Abstract
Background
The management of benign prostatic enlargement (BPE) in low resource settings poses a major challenge in Africa. The objective of the study was to investigate the accuracy of Bladder Voiding Efficiency (BVE) to assess lower Urinary Tract Symptoms (LUTS) among BPE patients in a low resource setting.
Methods
From December 2017 to March 2018, patients with benign prostatic enlargement (BPE) and Lower Urinary Tract Symptoms (LUTS) were recruited into the study. The study was a prospective cross-sectional study. Participants had the International Prostate Symptom Score (IPSS) recorded followed by evaluation of their Bladder Voiding Efficiency (BVE). The BVE was calculated as the ratio of the volume of Urine voided over total volume of Urine in the bladder at the time of the void. The data were analysed to show the Sensitivity and Specificity of BVE in symptomatic LUTS. The Pearson correlation co-efficient between IPSS and BVE was analysed.
Results
The study recruited 94 participants. The age range was 45 to 85 year. The mean age was 68.1 years. The sensitivity of BVE to detect severe LUTS was 97.97%, while the specificity of BVE to detect mild to moderate disease was 97.78%. The correlation coefficient between IPSS and BVE was negatively correlated at 0.89, and this was statistically significant (P < 0.001).
Conclusion
The Bladder Voiding Efficiency (BVE) is a highly sensitive and specific test in our population to detect LUTS. It is well correlated to the International Prostate Severity Score in this study population.
Similar content being viewed by others
1 Background
There has been an increase in the prevalence of BPE in Africa in the last 10 years because of life-style changes [1, 2]. The prevalence of BPE ranges from 40 to 60% among men over 50 years of age in Africa [3]. The increase in metabolic syndromes and the related changes in diet as well as life-style have also been linked to this increase in BPE/LUTS in Africa [4].
The evaluation of BPE/LUTS in low-resource setting poses a challenge because of the low utilisation of the IPSS score and the sparsity of Urological services in Africa [5, 6].
The use of BVE as an objective tool to determine the severity of BPE/LUTS in low-resource settings has been minimal [7].
The simple BVE technique is easy to use, minimally invasive and can be done by non-Physicians. This makes it very suitable for use in low-resource setting where other urological diagnostic services may not be available [8].
The objective of this study was to determine the acceptability and accuracy of using BVE to determine the severity of BPH/LUTS using the IPSS score as a gold standard.
2 Methods
The study was performed at the Ndola Teaching Hospital Urology Outpatient Clinic from December 2017 to March 2018. This study was approved by the Ethics Review Board of our hospital. Prior to recruitment, it was ensured that all patients included in the study had provided appropriate informed consent. A research questionnaire was administered to each patient to obtain all vital epidemiological data from the patient.
The case definition of a participant was any patient aged 45 to 85 years with clinical evidence of BPE and evidence of LUTS attributable to BPE. Patients with urethral disease, neurological disease, Prostate or Bladder malignancies or complicated BPE were excluded from the study. In addition all patients with medical conditions such as Diabetes Mellitus, Cardiac Failure or any conditions that might affect bladder function were also excluded.
The standard IPSS was administered to each patient by a trained nurse and the total score computed. The patient was asked to do an initial void, the voided volume (V) as well as the post-void residual urine (PVR) were measured. These were recorded as V1 and PVR1. The bladder was emptied completely thereafter. Once the bladder was emptied, it was filled passively with 200mls of Saline at room temperature. The patient was then instructed to void a second time. The volumes obtained were recorded as V2 (voided urine volume) and PVR2 (post-void urine volume), respectively. The average of V1 and V2 as well as PVR1 and PVR2 were used to obtain mean void and mean PVR volumes, respectively. The Bladder Voiding Efficiency (BVE) was then computed as the ratio of mean void to Total Bladder Capacity (mean void + mean post-void urine volume).
Each participant recruited had an IPSS administered them. The IPSS scores were grouped into two categories. Those with a score of ≤ 18 were Group 1, which was mild to moderate symptoms. Those with a score of ≥ 19 were Group 2, which was classed as severe symptoms.
