normalized local binary patterns histogram generated from reflectance (Cr) and YCb as the classification feature vector. Decision tree, Naive Bayes, support vector machine, K-nearest neighbor, and logistic regression were used as the classification algorithms. The performance evaluation on the test set indicates that the proposed approach is superior, with accuracy rates of 99.01%, 100%, and 98.46% across three different datasets, respectively. Naive Bayes, a probabilistic machine learning algorithm, emerged as the most resilient.
Conclusion
Our proposed method uses fewer handcrafted features, affordable computational resources, and less runtime than existing state-of-the-art approaches. Emerging nations where radiologists are in short supply can adopt this prototype. We made both coding materials and datasets accessible to the general public for further improvement. Check the manuscript’s availability of the data and materials under the declaration section for access.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
In 2019, the globe witnessed one of the most widespread outbreaks, the coronavirus (COVID-19). In January 2020, the World Health Organization (WHO) conceded COVID-19 as a public health emergency of international concern. WHO reported about 482.34 million infected cases with 6.15 million fatalities worldwide around March 2022 [1]. COVID-19 comes from SARS-CoV-2, one of the \(\beta\)-coronavirus family.It is one of the most transmissible, contagious, and infectious viruses among those implicated in Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS). Most infections occur by respiratory droplets, touching (nose, mouth, and eyes), or any other form of close contact [2].
Timely detection and diagnosis of the virus increase the prognostic probability of preventing its transmission. Thus, fewer infected cases and fatalities may occur. Nowadays, healthcare systems use reverse transcription-polymerase chain reaction (RT-PCR) [2]. RT-PCR yielded accurate results, associated with some limitations. Kameswari et al. [3] reported a limited sensitivity during the early stages of the disease. Purohit et al. [4] proved that the RT-PCR approach provides false-positive rates higher than expected. Another drawback of this method, it only recognizes viral RNA presence with the anticipation that a patient who recovered from COVID-19 may be detected as an infected one [5, 6].
To overcome RT-PCR limitations, researchers suggested deep learning, machine learning, and transfer learning models [7,8,9]. Nevertheless, deep learning and machine learning models [10, 11] exhibit notable limitations, such as the need for large datasets to train, expensive computational resources graphical processing unit (GPUs), more extensive trainable parameters, feature vector size, longer running, training, and testing time. Conversely, transfer learning models yielded negative transfer and overfitting concerns [12].
From the background of this work, it is within the scope to address the above limitations. We proposed a simple, coherent, and computationally efficient model to address some earlier drawbacks. The suggested method requires a smaller feature vector size, operates on a commodity CPU system, and exhibits less running time to detect COVID-19 chest X-ray (CXR) images and pneumonia diseases.
Our major contribution
-
In literature, high-performance deep learning methods are complex and require extensive data to train/test and run on expensive GPUs. However, we proposed a simple novel approach using CLAHE, YCrCb, and reflectance features, which runs on commodity hardware, and a low-cost CPU (see Table 7).
-
The proposed model demonstrates experimentally that CLAHE, YCrCb, and reflectance features improve previously studied handcrafted features. It uses basic handcrafted features and shows comparable performance results to state-of-the-art methods based on complex deep learning models (see Table 8).
-
Finally our model has a significant advantage in making real-time clinical decisions. It achieved high classification accuracy, detecting COVID-19 and Pneumonia, using less run time, and a smaller feature vector size of 25 (see Table 2).
The manuscript is structured in the following manner. Related works are given in “Related works” section. “Methods” section showcases the methods used. “Experimental results” and “Results” sections explain in detail the experimental results. Finally, comparative results and the conclusion are discussed in “Comparative results” and “Conclusion” sections.
Related works
Subramanian et al. [13] showed that transfer learning outperforms all proposed models. InceptionV3, DenseNet201, and Mobile-NetV2 attained better accuracy, while SqueezeNet and VGG19 reported high specificity. The study conducted by Purohit et al. [4] suggested a deep learning model using a multi-image augmentation technique. This work reported an accuracy of 98.97%. To facilitate COVID-19 detection, Bhattacharyya et al. [14] proposed a deep learning-based generative model (C-GAN). This reduces the complexity of images when computing discriminatory features. An accuracy of 96% was reported. The work proposed by Ismael et al. [15] adopted a deep feature extraction pre-trained on deep CNN models. They used SVM with a linear kernel function as their classifier. An accuracy score of 94.7% was obtained. A deep learning model to detect COVID-19 from CXR, CT scans, and ultrasound images was introduced by Horry et al. [16]. VGG19 model detected COVID-19, pneumonia, and normal images with an accuracy of 86%, 84%, and 100%, respectively. Alshayeji et al. [17] proposed a computer-aided diagnosis (CAD) technique to classify COVID-19 and normal lungs. Their method performed a three-class semantic segmentation of the lung CT image in infected regions. They presented a global accuracy of 99.47%, a mean accuracy of 94.04%, and a mean IoU (intersection over union) of 0.8968.
