Abstract
Purpose
To evaluate the association of intravesical prostatic protrusion (IPP) and overactive bladder (OAB) in male patients with lower urinary tract symptoms (LUTS). IPP has been suggested to correlate with storage symptoms in addition to bladder outlet obstruction.
Methods
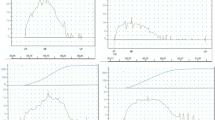
This was an open-labeled, single-center, prospective study involving 128 men older than 40 years presenting with LUTS. We analyzed the relationship of IPP with age, prostate volume, uroflowmetry, post-void residual urine volume (PVR), International Prostate Symptom Score (IPSS), urgency severity scale (USS), and OAB symptom score (OABSS). The patients with an urgency score of ≥ 2 (OABSS question 2) and sum score of ≥ 3 were considered to have OAB. IPP was measured in the mid-sagittal section using transrectal ultrasound. The degree of IPP was classified as grade 1 (≤ 5 mm), grade 2 (> 5–10 mm), and grade 3 (> 10 mm).
Results
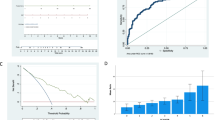
The mean age of the patients was 64.9 ± 9.2 years, and 101 patients were diagnosed with OAB (79%). Mean IPPs were 2.4 ± 1.4 mm (grade 1, n = 77), 7.6 ± 1.4 mm (grade 2, n = 27), and 14.8 ± 4.4 mm (grade 3, n = 24). IPP was positively correlated with age, prostate size, PSA, PVR, and OABSS nocturia subscore, but not correlated with the presence or severity of OAB. Areas under the receiver-operating characteristic (ROC) curves for the diagnosis of OAB were 0.807 and 0.604 for IPSS-storage subscore and IPP, respectively.
Conclusion
IPP is not a good predictor of OAB in men presenting with LUTS. However, grade 3 IPP indicates higher frequency of nocturia.


Similar content being viewed by others
References
Chia SJ, Heng CT, Chan SP, Foo KT (2003) Correlation of intravesical prostatic protrusion with bladder outlet obstruction. BJU Int 91(4):371–374
Lim KB, Ho H, Foo KT, Wong MY, Fook-Chong S (2006) Comparison of intravesical prostatic protrusion, prostate volume and serum prostatic-specific antigen in the evaluation of bladder outlet obstruction. Int J Urol 13(12):1509–1513. https://doi.org/10.1111/j.1442-2042.2006.01611.x
Knutson T, Edlund C, Fall M, Dahlstrand C (2001) BPH with coexisting overactive bladder dysfunction—an everyday urological dilemma. Neurourol Urodyn 20(3):237–247
Oelke M, Baard J, Wijkstra H, de la Rosette JJ, Jonas U, Hofner K (2008) Age and bladder outlet obstruction are independently associated with detrusor overactivity in patients with benign prostatic hyperplasia. Eur Urol 54(2):419–426. https://doi.org/10.1016/j.eururo.2008.02.017
Keqin Z, Zhishun X, Jing Z, Haixin W, Dongqing Z, Benkang S (2007) Clinical significance of intravesical prostatic protrusion in patients with benign prostatic enlargement. Urology 70(6):1096–1099. https://doi.org/10.1016/j.urology.2007.08.008
Lee JM, Chung H, Kim T-W, Kim HS, Wang JH, Yang S-K (2008) The Correlation of intravesical prostatic protrusion with storage symptoms, as measured by transrectal ultrasound. Korean J Urol 49(2):145–149
Kim KH, Kim YS (2010) Correlation of male overactive bladder with intravesical prostatic protrusion. Kor J Urol 51(12):843–846. https://doi.org/10.4111/kju.2010.51.12.843
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, van Kerrebroeck P, Victor A, Wein A (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 21(2):167–178
