Abstract
Physical exercise is recognized for its beneficial effects on brain health and executive function, particularly through the careful manipulation of key exercise parameters, including type, intensity, and duration. The aim of this systematic review and meta-analysis was to delineate the optimal types, intensities, and durations of exercise that improve cognitive functions in older adults with mild cognitive impairment (MCI) or dementia. A comprehensive search was conducted in Scopus, Web of Science, and PubMed from their inception until December 2023. The methodological quality and publication bias of the included studies were assessed using the PEDro scale and Egger’s regression test, respectively. Separate meta-analyses were performed to assess the overall impact of exercise on cognitive assessments and to explore the effects of different exercise types (i.e., aerobic, resistance, dual-task, mind-body, and multi-component exercises) and intensities (i.e., low, moderate, and high) on executive function. Results were presented as standardized mean differences (SMD) and 95% confidence intervals (95% CI). A meta-regression analysis was conducted to examine the correlation between exercise duration and mean effects. In total, 15,087 articles were retrieved from three databases, of which 35 studies were included in our final analyses. The results indicated high overall methodological quality (PEDro score = 8) but a potential for publication bias (t = 2.08, p = 0.045). Meta-analyses revealed that all types of exercise (SMD = 0.691, CI [0.498 to 0.885], p < 0.001) and intensities (SMD = 0.694, CI [0.485 to 0.903], p < 0.001) show significant effects favoring exercise. Notably, dual-task exercises (SMD = 1.136, CI [0.236 to 2.035], p < 0.001) and moderate-intensity exercises (SMD = 0.876, CI [0.533 to 1.219], p < 0.001) exhibited the greatest effect. No significant correlation was observed between exercise duration and SMD (R² = 0.038, p = 0.313). Overall, our meta-analyses support the role of physical exercise in enhancing executive function in older adults with MCI or dementia. It is essential to carefully tailor exercise parameters, particularly type and intensity, to meet the specific needs of older adults with MCI or dementia. Such customization is crucial for optimizing executive function outcomes and improving overall brain health.
Similar content being viewed by others
Introduction
With advancements in global medicine and healthcare, there has been a significant increase in average human life expectancy. This, combined with declining birthrates, has contributed to a growing aging population across developed and developing nations worldwide [1]. The World Health Organization (WHO) estimates that the global population over the age of 60 years would reach 2.1 billion by 2050 [2, 3]. Consequently, this demographic shift is associated with an increase in chronic neurodegenerative conditions such as mild cognitive impairment (MCI) and dementia, primarily affecting older adults [4,5,6,7]. Annually, the number of individuals affected by MCI and dementia increases, with an estimated 139 million people projected to live with dementia worldwide by 2025, as reported in the World Alzheimer Report (2023) [8]. Although physical and cognitive functions decline with age, it is important to recognize that MCI and dementia are not inevitable consequences of aging [9]. These conditions are characterized by abnormal changes in brain structure and function [10], resulting in significant declines in memory, language and communication skills, motor function, mood, and social behavior [11, 12]. To date, no pharmacological interventions have proven effective at reversing the progression of MCI or dementia [13,14,15]. Therefore, a combination of pharmacological and non-pharmacological approaches, including sleep, diet, physical, and cognitive exercises, have become crucial early strategies to mitigate cognitive decline in older adults.
Physical exercise is known to positively affect various bodily systems, including the musculoskeletal, cardiovascular, metabolic, and central nervous systems [16, 17]. Moreover, physical exercise influences the brain through mechanisms, such as increasing cerebral blood flow, upregulating neurotrophic factors (i.e., brain-derived neurotrophic factors and insulin-like growth factor-1) [18, 19], promoting the release of neurotransmitters (i.e., dopamine and serotonin), and enhancing muscle-brain interactions [20, 21]. Additionally, most exercises are performed socially, fostering interaction, collaboration, and pro-social behaviors among participants [22]. These social activities are likely to improve cognitive function and reduce social isolation in older adults [23].
While physical exercise is known to benefit brain health, identifying the optimal exercise parameters to maximize these benefits is a critical question. Like other bodily training, achieving neural adaptations from exercise necessitates careful consideration of parameters (type, intensity, and duration) when designing interventions [12, 24, 25]. Several types of exercise, such as aerobic [26], resistance [27], dual-task [28], multi-component [29], and mind-body exercises [30], are proven to enhance cognitive function. However, the mechanisms by which executive function is enhanced may vary among different types of exercise. For example, aerobic exercise enhances cardiorespiratory and cardiovascular function, potentially lowering the risk of vascular dementia and cognitive decline associated with cerebral small vessel disease [31, 32]. Resistance and dual-task training, emphasizing functional movement and balance, demand effective cognitive processing [28, 33,34,35]. Evidence also suggests an inverted U-shaped relationship between exercise intensity and cognitive function [20, 29, 36], where moderate intensity enhances arousal and cognitive performance, whereas high intensity might impair it due to overstimulation or fatigue (i.e., hyperarousal states) and/or fatigue [34, 36, 37]. However, this inverted U-shaped relationship between exercise intensity and executive function has largely been observed only in healthy populations under acute exercise situations.
Given the complexity and variety of criteria used to assess executive function in individuals with MCI or dementia, the precise mechanisms by which exercise parameters (i.e., exercise type, intensity, and duration) impact executive function in older adults with MCI and dementia are still not fully understood. Identifying and tailoring optimal exercise parameters is crucial to ensure older adults with MCI or dementia derive optimal benefits through physical exercise, which supports not only physical health but also brain and cognitive health. Therefore, this systematic review and meta-analysis aim to synthesize the existing literature on the effects of exercise on executive function in older adults with MCI or dementia, taking into account exercise moderators such as exercise type, intensity, and duration. The research questions guiding this systematic review and meta-analysis are as follows:
-
1.
Which type of physical exercise (i.e., aerobic, resistance, dual-tasking, and mind-body training) is most beneficial for executive function in older adults with MCI or dementia?
-
2.
Which physical exercise intensity level (i.e., low, moderate, and high) is most beneficial for improving executive function in older adults with MCI or dementia?
-
3.
What is the relationship between exercise duration and changes in executive function in older adults with MCI or dementia?
Methods
Study design and registration
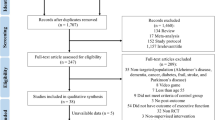
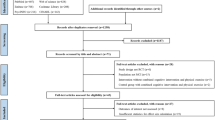
The systematic review and meta-analyses followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (Fig. 1) and is registered with the International Prospective Register of Systematic Reviews (XXX).
Literature search strategy
A systematic literature search was conducted using three databases: PubMed, Web of Science, and Scopus, from inception to December 2023. The search terms were collaboratively developed by the authors, drawing on recent systematic reviews related to similar topics. Keywords were derived using the PICO framework, which includes participant/patient, intervention, comparator/comparison, and outcomes. The search strings comprised terms such as: (‘Alzheimer’s disease’ OR ‘mild cognitive impairment’ OR ‘dementia’ OR ‘AD’ OR ‘MCI’) AND (‘Aerobic exercise’ OR ‘resistance exercise’ OR ‘dual-task training’ OR ‘cognitive-motor training’ OR ‘motor-motor training’ OR ‘strength training’ OR ‘physical training’ OR ‘cardiovascular exercise’ OR ‘Yoga’ OR ‘mind-body exercise’ OR ‘multicomponent exercise’ OR ‘Taichi’ OR ‘Baduanjin’) AND (‘executive function’ OR ‘cognitive function’ OR ‘cognitive abilities’ OR ‘working memory’ OR ‘inhibition’ OR ‘attention’). Furthermore, references from existing systematic reviews and meta-analyses, along with the studies included in these reviews, were examined to identify further relevant studies.