Shah et al. [18] proposed a hybrid deep learning method, combining a convolutional neural network (CNN) and gated recurrent unit (GRU) for detecting viral diseases in chest X-rays (CXRs).CNN extracted features and the GRU acted as a classifier. After training on 424 CXR images with 3 classes, the model achieved a precision, recall, and f1-score results of 0.96, 0.96, and 0.95, respectively. The work conducted by Bhyuyan et al. [19] proposed a full-resolution convolutional network (FrCN) to detect COVID-19 from CT scan images. Applying a fourfold cross-validation test, FrCN, with an accuracy of 99.9%, performed better than other state-of-the-art models. Khan et al. [20] proposed a novel SB-STM-BRNet CNN model, which incorporated squeezed and boosted (SB) and dilated convolutional-based split-transform-merge (STM) block to detect COVID-19. This model reported an accuracy of 98.21%. Khalifa et al. [11] developed a deep-learning semantic segmentation model for COVID-19 detection based on the encoder and decoder concepts. Their experimental results reported a global accuracy of 99.3% and a Weighted Intersection over Union (WIoU) of 98.7%. Khan et al. [21] proposed two novel deep learning frameworks: deep hybrid learning (DHL) and deep boosted hybrid learning (DBHL), using machine learning (ML) classifiers to detect COVID-19. The DBHL framework, merging the two-deep CNN features, reported an accuracy of 98.53%.
Mubarak et al. [9] proposed an integration of VGG-19 and a handcrafted LBP model to train KNN and SVM classifiers. An overall accuracy of 99.4% was reported. Adimoolam et al. [10] proposed a model which predicts and classifies diseases using chest X-ray images. Their model extracts textual and morphological features. Aggarwal et al. [2] proposed to use MobileNetV2, ResNet50, InceptionV3, NASNetMobile, VGG16, Xception, InceptionResNetV2, and DenseNet121. These transfer learning models were fine-tuned by adding a new set of layers to increase their performance. DensNet121 achieved an accuracy of 97% on the first dataset. Whereas, MobilNetV2 generated an overall accuracy of 81% on the second dataset. Zammit et al. [7] developed a generative model (shared variational auto-encoder) using a five-layer deep hierarchy of latent variables and deep convolutional mappings.
Machine learning models have emerged as powerful tools to diagnose and detect COVID-19 disease. The work by Kwekha-Rashid et al. [22] introduced a review study highlighting the importance of machine-learning algorithms in detecting COVID-19. Barstugan et al. [8] developed a classification model to detect COVID-19 from CT images using handcrafted features. They applied grey level co-occurrence, zone matrix (GLCM/GLZM), and local directional pattern (LDP) as feature extraction techniques. The work conducted by Kassania et al. [23] compared popular deep learning models. DensNet121 feature extractor with Bagging Tree classifier reported an overall accuracy of 99%. Kumar et al. [24] presented a machine-learning model based on deep features extracted using ResNet152. This approach achieved an accuracy of 97.3% using Random Forest and 97.7% using XGBoost. Mydukuri et al. [25] proposed a model based on LSRGNFM-LDC (least-square regressive Gaussian neuro-fuzzy multi-layered data classification) method. Their method uses a Deming least square regressive to extract features.
It is apparent from the literature review that most of the above models achieved good performances. Nevertheless, they used numerous integrated algorithms, larger feature vectors size, and many trainable parameters [2, 11, 16]. As a result, it engenders more running time and expensive computational resources (GPUs).
Methods
We propose a simple, coherent, and efficient computational technique to address the above drawbacks. We adopted CLAHE-YCrCb image processing technique [26, 27], the Illumination–Reflectance model [28], LBP [29], and machine learning classifiers [30]. First, Contrast Limited Adaptive Histogram Equalization is applied to enhance the contrast of the chest X-ray images. Second, we convert the output images from CLAHE into YCrCb color space. Third, we estimate reflectance from chrominance using the Illumination–Reflectance model. Finally, a normalized local binary patterns (LBP) histogram, generated from reflectance (Cr) and YCb, is used as the classification feature vector. DT, NB, SVM, KNN, and LR Machine learning algorithms are used to classify COVID-19, normal, and pneumonia CXR images. The overview of the proposed method is highlighted in Fig. 1.