Homma Y, Yoshida M, Seki N, Yokoyama O, Kakizaki H, Gotoh M, Yamanishi T, Yamaguchi O, Takeda M, Nishizawa O (2006) Symptom assessment tool for overactive bladder syndrome–overactive bladder symptom score. Urology 68(2):318–323. https://doi.org/10.1016/j.urology.2006.02.042
Kuo TL, Teo JS, Foo KT (2016) The role of intravesical prostatic protrusion (IPP) in the evaluation and treatment of bladder outlet obstruction (BOO). Neurourol Urodyn 35(4):535–537. https://doi.org/10.1002/nau.22741
Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, Coyne K, Kelleher C, Hampel C, Artibani W, Abrams P (2006) Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 50(6):1306–1314. https://doi.org/10.1016/j.eururo.2006.09.019(discussion 1314–1305)
Kim TH, Han DH, Lee KS (2014) The prevalence of lower urinary tract symptoms in korean men aged 40 years or older: a population-based survey. Int Neurourol J 18(3):126–132. https://doi.org/10.5213/inj.2014.18.3.126
Chapple C, Castro-Diaz D, Chuang YC, Lee KS, Liao L, Liu SP, Wang J, Yoo TK, Chu R, Sumarsono B (2017) Prevalence of Lower Urinary Tract Symptoms in China, Taiwan, and South Korea: results from a cross-sectional population-based study. Adv Ther 34(8):1953–1965. https://doi.org/10.1007/s12325-017-0577-9
Chuang YC, Liu SP, Lee KS, Liao L, Wang J, Yoo TK, Chu R, Sumarsono B (2019) Prevalence of overactive bladder in China, Taiwan and South Korea: results from a cross-sectional, population-based study. Lower Urinary Tract Sympt 11(1):48–55. https://doi.org/10.1111/luts.12193
Lee KS, Yoo TK, Liao L, Wang J, Chuang YC, Liu SP, Chu R, Sumarsono B (2017) Association of lower urinary tract symptoms and OAB severity with quality of life and mental health in China, Taiwan and South Korea: results from a cross-sectional, population-based study. BMC Urol 17(1):108. https://doi.org/10.1186/s12894-017-0294-3
D'Silva KA, Dahm P, Wong CL (2014) Does this man with lower urinary tract symptoms have bladder outlet obstruction?: The Rational Clinical Examination: a systematic review. JAMA 312(5):535–542. https://doi.org/10.1001/jama.2014.5555
Malde S, Nambiar AK, Umbach R, Lam TB, Bach T, Bachmann A, Drake MJ, Gacci M, Gratzke C, Madersbacher S, Mamoulakis C, Tikkinen KA, Gravas S (2017) Systematic review of the performance of noninvasive tests in diagnosing bladder outlet obstruction in men with lower urinary tract symptoms. Eur Urol 71(3):391–402. https://doi.org/10.1016/j.eururo.2016.09.026
Lu S-Y, Yang C-M, Fan Y-H, Lin AT-L, Chen K-K (2016) Intravesical prostatic protrusion correlates well with storage symptoms in elderly male patients with non-neurogenic overactive bladder. Urol Sci 27(1):17–20
Marshall SD, Raskolnikov D, Blanker MH, Hashim H, Kupelian V, Tikkinen KA, Yoshimura K, Drake MJ, Weiss JP (2015) Nocturia: current levels of evidence and recommendations from the international consultation on male lower urinary tract symptoms. Urology 85(6):1291–1299. https://doi.org/10.1016/j.urology.2015.02.043
Acknowledgements
The authors would like to thank Pei-Wen Chang Chien, Hui-Hsin Huang, and Biostatistics Center of Kaohsiung Chang Gung Memorial Hospital for statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tsai, CH., Lee, WC., Shen, YC. et al. The role of intravesical prostatic protrusion in the evaluation of overactive bladder in male patients with LUTS. Int Urol Nephrol 52, 815–820 (2020). https://doi.org/10.1007/s11255-019-02370-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-019-02370-4