Study inclusion and exclusion criteria
Initially, 15,087 articles were retrieved from three databases and managed using the reference management software Covidence (Melbourne, Australia). After excluding 2,283 duplicates, 12,398 articles underwent screening based on titles and abstracts, resulting in 406 full-text articles. Following a detailed assessment, 371 articles were excluded, leaving 35 for inclusion in the systematic review and meta-analysis. Each article was independently evaluated by two researchers at each stage, with any disagreements resolved by discussion and consensus. The final list of included studies was approved by all authors, adhering to the following inclusion criteria:
-
1.
The study included older adults with Alzheimer’s disease and MCI;
-
2.
Interventions consisted of any organized exercise form (aerobic, resistance, dual-tasking, mind-body training), either acutely (single-session to < 8 weeks) or chronically (> 8 weeks);
-
3.
Studies employed a randomized control design, with the control group performing routine programs such as usual-care treatments, simple motion exercises, or stretching at low-intensity;
-
4.
Primary outcome measures were standardized cognitive neuropsychology assessment tests, such as but not limited to, the Mini-Mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA) [38], Alzheimer’s Disease Assessment Scale–Cognitive Subscale (ADAS-Cog) [39], or dual-tasking performance [40, 41].
-
5.
Articles had to be written in English and published as full-text in peer-reviewed journals.
Figure 1 depicts the study inclusion process, highlighting how studies were excluded based on irrelevant titles or abstracts failing to meet the inclusion criteria. When titles or abstracts were unclear, the complete article was subjected to review. The final selection of literature for discussion in the full text received unanimous approval from all authors. For additional details on the included studies, refer to Supplementary (S1).
Identifying exercise parameters
The primary objective of this study is to assess the impact of exercise parameters on executive function in older adults with MCI or dementia. For subgroup analyses in the meta-analysis, the exercise parameters examined included exercise type, intensity, and duration. The definitions for each exercise parameter were derived from the guidelines provided by the American College of Sports Medicine (ACSM) [42, 43], essential for classifying and specifying the type, intensity, and duration of exercise in each study. For instance, exercise types were categorized according to their primary movements and intended goals, as outlined below:
-
1.
Aerobic exercises: These involve continuous and sustained activity over a period of time that targets cardiovascular function including, but not limited to walking, jogging, cycling, or swimming.
-
2.
Resistance exercises: These focus on muscle strengthening and require pushing or pulling against a resistance provided by either a machine, free weight, resistance band, or bodyweight.
-
3.
Mind-body exercises: These emphasize the connection between meditation or mindfulness and physical movement, including Tai Chi, Qi Gong, Baduanjin, and Yoga.
-
4.
Dual-tasking exercises: These involve performing two different tasks simultaneously, such as combining a motor task with a cognitive task or performing two motor tasks together.
-
5.
Multicomponent exercises: These consist of performing two different types of exercises sequentially, either within a single session or across sessions. This could include combining aerobic exercises with resistance exercises or other forms of exercise.
Exercise intensity evaluation utilized a combination of objective, subjective, and descriptive measures [44], detailed as follows:
-
1.
Low: Exercise that did not noticeably increase breathing rate and had a low energy requirement (< 3 METs, < 55% HRmax, < 40% HRR, < 40% VO2max, PRE(C) < 10, PRE(C-R) ≤ 2) (METs: metabolic equivalents; HRmax: heart rate maximum; HRR: heart rate recovery; VO2max: maximum oxygen consumption; Borg’s RPE scales C = category scale [6–20] and C-R = category-ratio scale [0–10]).
-
2.
Moderate: Exercises that could be performed while maintaining an uninterrupted conversation and typically lasted between 30 and 60 min (3–6 METs, 55–70% HRmax, 40–60% HRR, 40–60% VO2max, PRE(C): 11–13, PRE(C-R): 3–4).
-
3.
High: Exercises that made it difficult to maintain an uninterrupted conversation and usually lasted less than 30 min (≥ 6 METs, ≥ 70% HRmax, ≥ 60% HRR, ≥ 60% VO2max, PRE(C) ≥ 14, PRE(C-R) ≥ 5).
Lastly, exercise duration was the product of the number of exercise sessions per week, the duration of each exercise session, and the total number of weeks. For example, an exercise program that includes 3 sessions per week for 18 weeks, with each session lasting 30 min, would have a total duration of 1620 min (30 min/session × 2 sessions/week × 8 weeks).
Methodological quality and bias assessment
Two reviewers evaluated the methodological quality of all studies using the Physiotherapy Evidence Database (PEDro) rating scale, which scores from 1 to 11. This scale assesses studies across five domains: group allocation, blinding, attrition, statistical analysis, and data variability. Ratings were assigned as “Yes” for supervised studies and “No” for items that were not applicable. Any discrepancies in ratings were resolved by a third reviewer. Methodological quality was categorized as Low (< 5), Good (6–8), and Excellent (9–10) [45].
Data extraction
All retrieved titles and abstracts were imported into the reference management software, Covidence (Melbourne, Australia). After duplicate removal, two researchers independently screened the study titles and abstracts to identify studies potentially relevant for full-text retrieval. The full texts of relevant studies were independently reviewed by two researchers, who also examined potentially relevant articles in the reference lists. Two researchers extracted study characteristics, including first author, country, year of publication, population, design, number of participants, details of intervention and control groups (type, intensity, duration), and outcome measures for motor and cognitive functioning. Discrepancies in study selection or data extraction were resolved through discussions with a third researcher, and authors were contacted for additional information as necessary. Extracted data included domain-specific cognitions, categorized by researchers, encompassing pre- and post-intervention stimuli and quantitative data for the control (sham) condition, derived from text, tables, and graphs in each included study.
Statistical analyses
Random effects meta-analyses were conducted to account for systematic influences and random errors between study-level effect sizes; results were displayed in forest plots showing averaged standardized mean differences (SMDs) and 95% confidence intervals (95%CI) [45, 46]. Positive SMD values signified that the intervention group outperformed the control group in cognitive tests for the outcome variables [46,47,49]. Separate meta-analyses on executive function outcome measures were carried out to investigate the impact of exercise on different outcomes. Subgroup meta-analyses were conducted to explore the relationship between exercise type and intensity and SMDs, as agreed upon a-priori to assess the influence of exercise parameters on executive functioning [50]. The exercise parameters considered for subgroup analyses included:
-
1.
Exercise type – Aerobic vs. resistance vs. mind-body vs. dual-task vs. multicomponent exercises;
-
2.
Exercise intensity – Low vs. moderate vs. high.
The I2 statistic was employed to assess statistical heterogeneity, with cut-off points corresponding to low (25%), moderate (50%), and high (75%) heterogeneity [51]. Funnel plots were used to evaluate publication bias via Egger’s regression test, where non-significant asymmetry suggested no bias [52]. Additionally, a meta-regression was performed to explore the effects of exercise duration on cognitive function, to determine whether exercise duration could predict the SMD of each study. All statistical analyses were performed using Comprehensive Meta-Analysis (V3.0, Biostat, Englewood, USA), with an alpha level of P < 0.05 to determine significance
Results
Overall studies
Thirty-five studies, spanning from 2010 to 2023 [6, 7, 12, 14, 15, 20, 24,25,26,27,28,29,30,31,32,33,34,35,36,37, 40, 41, 52,55,56,57,58,59,60,61,62,63,64,65], were included in the analysis, with 65% (n = 23) published after 2018 [7, 12, 14, 15, 20, 24, 28, 29, 31, 35,36,37, 40, 52,54,55,56,57,58,59, 63,64,65]. These studies targeted older adults with MCI, MD, or cognitive decline, involving sample sizes ranging from 27 to 280 participants, aged between 60 and 92 years, with a mean age of 75.09 ± 6.13 years (see Supplementary Table S1).