Contrast limited adaptive histogram equalization (CLAHE)
CLAHE improves the appearance of an image and increases the performance of subsequent tasks, such as image segmentation, analysis, and object detection. Enhancing an image strengthens its quality and provides a better computational analysis. CLAHE performs better in image deblurring, noise removal, and contrast enhancement. It expands the gray level’s dynamic range [26, 31, 32]. This study adopted CLAHE to implement a local contrast image enhancement, enhancing image quality and enabling a better computational detection of COVID-19 from CXR images.
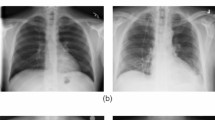
Figure 2 depicts the histogram equalizer (HE) and CLAHE enhancement on Normal, COVID-19, and pneumonia CXR images.
Converting CLAHE’s CXR images into YCrCb
YCrCb possesses a luminance Y and a chrominance CrCb. CrCb is red-difference and blue-difference from the chrominance constituents. Luminance, on the other hand, is an intensity constituent [28]. Equation 1 highlights the luminance. Equations 2 and 3 depict the chrominance Cb and Cr.
Several studies showed that chrominance is a suited component for detecting objects in medical images. In [33], authors identified skin color using three-color spaces, namely: HSV, YCrCb, and normalized RGB. This study detected the skin pixel with an accuracy of 91%. Using chrominance color space techniques to detect objects outperforms the existing model in facial recognition [34]. The Chroma component is an adequate feature for edge detection and localizing objects [34]. We opted to use CLAHE and chroma based on the advantages discussed above.
Extracting reflectance component from chroma
The Illumination–Reflectance model highlights how objects interact with light [33]. It is used in image enhancement applications that rely on the Homomorphic filter [35] or retinex [36]. This model presumes that each pixel intensity shows the quantity of light reflected by a specific object. This corresponds to the product of illumination and the scene reflectance component of an object.
L, R, and F depict the illumination, reflectance, and image formation, respectively [37]. Niyishaka et al. [28] highlighted that L relates to the low-frequency component, and R relates to the high-frequency component. Moving into the log domain (ln), to separate the illumination and reflectance components, we can turn a multiplicative component into an additive one. The following equation highlights the details. Equation 4 shows multiplicative component. Equation 5 shows the process of moving into the log domain (ln). Equation 6 turns a multiplicative component into an additive one.
Max–Min filter application
Fasihi et al. [38] demonstrated that the sharp edges of the image are located in high-frequency bands. Perceiving that R relates to the high-frequency component [28], we use the Max–Min filter that blurs CXR images by keeping essential edges.
From this perspective, the Max–Min filter (approximation of an edge-preserving filter) was applied to extract Cr from YCrCb. The final image is the estimated reflectance constituent R. Because both Cr and Cb are Chroma components, their performances have been compared; Cr performed better than Cb. Equation 7 define the Max–Min filter. F(x, y), represents the pixel value at coordinates (x, y) in the output (filtered) image. Sxy {K(i, j)}: This expression involves a neighborhood Sxy centered at the pixel (x, y) in the original image. K(i, j), represents the pixel value at coordinates (i, j) in the original image, within the defined neighborhood Sxy.
Algorithm 1 uses Cr with the Max–Min filter to estimate reflectance component R.

R is the estimated reflectance, X: training data, Y: class labels of X, t = 0.05 is a tiny positive value used to eliminate division zeros, and a= 1.1 is a small constant somewhat greater than 1 used to avoid an overly brilliant image [37].
Local binary pattern (LBP)
LBP is a valuable method for extracting and categorizing textual information [9]. Maheshwari et al. [29] highlighted that LBP encodes the information about local pixel intensities in a binary-coded decimal value. Hence, LBP is an adequate texture descriptor. Image texture emphasizes color, intensity, and spatial arrangement information from an image or a designated location of interest.
