Abstract
Physiological roles of Cl−, a major anion in the body, are not well known compared with those of cations. This review article introduces: (1) roles of Cl− in bodily and cellular functions; (2) the range of cytosolic Cl− concentration ([Cl−]c); (3) whether [Cl−]c could change with cell volume change under an isosmotic condition; (4) whether [Cl−]c could change under conditions where multiple Cl− transporters and channels contribute to Cl− influx and efflux in an isosmotic state; (5) whether the change in [Cl−]c could be large enough to act as signals; (6) effects of Cl− on cytoskeletal tubulin polymerization through inhibition of GTPase activity and tubulin polymerization-dependent biological activity; (7) roles of cytosolic Cl− in cell proliferation; (8) Cl−-regulatory mechanisms of ciliary motility; (9) roles of Cl− in sweet/umami taste receptors; (10) Cl−-regulatory mechanisms of with-no-lysine kinase (WNK); (11) roles of Cl− in regulation of epithelial Na+ transport; (12) relationship between roles of Cl− and H+ in body functions.
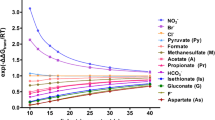
Similar content being viewed by others
Introduction
The ionic environment in the body plays an important role in bodily and cellular function [1,2,3,4,5,6,7,8,9,10]. The physiological role of cations has been studied in detail; i.e., Na+, K+, Ca2+, Mg2+ and H+ are well known to contribute to cellular functions such as generation of action potential, maintenance of resting membrane potential and control of enzyme activity. On the one hand, the most well-recognized role of Cl−, the major anion in the body, is as a counter ion to the cation for maintenance of electroneutrality, but other physiological significance of Cl− is currently only marginally recognized.
Active Cl− transport such as Na+-K+-2Cl− transporter (NKCC) and K+-Cl− transporter (KCC) is involved in the maintenance of the membrane potential [1,2,3,4,5]. NKCC contributes to water secretion into the luminal side of epithelial tissues driven by elevating luminal osmolarity via active transcellular Cl− secretion in concert with Cl− channels followed by the paracellular Na+ secretion [11, 12]. One of the most famous diseases based on impaired water secretion due to dysfunction of Cl− channels is cystic fibrosis (CF) in the lung, the liver, sinus, small and large intestines, pancreatic and hepatobiliary ducts, and male reproductive tracts [13,14,15,16,17,18]. CF is a genetic disease caused by mutations in cystic fibrosis transmembrane conductance regulator (CFTR), the cloning of which was performed in 1989 [19]. The main cause of death in CF patients is pulmonary infection due to drying of the lung cavity as a result from insufficient water secretion caused by dysfunction of certain Cl− channels. A Cl− channel was cloned as cystic fibrosis transmembrane conductance regulator (CFTR) [19], and CFTR has been characterized by many researchers [20]. Furthermore, the recently proposed role of CFTR as a modulator of immune tolerance may explain the presence of persistent portal vein inflammation leading to fibrosis, and the enterohepatic axis would also be involved in the presentation and progression of the disease [18]. In addition, Cl− also plays physiological roles in regulation of activities of enzymes, gene expression, ion channels, ion transporters, ion pumps, ion environments, infection prevention, etc.; e.g., GTPase activity [21], neurite elongation [22], resistance against anticancer drugs [23,24,25], cell death [26, 27], regulation of cell volume [28], autophagy [29, 30], cell proliferation [31], ciliary movements [32,33,34], sweet/umami taste sensing at sweet/umami taste receptors [35, 36], WNK activity [37], epithelial Na+ transport [38, 39], mRNA expression of epithelial Na+ channel (ENaC) [40,41,42,43], the Na+,K+-pump activity [44], and pH homeostasis cooperating with bicarbonate [45,46,47].
This review will introduce physiological roles of Cl−, molecular mechanisms of Cl− actions on a variety of physiological phenomena, and possibilities that cytosolic Cl− may act as intracellular signals.
Requirements for cytosolic Cl− to function as intracellular signals
For cytosolic Cl− to function as intracellular signals, Cl− must cause conformational changes in proteins, such as enzymes, which regulate intracellular functions. For this to happen, the cytosolic Cl− concentration ([Cl−]c) must change or the binding affinity of Cl− to these proteins must change. Since only a limited number of studies have been conducted so far to precisely investigate how the binding affinity of Cl− to various proteins is altered by any factors, this review article will primarily address whether [Cl−]c can in fact be altered and, if so, to what extent [Cl−]c must be altered for cytosolic Cl− to act as intracellular signals.
How much is [Cl−]c?
The [Cl−]c in gastric and respiratory epithelial cells is reported to be about 50 mM [48,49,50]. Several studies have also reported that [Cl−]c in the paranasal olfactory system (plough nose) cells are very variable, 5 ~ 80 mM [51,52,53,54,55,56,57,58,59,60]. [Cl−]c is known to be higher in the dendrites of neurons than in the cell bodies [51, 61]. Further, Engels et al. [60] has reported that under both control and chemical ischemia conditions, [Cl−]c values markedly differ in various subcellular regions and cell types. Their study [60] also indicates that the [Cl−]c in astrocytes of the hippocampal cornu ammonis region 1 is 21 mM, which is lower than that (28 mM) in dentate gyrus, but higher than that (14 mM) in neocortical astrocytes. In addition, the [Cl−]c in radial glia-like cells (20 mM) is comparable to the value (21 mM) of astrocytes in the hippocampal cornu ammonis region 1 [60]. These [Cl−]c values (14 ~ 28 mM) [60] are considerably much lower than 35 mM [Cl−]c determined in cerebellar Bergmann glia cells [59]. The studies [48, 49, 51,52,53,54,55,56,57,58,59,60,61] indicate that [Cl−]c values are very valuable depending on types and regions of cells. One of the most important points is whether [Cl−]c changes under an isosmotic condition; i.e., it should be considered whether [Cl−]c changes under an isosmotic condition due to the following reason. As Cl− moves, cations such as Na+ and K+ also move in the same direction as Cl− to maintain electrical neutrality, causing osmolarity elevation. This osmolarity elevation causes water movement in the same direction. Therefore, the increase in [Cl−]c due to Cl− movement is attenuated by the water movement. Thus, the change in [Cl−]c due to Cl− movement under an isosmotic condition should be carefully evaluated.
Does [Cl−]c change with cell volume change under an isosmotic condition?
Changes in [Cl−]c are discussed based on the relationship between water movement and cell volume associated with Cl− movement. One of the requirements for cytosolic Cl− to act as an intracellular signal is a change in [Cl−]c. It is recognized that unlike cytosolic Ca2+ concentration ([Ca2+]c), [Cl−]c may not change much. Furthermore, it is easy to imagine that changes in the extracellular fluid osmolarity would induce water movement in and out of the cell, which would change [Cl−]c. On the other hand, can the [Cl−]c change under an isosmotic condition of extracellular fluids? Cytosolic K+ concentration ([K+]c) generally does not change regardless of the amount of K+ efflux (or influx) in a state in the isosmotic state. This is due to the efflux (influx) of anions (generally Cl−) with an equivalent negative charge to maintain cytosolic electroneutrality at cationic K+ movement, followed by water movement to compensate for osmotic changes caused by these ion (K+ and Cl−) movements (Fig. 1). As a result, no change in [K+]c occurs. On the other hand, [Cl−]c changes under these circumstances unlike [K+]c (Fig. 1). In the case of anions, [Cl−]c is kept lower than [K+]c due to the presence of many anions (various proteins) in the cell that cannot pass through the plasma membrane (membrane-impermeable anions such as big molecule proteins: so-called fixed charges) (Fig. 1). The presence of many membrane-impermeable anions (proteins) causes [Cl−]c to change in response to K+ efflux (or influx) [1] (Fig. 1). This is because even if [Cl−]c is lower than [K+]c, Cl− efflux (or influx) occurs in the same amount as the K+ efflux (or influx) in order to maintain cytosolic electroneutrality, since Cl− is the major membrane-permeable anion in the cytosolic space under the condition that large amounts of membrane-impermeable anions (fixed charges) are present (Fig. 1).
A simple model of correlation between changes in cytosolic Cl− concentration ([Cl−]c) and cell volume under isosmotic conditions. This simple model shows contents and concentrations of K+, Cl− and membrane-impermeable fixed negative charges such as proteins, although other ions including Na+ and HCO3− significantly exist in cell. A Cell volume = 100%. Cell contains 150 mmoles/L K+ (150 mM), 45 mmoles/L Cl− and 105 mEq/L fixed negative charges. B Cell volume = 80%. When the cell volume reduces to 80% under an isosmotic condition, 20% K+ (30 mmoles/L) is released from the cytosolic space to the extracellular space; K+ remaining in the cytosolic space is 120 mmoles/L and the cytosolic K+ concentration (150 mM) is same as before the cell volume change occurs. On the one hand, when cell volume decreases by 20%, the same amount of Cl− (30 mmoles/L) as K+ must be released from the cytosolic space to the extracellular space to keep electroneutrality. This means that the cytosolic Cl− is reduced to 15 mmoles/L from 45 mmoles/L after the occurrence of 20% cell volume decrease, and the cytosolic Cl− concentration is reduced to 19 mM (15 mmoles/0.8 L) from 45 mM before the cell volume decrease occurs. This is because even though the cytoplasmic Cl− content (45 mmoles/L) is much lower than the cytoplasmic K+ content (150 mmoles/L), the same amount of Cl− as K+ must be released from the cytosolic space due to the presence of a large amount of membrane-impermeable fixed negative charge
Does [Cl−]c changes under the condition that multiple Cl− transporters and channels contribute to Cl− influx and efflux in an isosmotic state?
Cl− transport across the plasma membrane by Cl− transporters and channels participates in changes of [Cl−]c. Cl− transport can be broadly divided into active and passive transport systems. The most well-known active Cl− transporters are Na+-K+-2Cl− cotransporter (NKCC), Na+-Cl− transporter (NCC), Na+-driven Cl−/HCO3− exchanger (NDCBE) and K+-Cl− cotransporter (KCC) [62,63,64,65]. NKCC and NCC contribute to Cl− uptake into cells using electrochemical potential of Na+ generated by the Na+,K+-pump (ATPase), while NDCBE and KCC, respectively, participate in Cl− extrusion from cells using electrochemical potential of Na+ and K+ generated by the Na+,K+-pump (ATPase).
An increase in NKCC-mediated Cl− influx elevates [Cl−]c. The elevated [Cl−]c induces an increase in the chemical potential of cytosolic Cl−, which elevates Cl− efflux through Cl− channels. The [Cl−]c increases until the elevation of Cl− efflux through Cl− channels is equal to the increase in Cl− influx via NKCC. At this point, the [Cl−]c change reaches equilibrium. The opposite phenomenon occurs when NKCC-mediated Cl− influx is reduced; [Cl−]c decreases, causing reduction of Cl− efflux through Cl− channels. Then, the reduction in [Cl−]c reaches equilibrium at a point when the decrease in Cl− efflux through Cl− channels is equal to the reduction of Cl− influx via NKCC. Further, when activities of KCC change, similar phenomena occur, resulting in alternation of [Cl−]c. In addition, altering Cl− channel activity causes the same thing in [Cl−]c. An increase in Cl− channel activity induces elevation of Cl− flux (influx or efflux depending on the electrochemical potential of cytosolic Cl−), which changes [Cl−]c. This change in [Cl−]c alters the chemical potential of cytosolic Cl−, which changes the Cl− flux through Cl− channels and settles at the same point as the original Cl− flux through Cl− channels. Thus, even though multiple Cl− transporters and channels contribute to Cl− influx and efflux, [Cl−]c changes when activities of Cl− transporters and/or channels are altered. An interesting point in terms of Cl− flux is that changes in [Cl−]c due to changes in Cl− channel activity are transient, whereas changes in Cl− flux due to changes in Cl− transporter activity are persistent.
Is the change in [Cl−]c large enough to act as an intracellular signal?
Consideration should be given whether the change in [Cl−]c is large enough to act as an intracellular signal. [Ca2+]c increases about tenfold compared to the resting state, while [Cl−]c usually changes only about twofold (or 0.5-fold) [66]. Is it possible that Cl−, which fluctuates only over such a small range of change, could play an intracellular signaling role? The binding number of Cl− to target substances such as channel proteins and enzymes should be also considered. If the number of Cl− binding sites on a protein with enzyme activity is 3, a twofold change in Cl− concentration ([Cl−]) has the same effect on enzyme activity as an eightfold change (23 = 8: 2, twofold change in [Cl−]; 3, the number of binding sites). When the number of Cl− binding sites is 4, a twofold change in [Cl−] has the same effect as a 16-fold change in [Cl−] (24 = 16: 2, twofold change in [Cl−]; 4, the number of binding sites). The theoretical simulation suggests that a small [Cl−]c change such as twofold would be large enough to act as an intracellular signal.
Effects of Cl− on cytoskeletal tubulin polymerization through inhibition of GTPase activity and tubulin polymerization-dependent biological phenomena
Because [Cl−]c in GABAergic neurons is generally lower than that estimated when the membrane potential is set to the equilibrium potential of Cl−, the GABA-induced increase in the conductance of Cl− channel causes Cl− influx, resulting in membrane hyperpolarization, which develops during maturation [67,68,69]. The lower [Cl−]c in GABAergic neurons is maintained by KCC. However, in some cases of GABAergic neurons, GABA causes membrane depolarization by inducing an Cl− efflux via an increase in the Cl− channel conductance. The GABA-induced Cl− efflux is attributed to an actual [Cl−]c higher than that predicted when the membrane potential is taken as the equilibrium potential for Cl− and this higher [Cl−]c is maintained by NKCC. For example, in 'juvenile' neurons, GABA induces Cl− efflux from the cytosolic space to the extracellular one, and causes membrane depolarization [62, 69,70,71,72,73]. Over the course of development, the GABA-induced change in Cl− flux shows transition from efflux to influx [71]: GABA induces Cl− efflux due to a high [Cl−]c causing membrane depolarization in immature stages, while GABA induces Cl− influx due to a low [Cl−]c leading to membrane hyperpolarization in mature stages [71, 74]. The maturation-induced decrease in [Cl−]c is due to a change in functional expression of Cl− transporters contributing to Cl− uptake such as NKCC to KCC participating in Cl− extrusion. Here, significance of high [Cl−]c in immature stages should be considered [67,68,69, 75,76,77,78,79,80,81,82,83]. Of course, excitatory signals of GABAergic stimulation cause depolarization of the plasma membrane and an increase in [Ca2+]c via activation of voltage-gated Ca2+ channels. In addition, high [Cl−]c in immature stages would be required for the formation of neural networks via tubulin polymerization and its stability [84,85,86,87] as described below.