Figure 2 demonstrates the impact of physical exercise on executive function and various cognitive domains. Twelve clinical and cognitive scales were used for comparison, including the Alzheimer’s Disease Assessment Scale–Cognitive Subscale (ADAS-Cog, n = 5) [26, 33, 34, 59, 64], Montreal Cognitive Assessment/Cognitive Abilities Screening Instrument (MoCA/CASI, n = 18) [7, 12, 15, 20, 27,28,29, 31, 32, 35,36,37, 40, 52,54,55, 63, 65], Mini-Mental State Examination (MMSE, n = 14) [7, 24, 26, 27, 29, 30, 36, 53, 54, 57, 58, 60, 61, 65], Trail Making Test Part A & B (TMT A & B, n = 11) [12, 14, 20, 28, 33, 37, 52,54,56, 59], Immediate Recall/Working Memory (n = 5) [6, 14, 25, 34, 54], Delayed Recall (n = 4) [12, 34, 54, 62], Forward Digit Span (n = 4) [12, 20, 28, 33], Backward Digit Span (n = 3) [20, 28, 33], Verbal Fluency (n = 6) [6, 20, 37, 55, 60, 62], Symbol Digit Modalities Test (SDMT, n = 2) [34, 65], Digit Symbol Substitution Test (DSST, n = 2) [14, 37], and dual-tasking (n = 1) [41].
Our meta-analyses indicated significant improvements in ADAS-Cog (SMD = 0.353, CI [0.081 to 0.626], p = 0.011), MoCA/CASI (SMD = 1.086, CI [0.700 to 1.472], p < 0.001), MMSE (SMD = 1.047, CI [0.658 to 1.437], p < 0.001), TMT A & B(SMD = 0.635, CI [0.272 to 0.999], p = 0.001), delayed recall (SMD = 0.318, CI [0.045 to 0.592], p = 0.022), forward digit span (SMD = 1.162, CI [0.006 to 2.317], p = 0.049), backward digit span (SMD = 1.117, CI [-0.001 to 2.235], p = 0.050), verbal fluency (SMD = 0.793, CI [0.366 to 1.221], p < 0.001), and dual-tasking (SMD = 0.588, CI [0.003 to 1.173], p = 0.049). In contrast, immediate recall/working memory (SMD = 0.067, CI [-0.099 to 0.259], p = 0.463), SDMT (SMD = 0.157, CI [-0.320 to 0.633], p = 0.519), and DSST (SMD = 0.071, CI [-0.129 to 0.271], p = 0.487) did not demonstrate significant improvement.
Measure of methodological quality and publication bias
The methodological quality of the included studies, evaluated using the PEDro scale, was generally high, with an average score of 8 (Table 1) [66, 67]. However, most studies did not achieve blinding of both the subjects and the therapists administering the therapy. Additionally, 20 studies did not adequately report the concealment of subject group allocation, and 11 studies lacked reports on the blinding of assessors for at least one key outcome. Furthermore, Egger’s regression test indicated potential publication bias (t = 2.08, p = 0.045). The Duval and Tweedie’s trim and fill method revealed that the adjusted effect size, at an SMD of 0.68 [0.43 to 0.93], was slightly lower compared to the observed SMD of 0.82 [0.43 to 0.93] (as shown in Fig. 3) [68, 69].
Exercise types
The forest plot in Fig. 4 depicts how different types of exercise enhance executive function. Aerobic exercise emerged as the most common type (n = 9) [6, 15, 25, 26, 31, 32, 53, 61, 64], while resistance exercise was least common (n = 4) [27, 33, 34, 62]. Overall, all exercise types demonstrated a favorable impact on executive function (SMD = 0.691, CI [0.498 to 0.885], p < 0.001). Subgroup analyses revealed significant cognitive improvements across various exercises, including aerobic exercise (SMD = 0.684, CI [0.392 to 0.977], p < 0.001) [6, 15, 25, 26, 31, 32, 53, 61, 64], dual-task training (SMD = 1.136, CI [0.236 to 2.035], p = 0.013) [7, 14, 28, 35, 41], mind-body exercise (SMD = 0.599, CI [0.239 to 0.959], p = 0.001) [20, 30, 40, 54, 55, 58, 63], multi-component exercise (SMD = 0.992, CI [0.403 to 1.582], p = 0.001) [24, 29, 36, 37, 57, 59, 60], and resistance exercise (SMD = 0.502, CI [-0.052 to 1.056], p = 0.076) [27, 33, 34, 62], though no significant differences were observed between the exercise types. This was particularly evident as dual-task training exhibited the greatest enhancement in executive function, while mind-body exercise showed the least improvement.
Exercise intensity
Figure 5 depicts a forest plot that demonstrates the impact of exercise intensity on cognitive function, with separate groups for low- (n = 9) [20, 25, 30, 35, 40, 54, 55, 58, 63], moderate- (n = 18) [6, 7, 14, 15, 24, 26, 28, 29, 32, 33, 41, 53, 56, 57, 59, 61, 64, 65], and high-intensity (n = 6) [31, 34, 36, 37, 60, 62]. The study’s findings revealed significant enhancements in cognitive function across all exercise intensity levels, favoring the intervention group: low- (SMD = 0.602, CI [0.288 to 0.916], p < 0.001), moderate- (SMD = 0.876, CI [0.533 to 1.219], p < 0.001), and high-intensity (SMD = 0.549, CI [0.061 to 1.036], p = 0.027) exercises [7, 70], with no significant differences observed overall between the different exercise intensities.
Exercise duration
Based on our meta-regression analysis, our results showed that exercise duration was not a strong predictor of SMD (R2 = 0.0376, p = 0.313) (See Fig 6).
Discussion
In this systematic review and meta-analyses, the effects of physical exercise parameters, specifically exercise types, intensity, and duration on executive function in older adults with MCI or dementia were evaluated. The analysis produced four principal findings. First, the meta-analyses demonstrated that physical exercise positively influenced outcomes of standardized clinical tests such as the ADAS-Cog, MoCA/CASI, and MMSE, and most assessments of cognitive function, except for immediate recall, SDMT, and DSST measures. Second, all types of physical exercise (i.e., aerobic, resistance, dual-task, mind-body, and multi-component exercises) were found to enhance executive function, with dual-task exercises showing the greatest overall positive effect. Third, physical exercise performed at either low, moderate, or high-intensity resulted in significant improvements in cognitive and executive functioning, with moderate-intensity exercise yielding the greatest positive effects on executive function. Fourth, meta-regression analysis indicated no significant correlation between exercise duration and improvements in executive functioning [71]. The assessment of methodological quality and publication bias revealed that, although the overall quality of included studies was high, there was a potential for publication bias favoring studies reporting positive outcomes [72, 73]. Overall, our findings confirm the effectiveness of physical exercise in improving executive function in older adults with MCI or dementia, and highlight that careful consideration of exercise parameters, such as exercise type, intensity, and duration is essential to optimize executive function in older adults with MCI or dementia.
Methodological quality and publication bias
A total of 35 studies met the inclusion criteria for qualitative synthesis and quantitative meta-analyses. The average overall rating of these studies on the PEDro scale was 8, indicating high methodological quality [74, 75]. However, 4 categories on the PEDro scale (Category 3 – Subject allocation was concealed, Category 5 – Blinding of all subjects, Category 6 – Blinding of therapist administering the therapy, and Category 7 – Blinding of assessors administering at least one key outcome) had more than 50% of studies fail to meet these criteria. While lack of allocation concealment and blinding of subjects, therapists, and assessors can potentially bias outcomes, it is often difficult to employ a double-blinded study design for exercise trials, unlike drug trials where placebo drugs are available. To overcome the limitations of potential bias, a large proportion of included studies used active control groups, such as light stretching and exercise [20, 55], or health education programs [15] to control for environmental and social influences on cognitive and executive function that provided an added element of experimental rigor. In addition to assessing methodological quality, our analyses indicated potential publication bias, with most studies favoring the intervention group [76]. This phenomenon of potential publication bias favoring the intervention group is common in other fields of exercise science research, reflecting a systemic issue of publishing primarily successful findings [77]. However, including studies with null or negative results is essential for a comprehensive understanding of the true effects of exercise interventions on executive function outcomes. Notwithstanding the results from the Egger’s test indicating a possibility for publication bias, the adjusted SMD still indicated that the overall effect was large and in favor of the intervention condition.
