Abstract
Background
Voluntary medical male circumcision (VMMC) reduces the risk of HIV transmission. Task shifting of VMMCs to non-doctor health workers is recommended to enhance scale-up of VMMC programs. This study evaluated outcomes of circumcision conducted by doctors compared to non-doctors in central Uganda.
Methods
In this prospective observational study, we observed and followed 274 males at 3 health facilities in Kampala, Uganda. Each participant was observed during the circumcision procedure, monitored for 2 h post-surgery and assessed at 24 h, 3 days and after one week for adverse events.
Results
The median age of the circumcised men was 24.00(IQR, 20.00–28.00) years. Of the VMMCs, 19.3% (53/274) were carried out by doctors while 80.7% (221/274) by non-doctors. Following VMMC, 5.47% (15/274) men experienced adverse events and proportions of adverse events by cadre were similar; doctors (5.66% [3/53]) and non-doctor health workers (5.43% [12/221]), p = 0.99. Seven participants had pus discharge (all had been operated by non-doctors), 2 participants had bleeding at 2 h (one by doctor and one by non-doctor), and 4 participants had excessive skin removal (2 by doctors vs 2 by non-doctors). There was no reported urethral injury or glans amputation.
Conclusion
Our study found no statistically significant difference in the incidence of adverse events among VMMCs conducted by doctors compared to non-doctor health workers. Our study showed no incidence of serious adverse events such as death, urethral injury or glans amputation following VMMCs. Our results add to the existing literature to guide task shifting in the context of VMMCs.
Similar content being viewed by others
1 Background
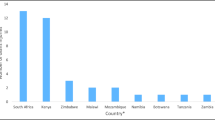
Male circumcision reduces HIV transmission by about 60% [1,2,3]. Estimates indicate that to avert 3.36 million HIV infections, about 29 million VMMCs are needed in 13 HIV high-risk sub-Saharan Africa countries in the years of 2011–2025; these countries are Botswana, Lesotho, Malawi, Mozambique, Namibia, Rwanda, South Africa, Swaziland, Tanzania, Uganda, Zambia, Zimbabwe and Kenya [4]. A key challenge to VMMCs scale-up in sub-Saharan Africa is the lack of skilled health personnel [5]. The region has a low doctor to population ratio of 0.16/1000 [6], and thus, task shifting is recommended, such that VMMCs are conducted by non-doctor health workers such as nurses and clinical officers [7, 8].
A systematic review of outcomes of VMMCs conducted by doctors compared to non-doctors showed no difference in the incidence of adverse events between these two cadres [9]. In Uganda, previous studies have indicated a low incidence of adverse events following VMMCs carried out by non-doctor health workers [10, 11] and similar findings have been reported in other countries such as Kenya [12] and South Africa [13]. However, a number of health professionals and policy makers still express skepticism to task shifting, due to factors such as perceived incompetence of non-doctors, fear of increased adverse events and lack of adequate support supervision for non-doctors [14,15,16,17]. Our study thus aimed at comparing clinical outcomes of VMMCs conducted by doctors and non-doctor health workers in central Uganda.
2 Methods
2.1 Study setting and participants
We carried out this study at two private not-for-profit hospitals (Mengo hospital and Kibuli hospital) and one government public health facility (Kisenyi Health center IV). These facilities are located in Uganda’s capital city, Kampala, and routinely carry out VMMCs as part of their services. The circumcision services are offered as outpatient procedures on a walk-in basis. In this study, we included participants who were aged 13 years and above, who were circumcised by doctors or non-doctors (clinical officers and nurses). We excluded those with comorbidities including sickle cell anemia, diabetes mellitus, history of hypertrophic scars or keloids, those receiving chemotherapy, bleeding disorders and severe penile anomalies like hypospadias.
2.2 Study design
This was a prospective observational study carried out from September 2013 to February 2014. We prospectively observed and followed up 274 males who had VMMCs during the study period. Men who came to the health facilities for VMMCs during the study period were consecutively recruited. To evaluate time taken to conduct the circumcision procedure, a stop clock was started from the moment of applying the antiseptic solution to the surgical site and ended after the wound dressing was applied. Participants were monitored in the health facility for 2 h post-surgery and then discharged home. A phone call was made to the participants at 24 h, at 3 days and after one week to assess for adverse events. In case of any reported complication, the participant was called back to the health facility for further evaluation and treatment.
Direct observation of the circumcision procedure was done by the principal investigator [HM] who was at the time a postgraduate student undertaking her master’s degree in surgery. HM observed the surgical procedure and conducted the surgical incision site inspection and follow-up of the participants working together with research assistants.
2.3 Data analysis
Data were entered using Epi data version 3.1. Frequencies and percentages for categorical variables were generated and stratified by medical doctors and non-doctors. Means and medians for continuous variables were generated. Chi-square or Fisher’s exact test was used to measure association between categorical variables, whereas the Student’s t test and Kruskal–Wallis test were used on continuous variables. The logistic regression model was used to measure factors associated with adverse events; factors with a p value of < 0.2 at bivariate analysis were included into the model and a p value of 0.05 was considered significant. A participant was regarded as having an adverse event if he experienced any of the following: postsurgical bleeding, evidence of glans amputation, evidence of excessive skin removal, evidence of urethral injury, fever post-surgery and evidence of pus discharge post-circumcision. Statistical analysis was performed using SAS Enterprise Guide 7.1.