Cl− has the ability to attenuate GTPase activity [21, 48, 66, 88,89,90] (Fig. 2A). Inhibition of GTPase promotes polymerization of tubulin, a type of cytoskeleton [21, 91,92,93] (Fig. 2A). Tubulin monomers are subclassified into three categories: i.e., α, ß, and γ subtypes [85, 94,95,96,97]. Polymerization of tubulin is formed by the binding of α- and ß-tubulin subtypes: the α/ß-tubulin heterodimer has two GTP-binding sites; one located on ß-tubulin (the E site) and the other on α-tubulin (the N site) [85, 98,99,100,101,102]. ß-tubulin has GTPase activity that hydrolyzes GTP during polymerization, and then produces GDP [85,86,87, 103] (Fig. 2A). This GDP is still bound to ß-tubulin, which is part of the tubulin polymer [85,86,87]. The GDP bound to ß-tubulin at depolymerization is exchanged to GTP, and GTP-bound ß-tubulin can polymerize once more [85,86,87, 103] (Fig. 2B). In contrast, the GTP bound to the N site in α-tubulin is neither hydrolyzed to GDP nor exchangeable to GDP during tubulin polymerizing/depolymerizing dynamics [85, 98, 103] (Fig. 2A and B). Moreover, the amino acid residues, Asp 251 and Glu 254, in α-tubulin stimulate the GTPase activity of ß-tubulin [84, 85, 87, 104]. The microtubule dynamic is achieved when the GTP molecule in the E site of ß-tubulin is hydrolyzed [85, 86]: Growth and stability in microtubule are facilitated by the presence of a “GTP cap” at its ( +), which is required in order for α and ß tubulin to stably bind to each other and promote polymerization [84, 85] (Fig. 2B-a). Like β-tubulin, actin subunits also have intrinsic GTPase activity related to microfilament stability [84]. Cl− has the ability diminishing GTPase activity [21, 48, 66, 88,89,90] (Fig. 2A). Therefore, Cl− at high concentrations inhibits the intrinsic GTPase activity of tubulin, thus preventing GTP degradation and promoting tubulin polymerization by stably binding GTP to tubulin [66, 88] (Fig. 2B-b). This suggests that cytosolic Cl− plays key roles in cellular functions by modulating tubulin-polymerization states such as formation of neuronal connectivity and network in immature stages [76, 81, 87] cancer aggressiveness, cell death, cell migration, invasion, and sensitivity to chemotherapy [107], meiosis [108], triggering of dynamic improvement in cell plasticity, regulation of energy transfer [86], and cardiac mechanics [109]. Thus, Cl−-induced promotion of the tubulin polymerization [21] serves as a plasma membrane lining structure in neurite outgrowth, and promotes plasma membrane elongation, which is essential for neurite outgrowth, resulting in neurite outgrowth [21, 110]. In fact, it has been reported that neurites lengthen as [Cl−] increases [110]. Activation of Cl− uptake into the cytosolic space in neurons enhances elongation of neurite [112, 113], while elevation of Cl− release from the cytosolic space in neurons negatively regulates elongation of neurite [113].
Action of Cl− on dynamics of tubulin polymerization and depolymerization. A Cl− suppresses conversion of GTP-ß-tubulin to GDP-ß-tubulin by inhibiting GTPase. B a In most cells, tubulin is present in concentrations of 10–20 μM, favoring the assembly of microtubules at the plus end. In filaments with slower growth rates, there is less lateral interaction between protofilaments. The inherent curvature of the GDP-tubulin dimer surface gives the appearance of fraying at this end. b High [Cl−]c stabilizes GTP-ß-tubulin by blocking GTPase activity [21], and leads to a condition of a higher concentrations of GTP-tubulin dimers. Thus, tubulin polymerization is promoted at the plus end by forming a rigid GTP-cap. c GTPase increases at low [Cl−]c. This leads to concerted GTP hydrolysis, weakening the tubulin dimer interactions, and rapidly disassembling tubulin polymerization. This figure is produced using the result obtained in a report by Nakajima et al. [21] combining information shown in ‘What is microtubule dynamic instability?’ by MBINFO DEFINING MECHANOBIOLOGY (see the information shown in “https://www.mechanobio.info/cytoskeleton-dynamics/what-is-the-cytoskeleton/what-are-microtubules/what-microtubule-dynamic-instability/#what-is-microtubule-dynamic-instability”) under a Creative Commons Attribution-NonCommercial 4.0 International License
In the early stage of cell division, microtubules composed of tubulin elongate from the centrosome (microtubule forming center), leading to cell division [115, 116]. The process of tubulin depolymerization (Fig. 2B-c) is then required for the ‘correct’ cell division at the end of cell division [115, 116]. Taxanes exert their anticancer effects by blocking tubulin depolymerization, thereby preventing cell division and arresting cancer cell division and proliferation [107, 117,118,119,120]. Cytosolic Cl− plays an important role in the action of taxanes [48]. When [Cl−]c decreases, endogenous GTPase activity in ß-tubulin increases, leading to enhancement of the degradation of GTP to GDP and the depolymerization of tubulin (Fig. 2B-c). Therefore, at low [Cl−]c, taxanes cannot inhibit tubulin depolymerization, thus taxanes cannot show their action as anticancer drugs [48], although low [Cl−]c slows the cell proliferation rate [31, 121,122,123,124].
Further, it has been reported that Cl− channels participate in resistance against anticancer drugs [23,24,25]. For instance, impaired activity of volume-sensitive Cl− channel (volume-sensitive, outwardly rectifying (VSOR) Cl− channel or volume-regulated anion channel (VRAC)) is involved in resistant potentials against an anticancer agent, cisplatin [23, 25]. Further, it has been reported that an increase in expression of ClC-3 Cl− channel would activate the NF-κB, leading to expression of P-glycoprotein, a type of ATP-binding cassette [24, 25]. P-glycoprotein plays an important role in the formation of so-called multidrug resistance by extruding anticancer drugs such as paclitaxel belonging to the taxanes [24, 25]. Thus, the ClC-3 Cl− channel would play an important role in the mechanism generating multidrug resistance [24, 25]. Another study [124] has also elucidated that ClC-3 Cl− channels generate paclitaxel resistance in ovarian cancer. In paclitaxel-resistant ovarian cancer cells (A2780/PTX cells), ClC-3 Cl− channels are found to be upregulated in both their protein expression and function compared with their parental A2780 cells [124]. The diminution of ClC-3 Cl− channel expression by siRNA in A2780/PTX cells has partly recovered the sensitivity to paclitaxel by causing the G2/M arrest via diminution of ClC-3 Cl− channel function and elevation of tubulin polymerization [124]. Paclitaxel also shows its blocking action on the current through ClC-3 Cl− channels in A2780 cells, but not in A2780/PTX cells [124]. These observations suggest us that the Cl− current (flux) through ClC-3 Cl− channel influences paclitaxel potential on tubulin polymerization by regulating [Cl−]c which participates in the sensitivity to paclitaxel. Furthermore, paclitaxel is known to cause damage of plasma membrane, leading to cell death in ovarian A2780 cancer cells [125]. Of interest, paclitaxel also induces cell swelling in ovarian A2780 cancer cells, causing pyroptosis [126, 127], which is one of cell death types, apoptosis, pyroptosis, and necrosis [128, 129]. Pyroptosis has been first reported in macrophages infected with Salmonella typhimurium [126]. The molecular mechanism producing pyroptosis is investigated from a biochemical viewpoint regarding gasdermins, a family of pore-forming proteins in humans [130, 131]. Cytosolic Cl− should be also considered to be a key player in pyroptosis via control of WNK (see Sect. "Cl--regulatory mechanisms of with-no-lysine kinase (WNK) and its physiological role") [132, 133]. Induction of apoptosis by activation of Cl− channels has been demonstrated by Shimizu et al. [133] (also refer to [27, 135]). Lee et al. [23] have reported that downregulation of VRAC is involved in multidrug resistance (also refer to [27, 135]). Further, VRAC contributes to lipopolysaccharide plus nigericin-induced pyroptosis in bone marrow-derived macrophages [135,136,137]. Thus, cytosolic Cl− and various types of Cl− channels including ClC-3 Cl− channel and VRAC are suggested to be key players involved in cell death and drug resistance.
Roles of cytosolic Cl− in cell proliferation
In gastric cancer cells, G0/G1 arrest is induced by decreased [Cl−]c [31, 121,122,123,124, 139,140,141,142,143,144,145,146,147,148,149,150,151,152]. G0/G1 arrest induced by decreased [Cl−]c is regulated via retinoblastoma protein (Rb) by a p53-independent, p21-dependent mechanism [120]: lowering [Cl−]c upregulates expression of p21, resulting in a decrease in CDK2 expression, which diminishes Rb phosphorylation, thus G0/G1 arrest occurs [120] (see a review article [152] regarding cell proliferation via p53-p21 dependent regulation).
Chloride intracellular channel 1 (CLIC1) is also reported to be a key factor in cell proliferation of esophageal squamous cell carcinoma [153,154,155]. Further, a cohort study [156] reports that genetic polymorphism in methylenetetrahydrofolate reductase Cl− transport protein 6 (MTHFR CLCN6) gene is associated with keratinocyte skin cancer, suggesting a role of Cl− in proliferation of human skin cancer. Thus, Cl− is one of key factors controlling cell proliferation.
Cl−-regulatory mechanisms of ciliary motility
Ciliary movement in the airways is essential for the function of the body's defense system by expelling foreign substances that enter the airways from the body through dynein-driven mechanisms [157] via cAMP-mediated pathways [158,159,160,161,162,163], protein kinase C-mediated pathways [164] and cytosolic Ca2+-mediated pathways [166, 167] in addition to water secretion from airway epithelia driven by Cl− secretion [88]. Cilia also play an important role in cerebrospinal flow [167]. The activity of ciliary movement is evaluated by two indices: (1) the amplitude (angle) of ciliary movement and (2) the frequency of ciliary movement (the number of ciliary movements per unit time) [32, 34, 169,170,171]. The amplitude and frequency of the ciliary movement are, respectively, controlled by the inner dynein arm (IDA) and outer dynein arm (ODA) [33, 169, 172, 173] (Fig. 3). Cytosolic Cl− has been reported to suppress both amplitude and frequency of ciliary movement, with the inhibitory action of Cl− on amplitude reaching the maximum level at low [Cl−]c and on frequency at high [Cl−]c [32,33,34]. Beta-agonist-induced cell shrinkage activates ciliary movements via a decrease in [Cl−]c (Fig. 1) [174]. Elevation of [Ca2+]c also enhances ciliary movements [176, 177]. These phenomena suggest that the Cl− sensors in IDA controlling the amplitude of ciliary movement are more sensitive to Cl− than Cl− sensors in ODA controlling the frequency of ciliary movement [168] (Fig. 3).
Cl−-regulation of ciliary beating in cultured human nasal epithelial cells. Outer dynein arms (ODAs) control the frequency of ciliary movement, and inner dynein arms (IDAs) control waveform including the amplitude (angle) of ciliary movement. Cytosolic Cl− inhibits, respectively, the function of ODAs and IDAs via binding to Cl− biding sites in the axonemal structures of ODAs and IDAs reducing the frequency and the amplitude (angle) of ciliary movement. The sensitivity of ODAs to cytosolic Cl− is less than that of IDA. Cytosolic Cl− at basal levels has no inhibitory effect on ODA function, but inhibits IDA function to some extent, but not completely. When [Cl−]c becomes lower than the basal level, ODA, which is not inhibited by basal levels of Cl−, maintains its activity, and IDA, which is partially inhibited by basal levels of Cl−, is no longer inhibited by Cl− and its activity is increased. Conversely, as [Cl−]c increases, the activity of both ODA and IDA decreases. This figure is modified from Fig. 8 reported in a study [168] under a Creative Commons Attribution-NonCommercial 4.0 International License
In sperm, mitochondrion forms a complex with rat sarcoma (Ras)-associated binding (Rab) protein 10 (RAB10) of active form (GTP bound form of RAB10; GTP-RAB10) via TOMM20 (a subunit protein of translocase in the outer membrane of mitochondria) [177,178,179]. GTP-RAB10 binds to dynein, which transports mitochondrion by forming a complex of DNAH7, a tubulin-related protein [179]. GTPase-activating protein (GAP) and guanine nucleotide exchange factor (GEF) are well known as the main factors regulating the activity of small GTP-binding proteins [181, 182]. GEF facilitates the dissociation of GDP-binding in small GTP-binding proteins, which is subsequently replaced by GTP [181, 182]. On the one hand, GAP activates the GTPase of small GTP-binding proteins, enhancing the conversion of GTP to GDP, leading to inactivation of small GTP-binding proteins [179,180,181]. ADP-ribosylation factor 6 (ARF6) is a GTPase [182]. GTP-locked mutant ARF6QL of ARF6 binds to dynein, enhancing autophagic vesicles transport in neurons, while GDP-locked mutant ARF6T27N of ARF6 impairs retrograde transport of autophagic vesicles along the axon [183, 184]. Taken together, when the GTP-bound form of dynein-binding protein binds to dynein, it promotes the transport capacity of dynein.
Cl− attenuates GTPase activity [21, 48, 66, 88,89,90], therefore high Cl− stabilizes GTP-bound form of dynein-binding protein. On the one and, cytosolic Cl− inhibits the amplitude of ciliary movement at low [Cl−]c, and the frequency of the ciliary movement at high [Cl−]c [32, 169] (Fig. 3). These observations indicate that Cl− of high concentration inhibits ciliary movements despite enhanced dynein transport activity by stabilizing active GTP-bound form of dynein-binding protein. From these observations, it is speculated that, unlike the unidirectional transport by dynein, the periodic appearance of GTP- and GDP-bound forms of dynein-binding proteins regulates ciliary reciprocal movement, although further direct evidence is needed to conclude the speculation.