Effects of physical exercise on measure of clinical neuropsychological and cognitive assessments
Our study demonstrated that physical exercise, regardless of type and intensity, positively impacted cognitive and executive function assessments. Specifically, the ADAS-Cog, MoCA/CASI, and MMSE demonstrated overall improvements following exercise, with the MoCA/CASI and MMSE showing the most significant enhancements compared to the ADAS-Cog. These results align with previous meta-analyses that employed similar outcome measures [78, 79]. Notably, the effects on the MoCA/CASI and MMSE were more pronounced than those on the ADAS-Cog. This is likely due to the higher number of studies utilizing MoCA and MMSE as assessment outcomes compared to ADAS-Cog. However, it is difficult to clearly ascertain why we see such large positive effects on these standardized neuropsychological assessments as they are often multi-dimensional, which assesses multiple domains of executive function to provide a composite score for diagnostic purposes.
To more accurately assess the impact of physical exercise on various cognitive functions, we conducted separate meta-analyses for each cognitive assessment. Our results revealed that physical exercise had the most significant effects on the TMT (i.e., a measure of visual searching, attention, and task-switching) and verbal fluency tests, compared to other cognitive measures such as immediate and delayed recall, forward and backward digit span, SDMT, DSST, and dual-tasking abilities [80]. While the outcomes of our findings may be influenced by the number of studies included for the TMT and verbal fluency domains, physical exercise could directly target the neural mechanisms underpinning these assessments. Both TMT and verbal fluency assessments require cognitive abilities, such as selective attention, inhibition, mental flexibility, response generation, and self-monitoring, which are likely to be specifically strengthened by physical exercise. Conversely, domains such as working memory may not be as significantly impacted. Although delayed recall, digit span, and dual-tasking also demonstrated positive effects from physical exercise, these were less pronounced due to fewer studies focusing on these areas [81, 82]. Research indicates that improvements in physical or cognitive functions are often specific to the type of training intervention used, with limited transfer to other cognitive domains [83]. Therefore, a targeted approach is crucial when selecting exercises to enhance cognitive and executive functions.
Exercise specificity: a focus on exercise type on cognitive and executive functioning
When considering exercise type as a moderator in our meta-analyses, our results indicated that all exercise modalities significantly benefited executive function in older adults with MCI or dementia. There is now ample evidence supporting that lifestyle interventions, particularly exercise, are among the most effective means to enhance brain health and function [84]. A key consideration for exercise is how it elicits neural and/or physiological adaptations that effect positive changes in executive functioning and behavior. In the meta-analyses, we identified five commonly used exercise types: aerobic, resistance, mind-body, multi-component, and dual-tasking. Aerobic exercises accounted for the largest proportion of studies included in this review, likely due to their ease of implementation and familiarity to older participants. Aerobic exercises also confer physiological benefits that support brain and cognitive health, improving cardiovascular and cardiometabolic functioning, which leads to better control of blood pressure [85], glucose metabolism [86], and cholesterol levels [87]. This, in turn, reduces the risk of cerebral small vessel disease, a major risk factor for vascular dementia, age-related cognitive declines, and strokes [88, 89]. Studies have shown that aerobic exercise upregulates the production of neurotrophic factors, such as brain-derived neurotrophic factor (BDNF), and neurotransmitters, such as dopamine and serotonin, which are essential for supporting neuroplasticity and brain function, particularly in older adults with MCI or dementia [90, 91, 92]. In resistance and dual-tasking exercises, the mechanisms of action for improving executive functioning may differ somewhat from aerobic exercises [93]. A key objective of resistance and dual-task training is not only to enhance neuromuscular function but also to develop functional movement proficiencies. These training types are designed to simulate daily activities and incorporate cognitive skills and strategic thinking, which lead to improved cognitive functioning [94, 95]. Unlike aerobic exercise, which creates a suitable physiological environment for optimal brain functioning, resistance and dual-task training directly targets cognitive processes [7, 27, 28]. Our findings showed that dual-tasking exercises had the greatest impact on cognitive outcomes [28], followed by multi-component exercises [29].
In multi-component exercises, unlike dual-task exercises which involve simultaneous motor and/or cognitive tasks, various types of exercises are performed sequentially within a session (e.g., 20 min of aerobic followed by 20 min of resistance training) or across sessions (e.g., aerobic exercise in one session and strength training in the next), aiming to combine benefits from different exercise modalities [96, 97]. These exercises, including aerobic, resistance, and mind-body exercises, aim to improve cardiovascular and neuromuscular functions [78]. It is unsurprising that multi-component exercise yielded higher effect sizes compared to single-type exercises. From a practical standpoint, multi-component exercise programs more closely represent real-world lifestyle programs that older adults are likely to engage in. More importantly, there are likely synergistic effects from combining various exercises. For example, a combination of aerobic exercise and dual-tasking is likely to result in better cardiovascular functioning (i.e., creating an optimal physiological environment) and strengthening of neural pathways involved with executive function, which are synergistic in nature. Indeed, studies combining physical exercise and cognitive training have reported greater effects of combined physical-cognitive training, as compared to either training method performed alone [98]. Finally, mind-body exercises such as Yoga, Taichi, Qigong, and Baduanjin have also been shown to significantly affect executive function. While the criteria for what constitutes mind-body exercises is still debated, a key component of mind-body exercise focuses on meditation during movement execution, which involves coordinating between breathing, body sense and awareness, and movement execution [20, 30, 58]. It is likely that the process of learning to coordinate these actions strengthens cognitive processes such as attention regulation, inhibition, and emotional regulation that are crucial for executive function.
Overall, when considering the effects of exercise type on executive functioning in older adults, it is important to acknowledge that physical exercise as a whole is beneficial for brain health and function. However, in response to our first research question of “Which type of physical exercise is most beneficial…”, a key consideration is determining the needs and capacity of older adults regarding physical exercise. The current consensus indicates that most exercise interventions adopt an aerobic approach, likely due to its functional nature, ease of administration, and widespread acceptability. However, as our findings demonstrate, other types of exercise are just as beneficial, and a multi-component approach may offer greater holistic benefits to support the cognitive, psychological, and physical health of older adults with MCI or dementia [99].
Exercise dosing: effects of exercise intensity and duration on executive functioning
Exercise intensity is another major consideration when examining the dosing effects and adaptations resulting from exercise. Like exercise type, all three exercise intensities significantly improved executive function, with moderate-intensity showing the greatest effect [70, 100]. Substantial evidence supports that even low-intensity physical activity benefits cardiovascular [78], cognitive [30], and psychological health [101]. However, the effects of physical exercise on physiological functions are often intensity-specific [102], necessitating increased intensity for greater adaptations. Although our findings revealed no significant differences in overall effect sizes among exercise intensities, studies using moderate-intensity exhibited the greatest overall effects compared to those using low or high intensities. This is consistent with previous meta-analyses where moderate exercise intensities elicited the largest effects on cognitive functioning markers [78, 103]. In acute or single-session studies, a commonly reported inverted-U relationship exists between exercise intensity and cognitive outcomes [104, 105]. These findings suggest the existence of an optimal exercise intensity range corresponding to moderate intensity [106]. This leads to optimal stimulation of psychological and physiological factors (i.e., arousal, hormone, and neurotransmitter production) that help to support cognitive functioning that, in turn, drives cognitive and behavioral changes. By contrast, low-intensity exercises are unlikely to provide sufficient stimulus to elicit physiological adaptations, while high-intensity or near-maximum exercises may induce fatigue and a heightened state of arousal (i.e., hyperfocality), which may limit the enactment and training of various cognitive processes. An additional consideration in our meta-analysis was that certain exercises, such as mind-body exercises, were mostly categorized as being low-intensity according to standard guidelines [40, 54, 55]. While this may potentially bias the distribution of exercise across the three exercise intensity categories, it also reflects the potential of such exercises, even at low intensities, to improve cognitive function in older adults with MCI or AD. Considering that older adults with MCI or AD are likely to have other comorbidities that would limit their ability to perform moderate or high intensity exercises, such low intensity exercises may offer a suitable alternative to improving cognitive functioning.