3 Results
3.1 Participant characteristics
A total of 274 men underwent VMMCs, with a median age of 24 years (IQR 20.00–28.00). The men who had the VMMCs conducted by doctors were younger than those operated by non-doctors (22.00, IQR 19.00–27.00 vs 24.00, IQR 20.00–28.00, p = 0.0320). Majority of the VMMCs were conducted from the government health facility (Kisenyi Health Centre IV) 157/274 (57.30%). Doctors took longer time while conducting the VMMCs compared to non-doctors, mean time of 32.72 min (SD 9.47) compared to 15.45 min (SD 13.96) p < 0.0001. (Table 1).
3.2 Adverse events
Overall, 15/274 (5.47%) participants had at least one adverse event with one participant having more than one adverse event (fever and evidence of pus discharge post-circumcision). Only two participants developed postsurgical bleeding in the 2 h post-VMMC; one had been operated by a doctor and the second participant operated by a non-doctor. Three participants (1.10%) developed fever in the postoperative period, and all had been operated by non-doctor health workers. Seven participants (2.57%) developed pus discharge from the circumcision wound during the 1-week follow-up period; all these 7 participants had been operated by non-doctors. No participant had glans amputation or urethral injury (Table 1).
There was no statistically significant difference in the occurrence of adverse events following VMMCs conducted by doctors compared to non-doctors (OR 1.0450, CI-0.2842–3.8430, p-0.9472). There was also no difference in the occurrence of adverse events among VMMCs conducted in private health facilities compared to the public health facility (AOR 0.5243, CI-0.1210–2.2714) (Table 2).
4 Discussion
This study evaluated the clinical outcomes of VMMCs conducted by doctors and non-doctors. Our results showed no difference in the incidence of adverse events following circumcisions conducted by doctors compared to VMMCs conducted by non-doctors. These findings are similar to previous studies which compared the incidence of adverse events based on these two different cadres of health workers [9]. These results thus add to the existing literature which indicates that non-doctor health workers can safely perform circumcisions, in the context of task shifting allowing doctors to focus on other essential services [8, 9].
The total prevalence of adverse events from our study of 5.47% was slightly higher compared to other studies in Uganda which show a prevalence of 2.1% in Kampala [10] and 0.6–1.4% Rakai district [11]. However, the prevalence of adverse events in our study is lower compared to studies which were conducted in other African countries which recorded prevalence of adverse events ranging from 0 to 24% [18] and 0.70 to 37.36% with an overall pooled prevalence of 2.31% [9]. Our study thus indicates that the rate of occurrence of adverse events following VMMCs is relatively low in the context of task shifting.
The proportion of males who developed signs of infections in our study was slightly higher (fever 1.35% and pus discharge 3.15%) as compared to what is described in other studies 0.30–1.85% [9]. In our study, all the participants with features of infections had been operated by non-doctor health workers. One of the reasons which we believe may explain this difference in infection rates among non-doctor compared to doctors is that the largest number of circumcisions was conducted by non-doctors and thus the higher proportions of infections were observed in this group. However, this could be explored in further studies to evaluate whether this is arising from differences in infection control practices during circumcisions procedures among doctors compared to non-doctors. In addition, this is an indicator for the need to emphasize infection control protocols when conducting circumcisions. As task shifting is being implemented as per the guidance by the WHO [7], we would recommend continuous training and evaluation of infection control practices to promote safe VMMCs.
In our study, there was no reported serious adverse event such as urethral injury, glans amputation or death. This is similar to other circumcision programs in Uganda [10, 11] and other sub-Saharan African countries [9]. This is reassuring since it indicates that VMMCs can be conducted safely by both non-doctor health workers with limited incidence of serious adverse events.
Doctors generally took longer time to complete the circumcision procedures compared to non-doctors. This finding is similar to a retrospective review conducted in South Africa where doctors took longer time compared to non-doctors [13]. However, a study by Buwembo and colleagues in Uganda showed that non-doctor health workers take more time to complete the circumcision procedure compared to doctors [11]. In general, a number of factors influence how long each health worker may take to complete a circumcision procedure among which include the health worker’s experience and proficiency [6, 11]. The time taken to conduct the circumcision procedure was not associated with occurrence of adverse events in our study.
One of the limitations to our study is that a high number of VMMCs were conducted by non-doctor health workers. The incidence of adverse events (such as infections) among circumcisions by non-doctor health workers compared to doctors may thus have been affected by the disproportionately higher number of VMMCs conducted by non-doctor health workers.