\(p_c\) as a pixel value in the central, P as the number of pixels in the close surroundings, and r as a neighborhood’s radius. Equation 9 shows the computational of LBP. LBPp,r: denotes the Local Binary Pattern value for a pixel with a radius of r and p sampling points (neighbors). For each sampling point (pi), S(\(p_i\)-\(p_c\)) computes a binary value by comparing the intensity of the sampling point (pi) with the intensity of the central pixel (pc). If the intensity of pi is greater than or equal to pc, S(\(p_i-p_c\)) is set to 1; otherwise, it is set to 0.
Figure 3 illustrates the local binary pattern (LBP) Transformation process applied to COVID-19, normal lungs, and pneumonia CXR images.
COVID-19 chest X-ray detection
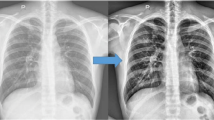
Figure 4 depicts the abnormal regions of CXR (yellow circle). The first row highlights two different infected CXR images with COVID-19. At the same time, the second row depicts their corresponding rainbow transformations. A professional radiologist performed the annotations.
To detect COVID-19 in the input CXR images, we used CLAHE-YCrCb, LBP, and machine learning algorithms. Running multiple classifiers and comparing their performances has been a common strategy. We have considered the classifier with the best results as the best performer. Mubarak et al. [9] provide instant access to a variety of classification techniques, such as KNN, SVM, LDA [39], LR [40], DT [41], and NB [42].
Experimental results
Datasets description
We used three different CXR datasets from [16, 43, 44]. The first dataset [16] has 139, 190, and 200 images of COVID-19, pneumonia, and normal lungs, respectively. The second dataset [43] is constructed based on the below Table 1.
Figure 5 highlights, in brief, a snapshot of used [16] datasets, Whereas Fig. 6 depicts the used datasets and their corresponding chest X-ray images.
The first row depicts COVID-19 images. Whereas the second row shows normal images. These images were randomly selected from [16] dataset
The third dataset [44] has 841 negative and 243 positives (COVID-19) images.
Performance metrics
The following metrics are used to evaluate the performance of the proposed model [48]: \(t_p\) are COVID-19 CXR images correctly identified (True positives). Mistakenly identified images as COVID-19 are \(f_p\) (False positives). Undetected COVID-19 chest X-Ray images classified as normal are \(f_n\) (False negatives). CXR images appropriately recognized as normal are \(t_n\) (True negatives). The true positive rate is denoted as \(tp_r\), while the false positive rate is given by \(fp_r\). Precision (\(p_r\)) specifies that a detected COVID-19 chest X-Ray image is genuinely a COVID-19 chest X-Ray image. In contrast, recall (\(r_c\)) denotes the probability of a valid COVID-19 CXR positive image being recognized. The \(f_1\) score is a metric that combines \(p_r\) and \(r_c\) into a specific numerical. acc denotes the accuracy.
Analysis of running time and platforms
The platforms adopted include a Dell laptop with an Intel (R) Core (TM) i7-3540 M CPU @ 3.00GHz x 4. 64-bit with 8GB RAM. Python 3.7.6, Scikit-learn 0.23.1, and Ubuntu 18.04.3 LTS OS. Table 2 reports the running time in minutes. Training size = \(70\%\) and test size = \(30\%\)
Results
The experiments are divided into three major sections: the first section used the dataset [16] to classify between Covid-19 and normal CXR images, and COVID-19 and pneumonia. The second section of the experiments focused on dataset [43] to classify between COVID-19 and normal CXR images. Finally, the dataset [44] was used in the last experimental section to detect COVID-19 and normal CXR images.
Experiment (section one) using [16] dataset
The proposed model was initially trained using dataset [16]. We classified normal lungs and COVID-19 CXR images. Figures 7 and 8 highlight the graphical plots of the receiver operating characteristics (ROC) curve and the confusion matrix.
Table 3 portrays the obtained accuracy of different classifiers. DT, KNN, and Naive Bayes reported the highest accuracy of 99.01% each. LR and SVM reported a lower accuracy of 55.88% each.
We conducted another experiment, considering the same dataset [16]. This time, we were classifying COVID-19 and pneumonia CXR images.
Figures 9 and 10 highlight the graphical plots of the ROC curve and the confusion matrix.
Table 4 highlights the attained accuracy. Both the DT and NB reported an accuracy of 98.9% each. KNN reported an accuracy of 97.9%. LR and SVM reported a lower accuracy of 58.50% each.
Experiment (section two) using [43] dataset
The second part of our experiment considered [43] dataset to classify between Normal and COVID-19 CXR images. Figures 11 and 12 highlight the graphical plots of the ROC curve and the confusion matrix.