A surprising finding from our results was that we did not observe any clear relationship between exercise duration and the observed effects of the included studies. Initially, we expected a positive relationship between exercise duration and its effects, anticipating that longer exercise durations would show greater benefits. Several plausible explanations exist for this observation. First, changes in executive functioning are likely influenced by factors such as baseline executive functioning levels and age-related comorbidities (i.e., cardiovascular, metabolic, and musculoskeletal declines) in older adults [107, 108]. That is, the included studies have recruited participants of differing severity of cognitive impairments, with some studies recruiting older adults with MCI [32, 40, 41, 55], while other studies recruited AD [25, 26, 62], or a combination of both [64]. This is likely to influence the magnitude of change in executive functioning outcomes from the exercise intervention. Further, risk factors and comorbidities such as cerebral small vessel disease, diabetes, high cholesterol, and blood pressure are particularly common in older adults, which could have influenced the effects of exercise. Secondly, changes to executive functioning likely follow a time course throughout the intervention. Specifically, executive functioning improvements are typically rapid in the early stages of an intervention and plateau during later stages (i.e., diminishing returns) [54], complicating the identification of a clear association. However, this does not imply that longer interventions are counterproductive. While no clear relationships were established within our review’s constraints, longer interventions might demonstrate more pronounced effects on the long-term retention of executive functioning than immediately observed effects. Indeed, several long-term exercise RCTs have shown significant improvements and maintenance of cognitive function months after the intervention, an important outcome beyond the scope of this review [109, 110].
In response to our research questions on “Which exercise intensity is most beneficial…” and “What is the relationship between exercise duration and changes in executive function…”, our findings indicate that although all exercise intensities benefit executive functioning, moderate intensity exercises may elicit the greatest changes. However, it is important to note that the goal of physical exercise extends beyond improving executive functioning; other bodily functions may require varying levels of exercise intensity to realize potential benefits [111]. Furthermore, there appears to be no clear relationship between exercise duration and immediate changes in executive function post-intervention. However, this may be due to our inclusion criteria more than actual effects, and further investigation into the retention effects of physical exercise on executive functions is warranted.
Gaps in the literature and future directions
Based on our results, physical exercise significantly improves executive functioning in older adults with MCI or dementia. However, several limitations within our meta-analyses should be acknowledged. First, since our review focused on the immediate effects of exercise parameters on executive function, we were unable to address the follow-up or retention of executive functioning skills resulting from physical exercise. It is likely that manipulation of exercise parameters may also influence the retention of executive functioning, which is a significant aspect of neurorehabilitation. Second, we were unable to distinguish our findings based on whether physical exercises were performed individually or in a group setting. Group settings may be influenced by social factors, such as interpersonal interactions, which could affect executive function outcomes. Finally, although we analyzed the relationship between exercise duration and observed effects, other factors such as exercise volume (the total amount of work done across all sessions) may also influence executive function outcomes. However, standardizing the calculation of exercise volume across studies is challenging, given the diversity in the range, type, and nature of exercises performed.
The findings from this systematic review and meta-analysis provide conclusive evidence that physical exercise benefits executive function in older adults with MCI or dementia. While the cognitive benefits of physical exercise are clear, a deeper understanding of the neurophysiological mechanisms underlying these effects is necessary. Particularly, understanding the synergistic effects of combining various exercise modalities to augment executive function is a critical gap that needs addressing. Additionally, the success of any exercise intervention critically depends on adherence levels to exercise programs in real-world settings. Understanding the social and cultural beliefs towards physical exercise is crucial to identify barriers and facilitators of exercise adherence. Given that social barriers and facilitators are often influenced by sociodemographic factors, successful exercise program implementation must consider the socio-cultural context and beliefs where these programs are conducted.
Conclusion
Our systematic review and meta-analyses align with existing literature regarding the impact of physical exercise on executive function in older adults with MCI and dementia. It was noted that all forms of physical exercise are advantageous, emphasizing the importance of customizing exercise regimens to suit the individual needs and abilities of older adults. Understanding the mechanisms through which exercise enhances executive function is crucial for tailoring exercise programs for optimal results. While varying intensities of physical exercise have positive effects on cognitive function, moderate intensity levels may be most effective in improving executive functioning. Future research should delve deeper into the neurophysiological mechanisms and combined effects of different exercise modalities on executive function in older adults with MCI or dementia.
Data availability
All data and materials pertaining to this systematic review and meta-analysis is available upon request via the corresponding author.
References
Collaborators G, Ärnlöv J. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the global burden of Disease Study 2019. Lancet. 2020;396(10258):1160–203.
Gustavsson A, Norton N, Fast T, Frölich L, Georges J, Holzapfel D, Kirabali T, Krolak Salmon P, Rossini PM, Ferretti MT. Global estimates on the number of persons across the Alzheimer’s disease continuum. Alzheimer’s Dement. 2023;19(2):658–70.
World Health Organization. Ageing 2022. https://www.who.int/health-topics/ageing#tab=tab_1
Lu Y, Liu CJ, Yu DH, Fawkes S, Ma J, Zhang M, Li CB. Prevalence of mild cognitive impairment in community-dwelling Chinese populations aged over 55 years: a meta-analysis and systematic review. BMC Geriatr. 2021;21:1–16.
Roberts R, Knopman DS. Classification and epidemiology of MCI. Clin Geriatr Med. 2013;29(4):753–72.
Sugano K, Yokogawa M, Yuki S, Dohmoto C, Yoshita M, Hamaguchi T, Yanase D, Iwasa K, Komai K, Yamada M. Effect of cognitive and aerobic training intervention on older adults with mild or no cognitive impairment: a derivative study of the Nakajima project. Dement Geriatric Cogn Disorders Extra. 2012;2(1):69–80.
Tao MD, Liu HJ, Cheng JX, Yu CY, Zhao LL. Motor–cognitive interventions may effectively improve cognitive function in older adults with mild cognitive impairment: a randomized controlled trial. Behav Sci. 2023;13(9):737.
World Alzheimer Report. 2023: Reducing dementia risk: never too early, never too late. Alzheimer’s Disease International. Retrieved from https://www.alzint.org/resource/world-alzheimer-report-2023/
Pacifico D, Fiordelli M, Fadda M, Serena S, Piumatti G, Carlevaro F, Magno F, Franscella G, Albanese E. Dementia is (not) a natural part of ageing: a cross-sectional study on dementia knowledge and misconceptions in Swiss and Italian young adults, adults, and older adults. BMC Public Health. 2022;22(1):2176.
Jung Y, Damoiseaux JS. The potential of blood neurofilament light as a marker of neurodegeneration for Alzheimer’s disease. Brain. 2024;147(1):12–25.
Ward A, Arrighi HM, Michels S, Cedarbaum JM. Mild cognitive impairment: disparity of incidence and prevalence estimates. Alzheimer’s Dement. 2012;8(1):14–21.
Yu AP, Chin EC, Yu DJ, Fong DY, Cheng CP, HuX, Wei GX, Siu PM. Tai Chi versus conventional exercise for improving cognitive function in older adults: a pilot randomized controlled trial. Sci Rep. 2022;12(1):8868.
Livingston G, Sommerlad A, Orgeta V, Costafreda SG, Huntley J, Ames D, Ballard C, Banerjee S, Burns A, Cohen-Mansfield J. Dementia prevention, intervention, and care. Lancet. 2017;390(10113):2673–734.
Lee S, Harada K, Bae S, Harada K, Makino K, Anan Y, Suzuki T, Shimada H. A non-pharmacological multidomain intervention of dual-task exercise and social activity affects the cognitive function in community-dwelling older adults with mild to moderate cognitive decline: a randomized controlled trial. Front Aging Neurosci. 2023;15:1005410.
Song D, Doris SF. Effects of a moderate-intensity aerobic exercise programme on the cognitive function and quality of life of community-dwelling elderly people with mild cognitive impairment: a randomised controlled trial. Int J Nurs Stud. 2019;93:97–105.