Roles of Cl− in sweet/umami taste sensing at sweet/umami taste receptors
Taste is a chemical sensation perceived on the tongue and proved by chemicals in foods and beverages, and plays a very important role in the ingestion of foods and other substances, as well as in sustaining life [184,185,186,187]. Cl− is considered to participate in taste sensing, however details of molecular mechanisms of Cl− involvement are unknown [35]. Recently, a Cl− binding site has been reported in taste receptor type 1 (T1r), a member of the sweet and umami receptors on the tongue [35]. The T1r2a/T1r3 heterodimer found in medaka fish, the only T1r currently available for structural analysis, has a Cl− specific binding site near the amino acid binding site in the ligand binding domain (LBD) of T1r3, which is likely conserved among species including human T1r3. This Cl− binding at sub-millimolar to low millimolar concentrations induces a conformational change in the ligand-binding domain of the T1r2a/T1r3LBD [35]. Further, a small amount of Cl− bound to the sweet and umami taste receptors stimulates the neuron connected to the receptor cells, suggesting a small amount (low concentration) of Cl− enhances sweet and umami taste [35]. This finding strongly supports what has been said so far that small amounts (low concentrations) of NaCl promote sweet sensitivity [36].
Cl−-regulatory mechanisms of with-no-lysine kinase (WNK) and its physiological role
WNK is named for the fact that it, a serine/threonine kinase, lacks a catalytic lysine in subdomain II, which serves an important role as an ATP binding site [188]. WNK regulates the activity of stress-related serine-threonine kinases, STE20 (sterile 20)/SPS1-related proline/alanine-rich kinase (SPAK) and oxidative stress-responsive kinase 1 (OSR1), which are targets of WNK signaling, and consequently regulates cellular functions by modulating activities of PI3K-AKT, TGF-ß, and NF-κB [189]. WNK also regulates cation-coupled Cl− cotransporters via SPAK/OSR1 activation in renal epithelia, such as NKCC (NKCC1 and NKCC2) and KCC (KCC1—KCC4) [65, 191,192,193,194,195,196,197,198], which play crucial roles in regulation of the body fluid contents and blood pressure. NKCC and KCC are also regulated by various factors including flavonoids like quercetin and myricetin [40, 66, 88, 111, 199,200,201,202,203,204,205], which also show various actions including anti-diabetic and anti-hypertensive ones [66, 203, 206]. Activity of WNK is controlled by Cl− [206]. Low [Cl−]c activates WNKs, which phosphorylate the paralogous Ste20 kinases, SPAK/OSR1, on a T-loop threonine (Thr 233 in SPAK, Thr 185 in OSR1) to activate the kinases, SPAK/OSR1 [207]. The activated SPAK/OSR1 phosphorylate NKCC1, NKCC2 and NCC on serine/threonine conserved in N-termini of the transporters [207]. Activated SPAK/OSR1 phosphorylate serine/threonine conserved at the N-terminus of NKCC1, NKCC2 and NCC, increasing the transporting activity of the transporters [207]. WNK has two domains, a smaller N-terminal domain and a larger C-terminal domain, which form an inactive, asymmetric dimer [207]. Cl− binds to its binding site in the subunit of unphosphorylated dimeric WNK, stabilizing the inactive dimer of WNK [207], thus Cl− inhibits WNK activity [207, 208]. The physiological meaning of Cl−-induced stabilization of inactive dimer of WNK is that a decrease in [Cl−]c activates NKCC and NCC that participate in Cl− uptake into the intracellular space via enhancement of WNK phosphorylation (activation), contributing to the homeostasis of [Cl−]c.
When cells migrate, cells need to change cell shape. WNK activated by lowered [Cl−]c induces phosphorylation (activation) of SPAK/OSR1, which increases activity of NKCC1 by phosphorylating NKCC1, then activated WNK participates in cell migration as follows [208]. NKCC1 is expressed on the front line side of cell migration and is involved in the uptake of Cl− into the cytosolic space along with Na+ and K+ (Fig. 4) [197, 209,210,211,212]. The uptake of these ions results in the water influx via aquaporin (AQP) into the cytosolic space by increasing cytosolic osmolarity [196]; i.e., the movement of Cl−, Na+, K+ and water results in cell expansion (an increase in cell volume) with elevation of [Cl−]c (Fig. 1), which stimulates polymerization (elongation) of tubulin in high [Cl−]c areas (Fig. 4) [212] by inhibiting GTPase activity (see Fig. 2A and B-b). Through these processes, cells migrate toward the front. On the one hand, KCC, volume-regulated anion channel (VRAC), Ca2+-activated K+ channel (K+Ca 3.1) and AQP are expressed at the tail end of cell migration and excretes Cl− along with K+ to the extracellular space [197, 212]. Water efflux to the extracellular space via AQP is caused by a decrease in cytosolic osmolarity due to excretion of these ions; the movement of Cl−, K+ and water results in a decrease in cell volume with diminution of [Cl−]c (Fig. 1), which leads to depolymerization (shortening) of tubulin in low [Cl−]c areas (Fig. 4) [212] by activating GTPase (see Fig. 2A and B-c).
Roles of cytosolic Cl−, ion transporters and ion/water channels in cell migration. When cells migrate, cells need to change cell shape. Na+-K+-2Cl− cotransporter 1 (NKCC1) and aquaporin (AQP) are expressed on the migrating side membrane. NKCC1 is involved in Cl− uptake into the cytosolic space with Na+ and K+ [197, 209,210,211,212]. The uptake of these ions results in an influx of water into the cytosolic space via AQP through an increase in cytosolic osmolarity [196]. The movement of Cl−, Na+, K+ and water causes an increase in cell volume accompanied with [Cl−]c elevation, which promotes tubulin polymerization (elongation) [212] by inhibiting GTPase activity (see Fig. 2B). Similar to tubulin polymerization, actin monomers are enhanced to be polymerized. Then, cells migrate via these processes. On the one hand, K+-Cl− cotransporter (KCC), volume-regulated anion channel (VRAC), Ca2+-activated K+ channel (K+Ca3.1) and AQP are expressed on the tail end membrane of cell migration and excretes Cl− with K+ to the extracellular space via KCC, VRAC and K+Ca3.1 [197, 212]. Water efflux to the extracellular space via AQP is caused by a decrease in cytosolic osmolarity due to excretion of these ions. The movement of Cl−, K+ and water results in a decrease in cell volume accompanied with [Cl−]c diminution, which leads to tubulin depolymerization (shortening) at the tail end of the cell migration [212] by activating GTPase (see Fig. 2C). WNK activated by lowered [Cl−]c induces phosphorylation (activation) of OSR1/SPACK, which increases activity of NKCC1 by phosphorylating NKCC1 [208]. Thus, WNK is importantly involved in cell migration [208]
Roles of Cl− in regulation of epithelial Na+ transport
Dinudom and Cook et al. [38, 39] have reported that as [Cl−]c rises from 5 to 150 mM, the amplitude of the inward Na+ current declines via G protein Gi and Go subclasses-mediated pathways by applying whole-cell patch-clamp techniques to the cells of the intralobular ducts of the mandibular glands of mice. Tohda et al. [49] have also reported that reduction in [Cl−]c caused by activation of Ca2+-activated K+ channels and cAMP-activated Cl− channels (see Fig. 1) increases the open probability (Po) of amiloride-sensitive Na+-permeable channels in lung epithelial cells treated with ß2 agonist by using patch clamp single channel recording and single cell imaging techniques. Further, the reduction in [Cl−]c caused by ß2 agonist has been reported to play an essentially important role in activation of amiloride-sensitive Na+-permeable channels in lung epithelial cells treated with ß2 agonist [213], suggesting that the cytosolic Cl− decreases the activity of amiloride-sensitive Na+-permeable channels in lung epithelial cells treated with ß2 agonist. A molecular model of the cytosolic Cl−-induced inhibition on amiloride-sensitive Na+ channels in ß2-agonist-treated lung epithelial cells has been proposed [214]. These reports [49, 214, 215] indicate that Cl− has physiologically important roles in epithelial Na+ transport. On the one hand, using single channel recording techniques, Yamada et al. [215] have reported that lowering pipette (extracellular) Cl− concentration decreases the Po of single ENaC expressed on the apical membrane of renal cells treated with arginine vasotocin (AVT) to 0.23 ± 0.02 from 0.30 ± 0.02 associated with a significant decrease in the open time from 0.78 ± 0.03 to 0.61 ± 0.02 s without any significant change in the closed time. Further, the activity of the Na+-K+ pump has been reported to depend on the Cl− conductance of the membrane on which the Na+-K+ pump is expressed [44], and this Cl− conductance-dependent Na+-K+ pump activity is regulated via PTK activity [44].
Expression of ENaC mRNA is also regulated by cytosolic Cl− [40,41,42,43]. Activation of Na+-K+-2Cl− cotransporter (NKCC) by flavonoids such as apigenin and quercetin or diminution of Cl− efflux by Cl− channel blockers such as (5-Nitro-2-(3-phenylpropylamino)benzoic acid (NPPB) diminishes mRNA expression of ENaC in renal epithelial cells via elevation of [Cl−]c. [40,41,42,43,44,45,46,47,48,49]. Further, hypotonicity applied to ENaC-expressed renal cells elevates mRNA expression of ENaC in renal epithelial cells via diminution of [Cl−]c by activating p38 MAPK and inducing MKP-1-mediated suppression of ERK [42, 43]. The hypotonicity-induced activation of p38 MAPK and suppression of ERK via MKP-1 would be mediated at least partially by the hypotonicity-induced decrease in [Cl−]c [66, 88, 203].
Relationship between roles of Cl− and H+ in body functions
pH is lowered by H+ and CO2 produced in metabolic cells such as myocytes, neurons, etc., H+ is produced via glycolysis, and also from CO2 (CO2 ↔ H+ + HCO3−) via TCA cycle in mitochondria: the produced H+ plays various important roles in cellular functions [201, 217,218,219,220,221,222,223,224,225,226,227,228,229,230,231,232,233,234,235,236,237]. Lowered pH disturbs various body functions such as appearance of insulin resistance, enhancement of cancer metastasis and elevation of amyloid-ß production [201, 217,218,219,220,221,222,223,224,225,226,227,228,229,230,231,232,233,234,235]. In peripheral tissues, CO2 produced by metabolic cells moves to capillary erythrocytes, where CO2 is converted to H+ and HCO3− via a carbonic anhydrase (CA)-facilitated process. H+ binds to Hb in erythrocytes, while HCO3− is exchanged for blood extracellular Cl− (outside erythrocytes) by anion exchanger (AE; Cl−/HCO3− exchanger), and is excreted out of erythrocytes; this Cl− movement is the so-called ‘Cl− shift’ (Fig. 5). Thus, the extracellular Cl− concentration in veins is lower than that in arteries. These phenomena mean that the serum Cl− concentration in veins would be an indicator of metabolic status and mitochondrial function. Although the serum HCO3− concentration is a more direct indicator than the serum Cl− concentration, the process of accurately measuring the serum HCO3− concentration is clinically cumbersome and it is not practical to easily measure the serum HCO3− concentration in many humans. In fact, the venous serum Cl− concentration has been reported to be an indicator of metabolic status and mitochondrial function in analysis of over 100,000 healthy humans [237]. It is interesting to note that in ‘healthy’ individuals, the venous Cl− concentration increases with age, whereas the venous serum Cl− concentration decreases with increasing fasting blood glucose (sugar: FBS) and HbA1c [237]. These phenomena suggest that in ‘healthy’ individuals aging diminishes mitochondrial function (lowering CO2 production, and leading to lower the venous serum HCO3− concentration coupled with a higher venous serum Cl− concentration [237] (Fig. 5A-a for younger persons and Fig. 5A-b for older persons); furthermore, ‘healthy’ individuals with high FBS and HbA1c levels may have higher intracellular glucose concentrations and consequently higher mitochondrial CO2 production, leading to elevate the venous serum HCO3− concentration coupled with a lower venous serum Cl− concentration [237] (Fig. 5B). Measuring changes in the venous serum Cl− concentration may provide a simple way to identify the aerobic metabolism status and mitochondrial function, although more direct evidence is needed to conclude this.
Aging- and FBS-dependent regulatory mechanisms of body fluid pH via transporting systems of Cl− and HCO3−. A Age effects on venous serum Cl− concentration ([Cl−]s). a Younger persons with normal mitochondrial function. Glucose is metabolized into pyruvic acid, and then CO2 is produced from the pyruvic acid in mitochondria with normal function. The produced CO2 moves into erythrocytes, and is converted into H+ and HCO3− via a CA-facilitated process. The HCO3− is exchanged with serum Cl− via a Cl−/HCO3 anion exchanger (AE). These processes lead to low [Cl−]s. b Older persons with low mitochondrial function. The amount of CO2 produced in mitochondria becomes low due to low mitochondrial function. Thus, the amount of H+ and HCO3− produced from CO2 becomes low. These processes keep high [Cl−]s. B FBS/HbA1c effects on [Cl−]s. with normal mitochondrial function. Glucose is metabolized into pyruvic acid, and then CO2 is produced from the pyruvic acid in mitochondria with normal function. The produced CO2 moves into erythrocytes, and is converted into H+ and HCO3− via a CA-facilitated process. The HCO3− is exchanged with serum Cl− via a Cl−/HCO3 anion exchanger (AE). In cases of high FBS/HBA1c with normal mitochondrial function, large amounts of CO2 are produced, resulting in production of large amounts of HCO3−. These processes lead to low [Cl−]s. Figure 5 has been originally published in Marunaka et. al. (2021) Int J Mol Sci 22:11111 [237] under a Creative Commons Attribution-NonCommercial 4.0 International License
Cl− is also responsible for acidification of the lumen of endosomes and lysosomes through the function of the Cl−/H+ exchange system [238,239,240]. The acidity of endosomal and lysosomal lumens is involved in a cellular recycling process called autophagy in various cell types [29, 30, 241]. For example, defects in microglial lysosomal acidification lead to impaired autophagy and phagocytosis, causing progressive neurodegeneration and persistent neuroinflammation [241]. Furthermore, autophagy has been reported to decrease with age, and this decrease plays an important role in both the development of age-related diseases and physiological aging [242]. Thus, Cl− plays a key role in autophagy, degeneration, inflammation and aging via acidification of endosomal and lysosomal lumens [242].