Table 5 outlines the reported accuracy. DT, KNN, and NB reported an accuracy of 100% each. While LR and SVM reported a lower accuracy of 53.59% each.
Experiment (section three) using [44] dataset
The third part of the experiments considered [44] dataset to classify between normal and COVID-19 CXR images. Table 6 and Fig. 13 highlight both the model’s accuracy summary and the graphical plot of the ROC curve, respectively. While Fig. 14 outlines the confusion matrix.
Below Fig. 15 portrays all classifiers and their corresponding accuracy, precision, recall, and F1-Score, respectively. Graph (a) corresponds to the first part (section one) experiment to classify COVID-19 and normal CXR images. The second graph (b) depicts the classification results between COVID-19 and pneumonia CXR images. Graph (C) represents the experimental results of the second part (section two). Finally, graph (d) displays the results of the experiment’s third part (section three).
From Fig. 15, NB and DT outperformed other classifiers. While LR and SVM poorly detected COVID-19, normal, and pneumonia CXR images.
Both experiments, one and three, used imbalanced datasets. Therefore, to evaluate the measurement of the uncertainty of the proposed model, we used an accuracy confidence interval and PR curve.
Figure 16, (A and B) highlights the Confidence interval and PR curve of the performed section one experiment classifying Covid-19 and normal images, respectively. Whereas (C and D) portray the confidence interval and PR curve of the performed section three experiment, classifying Covid-19 and normal, respectively.
Comparative results
The proposed model is computationally efficient (see Table 7). It has a simple model architecture (see Table 8), and uses a small feature vector size (see Table 9).
Table 7 demonstrates the platform and obtained accuracy. Taking into consideration the work performed by [16], they adopted an Intel Xeon Gold 6150 2.7GHz 18-core (16 cores enabled) server with 24.75MB L3 Cache, (Max Turbo Freq. 3.7GHz, Min 3.4GHz). The GPU on this server was an NVIDIA Quadro P5000 (2,560 Cores, 16GB Memory). RAM on the server was Three hundred and sixty GB (Six channels).
Our proposed model uses a Dell laptop with an Intel (R) Core (TM) i7- 3540 M CPU @ 3.00GHz x 4. 64-bit with 8GB RAM. Python 3.7.6, Scikit-learn 0.23.1, and Ubuntu 18.04.3 LTS OS.
Table 8 highlights the reported accuracy and the model descriptions. El-Sayed et al. [43] used the RESCOVIDTCNNet model. This integrates the empirical wavelet transform (EWT), temporal convolutional neural network (TCN), dilated Causal Convolution Layer, and residual block. They reported an accuracy of 100%. Rahman et al. [49] adopted a transfer learning model (ChexNET). They reported an accuracy of 96.29%. Chowdhury et al. [47] used the DensNet201 transfer learning model. An accuracy of 99.70% was computed.
In contrast, our proposed model uses a simple architecture of CLAHE, YCrCb, LBP, and machine learning algorithms to classify our CXR images.
Table 9 depicts reported accuracy, trainable parameters, and the feature vector size. The work performed by [44] used estimated trainable parameters of 2112. These methods compute the trainable parameters [50, 51].
Conclusion
This paper presents a novel method to detect COVID-19, Normal, and pneumonia using CXR images. The proposed method is based on Contrast Limited Adaptive Histogram Equalization, Illumination–Reflectance model, and LBP. This method takes input chest X-ray images and enhances them using the CLAHE algorithm. The output images from CLAHE are converted into YCrCb color space. The reflectance component is estimated using the Illumination–Reflectance model from Cr. Finally, the Local Binary Patterns (LBP) histogram generated from reflectance and YCb is used as the feature vector. Experimental results from three publicly available datasets reported accuracy of 99.01%, 100%, and 98.46%, respectively. Our model is computationally efficient, using a small feature vector size and less running time. Emerging nations can use this prototype where radiologists need more supply.
Our future work will explore other modalities, such as CT scans, ultrasounds, and chest MRIs. We will investigate multi-classification tasks between COVID-19, normal, and pneumonia, also exploring why SVM and LR are ineffective. Additionally, we will utilize image blob visualization techniques to precisely and accurately locate the infected area. Ultimately, we hope to develop an AI model that can be integrated with electronic health records (EHRs) to extract critical clinical data, including vital signs, lab results, and patient demographics, and combine it with chest X-ray images to enhance the accuracy of COVID-19 diagnosis and interpretability.