The BVE results were also grouped into two. The participants with a BVE ≥ 75% were in Group 1 and were said to have good voiding efficiency. Those with a BVE ≤ 74% were Group 2, with poor voiding efficiency. The cut-off used was based on recently published literature on BVE measure of good bladder function [9].
The participants were also asked about the acceptability of BVE as a method of assessing severity of LUTS. The results were analysed to provide an acceptability rate of the technique among the participants.
The data were coded and then entered into the Excel 2013 software with double entry verification. The IPSS was used as the Gold Standard. Sensitivity was defined as the ability of the BVE to detect severe IPSS, while Specificity was defined as the ability of BVE to detect mild and moderate IPSS. These ratios were computed as percentages. The correlation coefficient was the extent and direction of the relationship between the BVE and the IPSS in this data set. The Pearson coefficients and the specificity/sensitivity were analysed using SPSS version 20 software.
3 Results
The study recruited a total of 102 patients. However, 8 were not enrolled because they had confounding co-morbidities. The study had 94 participants who were enroled into the study and for whom a complete data set was collected. The age-range was between 49 and 85 years with a mean age of 68.1 (standard deviation [SD] ± 7.49 years). (Table 1).
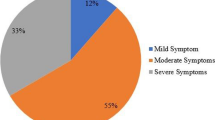
The mean IPSS score was 18.81 ± 10.7 SD with a minimum score of 1 and a maximum score of 31. Of the 94 enroled, 49 (52%) had severe symptoms, 21 (22%) had moderate symptoms and 24 (26%) showed scores mild symptoms (Table 1).
In assessment of the acceptability of the procedure by participants, 86 (91.5%) found it acceptable and 8 (8.5%) did not find it acceptable.
The BVE was used as the test and the IPSS as the gold standard. Table 2 shows the sensitivity, specificity, as well as the positive and negative predictive values. The sensitivity of the BVE was 97.96%. The specificity was calculated as 97.78%. The positive predictive value was 97.96% and negative predictive values were both 97.78%.
The Pearson correlation coefficient was 0.89. This was a negative correlation with a P value of < 0.001.
4 Discussion
There is a rising prevalence of BPE/LUTS in Africa due to increasing lifestyle change and an increase in life expectancy [1, 2].The study found the mean age at presentation to be 68.1 years. The IPSS pattern found in the study is similar to what other studies in this region have shown [11, 12]. The mean IPSS score of 18.8 did not differ significantly from that found in previous studies at the site as well as other regional studies [4, 13]. The pattern of presentation in the study of 52% with severe symptoms (Table 1) was high compared to other studies which have shown mainly predominance of moderate symptoms [4, 13]. Ogwuche et al. in their study of 120 patients at the Jos University Teaching Hospital showed that most patients (59%) had moderate symptoms. Strother et al. in their study of 473 patients in Uganda showed increasing severity of symptoms score in the specialist clinics relative to those in the community-based studies [14]. This suggests that patients present late due to difficulty of access to urology services in Africa, which is well documented [4, 13,14,15].
The determination of the severity of BPH/LUTS in clinical settings, especially in low resourced settings is difficult. The introduction of IPSS by Barry in 1992 provided a tool for assessing severity of BPH/LUTS. However its use in low resourced setting has been difficult due to various problems including low literacy rates, visual problems in elderly men and the low number of Urologist to population in these settings [4, 5]. Unlike the Cardiac emptying which leaves an end systolic volume to promote contractility, Bladder emptying is normally expected to leave minimal to no residual urine. The increase in post-void residual has been used by Urologists as an index to measure of Bladder outflow obstruction. However the absence of a clear cut off for post-void residual urine has reduced its usage and value. Increasingly the use of BVE as a more accurate measure of Bladder Function or Dysfunction has been shown by a number of studies (7.8.9.10). This is especially important in the distinction between medical and surgical management of BPH/LUTs as shown by Choo et al. in 2014. In their study they propose a BVE cut off of 75%. When BVE falls below this cut off secondary Bladder changes are likely to occur which may be inversible, because of the persistence of high Bladder pressures.