Geda YE, Roberts RO, Knopman DS, Christianson TJ, Pankratz VS, Ivnik RJ, Boeve BF, Tangalos EG, Petersen RC, Rocca WA. Physical exercise, aging, and mild cognitive impairment: a population-based study. Arch Neurol. 2010;67(1):80–6.
Öhman H, Savikko N, Strandberg TE, Pitkälä KH. Effect of physical exercise on cognitive performance in older adults with mild cognitive impairment or dementia: a systematic review. Dement Geriatr Cogn Disord. 2014;38(5–6):347–65.
Erickson KI, Miller DL, Roecklein KA. The aging hippocampus: interactions between exercise, depression, and BDNF. Neuroscientist. 2012;18(1):82–97.
LLorens-Martín M, Torres-Alemán I, Trejo JL. Exercise modulates insulin-like growth factor 1-dependent and-independent effects on adult hippocampal neurogenesis and behaviour. Mol Cell Neurosci. 2010;44(2):109–17.
Li FZ, Harmer P, Fitzgerald K, Winters-Stone K. A cognitively enhanced online Tai Ji Quan training intervention for community-dwelling older adults with mild cognitive impairment: a feasibility trial. BMC Geriatr. 2022;76:22.
Suzuki T, Shimada H, Makizako H, Doi T, Yoshida D, Ito K, Shimokata H, Washimi Y, Endo H, Kato T. A randomized controlled trial of multicomponent exercise in older adults with mild cognitive impairment. PLoS ONE. 2013;8(4):e61483.
Shvedko A, Whittaker AC, Thompson JL, Greig CA. Physical activity interventions for treatment of social isolation, loneliness or low social support in older adults: a systematic review and meta-analysis of randomised controlled trials. Psychol Sport Exerc. 2018;34:128–37.
Singh NA, Clements KM, Singh MAF. The efficacy of exercise as a long-term antidepressant in elderly subjects: a randomized, controlled trial. Journals Gerontol Ser A: Biol Sci Med Sci. 2001;56(8):M497–504.
Uysal İ, Başar S, Aysel S, Kalafat D, Büyüksünnetçi AÖ. Aerobic exercise and dual-task training combination is the best combination for improving cognitive status, mobility and physical performance in older adults with mild cognitive impairment. Aging Clin Exp Res. 2023;35(2):271–81.
Yágüez L, Shaw KN, Morris R, Matthews D. The effects on cognitive functions of a movement-based intervention in patients with Alzheimer’s type dementia: a pilot study. Int J Geriatr Psychiatry. 2011;26(2):173–81.
Yang S, Shan C, Qing H, Wang W, Zhu Y, Yin M, Machado S, Yuan T, Wu T. The effects of aerobic exercise on cognitive function of Alzheimer’s disease patients. CNS Neurol Disorders-Drug Targets. 2015;14(10):1292–7.
Yoon DH, Kang D, Kim HJ, Kim JS, Song HS, Song W. Effect of elastic band-based high‐speed power training on cognitive function, physical performance and muscle strength in older women with mild cognitive impairment. Geriatr Gerontol Int. 2017;17(5):765–72.
Parial LL, Kor PPK, Sumile EF, Leung AYM. Dual-Task Zumba Gold for improving the cognition of people with mild cognitive impairment: a pilot randomized controlled trial. Gerontologist. 2023;63(7):1248–61.
Li L, Liu MJ, Zeng H, Pan L. Multi-component exercise training improves the physical and cognitive function of the elderly with mild cognitive impairment: a six-month randomized controlled trial. Annals Palliat Med. 2021;10(8):8919–29.
Li FZ, Harmer P, Liu Y, Chou L. Tai Ji Quan and global cognitive function in older adults with cognitive impairment: a pilot study. Arch Gerontol Geriatr. 2014;58(3):434–9.
Chang JD, Zhu WB, Zhang J, Yong LM, Yang M, Wang JB, Yan JG. The effect of Chinese square dance exercise on cognitive function in older women with mild cognitive impairment: the mediating effect of mood status and quality of life. Front Psychiatry. 2021;12:711079.
Greblo Jurakic Z, Krizanic V, Sarabon N, Markovic G. Effects of feedback-based balance and core resistance training vs. pilates training on cognitive functions in older women with mild cognitive impairment: a pilot randomized controlled trial. Aging Clin Exp Res. 2017;29(6):1295–8.
Lü JJ, Sun MY, Liang LC, Feng Y, Pan XY, Liu Y. Effects of momentum-based dumbbell training on cognitive function in older adults with mild cognitive impairment: a pilot randomized controlled trial. Clin Interv Aging. 2016;11:9–16.
Mavros Y, Gates N, Wilson GC, Jain N, Meiklejohn J, Brodaty H, Wen W, Singh N, Baune BT, Suo C, Baker MK, Foroughi N, Wang Y, Sachdev PS, Valenzuela M, Fiatarone Singh MA. Mediation of cognitive function improvements by strength gains after resistance training in older adults with mild cognitive impairment: outcomes of the study of mental and resistance training. J Am Geriatr Soc. 2017;65(3):550–9.
Rojasavastera R, Bovonsunthonchai S, Hiengkaew V, Senanarong V. Action observation combined with gait training to improve gait and cognition in elderly with mild cognitive impairment a randomized controlled trial. Dement Neuropsychologia. 2020;14(2):118–27.
Liu I, Lee W, Lin S, Chang S, Kao C, Cheng Y. Therapeutic effects of exercise training on elderly patients with dementia: a randomized controlled trial. Arch Phys Med Rehabil. 2020;101(5):762–9.
Rivas-Campo Y, Aibar-Almazán A, Rodríguez-López C, Afanador-Restrepo DF, García-Garro PA, Castellote-Caballero Y, Achalandabaso-Ochoa A, Hita-Contreras F. Enhancing cognition in older adults with mild cognitive impairment through high-intensity functional training: a single-blind randomized controlled trial. J Clin Med. 2023;12(12):4049.
Yu F, Nelson NW, Savik K, Wyman JF, Dysken M, Bronas UG. Affecting cognition and quality of life via aerobic exercise in Alzheimer’s disease. West J Nurs Res. 2013;35(1):24–38.
Yu F, Swartwood RM. Feasibility and perception of the impact from aerobic exercise in older adults with Alzheimer’s disease. Am J Alzheimer’s Disease Other Dementias®. 2012;27(6):397–405.
Hsieh C, Lin P, Hsu W, Wang J, Huang Y, Lim A, Hsu Y. The effectiveness of a virtual reality-based Tai Chi exercise on cognitive and physical function in older adults with cognitive impairment. Dement Geriatr Cogn Disord. 2019;46(5–6):358–70.
Hauer K, Schwenk M, Zieschang T, Oster P. Dual-task performances can be improved in patients with dementia: a randomized controlled trial. Neurology. 2010;74(24):1961–8.
Schmitz KH, Courneya KS, Matthews C, Demark-Wahnefried W, Galvão DA, Pinto BM, Irwin ML, Wolin KY, Segal RJ, Lucia A, Schneider CM, von Gruenigen VE, Schwartz AL. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. 2010;42(7):1409–26.
Haskell WL, Lee I, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081.
Norton K, Norton L, Sadgrove D. Position statement on physical activity and exercise intensity terminology. J Sci Med Sport. 2010;13(5):496–502.
Phatak VS, Smith GE, Locke D, Shandera-Ochsner A, Dean PM, Ball C, Gutierrez G, Chandler MJ. Computerized cognitive training (CCT) versus yoga impact on 12 month post intervention cognitive outcome in individuals with mild cognitive impairment. Brain Sci. 2021;11(8):988.
Sato K, Ochi A, Watanabe K, Yamada K. Effects of dance video game training on cognitive functions of community-dwelling older adults with mild cognitive impairment. Aging Clin Exp Res. 2023;35(5):987–94.