Conclusion
Cl− plays an important role in maintaining electrical neutrality by being transported as counter ions when cations such as Na+ and K+ are transported. However, little is known about the physiological roles of Cl− other than maintaining electroneutrality. As described in this review article, cytosolic Cl− is an important factor in the regulation of biological functions, possessing various physiological activities. I would like to conclude this review with my sincere hope that the recognition that Cl− itself is an important regulator of various enzymatic activities will spread beyond its significance in maintaining the electroneutrality during cations movements, and that further research on the physiological roles of Cl− will progress.
Availability of data and materials
The data underlying this article will be obtained via PubMed and Google Scholar.
References
Marunaka Y (1997) Hormonal and osmotic regulation of NaCl transport in renal distal nephron epithelium. Jpn J Physiol 47:499–511. https://doi.org/10.2170/jjphysiol.47.499
Vardi N, Zhang LL, Payne JA, Sterling P (2000) Evidence that different cation chloride cotransporters in retinal neurons allow opposite responses to GABA. J Neurosci 20:7657–7663. https://doi.org/10.1523/jneurosci.20-20-07657.2000
Grob M, Mouginot D (2005) Heterogeneous chloride homeostasis and GABA responses in the median preoptic nucleus of the rat. J Physiol 569:885–901. https://doi.org/10.1113/jphysiol.2005.095794
Brumback AC, Staley KJ (2008) Thermodynamic regulation of NKCC1-mediated Cl- cotransport underlies plasticity of GABAA signaling in neonatal neurons. J Neurosci 28:1301–1312. https://doi.org/10.1523/jneurosci.3378-07.2008
Fernandez-Abascal J, Graziano B, Encalada N, Bianchi L (2021) Glial chloride channels in the function of the nervous system across species. Adv Exp Med Biol 1349:195–223. https://doi.org/10.1007/978-981-16-4254-8_10
Kuwahara A, Kuwahara Y, Inui T, Marunaka Y (2018) Regulation of ion transport in the intestine by free fatty acid receptor 2 and 3: possible involvement of the diffuse chemosensory system. Int J Mol Sci 19:735. https://doi.org/10.3390/ijms19030735
Kuwahara A, Kuwahara Y, Kato I, Kawaguchi K, Harata D, Asano S, Inui T, Marunaka Y (2019) Xenin-25 induces anion secretion by activating noncholinergic secretomotor neurons in the rat ileum. Am J Physiol Gastrointest Liver Physiol 316:G785–G796. https://doi.org/10.1152/ajpgi.00333.2018
Kuwahara Y, Kato I, Inui T, Marunaka Y, Kuwahara A (2021) The effect of Xenin25 on spontaneous circular muscle contractions of rat distal colon in vitro. Physiol Rep 9:e14752. https://doi.org/10.14814/phy2.14752
Kuwahara Y, Takahashi K, Akai M, Kato I, Kozakai T, Asano S, Inui T, Marunaka Y, Kuwahara A (2022) Minimum biological domain of xenin-25 required to induce anion secretion in the rat ileum. Peptides 147:170680. https://doi.org/10.1016/j.peptides.2021.170680
Takahashi K, Kuwahara Y, Kato I, Asano S, Kozakai T, Marunaka Y, Kuwahara A (2022) Secondary bile acid lithocholic acid attenuates neurally evoked ion transport in the rat distal colon. Biomed Res 43:223–239. https://doi.org/10.2220/biomedres.43.223
Marunaka Y (2014) Characteristics and pharmacological regulation of epithelial Na+ channel (ENaC) and epithelial Na+ transport. J Pharmacol Sci 126:21–36. https://doi.org/10.1254/jphs.14R01SR
Zheng S, Krump NA, McKenna MM, Li YH, Hannemann A, Garrett LJ, Gibson JS, Bodine DM, Low PS (2019) Regulation of erythrocyte Na+/K+/2Cl- cotransport by an oxygen-switched kinase cascade. J Biol Chem 294:2519–2528. https://doi.org/10.1074/jbc.RA118.006393
Cabrini G, Rimessi A, Borgatti M, Pinton P, Gambari R (2022) Overview of CF lung pathophysiology. Curr Opin Pharmacol 64:102214. https://doi.org/10.1016/j.coph.2022.102214
Sinha M, Zabini D, Guntur D, Nagaraj C, Enyedi P, Olschewski H, Kuebler WM, Olschewski A (2022) Chloride channels in the lung: challenges and perspectives for viral infections, pulmonary arterial hypertension, and cystic fibrosis. Pharmacol Ther 237:108249. https://doi.org/10.1016/j.pharmthera.2022.108249
Niisato N, Marunaka Y (2022) Ion transport: Calcium channels, 2nd edn. Elsevier, Amsterdam
Putman MS, Norris AW, Hull RL, Rickels MR, Sussel L, Blackman SM, Chan CL, Ode KL, Daley T, Stecenko AA, Moran A, Helmick MJ, Cray S, Alvarez JA, Stallings VA, Tuggle KL, Clancy JP, Eggerman TL, Engelhardt JF, Kelly A (2023) Cystic fibrosis-related diabetes workshop: Research priorities spanning disease pathophysiology, diagnosis, and outcomes. Diabetes 72:677–689. https://doi.org/10.2337/db22-0949
Raymond CM, Gaul SP, Han S, Huang G, Dong J (2023) Variability of clinical presentation in patients heterozygous for the F508del cystic fibrosis variant: A series of three cases and a review of the literature. Cureus 15:e40185. https://doi.org/10.7759/cureus.40185
Costaguta G, Patey N, Álvarez F (2023) Cystic fibrosis liver disease in children - A review of our current understanding. Arch Argent Pediatr 121:e202202905. https://doi.org/10.5546/aap.2022-02905.eng
Riordan JR, Rommens JM, Kerem B, Alon N, Rozmahel R, Grzelczak Z, Zielenski J, Lok S, Plavsic N, Chou JL, Drumm ML, Iannuzzi MC, Collins FS, Tsui LC (1989) Identification of the cystic fibrosis gene: cloning and characterization of complementary DNA. Science 245:1066–1073. https://doi.org/10.1126/science.2475911
Csanády L, Vergani P, Gadsby DC (2019) Structure, gating, and regulation of the CFTR anion channel. Physiol Rev 99:707–738. https://doi.org/10.1152/physrev.00007.2018
Nakajima K, Niisato N, Marunaka Y (2012) Enhancement of tubulin polymerization by Cl–induced blockade of intrinsic GTPase. Biochem Biophys Res Commun 425:225–229. https://doi.org/10.1016/j.bbrc.2012.07.072
André S, Boukhaddaoui H, Campo B, Al-Jumaily M, Mayeux V, Greuet D, Valmier J, Scamps F (2003) Axotomy-induced expression of calcium-activated chloride current in subpopulations of mouse dorsal root ganglion neurons. J Neurophysiol 90:3764–3773. https://doi.org/10.1152/jn.00449.2003
Lee EL, Shimizu T, Ise T, Numata T, Kohno K, Okada Y (2007) Impaired activity of volume-sensitive Cl- channel is involved in cisplatin resistance of cancer cells. J Cell Physiol 211:513–521. https://doi.org/10.1002/jcp.20961
Chen Q, Liu X, Luo Z, Wang S, Lin J, Xie Z, Li M, Li C, Cao H, Huang Q, Mao J, Xu B (2019) Chloride channel-3 mediates multidrug resistance of cancer by upregulating P-glycoprotein expression. J Cell Physiol 234:6611–6623. https://doi.org/10.1002/jcp.27402
Wilczyński B, Dąbrowska A, Saczko J, Kulbacka J (2021) The role of chloride channels in the multidrug resistance. Membranes (Basel) 12:38. https://doi.org/10.3390/membranes12010038
Maeno E, Ishizaki Y, Kanaseki T, Hazama A, Okada Y (2000) Normotonic cell shrinkage because of disordered volume regulation is an early prerequisite to apoptosis. Proc Natl Acad Sci USA 97:9487–9492. https://doi.org/10.1073/pnas.140216197
Okada Y, Okada T, Sato-Numata K, Islam MR, Ando-Akatsuka Y, Numata T, Kubo M, Shimizu T, Kurbannazarova RS, Marunaka Y, Sabirov RZ (2019) Cell volume-activated and volume-correlated anion channels in mammalian cells: Their biophysical, molecular, and pharmacological properties. Pharmacol Rev 71:49–88. https://doi.org/10.1124/pr.118.015917
Hazama A, Okada Y (1988) Ca2+ sensitivity of volume-regulatory K+ and Cl- channels in cultured human epithelial cells. J Physiol 402:687–702. https://doi.org/10.1113/jphysiol.1988.sp017229
Wartosch L, Fuhrmann JC, Schweizer M, Stauber T, Jentsch TJ (2009) Lysosomal degradation of endocytosed proteins depends on the chloride transport protein ClC-7. FASEB J 23:4056–4068. https://doi.org/10.1096/fj.09-130880
Wartosch L, Stauber T (2010) A role for chloride transport in lysosomal protein degradation. Autophagy 6:158–159. https://doi.org/10.4161/auto.6.1.10590
Shiozaki A, Miyazaki H, Niisato N, Nakahari T, Iwasaki Y, Itoi H, Ueda Y, Yamagishi H, Marunaka Y (2006) Furosemide, a blocker of Na+/K+/2Cl- cotransporter, diminishes proliferation of poorly differentiated human gastric cancer cells by affecting G0/G1 state. J Physiol Sci 56:401–406. https://doi.org/10.2170/physiolsci.RP010806
Inui T-A, Yasuda M, Hirano S, Ikeuchi Y, Kogiso H, Inui T, Marunaka Y, Nakahari T (2018) Daidzein-stimulated increase in the ciliary beating amplitude via an [Cl-]i decrease in ciliated human nasal epithelial cells. Int J Mol Sci 19:3754. https://doi.org/10.3390/ijms19123754
Ikeuchi Y, Kogiso H, Hosogi S, Tanaka S, Shimamoto C, Matsumura H, Inui T, Marunaka Y, Nakahari T (2019) Carbocisteine stimulated an increase in ciliary bend angle via a decrease in [Cl-]i in mouse airway cilia. Pflüg Arch 471:365–380. https://doi.org/10.1007/s00424-018-2212-2
Inui TA, Yasuda M, Hirano S, Ikeuchi Y, Kogiso H, Inui T, Marunaka Y, Nakahari T (2020) Enhancement of ciliary beat amplitude by carbocisteine in ciliated human nasal epithelial cells. Laryngoscope 130:E289–E297. https://doi.org/10.1002/lary.28185
Atsumi N, Yasumatsu K, Takashina Y, Ito C, Yasui N, Margolskee RF, Yamashita A (2023) Chloride ions evoke taste sensations by binding to the extracellular ligand-binding domain of sweet/umami taste receptors. Elife 12:e84291. https://doi.org/10.7554/eLife.84291
Taruno A, Gordon MD (2023) Molecular and cellular mechanisms of salt taste. Annu Rev Physiol 85:25–45. https://doi.org/10.1146/annurev-physiol-031522-075853
Wu Y, Schellinger JN, Huang CL, Rodan AR (2014) Hypotonicity stimulates potassium flux through the WNK-SPAK/OSR1 kinase cascade and the Ncc69 sodium-potassium-2-chloride cotransporter in the Drosophila renal tubule. J Biol Chem 289:26131–26142. https://doi.org/10.1074/jbc.M114.577767
Dinudom A, Young JA, Cook DI (1993) Na+ and Cl- conductances are controlled by cytosolic Cl- concentration in the intralobular duct cells of mouse mandibular glands. J Membr Biol 135:289–295. https://doi.org/10.1007/bf00211100
Cook DI, Dinudom A, Komwatana P, Young JA (1998) Control of Na+ transport in salivary duct epithelial cells by cytosolic Cl- and Na+. Eur J Morphol 36:67–73
Niisato N, Eaton DC, Marunaka Y (2004) Involvement of cytosolic Cl- in osmoregulation of alpha-ENaC gene expression. Am J Physiol Renal Physiol 287:F932–F399. https://doi.org/10.1152/ajprenal.00131.2004
Fujimoto S, Niisato N, Sugimoto T, Marunaka Y (2005) Quercetin and NPPB-induced diminution of aldosterone action on Na+ absorption and ENaC expression in renal epithelium. Biochem Biophys Res Commun 336:401–407. https://doi.org/10.1016/j.bbrc.2005.08.096
Niisato N, Taruno A, Marunaka Y (2007) Involvement of p38 MAPK in hypotonic stress-induced stimulation of β- and γ-ENaC expression in renal epithelium. Biochem Biophys Res Commun 358:819–824. https://doi.org/10.1016/j.bbrc.2007.04.192
Niisato N, Ohta M, Eaton DC, Marunaka Y (2012) Hypotonic stress upregulates beta- and gamma-ENaC expression through suppression of ERK by inducing MKP-1. Am J Physiol Renal Physiol 303:F240-252. https://doi.org/10.1152/ajprenal.00198.2011
Niisato N, Marunaka Y (1999) Activation of the Na+-K+ pump by hyposmolality through tyrosine kinase-dependent Cl- conductance in Xenopus renal epithelial A6 cells. J Physiol 518:417–432. https://doi.org/10.1111/j.1469-7793.1999.0417p.x
Kitahara S, Fox KR, Hogben CA (1967) Depression of chloride transport by carbonic anhydrase inhibitors in the absence of carbonic anhydrase. Nature 214:836–837. https://doi.org/10.1038/214836a0
Cousin JL, Motais R, Sola F (1975) Transmembrane exchange of chloride with bicarbonate ion in mammalian red blood cells: evidence for a sulphonamide-sensitive “carrier.” J Physiol 253:385–399. https://doi.org/10.1113/jphysiol.1975.sp011195