Availability of data and materials
The three datasets used during the current study are available in the following repositories:
1 N-CLAHE-MEDICAL-IMAGES, https://github.com/mhorry/N-CLAHE-MEDICAL-IMAGES/tree/master/CXR/C-P-N
2 CoronaHack -Chest X-Ray-Dataset, https://www.kaggle.com/datasets/praveengovi/coronahack-chest-xraydataset
3 DLAI3 Hackathon, https://www.kaggle.com/c/dlai3/
The coding materials used during the current study are available in the CLAHE-YCrCB-LBP-COVID-19-Detection repository. https://github.com/rukuprince/CLAHE-YCrCB-LBP-COVID-19-Detection.
Abbreviations
- C.X.R:
-
Chest X-rays
- LBP:
-
Local binary pattern
- HE:
-
Histogram equalizer
- CLAHE:
-
Contrast limited adaptive histogram equalization
- R.O.C:
-
Receiver operating characteristics
- CNN:
-
Convolutional neural network
- TL:
-
Transfer learning
- AUC:
-
Area under the curve
- PR:
-
Precision–recall
- CI:
-
Confidence interval
References
Worldometer. COVID-19 corona virus pandemic: coronavirus cases. https://www.worldometers.info/coronavirus/. Accessed 28 March 2022.
Aggarwal S, Gupta S, Alhudhaif A, Koundal D, Gupta R, Polat K. Automated COVID-19 detection in chest X-ray images using fine-tuned deep learning architectures. Expert Syst. 2022;39(3):12749.
Kameswari S, Brundha M, Ezhilarasan D. Advantages and disadvantages of RT-PCR in COVID 19. Eur J Mol Clin Med. 2020;7:1174–81.
Purohit K, Kesarwani A, Ranjan Kisku D, Dalui M. Covid-19 detection on chest X-ray and CT scan images using multi-image augmented deep learning model. In: Proceedings of the seventh international conference on mathematics and computing. Springer; 2022. p. 395–413.
Jones JL. Reverse transcription polymerase chain reaction. https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/reverse-transcription-polymerase-chain-reaction. Accessed 20 June 2022.
Aziz S, Khan MU, Rehman A, Tariq Z, Iqtidar K. Computer-aided diagnosis of COVID-19 disease from chest X-ray images integrating deep feature extraction. Expert Syst. 2021;39: e12919.
Zammit J, Fung DL, Liu Q, Leung CK-S, Hu P. Semi-supervised COVID-19 CT image segmentation using deep generative models. BMC Bioinform. 2022;23(7):1–16.
Barstugan M, Ozkaya U, Ozturk S. Coronavirus (COVID-19) classification using CT images by machine learning methods. 2020. arXiv:2003.09424.
Mubarak AS, Serte S, Al-Turjman F, Ameen ZS, Ozsoz M. Local binary pattern and deep learning feature extraction fusion for COVID-19 detection on computed tomography images. Expert Syst. 2021;39:e12842.
Adimoolam M, Govindharaju K, John A, Mohan S, Ahmadian A, Ciano T. A hybrid learning approach for the stage-wise classification and prediction of COVID-19 X-ray images. Expert Syst. 2021.
Khalifa NEM, Manogaran G, Taha MHN, Loey M. A deep learning semantic segmentation architecture for COVID-19 lesions discovery in limited chest CT datasets. Expert Syst. 2021;39: e12742.
Joshi N. Exploring the limits of transfer learning. https://www.allerin.com/blog/exploring-the-limits-of-transfer-learning. Accessed 07 Feb 2020.
Subramanian N, Elharrouss O, Al-Maadeed S, Chowdhury M. A review of deep learning-based detection methods for COVID-19. Comput Biol Med. 2022;143: 105233.
Bhattacharyya A, Bhaik D, Kumar S, Thakur P, Sharma R, Pachori RB. A deep learning based approach for automatic detection of COVID-19 cases using chest X-ray images. Biomed Signal Process Control. 2022;71: 103182.
Ismael AM, Şengür A. Deep learning approaches for COVID-19 detection based on chest X-ray images. Expert Syst Appl. 2021;164: 114054.
Horry MJ, Chakraborty S, Paul M, Ulhaq A, Pradhan B, Saha M, Shukla N. Covid-19 detection through transfer learning using multimodal imaging data. IEEE Access. 2020;8:149808–24.
Alshayeji MH, ChandraBhasi Sindhu S, Abed S. Cad systems for COVID-19 diagnosis and disease stage classification by segmentation of infected regions from CT images. BMC Bioinform. 2022;23(1):1–28.