Roberts SSH, Teo W, Warmington SA. Effects of training and competition on the sleep of elite athletes: a systematic review and meta-analysis. Br J Sports Med. 2019;53(8):513–22.
Boulares A, Fabre C, Cherni A, Jdidi H, Gaied Chortane S, Trompetto C, Puce L, Bragazzi NL. Effects of a physical activity program that incorporates exercises targeting balance, strength, and proprioception on cognitive functions and physical performance in old adults with mild cognitive impairment. J Alzheimers Dis 2023; (96): 245–60.
Chobe S, Patra SK, Chobe M, Metri K. Efficacy of Integrated yoga and Ayurveda Rasayana on cognitive functions in elderly with mild cognitive impairment: non-randomized three-arm clinical trial. J Ayurveda Integr Med. 2022;13(1):100373.
Shimada H, Makizako H, Doi T, Park H, Tsutsumimoto K, Verghese J, Suzuki T. Effects of combined physical and cognitive exercises on cognition and mobility in patients with mild cognitive impairment: a randomized clinical trial. J Am Med Dir Assoc. 2018;19(7):584–91.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ-British Med J. 2003;327(7414):557–60.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ-British Med J. 1997;315(7109):629–34.
Hafsah Gul K, Zahoor A, Hafsah A, Kinza A. Effect of aerobic exercise on cognition in elderly persons with mild cognitive impairment. Rawal Med J. 2022;47(3):696–9.
Huang NY, Li WJ, Rong XJ, Champ M, Wei L, Li M, Mu HY, Hu YQ, Ma ZJ, Lyu JH. Effects of a modified Tai Chi program on older people with mild dementia: a randomized controlled trial. J Alzheimers Dis. 2019;72(3):947–56.
Khanthong P, Sriyakul K, Dechakhamphu A, Krajarng A, Kamalashiran C, Tungsukruthai P. Traditional Thai exercise (Ruesi Dadton) for improving motor and cognitive functions in mild cognitive impairment: a randomized controlled trial. J Exerc Rehabilitation. 2021;17(5):331–8.
Law LLF, Mok VCT, Yau MMK. Effects of functional tasks exercise on cognitive functions of older adults with mild cognitive impairment: a randomized controlled pilot trial. Alzheimers Res Ther. 2019;11(98):1–10.
Lee HJ, Lee M, Park H, Park JH, Park KW. The effect of multi-tasking exercise intervention on cognitive function in elderly and cognitive impairment patients: a pilot multicenter study. Dement Neurocognitive Disorders. 2019;18(4):122–9.
Siu M, Lee DTF. Effects of Tai Chi on cognition and instrumental activities of daily living in community dwelling older people with mild cognitive impairment. BMC Geriatr. 2018;18(37):1–10.
Thaiyanto J, Sittichoke C, Phirom K, Sungkarat S. Effects of multicomponent exercise on cognitive performance and fall risk in older women with mild cognitive impairment. J Nutr Health Aging. 2021;25(2):160–4.
Toots A, Littbrand H, Boström G, Hörnsten C, Holmberg H, Lundin-Olsson L, Lindelöf N, Nordström P, Gustafson Y, Rosendahl E. Effects of exercise on cognitive function in older people with dementia: a randomized controlled trial. J Alzheimers Dis. 2017;60(1):323–32.
Varela S, Ayán C, Cancela JM, Martín V. Effects of two different intensities of aerobic exercise on elderly people with mild cognitive impairment: a randomized pilot study. Clin Rehabil. 2012;26(5):442–50.
Vital TM, Hernandez SSS, Pedroso RV, Teixeira CVL, Garuffi M, Stein AM, Costa JLR, Stella F. Effects of weight training on cognitive functions in elderly with Alzheimer’s disease. Dement Neuropsychologia. 2012;6(4):253–9.
Xia R, Wan MY, Lin HY, Ye Y, Chen SJ, Zheng GH. Effects of mind-body exercise Baduanjin on cognition in community-dwelling older people with mild cognitive impairment: a randomized controlled trial. Neuropsychological Rehabilitation. 2023;33(8):1368–83.
Yu F, Vock DM, Zhang L, Salisbury D, Nelson NW, Chow LS, Smith G, Barclay TR, Dysken M, Wyman JF. Cognitive effects of aerobic exercise in Alzheimer’s disease: a pilot randomized controlled trial. J Alzheimers Dis. 2021;80(1):233–44.
Zhang Q, Zhu ML, Huang LL, Zhu M, Liu XL, Zhou P, Meng T. A study on the effect of traditional Chinese exercise combined with rhythm training on the intervention of older adults with mild cognitive impairment. Am J Alzheimer’s Disease Other Dementias®. 2023;38:1–12.
Sherrington C, Herbert RD, Maher CG, Moseley AM, PEDro. A database of randomized trials and systematic reviews in physiotherapy. Man Therap. 2000;5(4):223–6.
Verhagen AP, De Vet HC, De Bie RA, Boers M, Van Den Brandt PA. The art of quality assessment of RCTs included in systematic reviews. J Clin Epidemiol. 2001;54(7):651–4.
Sterne JAC, Egger M. Regression methods to detect publication and other bias in meta-analysis. Publication Bias in Meta-Analysis: Prevention, Assessment and adjustments. New York, USA: Wiley; 2006.
Lin LF, Chu HT, Murad MH, Hong C, Qu ZY, Cole SR, Chen Y. Empirical comparison of publication bias tests in meta-analysis. J Gen Intern Med. 2018;33:1260–7.
Sungkarat S, Boripuntakul S, Chattipakorn N, Watcharasaksilp K, Lord SR. Effects of Tai Chi on cognition and fall risk in older adults with mild cognitive impairment: a randomized controlled trial. J Am Geriatr Soc. 2017;65(4):721–7.
Cuijpers P, Smit F, Bohlmeijer E, Hollon SD, Andersson G. Efficacy of cognitive–behavioural therapy and other psychological treatments for adult depression: Meta-analytic study of publication bias. Br J Psychiatry. 2010;196(3):173–8.
Ioannidis JP, Munafo MR, Fusar-Poli P, Nosek BA, David SP. Publication and other reporting biases in cognitive sciences: detection, prevalence, and prevention. Trends Cogn Sci. 2014;18(5):235–41.
Schuch FB, Vancampfort D, Richards J, Rosenbaum S, Ward PB, Stubbs B. Exercise as a treatment for depression: a meta-analysis adjusting for publication bias. J Psychiatr Res. 2016;77:42–51.
Armijo Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the Cochrane collaboration risk of bias tool and the effective public health practice project quality assessment tool: methodological research. J Eval Clin Pract. 2012;18(1):12–8.
Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–21.
Ioannidis JP. Why most published research findings are false. PLoS Med. 2005;2(8):e124.
Ayorinde AA, Williams I, Mannion R, Song FJ, Skrybant M, Lilford RJ, Chen Y. Publication and related biases in health services research: a systematic review of empirical evidence. BMC Med Res Methodol. 2020;20(1):137.
Northey JM, Cherbuin N, Pumpa KL, Smee DJ, Rattray B. Exercise interventions for cognitive function in adults older than 50: a systematic review with meta-analysis. Br J Sports Med. 2018;52(3):154–60.
Biazus-Sehn LF, Schuch FB, Firth J, de Souza Stigger F. Effects of physical exercise on cognitive function of older adults with mild cognitive impairment: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2020;89:104048.
Hillman CH, Erickson KI, Kramer AF. Be smart, exercise your heart: exercise effects on brain and cognition. Nat Rev Neurosci. 2008;9(1):58–65.
Kramer AF, Colcombe S. Fitness effects on the cognitive function of older adults: a meta-analytic study—revisited. Perspect Psychol Sci. 2018;13(2):213–7.
Erickson KI, Hillman CH, Kramer AF. Physical activity, brain, and cognition. Curr Opin Behav Sci. 2015;4:27–32.
von Bastian CC, Belleville S, Udale RC, Reinhartz A, Essounni M, Strobach T. Mechanisms underlying training-induced cognitive change. Nat Reviews Psychol. 2022;1(1):30–41.