Gunn RB, Dalmark M, Tosteson DC, Wieth JO (1973) Characteristics of chloride transport in human red blood cells. J Gen Physiol 61:185–206. https://doi.org/10.1085/jgp.61.2.185
Tanaka S, Miyazaki H, Shiozaki A, Ichikawa D, Otsuji E, Marunaka Y (2017) Cytosolic Cl- affects the anticancer activity of paclitaxel in the gastric cancer cell line, MKN28 cell. Cell Physiol Biochem 42:68–80. https://doi.org/10.1159/000477116
Tohda H, Foskett JK, O’Brodovich H, Marunaka Y (1994) Cl- regulation of a Ca2+ activated non selective cation channel in beta-agonist-treated fetal distal lung epithelium. Am J Physiol 266:C104–C109. https://doi.org/10.1152/ajpcell.1994.266.1.C104
Ikeuchi Y, Kogiso H, Hosogi S, Tanaka S, Shimamoto C, Inui T, Nakahari T, Marunaka Y (2018) Measurement of [Cl-]i unaffected by the cell volume change using MQAE-based two-photon microscopy in airway ciliary cells of mice. J Physiol Sci 68:191–199. https://doi.org/10.1007/s12576-018-0591-y
Untiet V, Moeller LM, Ibarra-Soria X, Sanchez-Andrade G, Stricker M, Neuhaus EM, Logan DW, Gensch T, Spehr M (2016) Elevated cytosolic Cl− concentrations in dendritic knobs of mouse vomeronasal sensory neurons. Chem Senses 41:669–676. https://doi.org/10.1093/chemse/bjw077
Staley KJ, Soldo BL, Proctor WR (1995) Ionic mechanisms of neuronal excitation by inhibitory GABAA receptors. Science 269:977–981. https://doi.org/10.1126/science.7638623
Thompson SM, Gähwiler BH (1989) Activity-dependent disinhibition. I. Repetitive stimulation reduces IPSP driving force and conductance in the hippocampus in vitro. J Neurophysiol 61:501–511. https://doi.org/10.1152/jn.1989.61.3.501
Bekar LK, Walz W (2002) Intracellular chloride modulates A-type potassium currents in astrocytes. Glia 39:207–216. https://doi.org/10.1002/glia.10096
Bevensee MO, Apkon M, Boron WF (1997) Intracellular pH regulation in cultured astrocytes from rat hippocampus. II. Electrogenic Na/HCO3 cotransport. J Gen Physiol 110:467–483. https://doi.org/10.1085/jgp.110.4.467
Kettenmann H, Backus KH, Schachner M (1987) γ-Aminobutyric acid opens Cl-channels in cultured astrocytes. Brain Res 404:1–9. https://doi.org/10.1016/0006-8993(87)91349-7
Smith QR, Johanson CE, Woodbury DM (1981) Uptake of 36Cl and 22Na by the brain-cerebrospinal fluid system: comparison of the permeability of the blood-brain and blood-cerebrospinal fluid barriers. J Neurochem 37:117–124. https://doi.org/10.1111/j.1471-4159.1981.tb05298.x
Walz W, Mukerji S (1988) KCl movements during potassium-induced cytotoxic swelling of cultured astrocytes. Exp Neurol 99:17–29. https://doi.org/10.1016/0014-4886(88)90123-9
Untiet V, Kovermann P, Gerkau NJ, Gensch T, Rose CR, Fahlke C (2017) Glutamate transporter-associated anion channels adjust intracellular chloride concentrations during glial maturation. Glia 65:388–400. https://doi.org/10.1002/glia.23098
Engels M, Kalia M, Rahmati S, Petersilie L, Kovermann P, van Putten M, Rose CR, Meijer HGE, Gensch T, Fahlke C (2021) Glial Chloride Homeostasis Under Transient Ischemic Stress. Front Cell Neurosci 15:735300. https://doi.org/10.3389/fncel.2021.735300
Nakajima KI, Marunaka Y (2016) Intracellular chloride ion concentration in differentiating neuronal cell and its role in growing neurite. Biochem Biophys Res Commun 479:338–342. https://doi.org/10.1016/j.bbrc.2016.09.075
Pressey JC, de Saint-Rome M, Raveendran VA, Woodin MA (2023) Chloride transporters controlling neuronal excitability. Physiol Rev 103:1095–1135. https://doi.org/10.1152/physrev.00025.2021
Talifu Z, Pan Y, Gong H, Xu X, Zhang C, Yang D, Gao F, Yu Y, Du L, Li J (2022) The role of KCC2 and NKCC1 in spinal cord injury: from physiology to pathology. Front Physiol 13:1045520. https://doi.org/10.3389/fphys.2022.1045520
Garneau AP, Slimani S, Haydock L, Nsimba-Batomene TR, Préfontaine FCM, Lavoie MM, Tremblay LE, Fiola MJ, Mac-Way F, Isenring P (2022) Molecular mechanisms, physiological roles, and therapeutic implications of ion fluxes in bone cells: emphasis on the cation-Cl- cotransporters. J Cell Physiol 237:4356–4368. https://doi.org/10.1002/jcp.30879
Liang L, Shimosawa T (2022) Molecular mechanisms of Na-Cl cotransporter in relation to hypertension in chronic kidney disease. Int J Mol Sci 24:286. https://doi.org/10.3390/ijms24010286
Marunaka Y (2017) Actions of quercetin, a flavonoid, on ion transporters: its physiological roles. Ann NY Acad Sci 1398:142–151. https://doi.org/10.1111/nyas.13361
Fukuda A, Mody I, Prince DA (1993) Differential ontogenesis of presynaptic and postsynaptic GABAB inhibition in rat somatosensory cortex. J Neurophysiol 70:448–452. https://doi.org/10.1152/jn.1993.70.1.448
Fukuda A, Muramatsu K, Okabe A, Shimano Y, Hida H, Fujimoto I, Nishino H (1998) Changes in intracellular Ca2+ induced by GABAA receptor activation and reduction in Cl- gradient in neonatal rat neocortex. J Neurophysiol 79:439–446. https://doi.org/10.1152/jn.1998.79.1.439
Yamada J, Okabe A, Toyoda H, Kilb W, Luhmann HJ, Fukuda A (2004) Cl- uptake promoting depolarizing GABA actions in immature rat neocortical neurones is mediated by NKCC1. J Physiol 557:829–841. https://doi.org/10.1113/jphysiol.2004.062471
Ito S (2016) GABA and glycine in the developing brain. J Physiol Sci 66:375–379. https://doi.org/10.1007/s12576-016-0442-7
Gascoigne DA, Serdyukova NA, Aksenov DP (2021) Early development of the GABAergic system and the associated risks of neonatal anesthesia. Int J Mol Sci 22:12951. https://doi.org/10.3390/ijms222312951
Nakanishi K, Yamada J, Takayama C, Oohira A, Fukuda A (2007) NKCC1 activity modulates formation of functional inhibitory synapses in cultured neocortical neurons. Synapse 61:138–149. https://doi.org/10.1002/syn.20352
Shimizu-Okabe C, Okabe A, Kilb W, Sato K, Luhmann HJ, Fukuda A (2007) Changes in the expression of cation-Cl- cotransporters, NKCC1 and KCC2, during cortical malformation induced by neonatal freeze-lesion. Neurosci Res 59:288–295. https://doi.org/10.1016/j.neures.2007.07.010
Egawa K, Fukuda A (2013) Pathophysiological power of improper tonic GABAA conductances in mature and immature models. Front Neural Circuits 7:170. https://doi.org/10.3389/fncir.2013.00170
Kanaka C, Ohno K, Okabe A, Kuriyama K, Itoh T, Fukuda A, Sato K (2001) The differential expression patterns of messenger RNAs encoding K-Cl cotransporters (KCC1,2) and Na-K-2Cl cotransporter (NKCC1) in the rat nervous system. Neuroscience 104:933–946. https://doi.org/10.1016/s0306-4522(01)00149-x
Heck N, Kilb W, Reiprich P, Kubota H, Furukawa T, Fukuda A, Luhmann HJ (2007) GABA-A receptors regulate neocortical neuronal migration in vitro and in vivo. Cereb Cortex 17:138–148. https://doi.org/10.1093/cercor/bhj135
Furukawa T, Yamada J, Akita T, Matsushima Y, Yanagawa Y, Fukuda A (2014) Roles of taurine-mediated tonic GABAA receptor activation in the radial migration of neurons in the fetal mouse cerebral cortex. Front Cell Neurosci 8:88. https://doi.org/10.3389/fncel.2014.00088
Luhmann HJ, Fukuda A, Kilb W (2015) Control of cortical neuronal migration by glutamate and GABA. Front Cell Neurosci 9:4. https://doi.org/10.3389/fncel.2015.00004
Watanabe M, Fukuda A (2015) Development and regulation of chloride homeostasis in the central nervous system. Front Cell Neurosci 9:371. https://doi.org/10.3389/fncel.2015.00371
Kilb W, Fukuda A (2017) Taurine as an essential neuromodulator during perinatal cortical development. Front Cell Neurosci 11:328. https://doi.org/10.3389/fncel.2017.00328
Fukuda A (2020) Chloride homeodynamics underlying modal shifts in cellular and network oscillations. Neurosci Res 156:14–23. https://doi.org/10.1016/j.neures.2020.02.010
Neuwirth LS, El Idrissi A, Fukuda A, Kilb W (2023) Editorial: The role of GABA-shift in neurodevelopment and psychiatric disorders. Front Mol Neurosci 16:1162689. https://doi.org/10.3389/fnmol.2023.1162689
Egawa K, Watanabe M, Shiraishi H, Sato D, Takahashi Y, Nishio S, Fukuda A (2023) Imbalanced expression of cation-chloride cotransporters as a potential therapeutic target in an Angelman syndrome mouse model. Sci Rep 13:5685. https://doi.org/10.1038/s41598-023-32376-z
Schappi JM, Krbanjevic A, Rasenick MM (2014) Tubulin, actin and heterotrimeric G proteins: coordination of signaling and structure. Biochim Biophys Acta 1838:674–681. https://doi.org/10.1016/j.bbamem.2013.08.026
Kristensson MA (2021) The game of tubulins Cells 10:745. https://doi.org/10.3390/cells10040745
Ilan Y (2023) Microtubules as a potential platform for energy transfer in biological systems: a target for implementing individualized, dynamic variability patterns to improve organ function. Mol Cell Biochem 478:375–392. https://doi.org/10.1007/s11010-022-04513-1
Atkins M, Nicol X, Fassier C (2023) Microtubule remodelling as a driving force of axon guidance and pruning. Semin Cell Dev Biol 140:35–53. https://doi.org/10.1016/j.semcdb.2022.05.030
Marunaka Y, Niisato N, Miyazaki H, Nakajima KI, Taruno A, Sun H, Marunaka R, Okui M, Yamamoto T, Kanamura N, Kogiso H, Ikeuchi Y, Kashio M, Hosogi S, Nakahari T (2018) Quercetin is a useful medicinal compound showing various actions including control of blood pressure, neurite elongation and epithelial ion transport. Curr Med Chem 25:4876–4887. https://doi.org/10.2174/0929867323666160919095043
Higashijima T, Ferguson KM, Sternweis PC (1987) Regulation of hormone-sensitive GTP-dependent regulatory proteins by chloride. J Biol Chem 262:3597–3602
Nakajima T, Sugimoto T, Kurachi Y (1992) Effects of anions on the G protein-mediated activation of the muscarinic K+ channel in the cardiac atrial cell membrane. Intracellular chloride inhibition of the GTPase activity of GK. J Gen Physiol 99:665–682. https://doi.org/10.1085/jgp.99.5.665
Horio T, Murata T (2014) The role of dynamic instability in microtubule organization. Front Plant Sci 5:511. https://doi.org/10.3389/fpls.2014.00511
Malacrida A, Semperboni S, Di Domizio A, Palmioli A, Broggi L, Airoldi C, Meregalli C, Cavaletti G, Nicolini G (2021) Tubulin binding potentially clears up Bortezomib and Carfilzomib differential neurotoxic effect. Sci Rep 11:10523. https://doi.org/10.1038/s41598-021-89856-3
Shemesh A, Ghareeb H, Dharan R, Levi-Kalisman Y, Metanis N, Ringel I, Raviv U (2023) Effect of tubulin self-association on GTP hydrolysis and nucleotide exchange reactions. Biochim Biophys Acta Proteins Proteom 1871:140869. https://doi.org/10.1016/j.bbapap.2022.140869
Moritz M, Braunfeld MB, Sedat JW, Alberts B, Agard DA (1995) Microtubule nucleation by gamma-tubulin-containing rings in the centrosome. Nature 378:638–640. https://doi.org/10.1038/378638a0
Wade RH, Hyman AA (1997) Microtubule structure and dynamics. Curr Opin Cell Biol 9:12–17. https://doi.org/10.1016/s0955-0674(97)80146-9
Liu G, Dwyer T (2014) Microtubule dynamics in axon guidance. Neurosci Bull 30:569–583. https://doi.org/10.1007/s12264-014-1444-6
Sk C, Gadewal N, Choudhary RK, Dasgupta D (2019) Insights into the flexibility of the T3 loop and GTPase activating protein (GAP) domain of dimeric α and β tubulins from a molecular dynamics perspective. Comput Biol Chem 82:37–43. https://doi.org/10.1016/j.compbiolchem.2019.06.006
Spiegelman BM, Penningroth SM, Kirschner MW (1977) Turnover of tubulin and the N site GTP in Chinese hamster ovary cells. Cell 12:587–600. https://doi.org/10.1016/0092-8674(77)90259-8
Peng N, Nakamura F (2023) Microtubule-associated proteins and enzymes modifying tubulin. Cytoskeleton (Hoboken) 80:60–76. https://doi.org/10.1002/cm.21748
Howes SC, Geyer EA, LaFrance B, Zhang R, Kellogg EH, Westermann S, Rice LM, Nogales E (2017) Structural differences between yeast and mammalian microtubules revealed by cryo-EM. J Cell Biol 216:2669–2677. https://doi.org/10.1083/jcb.201612195
Goodson HV, Jonasson EM (2018) Microtubules and microtubule-associated proteins. Cold Spring Harb Perspect Biol 10:a022608. https://doi.org/10.1101/cshperspect.a022608