The study found a high acceptability for the use of the BVE for evaluation of severity of LUTS at 91.5% (Table 1). Other studies have shown high acceptability for this tool in accessing LUTS in BPH and other Bladder Outflow Obstruction (BOO) patients [7, 9, 15].
The Sensitivity and Specificity of BVE were very high at 97.96% and 97.87%, respectively. This was much higher than that found at the same site using the Single Question Nocturia Score (SQNS) where the Sensitivity and Specificity of this tool was 87% and 91%, respectively [4]. Other tools have demonstrated higher correlation with IPSS score such as the Visual IPSS Score and the UWIN score with a correlation coefficient of 0.72 and 0.913, respectively [17,18,19,20].The study found the BVE had a high correlation with IPSS though the correlation was negative. This meant the higher the voiding efficiency, the lower the IPSS score. The correlation coefficient was 0.89 (P < 0.001) Fig. 1.
The BVE parameter has also been used successfully to measure post-operation LUTS as well as to measure LUTS in women with BOO [8, 9].
The BE may also have value in the discrimination of those patients with severe LUTS requiring early surgical treatment over those with whom initial medical treatment may improve symptoms. It is possible that a delay in this process may result in secondary Bladder changes which may not be correctable even after surgery [9, 10].
5 Conclusion
This study finding shows that simple BVE evaluation can be used to accurately assess LUTS, in low-resource settings. This tool also has a high acceptability in this study population. The BVE indices may also be valuable in distinguishing those patients in whom surgery is indicated in contrast to those who can be given medical treatment. This decision could help to reduce the number of patients whose LUTS persists even after medical treatment.
Availability of data and materials
The data base contain the study variables is available in MS Excel and is accessible to the journal and reviewers upon request. It has also been attached as supplementary file in the submission documents.
Abbreviations
- BOO:
-
Bladder outflow obstruction
- BPE:
-
Benign prostatic enlargement
- BVE:
-
Bladder voiding efficiency
- IPSS:
-
International prostate severity score
- LUTS:
-
Lower urinary tract symptoms
- PVR:
-
Post void residual urine
- SQNS:
-
Single question nocturia score
- UWIN:
-
Urgency, weak stream, incomplete emptying and nocturia
References
Yeboah ED (2016) Prevalence of benign prostatic hyperplasia and prostate cancer in Africans and Africans in the diaspora. J West Afr College Surg 6(4):1
Chokkalingam AP, Yeboah ED, Demarzo A, Netto G, Yu K, Biritwum RB, Tettey Y, Adjei A, Jadallah S, Li Y, Chu LW (2012) Prevalence of BPH and lower urinary tract symptoms in West Africans. Prostate Cancer Prostatic Dis 15(2):170–176
Ejike CE, Ezeanyika LU (2008) Metabolic syndrome in sub-Saharan Africa:“smaller twin” of a region’s prostatic diseases? Int Urol Nephrol 40(4):909–920
Kajimotu T, Bowa K (2018) Accuracy of a “single question nocturia score” compared to the “international prostate symptoms score” in the evaluation of lower urinary tract symptoms in benign prostatic hyperplasia: a study performed at Ndola teaching hospital, Ndola. Zambia Plos one 13(6):e0198096
Bowa K (2013) International prostate symptoms score usage in a developing country. Annal Afr Med 12(3):174
Launer BM, McVary KT, Ricke WA, Lloyd GL (2021) The rising worldwide impact of benign prostatic hyperplasia. BJU Int 127(6):722
Abrams P (1999) Bladder outlet obstruction index, bladder contractility index and bladder voiding efficiency: three simple indices to define bladder voiding function. Br J Urol Int 84:14–15
Bosch RSLH, Krause R (1995) Dependence of male voiding efficiency on age, bladder contractility and urethral resistance: development of a voiding efficiency normogram. J Urol 154:190–194
Choo MS, Cho SY, Han JH, Lee SH, Paick JS, Son H (2014) The cutoff value of bladder voiding efficiency for predicting surgical outcomes after GreenLight HPS™ laser photoselective vaporization of the prostate. J Endourol 28(8):969–974
O’Leary MP, Barry MJ, Fowler FJ Jr (1992) Hard measures of subjective outcomes: validating symptom indexes in urology. J Urol. https://doi.org/10.1016/S0022-5347(17)36965-3
Jumbe SA (1982) Experience in prostatectomy in Zanzibar using roll-gauge packing. East Afr Med J 59(9):599–604
Kachimba SJ (1988) Surgical management of benign prostate hyperplasia in the university teaching hospital. M. Med Dissertation 1988: University of Zambia, Lusaka, Zambia.