Law LL, Barnett F, Yau MK, Gray MA. Effects of combined cognitive and exercise interventions on cognition in older adults with and without cognitive impairment: a systematic review. Ageing Res Rev. 2014;15:61–75.
Cornelissen VA, Fagard RH. Effects of endurance training on blood pressure, blood pressure–regulating mechanisms, and cardiovascular risk factors. Hypertension. 2005;46(4):667–75.
Yardley JE, Kenny GP, Perkins BA, Riddell MC, Balaa N, Malcolm J, Boulay P, Khandwala F, Sigal RJ. Resistance versus aerobic exercise: Acute effects on glycemia in type 1 diabetes. Diabetes Care. 2013;36(3):537–42.
Nybo L, Sundstrup E, Jakobsen MD, Mohr M, Hornstrup T, Simonsen L, Bülow J, Randers MB, Nielsen JJ, Aagaard P. High-intensity training versus traditional exercise interventions for promoting health. Med Sci Sports Exerc. 2010;42(10):1951–8.
Liu-Ambrose T, Best JR, Davis JC, Eng JJ, Lee PE, Jacova C, Boyd LA, Brasher PM, Munkacsy M, Cheung W. Aerobic exercise and vascular cognitive impairment: a randomized controlled trial. Neurology. 2016;87(20):2082–90.
Chapman SB, Aslan S, Spence JS, DeFina LF, Keebler MW, Didehbani N, Lu HZ. Shorter term aerobic exercise improves brain, cognition, and cardiovascular fitness in aging. Front Aging Neurosci. 2013;5:75.
Park DC, Reuter-Lorenz P. The adaptive brain: aging and neurocognitive scaffolding. Ann Rev Psychol. 2009;60:173–96.
Wollesen B, Wildbredt A, van Schooten KS, Lim ML, Delbaere K. The effects of cognitive-motor training interventions on executive functions in older people: a systematic review and meta-analysis. Eur Rev Aging Phys Activity. 2020;17:1–22.
Gheysen F, Poppe L, DeSmet A, Swinnen S, Cardon G, De Bourdeaudhuij I, Chastin S, Fias W. Physical activity to improve cognition in older adults: can physical activity programs enriched with cognitive challenges enhance the effects? A systematic review and meta-analysis. Int J Behav Nutr Phys Activity. 2018;15:1–13.
Chow ZS, Moreland AT, Macpherson H, Teo WP. The central mechanisms of resistance training and its effects on cognitive function. Sports Med. 2021;51(12):2483–506.
Gavelin HM, Dong C, Minkov R, Bahar-Fuchs A, Ellis KA, Lautenschlager NT, Mellow ML, Wade AT, Smith AE, Finke C. Combined physical and cognitive training for older adults with and without cognitive impairment: a systematic review and network meta-analysis of randomized controlled trials. Ageing Res Rev. 2021;66:101232.
Zhu XY, Yin SF, Lang MJ, He RQ, Li J. The more the better? A meta-analysis on effects of combined cognitive and physical intervention on cognition in healthy older adults. Ageing Res Rev. 2016;31:67–79.
Borges-Machado F, Silva N, Farinatti P, Poton R, Ribeiro Ó, Carvalho J. Effectiveness of multicomponent exercise interventions in older adults with dementia: a meta-analysis. Gerontologist. 2021;61(8):e449–62.
Baker MK, Atlantis E, Fiatarone Singh MA. Multi-modal exercise programs for older adults. Age Ageing. 2007;36(4):375–81.
Lauenroth A, Ioannidis AE, Teichmann B. Influence of combined physical and cognitive training on cognition: a systematic review. BMC Geriatr. 2016;16:1–14.
Lautenschlager NT, Cox KL, Flicker L, Foster JK, Van Bockxmeer FM, Xiao J, Greenop KR, Almeida OP. Effect of physical activity on cognitive function in older adults at risk for Alzheimer disease: a randomized trial. Jama-Journal Am Med Association. 2008;300(9):1027–37.
Balducci S, Zanuso S, Cardelli P, Salvi L, Bazuro A, Pugliese L, Maccora C, Iacobini C, Conti FG, Nicolucci A. Effect of high-versus low-intensity supervised aerobic and resistance training on modifiable cardiovascular risk factors in type 2 diabetes; the Italian diabetes and Exercise Study (IDES). PLoS ONE. 2012;7(11):e49297.
Shepherd SO, Wilson OJ, Taylor AS, Thøgersen-Ntoumani C, Adlan AM, Wagenmakers AJ, Shaw CS. Low-volume high-intensity interval training in a gym setting improves cardio-metabolic and psychological health. PLoS ONE. 2015;10(9):e139056.
Gibala MJ, Little JP, MacDonald MJ, Hawley JA. Physiological adaptations to low-volume, high‐intensity interval training in health and disease. J Physiol. 2012;590(5):1077–84.
McMorris T, Hale BJ. Differential effects of differing intensities of acute exercise on speed and accuracy of cognition: a meta-analytical investigation. Brain Cogn. 2012;80(3):338–51.
McMorris T, Sproule J, Turner A, Hale BJ. Acute, intermediate intensity exercise, and speed and accuracy in working memory tasks: a meta-analytical comparison of effects. Physiol Behav. 2011;102(3–4):421–8.
Nanda B, Balde J, Manjunatha S. The acute effects of a single bout of moderate-intensity aerobic exercise on cognitive functions in healthy adult males. J Clin Diagn Res. 2013;7(9):1883–5.
McMorris T, Hale BJ, Corbett J, Robertson K, Hodgson CI. Does acute exercise affect the performance of whole-body, psychomotor skills in an inverted-U fashion? A meta-analytic investigation. Physiol Behav. 2015;141:180–9.
Donnezan LC, Perrot A, Belleville S, Bloch F, Kemoun G. Effects of simultaneous aerobic and cognitive training on executive functions, cardiovascular fitness and functional abilities in older adults with mild cognitive impairment. Ment Health Phys Act. 2018;15:78–87.
Sanders LM, Hortobagyi T, la, Bastide-van Gemert S, van der Zee EA, van Heuvelen MJ. Dose-response relationship between exercise and cognitive function in older adults with and without cognitive impairment: A systematic review and meta-analysis. PLoS One. 2019; 14(1): e210036.
Maaß A, Düzel S, Goerke M, Becke A, Sobieray U, Neumann K, Lövdén M, Lindenberger U, Bäckman L, Braun-Dullaeus R. Vascular hippocampal plasticity after aerobic exercise in older adults. Mol Psychiatry. 2015;20(5):585–93.
Ten Brinke LF, Bolandzadeh N, Nagamatsu LS, Hsu CL, Davis JC, Miran-Khan K, Liu-Ambrose T. Aerobic exercise increases hippocampal volume in older women with probable mild cognitive impairment: a 6-month randomised controlled trial. Br J Sports Med. 2015;49(4):248–54.
Voss MW, Vivar C, Kramer AF, van Praag H. Bridging animal and human models of exercise-induced brain plasticity. Trends Cogn Sci. 2013;17(10):525–44.
Acknowledgements
The authors thank the authors contacted who provided data and/or information about their published work.
Funding
No funding was received for the conduct of this review.
Author information
Authors and Affiliations
Contributions
WX Chen contributed to planning, literature search, data extraction, data analysis, and writing of the manuscript. J S-P Leuk contributed to data analysis and editing of the manuscript. YH Wu contributed to literature search, data extraction, data analysis, and editing of the manuscript. N Huang contributed to data analysis and editing of the manuscript. WP Teo contributed to planning, data analysis, and editing of the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
All authors declare that they do not have any competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, W., Siew-Pin, J.L., Wu, Y. et al. Identifying exercise and cognitive intervention parameters to optimize executive function in older adults with mild cognitive impairment and dementia: a systematic review and meta-analyses of randomized controlled trials. Eur Rev Aging Phys Act 21, 22 (2024). https://doi.org/10.1186/s11556-024-00357-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s11556-024-00357-4