Al-Bassam J, Chang F (2011) Regulation of microtubule dynamics by TOG-domain proteins XMAP215/Dis1 and CLASP. Trends Cell Biol 21:604–614. https://doi.org/10.1016/j.tcb.2011.06.007
Bera A, Gupta ML Jr (2022) Microtubules in microorganisms: How tubulin isotypes contribute to diverse cytoskeletal functions. Front Cell Dev Biol 10:913809. https://doi.org/10.3389/fcell.2022.913809
Anders KR, Botstein D (2001) Dominant-lethal α-tubulin mutants defective in microtubule depolymerization in yeast. Mol Biol Cell 12:3973–3986. https://doi.org/10.1091/mbc.12.12.3973
Weisenberg RC, Deery WJ, Dickinson PJ (1976) Tubulin-nucleotide interactions during the polymerization and depolymerization of microtubules. Biochemistry 15:4248–4254. https://doi.org/10.1021/bi00664a018
Amos L, Klug A (1974) Arrangement of subunits in flagellar microtubules. J Cell Sci 14:523–549. https://doi.org/10.1242/jcs.14.3.523
Wattanathamsan O, Pongrakhananon V (2023) Post-translational modifications of tubulin: their role in cancers and the regulation of signaling molecules. Cancer Gene Ther 30:521–528. https://doi.org/10.1038/s41417-021-00396-4
Akera T (2023) Tubulin post-translational modifications in meiosis. Semin Cell Dev Biol 137:38–45. https://doi.org/10.1016/j.semcdb.2021.11.014
Caporizzo MA, Prosser BL (2022) The microtubule cytoskeleton in cardiac mechanics and heart failure. Nat Rev Cardiol 19:364–378. https://doi.org/10.1038/s41569-022-00692-y
Nakajima K, Niisato N, Marunaka Y (2011) Quercetin stimulates NGF-induced neurite outgrowth in PC12 cells via activation of Na+/K+/2Cl- cotransporter. Cell Physiol Biochem 28:147–156. https://doi.org/10.1159/000331723
Nakajima K, Miyazaki H, Niisato N, Marunaka Y (2007) Essential role of NKCC1 in NGF-induced neurite outgrowth. Biochem Biophys Res Commun 359:604–610. https://doi.org/10.1016/j.bbrc.2007.05.133
Nakajima K, Niisato N, Marunaka Y (2011) Genistein enhances the NGF-induced neurite outgrowth. Biomed Res 32:351–356. https://doi.org/10.2220/biomedres.32.351
Nagao H, Nakajima K, Niisato N, Hirota R, Bando H, Sakaguchi H, Hisa Y, Marunaka Y (2012) K+-Cl- cotransporter 1 (KCC1) negatively regulates NGF-induced neurite outgrowth in PC12 cells. Cell Physiol Biochem 30:538–551. https://doi.org/10.1159/000341436
de Forges H, Bouissou A, Perez F (2012) Interplay between microtubule dynamics and intracellular organization. Int J Biochem Cell Biol 44:266–274. https://doi.org/10.1016/j.biocel.2011.11.009
Roychowdhury S, Rasenick MM (2008) Submembraneous microtubule cytoskeleton: regulation of microtubule assembly by heterotrimeric G proteins. FEBS J 275:4654–4663. https://doi.org/10.1111/j.1742-4658.2008.06614.x
Florian S, Mitchison TJ (2016) Anti-microtubule drugs. Methods Mol Biol 1413:403–421. https://doi.org/10.1007/978-1-4939-3542-0_25
Gupta R, Kadhim MM, Turki Jalil A, Qasim Alasheqi M, Alsaikhan F, Khalimovna Mukhamedova N, Alexis Ramírez-Coronel A, Hassan Jawhar Z, Ramaiah P, Najafi M (2023) The interactions of docetaxel with tumor microenvironment. Int Immunopharmacol 119:110214. https://doi.org/10.1016/j.intimp.2023.110214
Das T, Anand U, Pandey SK, Ashby CR Jr, Assaraf YG, Chen ZS, Dey A (2021) Therapeutic strategies to overcome taxane resistance in cancer. Drug Resist Updat 55:100754. https://doi.org/10.1016/j.drup.2021.100754
Naaz F, Haider MR, Shafi S, Yar MS (2019) Anti-tubulin agents of natural origin: Targeting taxol, vinca, and colchicine binding domains. Eur J Med Chem 171:310–331. https://doi.org/10.1016/j.ejmech.2019.03.025
Miyazaki H, Shiozaki A, Niisato N, Ohsawa R, Itoi H, Ueda Y, Otsuji E, Yamagishi H, Iwasaki Y, Nakano T, Nakahari T, Marunaka Y (2008) Chloride ions control the G1/S cell-cycle checkpoint by regulating the expression of p21 through a p53-independent pathway in human gastric cancer cells. Biochem Biophys Res Commun 366:506–512. https://doi.org/10.1016/j.bbrc.2007.11.144
Ohsawa R, Miyazaki H, Niisato N, Shiozaki A, Iwasaki Y, Otsuji E, Marunaka Y (2010) Intracellular chloride regulates cell proliferation through the activation of stress-activated protein kinases in MKN28 human gastric cancer cells. J Cell Physiol 223:764–770. https://doi.org/10.1002/jcp.22088
Hosogi S, Miyazaki H, Nakajima K, Ashihara E, Niisato N, Kusuzaki K, Marunaka Y (2012) An inhibitor of Na+/H+ exchanger (NHE), ethyl-isopropyl amiloride (EIPA), diminishes proliferation of MKN28 human gastric cancer cells by decreasing the cytosolic Cl- concentration via DIDS-sensitive pathways. Cell Physiol Biochem 30:1241–1253. https://doi.org/10.1159/000343315
Kitagawa M, Niisato N, Shiozaki A, Ohta-Fujimoto M, Hosogi S, Miyazaki H, Ichikawa D, Otsuji E, Marunaka Y (2013) A regulatory role of K+-Cl- cotransporter in the cell cycle progression of breast cancer MDA-MB-231 cells. Arch Biochem Biophys 539:92–98. https://doi.org/10.1016/j.abb.2013.06.014
Feng J, Peng Z, Gao L, Yang X, Sun Z, Hou X, Li E, Zhu L, Yang H (2021) ClC-3 promotes paclitaxel resistance via modulating tubulins polymerization in ovarian cancer cells. Biomed Pharmacother 138:111407. https://doi.org/10.1016/j.biopha.2021.111407
Yang X, Li C, Liao X, Liu S, Li X, Hou X, Wang K, Yang H, Gao L, Zhu L (2023) Paclitaxel induces pyroptosis by inhibiting the volume-sensitive chloride channel leucine-rich repeat-containing 8a in ovarian cancer cells. Oncol Rep 49:115. https://doi.org/10.3892/or.2023.8552
Brennan MA, Cookson BT (2000) Salmonella induces macrophage death by caspase-1-dependent necrosis. Mol Microbiol 38:31–40. https://doi.org/10.1046/j.1365-2958.2000.02103.x
Fink SL, Cookson BT (2005) Apoptosis, pyroptosis, and necrosis: mechanistic description of dead and dying eukaryotic cells. Infect Immun 73:1907–1916. https://doi.org/10.1128/iai.73.4.1907-1916.2005
Kroemer G, Galluzzi L, Vandenabeele P, Abrams J, Alnemri ES, Baehrecke EH, Blagosklonny MV, El-Deiry WS, Golstein P, Green DR, Hengartner M, Knight RA, Kumar S, Lipton SA, Malorni W, Nuñez G, Peter ME, Tschopp J, Yuan J, Piacentini M, Zhivotovsky B, Melino G (2009) Classification of cell death: recommendations of the Nomenclature Committee on Cell Death 2009. Cell Death Differ 16:3–11. https://doi.org/10.1038/cdd.2008.150
Wang D, Wan X (2023) Progress in the study of molecular mechanisms of cell pyroptosis in tumor therapy. Int Immunopharmacol 118:110143. https://doi.org/10.1016/j.intimp.2023.110143
Ouyang X, Zhou J, Lin L, Zhang Z, Luo S, Hu D (2023) Pyroptosis, inflammasome, and gasdermins in tumor immunity. Innate Immun 29:3–13. https://doi.org/10.1177/17534259221143216
Koumangoye R (2022) The role of Cl- and K+ efflux in NLRP3 inflammasome and innate immune response activation. Am J Physiol Cell Physiol 322:C645–C652. https://doi.org/10.1152/ajpcell.00421.2021
Mayes-Hopfinger L, Enache A, Xie J, Huang CL, Köchl R, Tybulewicz VLJ, Fernandes-Alnemri T, Alnemri ES (2021) Chloride sensing by WNK1 regulates NLRP3 inflammasome activation and pyroptosis. Nat Commun 12:4546. https://doi.org/10.1038/s41467-021-24784-4
Shimizu T, Numata T, Okada Y (2004) A role of reactive oxygen species in apoptotic activation of volume-sensitive Cl- channel. Proc Natl Acad Sci USA 101:6770–6773. https://doi.org/10.1073/pnas.0401604101
Kunzelmann K (2016) Ion channels in regulated cell death. Cell Mol Life Sci 73:2387–2403. https://doi.org/10.1007/s00018-016-2208-z
Daniels MJ, Rivers-Auty J, Schilling T, Spencer NG, Watremez W, Fasolino V, Booth SJ, White CS, Baldwin AG, Freeman S, Wong R, Latta C, Yu S, Jackson J, Fischer N, Koziel V, Pillot T, Bagnall J, Allan SM, Paszek P, Galea J, Harte MK, Eder C, Lawrence CB, Brough D (2016) Fenamate NSAIDs inhibit the NLRP3 inflammasome and protect against Alzheimer’s disease in rodent models. Nat Commun 7:12504. https://doi.org/10.1038/ncomms12504
Green JP, Yu S, Martín-Sánchez F, Pelegrin P, Lopez-Castejon G, Lawrence CB, Brough D (2018) Chloride regulates dynamic NLRP3-dependent ASC oligomerization and inflammasome priming. Proc Natl Acad Sci USA 115:E9371–E9380. https://doi.org/10.1073/pnas.1812744115
Ye X, Liu X, Wei W, Yu H, Jin X, Yu J, Li C, Xu B, Guo X, Mao J (2021) Volume-activated chloride channels contribute to lipopolysaccharide plus nigericin-induced pyroptosis in bone marrow-derived macrophages. Biochem Pharmacol 193:114791. https://doi.org/10.1016/j.bcp.2021.114791
Maki M, Miyazaki H, Nakajima K, Yamane J, Niisato N, Morihara T, Kubo T, Marunaka Y (2007) Chloride-dependent acceleration of cell cycle via modulation of Rb and cdc2 in osteoblastic cells. Biochem Biophys Res Commun 361:1038–1043. https://doi.org/10.1016/j.bbrc.2007.07.131
Shiozaki A, Otsuji E, Marunaka Y (2011) Intracellular chloride regulates the G1/S cell cycle progression in gastric cancer cells. World J Gastrointest Oncol 3:119–122. https://doi.org/10.4251/wjgo.v3.i8.119
Xu B, Mao J, Wang L, Zhu L, Li H, Wang W, Jin X, Zhu J, Chen L (2010) ClC-3 chloride channels are essential for cell proliferation and cell cycle progression in nasopharyngeal carcinoma cells. Acta Biochim Biophys Sin (Shanghai) 42:370–380. https://doi.org/10.1093/abbs/gmq031
Shiozaki A, Ichikawa D, Otsuji E, Marunaka Y (2014) Cellular physiological approach for treatment of gastric cancer. World J Gastroenterol 20:11560–11566. https://doi.org/10.3748/wjg.v20.i33.11560
Mitsuda M, Shiozaki A, Kudou M, Shimizu H, Arita T, Kosuga T, Konishi H, Komatsu S, Kubota T, Fujiwara H, Okamoto K, Kishimoto M, Konishi E, Otsuji E (2021) Functional analysis and clinical significance of chloride channel 2 expression in esophageal squamous cell carcinoma. Ann Surg Oncol 28:5384–5397. https://doi.org/10.1245/s10434-021-09659-8
Wang H, Wang T, Zhang Z, Fan Y, Zhang L, Gao K, Luo S, Xiao Q, Sun C (2021) Simvastatin inhibits oral squamous cell carcinoma by targeting TMEM16A Ca2+-activated chloride channel. J Cancer Res Clin Oncol 147:1699–1711. https://doi.org/10.1007/s00432-021-03575-w
Luo Y, Liu X, Li X, Zhong W, Lin J, Chen Q (2022) Identification and validation of a signature involving voltage-gated chloride ion channel genes for prediction of prostate cancer recurrence. Front Endocrinol (Lausanne) 13:1001634. https://doi.org/10.3389/fendo.2022.1001634
Shiozaki A, Nako Y, Ichikawa D, Konishi H, Komatsu S, Kubota T, Fujiwara H, Okamoto K, Kishimoto M, Marunaka Y, Otsuji E (2014) Role of the Na+/K+/2Cl- cotransporter NKCC1 in cell cycle progression in human esophageal squamous cell carcinoma. World J Gastroenterol 20:6844–6859. https://doi.org/10.3748/wjg.v20.i22.6844
Shiozaki A, Takemoto K, Ichikawa D, Fujiwara H, Konishi H, Kosuga T, Komatsu S, Okamoto K, Kishimoto M, Marunaka Y, Otsuji E (2014) The K-Cl cotransporter KCC3 as an independent prognostic factor in human esophageal squamous cell carcinoma. BioMed Res Int 2014:936401. https://doi.org/10.1155/2014/936401
Katsurahara K, Shiozaki A, Kosuga T, Kudou M, Shoda K, Arita T, Konishi H, Komatsu S, Kubota T, Fujiwara H, Okamoto K, Kishimoto M, Konishi E, Marunaka Y, Otsuji E (2020) ANO9 regulated cell cycle in human esophageal squamous cell carcinoma. Ann Surg Oncol 27:3218–3230. https://doi.org/10.1245/s10434-020-08368-y
Iitaka D, Shiozaki A, Ichikawa D, Kosuga T, Komatsu S, Okamoto K, Fujiwara H, Ishii H, Nakahari T, Marunaka Y, Otsuji E (2012) Blockade of chloride ion transport enhances the cytocidal effect of hypotonic solution in gastric cancer cells. J Surg Res 176:524–534. https://doi.org/10.1016/j.jss.2011.10.039
Kosuga T, Shiozaki A, Ichikawa D, Fujiwara H, Komatsu S, Iitaka D, Tsujiura M, Morimura R, Takeshita H, Nagata H, Okamoto K, Nakahari T, Marunaka Y, Otsuji E (2011) Pleural lavage with distilled water during surgery for esophageal squamous cell carcinoma. Oncol Rep 26:577–586. https://doi.org/10.3892/or.2011.1307