Shah PM, Ullah F, Shah D, Gani A, Maple C, Wang Y, Abrar M, Islam SU, et al. Deep GRU-CNN model for COVID-19 detection from chest X-rays data. IEEE Access. 2021;10:35094–105.
Bhuyan HK, Chakraborty C, Shelke Y, Pani SK. COVID-19 diagnosis system by deep learning approaches. Expert Syst. 2022;39(3):12776.
Khan SH. COVID-19 detection and analysis from lung CT images using novel channel boosted CNNS. 2022. arXiv:2209.10963.
Khan SH, Sohail A, Khan A, Hassan M, Lee YS, Alam J, Basit A, Zubair S. Covid-19 detection in chest X-ray images using deep boosted hybrid learning. Comput Biol Med. 2021;137: 104816.
Kwekha-Rashid AS, Abduljabbar HN, Alhayani B. Coronavirus disease (COVID-19) cases analysis using machine-learning applications. Appl Nanosci. 2021;13:1–13.
Kassania SH, Kassanib PH, Wesolowskic MJ, Schneidera KA, Detersa R. Automatic detection of coronavirus disease (COVID-19) in X-ray and CT images: a machine learning based approach. Biocybern Biomed Eng. 2021;41(3):867–79.
Kumar R, Arora R, Bansal V, Sahayasheela VJ, Buckchash H, Imran J, Narayanan N, Pandian GN, Raman B. Accurate prediction of COVID-19 using chest X-ray images through deep feature learning model with smote and machine learning classifiers. MedRxiv. 2020.
Mydukuri RV, Kallam S, Patan R, Al-Turjman F, Ramachandran M. Deming least square regressed feature selection and Gaussian neuro-fuzzy multi-layered data classifier for early COVID prediction. Expert Syst. 2021;39:12694.
Campos GFC, Mastelini SM, Aguiar GJ, Mantovani RG, Melo LF, Barbon S. Machine learning hyperparameter selection for contrast limited adaptive histogram equalization. EURASIP J Image Video Process. 2019;2019(1):1–18.
Zhu H, Fan H, Shu Z, Yu Q, Zhao X, Gan P. Edge detection with chroma components of video frame based on local autocorrelation. IEEE Access. 2019;7:48543–50.
Niyishaka P, Bhagvati C. Image splicing detection technique based on illumination–reflectance model and LBP. Multimed Tools Appl. 2021;80(2):2161–75.
Maheshwari S, Sharma RR, Kumar M. LBP-based information assisted intelligent system for COVID-19 identification. Comput Biol Med. 2021;134: 104453.
Saha P, Sadi MS, Islam MM. EMCNet: automated COVID-19 diagnosis from X-ray images using convolutional neural network and ensemble of machine learning classifiers. Inform Med Unlocked. 2021;22: 100505.
Jiang H, Chen F, Liu X, Chen J, Zhang K, Chen L. Thermal wave image deblurring based on depth residual network. Infrared Phys Technol. 2021;117: 103847.
Salem N, Malik H, Shams A. Medical image enhancement based on histogram algorithms. Procedia Comput Sci. 2019;163:300–11.
Rahmat RF, Chairunnisa T, Gunawan D, Sitompul OS. Skin color segmentation using multi-color space threshold. In: 2016 3rd international conference on computer and information sciences (ICCOINS). IEEE; 2016. p. 391–6.
Lu Z, Jiang X, Kot A. Color space construction by optimizing luminance and chrominance components for face recognition. Pattern Recognit. 2018;83:456–68.
Singla R, Singh S. A framework for detection of jaundice in new born babies using homomorphic filtering based image processing. In: 2016 International conference on inventive computation technologies (ICICT), vol. 3. IEEE; 2016. p. 1–5.
Cao N, Lyu S, Hou M, Wang W, Gao Z, Shaker A, Dong Y. Restoration method of sootiness mural images based on dark channel prior and Retinex by bilateral filter. Herit Sci. 2021;9(1):1–19.
Chen D, Lan S, Xu P, Zhang Y. Illumination-reflectance based image enhancement method for character recognition. In: 2016 9th international congress on image and signal processing, biomedical engineering and informatics (CISP-BMEI). IEEE; 2016. p. 207–11.
Fasihi MS, Mikhael WB. Brain tumor grade classification using LSTM neural networks with domain pre-transforms. 2021. arXiv:2106.10889.