5 Conclusions
Our study showed no incidence of serious adverse events such as death, urethral injury or glans amputation following VMMCs. There was no statistically significant difference in the incidence of adverse events among VMMCs conducted by doctors compared to non-doctor health workers. However, all participants who had features of infection had been operated by non-doctor health workers. These findings indicate that doctors and non-doctor health workers can provide safe VMMCs with a low incidence of adverse events. We recommend the need to improve infection control practices for VMMCs especially among non-doctor health workers. Our study adds to the existing literature to guide health workers and policy makers on task shifting in the scaling up of VMMCs.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- VMMC:
-
Medical male circumcision
- WHO:
-
World Health Organization
References
Gray RH, Kigozi G, Serwadda D, Makumbi F, Watya S, Nalugoda F, Kiwanuka N, Moulton LH, Chaudhary MA, Chen MZ (2007) Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet 369(9562):657–666
Bailey RC, Moses S, Parker CB, Agot K, Maclean I, Krieger JN, Williams CF, Campbell RT, Ndinya-Achola JO (2007) Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet 369(9562):643–656
Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A (2005) Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med 2(11):e298
Njeuhmeli E, Forsythe S, Reed J, Opuni M, Bollinger L, Heard N, Castor D, Stover J, Farley T, Menon V (2011) Voluntary medical male circumcision: modeling the impact and cost of expanding male circumcision for HIV prevention in eastern and southern Africa. PLoS Med 8(11):e1001132
Curran K, Njeuhmeli E, Mirelman A, Dickson K, Adamu T, Cherutich P, Mahler H, Fimbo B, Mavuso TK, Albertini J (2011) Voluntary medical male circumcision: strategies for meeting the human resource needs of scale-up in southern and eastern Africa. PLoS Med 8(11):e1001129
Gray RH, Wawer MJ, Kigozi G (2013) Programme science research on medical male circumcision scale-up in sub-Saharan Africa. Sex Transm Infect 89(5):345–349
World Health Organisation (2008) Task shifting : rational redistribution of tasks among health workforce teams : global recommendations and guidelines., Geneva, Switzerland
World Health Organisation, Considerations for implementing models for optimizing the volume and efficiency of male circumcision services for HIV prevention, Geneva, Switzerland, 2010.
Ford N, Chu K, Mills EJ (2012) Safety of task-shifting for male medical circumcision: a systematic review and meta-analysis. AIDS 26(5):559–566
M. Galukande, D.B. Sekavuga, K. Duffy, N. Wooding, S. Rackara, F. Nakaggwa, T. Nagaddya, A.E. Elobu, A. Coutinho, Mass safe male circumcision: early lessons from a Ugandan urban site-a case study. Pan Afr Med J 13:88 (2012).
Buwembo DR, Musoke R, Kigozi G, Ssempijja V, Serwadda D, Makumbi F, Watya S, Namuguzi D, Nalugoda F, Kiwanuka N (2012) Evaluation of the safety and efficiency of the dorsal slit and sleeve methods of male circumcision provided by physicians and clinical officers in Rakai Uganda. BJU Int 109(1):104–108
Frajzyngier V, Odingo G, Barone M, Perchal P, Pavin M (2014) Safety of adult medical male circumcision performed by non-physician clinicians in Kenya: a prospective cohort study. Global Health Sci Pract 2(1):93–102
Ngcobo S, Wolvaardt JE, Bac M, Webb E (2018) The quality of voluntary medical male circumcision done by mid-level workers in Tshwane District, South Africa: A retrospective analysis. PLoS ONE 13(1):e0190795
Galukande M, Kaggwa S, Sekimpi P, Kakaire O, Katamba A, Munabi I, Runumi FM, Mills E, Hagopian A, Blair G (2013) Use of surgical task shifting to scale up essential surgical services: a feasibility analysis at facility level in Uganda. BMC Health Serv Res 13(1):292
Baine SO, Kasangaki A, Baine EMM (2018) Task shifting in health service delivery from a decision and policy makers’ perspective: a case of Uganda. Hum Resour Health 16(1):20
Baine SO, Kasangaki A (2014) A scoping study on task shifting; the case of Uganda. BMC Health Serv Res 14(1):184
Dambisya YM, Matinhure S (2012) Policy and programmatic implications of task shifting in Uganda: a case study. BMC Health Serv Res 12(1):61
Muula AS, Prozesky HW, Mataya RH, Ikechebelu JI (2007) Prevalence of complications of male circumcision in Anglophone Africa: a systematic review. BMC Urol 7(1):4
Acknowledgements
Not applicable
Funding
This study was supported by the Infectious Diseases Research Collaboration (IDRC) under grant number 105968–001. The funder did not have any role in manuscript preparation.
Author information
Authors and Affiliations
Contributions
HKM coordinated and conceptualized the study. All authors (HKM, AB, KO, EL and SL) participated in data interpretation and writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Makerere University School of Medicine Research and Ethics Committee (Ref 2013–092). Written informed consent was obtained from each participant, and assent for all those below 18 years was obtained prior to their participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Matumaini, H.K., Batte, A., Otwombe, K. et al. Outcomes of voluntary medical male circumcision performed by medical doctors and non-doctor health workers in central Uganda. Afr J Urol 27, 55 (2021). https://doi.org/10.1186/s12301-021-00156-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-021-00156-8