Nako Y, Shiozaki A, Ichikawa D, Komatsu S, Konishi H, Iitaka D, Ishii H, Ikoma H, Kubota T, Fujiwara H, Okamoto K, Ochiai T, Nakahari T, Marunaka Y, Otsuji E (2012) Enhancement of the cytocidal effects of hypotonic solution using a chloride channel blocker in pancreatic cancer cells. Pancreatology 12:440–448. https://doi.org/10.1016/j.pan.2012.08.003
Shiozaki A, Marunaka Y, Otsuji E (2021) Roles of ion and water channels in the cell death and survival of upper gastrointestinal tract cancers. Front Cell Dev Biol 9:616933. https://doi.org/10.3389/fcell.2021.616933
Engeland K (2022) Cell cycle regulation: p53–p21-RB signaling. Cell Death Differ 29:946–960. https://doi.org/10.1038/s41418-022-00988-z
Kobayashi T, Shiozaki A, Nako Y, Ichikawa D, Kosuga T, Shoda K, Arita T, Konishi H, Komatsu S, Kubota T, Fujiwara H, Okamoto K, Kishimoto M, Konishi E, Marunaka Y, Otsuji E (2018) Chloride intracellular channel 1 as a switch among tumor behaviors in human esophageal squamous cell carcinoma. Oncotarget 9:23237–23252. https://doi.org/10.1863/oncotarget.25296
Dai X, Li J, Hu X, Ye J, Cai W (2022) SLC26A4 mutation promotes cell apoptosis by inducing pendrin transfer, reducing Cl- transport, and inhibiting PI3K/Akt/mTOR pathway. Biomed Res Int 2022:6496799. https://doi.org/10.1155/2022/6496799
Geng H, Feng C, Sun Z, Fan X, Xie Y, Gu J, Fan L, Liu G, Li C, Thorne RF, Zhang XD, Li X, Liu X (2023) Chloride intracellular channel 1 promotes esophageal squamous cell carcinoma proliferation via mTOR signalling. Transl Oncol 27:101560. https://doi.org/10.1016/j.tranon.2022.101560
Griffin L, Ho L, Akhurst RJ, Arron ST, Boggs JME, Conlon P, O’Kelly P, Toland AE, Epstein EH, Balmain A, Bastian BC, Moloney FJ, Murphy GM, Laing ME (2022) Genetic polymorphism in methylenetetrahydrofolate reductase chloride transport protein 6 (MTHFR CLCN6) gene is associated with keratinocyte skin cancer in a cohort of renal transplant recipients. Skin Health Dis 2:e95. https://doi.org/10.1002/ski2.95
Bicka M, Joachimiak E, Urbanska P, Osinka A, Konopka A, Bulska E, Wloga D (2022) Cfap91-dependent stability of the RS2 and RS3 base proteins and adjacent Inner dynein arms in tetrahymena cilia. Cells 11:4048. https://doi.org/10.3390/cells11244048
Satir P, Barkalow K, Hamasaki T (1993) The control of ciliary beat frequency. Trends Cell Biol 3:409–412. https://doi.org/10.1016/0962-8924(93)90092-f
Komatani-Tamiya N, Daikoku E, Takemura Y, Shimamoto C, Nakano T, Iwasaki Y, Kohda Y, Matsumura H, Marunaka Y, Nakahari T (2012) Procaterol-stimulated increases in ciliary bend amplitude and ciliary beat frequency in mouse bronchioles. Cell Physiol Biochem 29:511–522. https://doi.org/10.1159/000338505
Kogiso H, Hosogi S, Ikeuchi Y, Tanaka S, Shimamoto C, Matsumura H, Nakano T, Sano KI, Inui T, Marunaka Y, Nakahari T (2017) A low [Ca2+]i-induced enhancement of cAMP-activated ciliary beating by PDE1A inhibition in mouse airway cilia. Pflüg Arch 469:1215–1227. https://doi.org/10.1007/s00424-017-1988-9
Kogiso H, Hosogi S, Ikeuchi Y, Tanaka S, Inui T, Marunaka Y, Nakahari T (2018) [Ca2+]i modulation of cAMP-stimulated ciliary beat frequency via PDE1 in airway ciliary cells of mice. Exp Physiol 103:381–390. https://doi.org/10.1113/ep086681
Kogiso H, Ikeuchi Y, Sumiya M, Hosogi S, Tanaka S, Shimamoto C, Inui T, Marunaka Y, Nakahari T (2018) Seihai-to (TJ-90)-induced activation of airway ciliary beatings of mice: Ca2+ modulation of cAMP-stimulated ciliary beatings via PDE1. Int J Mol Sci 19:658. https://doi.org/10.3390/ijms19030658
Kawaguchi K, Nakayama S, Saito D, Kogiso H, Yasuoka K, Marunaka Y, Nakahari T, Asano S (2022) Ezrin knockdown reduces procaterol-stimulated ciliary beating without morphological changes in mouse airway cilia. J Cell Sci 135:jcs259201. https://doi.org/10.1242/jcs.259201
Salathe M, Pratt MM, Wanner A (1993) Protein kinase C-dependent phosphorylation of a ciliary membrane protein and inhibition of ciliary beating. J Cell Sci 106(Pt 4):1211–1220. https://doi.org/10.1242/jcs.106.4.1211
Kuremoto T, Kogiso H, Yasuda M, Inui T-A, Murakami K, Hirano S, Ikeuchi Y, Hosogi S, Inui T, Marunaka Y, Nakahari T (2018) Spontaneous oscillation of the ciliary beat frequency regulated by release of Ca2+ from intracellular stores in mouse nasal epithelia. Biochem Biophys Res Commun 507:211–216. https://doi.org/10.1016/j.bbrc.2018.11.010
Ikeuchi-Yamamoto Y, Kogiso H, Saito D, Kawaguchi K, Ikeda R, Asano S, Inui T, Marunaka Y, Nakahari T (2022) Hochu-ekki-to enhanced airway ciliary beating by an [Ca2+]i increase via TRPV4 in mice. Phytomed Plus 2:100243. https://doi.org/10.1016/j.phyplu.2022.100243
Hirao T, Kim BG, Habuchi H, Kawaguchi K, Nakahari T, Marunaka Y, Asano S (2023) Transforming growth factor-β1 and bone morphogenetic protein-2 inhibit differentiation into mature ependymal multiciliated cells. Biol Pharm Bull 46:111–122. https://doi.org/10.1248/bpb.b22-00733
Yasuda M, Inui TA, Hirano S, Asano S, Okazaki T, Inui T, Marunaka Y, Nakahari T (2020) Intracellular Cl- regulation of ciliary beating in ciliated human nasal epithelial cells: Frequency and distance of ciliary beating observed by high-speed video microscopy. Int J Mol Sci 21:4052. https://doi.org/10.3390/ijms21114052
Inui T-A, Murakami K, Yasuda M, Hirano S, Ikeuchi Y, Kogiso H, Hosogi S, Inui T, Marunaka Y, Nakahari T (2019) Ciliary beating amplitude controlled by intracellular Cl- and a high rate of CO2 production in ciliated human nasal epithelial cells. Pflüg Arch 471:1127–1142. https://doi.org/10.1007/s00424-019-02280-5
Inui T-A, Yasuda M, Hirano S, Ikeuchi Y, Kogiso H, Inui T, Marunaka Y, Nakahari T (2019) Enhancement of ciliary beat amplitude by carbocisteine in ciliated human nasal epithelial cells. Laryngoscope 130:E289–E297. https://doi.org/10.1002/lary.28185
Brokaw CJ (1994) Control of flagellar bending: a new agenda based on dynein diversity. Cell Motil Cytoskeleton 28:199–204. https://doi.org/10.1002/cm.970280303
Brokaw CJ, Kamiya R (1987) Bending patterns of Chlamydomonas flagella: IV. Mutants with defects in inner and outer dynein arms indicate differences in dynein arm function. Cell Motil Cytoskeleton 8:68–75. https://doi.org/10.1002/cm.970080110
Kogiso H, Raveau M, Yamakawa K, Saito D, Ikeuchi Y, Okazaki T, Asano S, Inui T, Marunaka Y, Nakahari T (2020) Airway ciliary beating affected by the Pcp4 dose-dependent [Ca2+]i increase in Down syndrome mice, Ts1Rhr. Int J Mol Sci 21:1947. https://doi.org/10.3390/ijms21061947
Shiima-Kinoshita C, Min KY, Hanafusa T, Mori H, Nakahari T (2004) Beta 2-adrenergic regulation of ciliary beat frequency in rat bronchiolar epithelium: potentiation by isosmotic cell shrinkage. J Physiol 554:403–416. https://doi.org/10.1113/jphysiol.2003.056481
Saitoh D, Kawaguchi K, Asano S, Inui T, Marunaka Y, Nakahari T (2022) Enhancement of airway ciliary beating mediated via voltage-gated Ca2+ channels/α7-nicotinic receptors in mice. Pflüg Arch 474:1091–1106. https://doi.org/10.1007/s00424-022-02724-5
Saito D, Suzuki C, Tanaka S, Hosogi S, Kawaguchi K, Asano S, Okamoto S, Yasuda M, Hirano S, Inui T, Marunaka Y, Nakahari T (2023) Ambroxol-enhanced ciliary beating via voltage-gated Ca2+ channels in mouse airway ciliated cells. Eur J Pharmacol 941:175496. https://doi.org/10.1016/j.ejphar.2023.175496
Corbeel L, Freson K (2008) Rab proteins and Rab-associated proteins: major actors in the mechanism of protein-trafficking disorders. Eur J Pediatr 167:723–729. https://doi.org/10.1007/s00431-008-0740-z
Keeton AB, Salter EA, Piazza GA (2017) The RAS-effector interaction as a drug target. Cancer Res 77:221–226. https://doi.org/10.1158/0008-5472.Can-16-0938
Wang YY, Ke CC, Chen YL, Lin YH, Yu IS, Ku WC, O’Bryan MK, Lin YH (2020) Deficiency of the Tbc1d21 gene causes male infertility with morphological abnormalities of the sperm mitochondria and flagellum in mice. PLoS Genet 16:e1009020. https://doi.org/10.1371/journal.pgen.1009020
Pan X, Eathiraj S, Munson M, Lambright DG (2006) TBC-domain GAPs for Rab GTPases accelerate GTP hydrolysis by a dual-finger mechanism. Nature 442:303–306. https://doi.org/10.1038/nature04847
Bos JL, Rehmann H, Wittinghofer A (2007) GEFs and GAPs: critical elements in the control of small G proteins. Cell 129:865–877. https://doi.org/10.1016/j.cell.2007.05.018
Dou D, Smith EM, Evans CS, Boecker CA, Holzbaur ELF (2023) Regulatory imbalance between LRRK2 kinase, PPM1H phosphatase, and ARF6 GTPase disrupts the axonal transport of autophagosomes. Cell Rep 42:112448. https://doi.org/10.1016/j.celrep.2023.112448
Cason SE, Holzbaur ELF (2023) Axonal transport of autophagosomes is regulated by dynein activators JIP3/JIP4 and ARF/RAB GTPases. bioRxiv. https://doi.org/10.1101/2023.01.28.526044
Taruno A, Nomura K, Kusakizako T, Ma Z, Nureki O, Foskett JK (2021) Taste transduction and channel synapses in taste buds. Pflüg Arch 473:3–13. https://doi.org/10.1007/s00424-020-02464-4
Ma Z, Taruno A, Ohmoto M, Jyotaki M, Lim JC, Miyazaki H, Niisato N, Marunaka Y, Lee RJ, Hoff H, Payne R, Demuro A, Parker I, Mitchell CH, Henao-Mejia J, Tanis JE, Matsumoto I, Tordoff MG, Foskett JK (2018) CALHM3 Is essential for rapid Ion channel-mediated purinergic neurotransmission of GPCR-mediated tastes. Neuron 98:547–561. https://doi.org/10.1016/j.neuron.2018.03.043
Taruno A, Sun H, Nakajo K, Murakami T, Ohsaki Y, Kido MA, Ono F, Marunaka Y (2017) Post-translational palmitoylation controls the voltage gating and lipid raft association of the CALHM1 channel. J Physiol 595:6121–6145. https://doi.org/10.1113/jp274164
Taruno A, Kashio M, Sun H, Kobayashi K, Sano H, Nambu A, Marunaka Y (2017) Adeno-Associated Virus-Mediated Gene Transfer into Taste Cells In Vivo. Chem Senses 42:69–78. https://doi.org/10.1093/chemse/bjw101
Xu B, English JM, Wilsbacher JL, Stippec S, Goldsmith EJ, Cobb MH (2000) WNK1, a novel mammalian serine/threonine protein kinase lacking the catalytic lysine in subdomain II. J Biol Chem 275:16795–167801. https://doi.org/10.1074/jbc.275.22.16795
Gallolu Kankanamalage S, Karra AS, Cobb MH (2018) WNK pathways in cancer signaling networks. Cell Commun Signal 16:72. https://doi.org/10.1186/s12964-018-0287-1
Subramanya AR, Yang CL, McCormick JA, Ellison DH (2006) WNK kinases regulate sodium chloride and potassium transport by the aldosterone-sensitive distal nephron. Kidney Int 70:630–634. https://doi.org/10.1038/sj.ki.5001634
Saha B, Leite-Dellova DCA, Demko J, Sørensen MV, Takagi E, Gleason CE, Shabbir W, Pearce D (2022) WNK1 is a chloride-stimulated scaffold that regulates mTORC2 activity and ion transport. J Cell Sci 135:jcs260313. https://doi.org/10.1242/jcs.260313
Côme E, Blachier S, Gouhier J, Russeau M, Lévi S (2023) Lateral diffusion of NKCC1 contributes to chloride homeostasis in neurons and Is rapidly regulated by the WNK signaling pathway. Cells 12:464. https://doi.org/10.3390/cells12030464
Boyd-Shiwarski CR, Shiwarski DJ, Griffiths SE, Beacham RT, Norrell L, Morrison DE, Wang J, Mann J, Tennant W, Anderson EN, Franks J, Calderon M, Connolly KA, Cheema MU, Weaver CJ, Nkashama LJ, Weckerly CC, Querry KE, Pandey UB, Donnelly CJ, Sun D, Rodan AR, Subramanya AR (2022) WNK kinases sense molecular crowding and rescue cell volume via phase separation. Cell 185:4488-4506.e4420. https://doi.org/10.1016/j.cell.2022.09.042
Bahena-Lopez JP, Gamba G, Castañeda-Bueno M (2022) WNK1 in the kidney. Curr Opin Nephrol Hypertens 31:471–478. https://doi.org/10.1097/mnh.0000000000000820
Gao M, Ma MM, Lu FT, Huang CC, Sun L, Lv XF, Zhang B, Wang GL, Guan YY (2022) Low chloride-regulated ClC-5 contributes to arterial smooth muscle cell proliferation and cerebrovascular remodeling. Hypertension 79:e73–e85. https://doi.org/10.1161/hypertensionaha.121.18472