Udeh EI, Ozoemena OF, Ogwuche E (2012) The relationship between prostate volume and international prostate symptom score in Africans with benign prostatic hyperplasia. Niger J Med 21(3):290–295
Stothers L, Macnab AJ, Bajunirwe F, Mutabazi S, Berkowitz J (2017) Associations between the severity of obstructive lower urinary tract symptoms and care-seeking behavior in rural Africa: a cross-sectional survey from Uganda. PLoS ONE 12(3):e0173631
Bajunirwe F, Stothers L, Berkowitz J, Macnab AJ (2018) Prevalence estimates for lower urinary tract symptom severity among men in Uganda and sub-Saharan Africa based on regional prevalence data. Can Urol Assoc J 12(11):E447
Roehrborn CG, Kaminetsky JC, Auerbach SM, Montelongo RM, Elion-Mboussa A, Viktrup L (2010) Changes in peak urinary flow and voiding efficiency in men with signs and symptoms of benign prostatic hyperplasia during once daily tadalafil treatment. BJU Int 105(4):502–507
Ramaraju K, Rajan K, Kalyanasundaram S, Chennakrishnan I (2016) Comparison of uwin score with international prostatic symptom score in patients with lower urinary tract symptoms. J Evol Med Dent Sci 5(80):5942–5947
Heyns CF, Van der Walt CLE, Groeneveld AE (2012) Correlation between a new visual prostate symptom score (VPSS) and uroflowmetry parameters in men with lower urinary tract symptoms. S Afr Med J 102(4):237–240
Badı́a X, Garcı́a-Losa M, Dal-Ré R, Carballido J, Serra M. (1998) Validation of a harmonized Spanish version of the IPSS: evidence of equivalence with the original American scale. Urology 52(4):614–620
Mallya A, Keshavamurthy R, Karthikeyan VS, Kumar S, Nagabhushana M, Kamath AJ (2017) UWIN (Urgency, Weak stream, Incomplete Void, Nocturia) Score for assessment of lower urinary tract symptoms: could it replace the American urology association symptom index score? An open label randomized cross over trial. LUTS: Lower Urinary Tract Symptoms. Feb 1.
Acknowledgements
The authors acknowledge the Ndola Teaching Hospital Urology Unit and the Copperbelt University School of Medicine for hosting the study.
Funding
The study received no external funding.
Author information
Authors and Affiliations
Contributions
KB conceptualised and supervised the research. PK organised the research site, collected and analysed the data. The final paper was co-written by both KB and PK. Both authors read and approved by the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Research Ethic Committee of the Tropical Disease Research Centre in December 2017.Research approval was obtained from the Bio-medical Ethics Review Committee of Tropical Diseases Research Centre (TDRC), IRB registration number: 00002911, FWA number: 00003729 and research number TRC/C4/09/2017. The methods outlined in this research were strictly adhered to the safety and well-being of the patient.
Consent for publication
The authors provide consent to the AFJU to publish the materials and pictures contained in the manuscripts.
Competing of interests
The authors declare that we have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
This file contains the patient data for all the patients who were recruited in the study. It includes the independent and dependent variables on which all the study results are based.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kapesa, P., Bowa, K. The use of bladder voiding efficiency in assessing benign prostatic enlargement. Afr J Urol 28, 56 (2022). https://doi.org/10.1186/s12301-022-00319-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-022-00319-1