Tzalavra AG, Andreadis I, Dalakleidi KV, Constantinidis F, Zacharaki EI, Nikita KS. Dynamic contrast enhanced-magnetic resonance imaging radiomics combined with a hybrid adaptive neuro-fuzzy inference system-particle swarm optimization approach for breast tumour classification. Expert Syst. 2021;39:e12895.
Sharma P, Sharma K. A novel quantum-inspired binary bat algorithm for leukocytes classification in blood smear. Expert Syst. 2021;39:e12813.
Chen G, Zhang W. Application of big data information system in early diagnosis, treatment, and nursing of cervical cancer infected by human papillomavirus. Expert Syst. 2021;40: e12791.
Tiwari D, Bhati BS, Al-Turjman F, Nagpal B. Pandemic coronavirus disease (COVID-19): world effects analysis and prediction using machine-learning techniques. Expert Syst. 2021;39: e12714.
El-Dahshan E-SA, Bassiouni MM, Hagag A, Chakrabortty RK, Loh H, Acharya UR. RESCOVIDTCNnet: A residual neural network-based framework for COVID-19 detection using TCN and EWT with chest X-ray images. Expert Syst Appl. 2022;204:117410.
Li C, Wang M, Wu G, Rana K, Charoenkitkarn N, Chan J. Covid19 chest X-ray classification with simple convolutional neural network. In: CSBio’20: proceedings of the eleventh international conference on computational systems-biology and bioinformatics. 2020; p. 97–100.
Ozturk T, Talo M, Yildirim EA, Baloglu UB, Yildirim O, Acharya UR. Automated detection of COVID-19 cases using deep neural networks with X-ray images. Comput Biol Med. 2020;121: 103792.
MOONEY P. Chest x-ray images (pneumonia). https://www.kaggle.com/datasets/paultimothymooney/chest-xray-pneumonia. Accessed 30 June 2022.
Chowdhury ME, Rahman T, Khandakar A, Mazhar R, Kadir MA, Mahbub ZB, Islam KR, Khan MS, Iqbal A, Al Emadi N, et al. Can AI help in screening viral and COVID-19 pneumonia? IEEE Access. 2020;8:132665–76.
Saminathan M, Ramachandran M, Kumar A, Rajkumar K, Khanna A, Singh P. A study on specific learning algorithms pertaining to classify lung cancer disease. Expert Syst. 2022;39(3):12797.
Rahman T, Khandakar A, Qiblawey Y, Tahir A, Kiranyaz S, Kashem SBA, Islam MT, Al Maadeed S, Zughaier SM, Khan MS, et al. Exploring the effect of image enhancement techniques on COVID-19 detection using chest X-ray images. Comput Biol Med. 2021;132:104319.
Madhivarman. How to calculate the number of parameters in the CNN? https://medium.com/@iamvarman/how-to-calculate-the-number-of-parameters-in-the-cnn-5bd55364d7ca. Accessed 30 May 2018.
Vasudev R. Understanding and calculating the number of parameters in convolution neural networks (CNNs). https://towardsdatascience.com/understanding-and-calculating-the-number-of-parameters-in-convolution-neural-networks-cnns-fc88790d530d. Accessed 11 Feb 2019.
Khalifa NEM, Taha MHN, Chakrabortty RK, Loey M. Covid-19 chest X-rays classification through the fusion of deep transfer learning and machine learning methods. In: Proceedings of 7th international conference on harmony search, soft computing and applications. Springer. 2022; p. 1–11.
Acknowledgements
We gratefully acknowledge all the support from the Beijing Institute of Technology, the School of Computer Science and Technology, and the Chinese Scholarship Council (CSC) for making this work successful.
Funding
This work was supported by the African Center of Excellence in Data Science, the African Center of Excellence in the Internet of Things (ACE-DS, ACEIoT), and the University of Rwanda.
Author information
Authors and Affiliations
Contributions
R.P. initiated, designed, researched, and wrote this manuscript. Z.N. directed, organized, and provided all significant technical support for this work. Z.Y.K. gathered the background and revised the results. N.P. and M.E. prepared the related works and revised the results. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Prince, R., Niu, Z., Khan, Z.Y. et al. COVID-19 detection from chest X-ray images using CLAHE-YCrCb, LBP, and machine learning algorithms. BMC Bioinformatics 25, 28 (2024). https://doi.org/10.1186/s12859-023-05427-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12859-023-05427-5