Shekarabi M, Zhang J, Khanna AR, Ellison DH, Delpire E, Kahle KT (2017) WNK kinase signaling in ion homeostasis and human disease. Cell Metab 25:285–299. https://doi.org/10.1016/j.cmet.2017.01.007
Inoue K, Furukawa T, Kumada T, Yamada J, Wang T, Inoue R, Fukuda A (2012) Taurine inhibits K+-Cl- cotransporter KCC2 to regulate embryonic Cl- homeostasis via with-no-lysine (WNK) protein kinase signaling pathway. J Biol Chem 287:20839–20850. https://doi.org/10.1074/jbc.M111.319418
Aoi W, Niisato N, Miyazaki H, Marunaka Y (2004) Flavonoid-induced reduction of ENaC expression in the kidney of Dahl salt-sensitive hypertensive rat. Biochem Biophys Res Commun 315:892–896. https://doi.org/10.1016/j.bbrc.2004.01.150
Asano J, Niisato N, Nakajima K, Miyazaki H, Yasuda M, Iwasak.i Y, Hama T, Dejima K, Hisa Y, Marunaka Y, (2009) Quercetin stimulates Na+/K+/2Cl- cotransport via PTK-dependent mechanisms in human airway epithelium. Am J Respir Cell Mol Biol 41:688–695. https://doi.org/10.1165/rcmb.2008-0338OC
Marunaka Y (2021) Roles of interstitial fluid pH and weak organic acids in development and amelioration of insulin resistance. Biochem Soc Trans 49:715–726. https://doi.org/10.1042/bst20200667
Aoi W, Iwasa M, Marunaka Y (2021) Metabolic functions of flavonoids: From human epidemiology to molecular mechanism. Neuropeptides 88:102163. https://doi.org/10.1016/j.npep.2021.102163
Marunaka Y, Marunaka R, Sun H, Yamamoto T, Kanamura N, Inui T, Taruno A (2017) Actions of quercetin, a polyphenol, on blood pressure. Molecules 22:209. https://doi.org/10.3390/molecules22020209
Sun H, Niisato N, Nishio K, Hamilton KL, Marunaka Y (2014) Distinct action of flavonoids, myricetin and quercetin, on epithelial Cl- secretion: useful tools as regulators of Cl- secretion. BioMed Res Int 2014:902735. https://doi.org/10.1155/2014/902735
Niisato N, Ito Y, Marunaka Y (1999) Activation of Cl- channel and Na+/K+/2Cl- cotransporter in renal epithelial A6 cells by flavonoids: genistein, daidzein, and apigenin. Biochem Biophys Res Commun 254:368–371. https://doi.org/10.1006/bbrc.1998.9952
Niisato N, Marunaka Y (2023) Therapeutic potential of multifunctional myricetin for treatment of type 2 diabetes mellitus. Front Nutr 10:1175660. https://doi.org/10.3389/fnut.2023.1175660
Piala AT, Moon TM, Akella R, He H, Cobb MH, Goldsmith EJ (2014) Chloride sensing by WNK1 involves inhibition of autophosphorylation. Sci Signal 7:ra41. https://doi.org/10.1126/scisignal.2005050
Goldsmith EJ, Rodan AR (2023) Intracellular ion control of WNK signaling. Annu Rev Physiol 85:383–406. https://doi.org/10.1146/annurev-physiol-031522-080651
Köchl R, Thelen F, Vanes L, Brazão TF, Fountain K, Xie J, Huang CL, Lyck R, Stein JV, Tybulewicz VL (2016) WNK1 kinase balances T cell adhesion versus migration in vivo. Nat Immunol 17:1075–1083. https://doi.org/10.1038/ni.3495
Garzon-Muvdi T, Schiapparelli P, ap Rhys C, Guerrero-Cazares H, Smith C, Kim DH, Kone L, Farber H, Lee DY, An SS, Levchenko A, Quiñones-Hinojosa A (2012) Regulation of brain tumor dispersal by NKCC1 through a novel role in focal adhesion regulation. PLoS Biol 10:e1001320. https://doi.org/10.1371/journal.pbio.1001320
Haas BR, Cuddapah VA, Watkins S, Rohn KJ, Dy TE, Sontheimer H (2011) With-No-Lysine Kinase 3 (WNK3) stimulates glioma invasion by regulating cell volume. Am J Physiol Cell Physiol 301:C1150–C1160. https://doi.org/10.1152/ajpcell.00203.2011
Schwab A, Fabian A, Hanley PJ, Stock C (2012) Role of ion channels and transporters in cell migration. Physiol Rev 92:1865–1913. https://doi.org/10.1152/physrev.00018.2011
Carmona B, Marinho HS, Matos CL, Nolasco S, Soares H (2023) Tubulin post-translational modifications: the elusive roles of acetylation. Biology (Basel) 12:561. https://doi.org/10.3390/biology12040561
Marunaka Y, Niisato N (2001) The essential role of cytosolic Cl- in Ca2+ regulation of an amiloride-sensitive channel in fetal rat pneumocyte. J Membr Biol 180:91–99. https://doi.org/10.1007/s002320010061
Marunaka Y, Niisato N, O’Brodovich H, Eaton DC (1999) Regulation of an amiloride-sensitive Na+-permeable channel by a beta2-adrenergic agonist, cytosolic Ca2+ and Cl- in fetal rat alveolar epithelium. J Physiol 515:669–683
Yamada T, Niisato N, Marunaka Y (2009) Effects of extracellular chloride ion on epithelial sodium channel (ENaC) in arginine vasotocin (AVT)-stimulated renal epithelial cells. Biomed Res 30:193–198. https://doi.org/10.2220/biomedres.30.193
Marunaka Y (2023) Molecular mechanisms of obesity-induced development of insulin resistance and promotion of amyloid-β accumulation: Dietary therapy using weak organic acids via improvement of lowered interstitial fluid pH. Biomolecules 13:779. https://doi.org/10.3390/biom13050779
Hosogi S, Kuwahara A, Kuwahara Y, Tanaka S, Shimamoto C, Tagawa N, Kato I, Yoshimoto K, Aoi W, Takata K, Miyazaki H, Niisato N, Tsubo Y, Yagi K, Nakahari T, Marunaka Y (2023) Mumefural prevents insulin resistance and amyloid-beta accumulation in the brain by improving lowered interstitial fluid pH in type 2 diabetes mellitus. Biomed Res 44:17–29. https://doi.org/10.2220/biomedres.44.17
Marunaka Y, Niisato N, Zou X, Xiao JB, Nakahari T (2020) Food intake targeting and improving acidity in diabetes and cancer. Food Frontiers 1:9–12. https://doi.org/10.1002/fft2.5
Aoi W, Zou X, Xiao JB, Marunaka Y (2020) Body fluid pH balance in metabolic health and possible benefits of dietary alkaline foods. eFood 1:12–23. https://doi.org/10.2991/efood.k.190924.001
Fais S, Marunaka Y (2020) The acidic microenvironment: Is it a phenotype of all cancers? A focus on multiple myeloma and some analogies with diabetes mellitus. Cancers 12:3226. https://doi.org/10.3390/cancers12113226
Pillai SR, Damaghi M, Marunaka Y, Spugnini EP, Fais S, Gillies RJ (2019) Causes, consequences, and therapy of tumors acidosis. Cancer Metastasis Rev 38:205–222. https://doi.org/10.1007/s10555-019-09792-7
Gillies RJ, Pilot C, Marunaka Y, Fais S (2019) Targeting acidity in cancer and diabetes. Biochim Biophys Acta Rev Cancer 1871:273–280. https://doi.org/10.1016/j.bbcan.2019.01.003
Marunaka Y (2018) The proposal of molecular mechanisms of weak organic acids intake-induced improvement of insulin resistance in diabetes mellitus via elevation of interstitial fluid pH. Int J Mol Sci 19:3244. https://doi.org/10.3390/ijms19103244
Marunaka Y (2018) Effects of Ninjin’yoeito on insulin resistance via improvement of the interstitial fluid pH. Jpn J Geriatrics 55:S188
Hosogi S, Ohsawa M, Kato I, Kuwahara A, Inui T, Inui A, Marunaka Y (2018) Improvement of diabetes mellitus symptoms by intake of ninjin’yoeito. Front Nutr 5:112. https://doi.org/10.3389/fnut.2018.00112
Marunaka Y (2015) Roles of interstitial fluid pH in diabetes mellitus: Glycolysis and mitochondrial function. World J Diabetes 6:125–135. https://doi.org/10.4239/wjd.v6.i1.125
Fukuda T, Fukui M, Tanaka M, Senmaru T, Iwase H, Yamazaki M, Aoi W, Inui T, Nakamura N, Marunaka Y (2015) Effect of Brazilian green propolis in patients with type 2 diabetes: A double-blind randomized placebo-controlled study. Biomed Rep 3:355–360. https://doi.org/10.3892/br.2015.436
Marunaka Y, Yoshimoto K, Aoi W, Hosogi S, Ikegaya H (2014) Low pH of interstitial fluid around hippocampus of the brain in diabetic OLETF rats. Mol Cell Therapies 2:6. https://doi.org/10.2174/138161212799504812
Hayata H, Miyazaki H, Niisato N, Yokoyama N, Marunaka Y (2014) Lowered extracellular pH is involved in the pathogenesis of skeletal muscle insulin resistance. Biochem Biophys Res Commun 445:170–174. https://doi.org/10.1016/j.bbrc.2014.01.162
Aoi W, Marunaka Y (2014) The importance of regulation of body fluid pH in the development and progression of metabolic diseases. In: Berhardt LV (ed) Advances in medicine and biology. Nova Publishers, Hauppauge
Aoi W, Marunaka Y (2014) Importance of pH homeostasis in metabolic health and diseases: crucial role of membrane proton transport. BioMed Res Int 2014:598986. https://doi.org/10.1155/2014/598986
Marunaka Y, Aoi W, Hosogi S, Niisato N, Yokoyama N, Hayata H, Miyazaki H, Kusuzaki K, Taruno A, Nomura T (2013) What is the role of interstitial pH in diabetes mellitus? Improving action of propolis on type II diabetes mellitus via pH regulation. Int J Mol Med 32:S50
Aoi W, Hosogi S, Niisato N, Yokoyama N, Hayata H, Miyazaki H, Kusuzaki K, Fukuda T, Fukui M, Nakamura N, Marunaka Y (2013) Improvement of insulin resistance, blood pressure and interstitial pH in early developmental stage of insulin resistance in OLETF rats by intake of propolis extracts. Biochem Biophys Res Commun 432:650–653. https://doi.org/10.1016/j.bbrc.2013.02.029
Kusuzaki K, Hosogi S, Ashihara E, Matsubara T, Satonaka H, Nakamura T, Matsumine A, Sudo A, Uchida A, Murata H, Baldini N, Fais S, Marunaka Y (2012) Translational research of photodynamic therapy with acridine orange which targets cancer acidity. Curr Pharm Des 18:1414–1420. https://doi.org/10.2174/138161212799504812
Puppulin L, Hosogi S, Sun H, Matsuo K, Inui T, Kumamoto Y, Suzaki T, Tanaka H, Marunaka Y (2018) Bioconjugation strategy for cell surface labelling with gold nanostructures designed for highly localized pH measurement. Nat Commun 9:5278. https://doi.org/10.1038/s41467-018-07726-5
Hosogi S, Marunaka Y, Ashihara E, Yamada T, Sumino A, Tanaka H, Puppulin L (2021) Plasma membrane anchored nanosensor for quantifying endogenous production of H2O2 in living cells. Biosens Bioelectron 179:113077. https://doi.org/10.1016/j.bios.2021.113077
Marunaka Y, Yagi K, Imagawa N, Kobayashi H, Murayama M, Minamibata A, Takanashi Y, Nakahari T (2021) Possibility of venous serum Cl- concentration ([Cl-]s) as a marker for human metabolic status: Correlation of [Cl-]s to age, fasting blood sugar (FBS), and glycated hemoglobin (HbA1c). Int J Mol Sci 22:11111. https://doi.org/10.3390/ijms222011111
Scheel O, Zdebik AA, Lourdel S, Jentsch TJ (2005) Voltage-dependent electrogenic chloride/proton exchange by endosomal CLC proteins. Nature 436:424–427. https://doi.org/10.1038/nature03860
Jentsch TJ, Pusch M (2018) CLC Chloride Channels and Transporters: Structure, Function, Physiology, and Disease. Physiol Rev 98:1493–1590. https://doi.org/10.1152/physrev.00047.2017
Hosogi S, Kusuzaki K, Inui T, Wang X, Marunaka Y (2014) Cytosolic chloride ion is a key factor in lysosomal acidification and function of autophagy in human gastric cancer cell. J Cell Mol Med 18:1124–1133. https://doi.org/10.1111/jcmm.12257
Quick JD, Silva C, Wong JH, Lim KL, Reynolds R, Barron AM, Zeng J, Lo CH (2023) Lysosomal acidification dysfunction in microglia: an emerging pathogenic mechanism of neuroinflammation and neurodegeneration. J Neuroinflammation 20:185. https://doi.org/10.1186/s12974-023-02866-y
Nieto-Torres JL, Hansen M (2021) Macroautophagy and aging: The impact of cellular recycling on health and longevity. Mol Aspects Med 82:101020. https://doi.org/10.1016/j.mam.2021.101020
Acknowledgements
I would like to thank all staffs of Medical Research Institute, Kyoto Industrial Health association for their support so that I could concentrate on the present study.
Funding
This work was supported by Grants-in-Aid for Scientific Research (B) from Japan Society of the Promotion of Science (JSPS KAKENHI Grant Numbers JP18H03182 and JP21H03368 to YM).
Author information
Authors and Affiliations
Contributions
YM conceptualized the study; YM prepared an original draft; YM reviewed and edited the manuscript; YM read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Marunaka, Y. Physiological roles of chloride ions in bodily and cellular functions. J Physiol Sci 73, 31 (2023). https://doi.org/10.1186/s12576-023-00889-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12576-023-00889-x