Abstract
Background
The ability to walk is an important indicator of general health and mobility deficits have wide-ranging economic implications. We undertook a systematic review to elucidate the impact of walking parameters on health care costs.
Methods
Publications reporting on associations between health care costs and walking parameters were identified by a systematic literature search in MEDLINE, Embase, and manual reference screening, following the PRISMA reporting guidelines. First, titles and abstracts were screened by two independent reviewers followed by a review of the full articles if they met the inclusion criteria. Costs were converted to US-Dollars with inflation adjustment for 2021. A narrative synthesis was performed.
Results
Ten studies conducted between 2001 and 2021 fulfilled the inclusion criteria. Assessment of walking ability was carried out via patient reported outcomes, performance tests, or using wearable digital devices. Walking more than one hour per day, a faster walking speed and the ability to walk without impairments are associated with significant lower health care costs. A higher number of steps per day is associated with significant lower costs in two simulation studies, while in the study using a digital device, taking more than 10,000 steps per day is not significantly associated with lower direct costs. The heterogeneity of mobility assessments and of economic analyses both precluded a quantitative synthesis.
Conclusion
Cross-sectional and observational studies from this systematic review suggest a significant association of better walking performance with lower health care costs. Future health economic research and health technology assessments should use quantifiable mobility outcomes when evaluating new drugs or non-pharmacological interventions.
Similar content being viewed by others
Introduction
Walking ability has emerged as important indicator of general health and has even been proposed to be a ‘vital sign’ [1, 2]. Significant correlations between walking parameters (e. g. gait speed or sedentary time) and health outcomes such as mortality, morbidity, and quality of life have been established in recent years [3,4,5]. For example, taking more steps per day is associated with progressively lower all-cause mortality for young-middle age adults as well as for older adults [6]. In hip fracture patients, the ability to walk is a strong indicator of long-term survivorship [7], and Parkinson's disease patients with disturbed movement and physical impairments more likely experience falls [8]. Walking related adverse events (e.g. falls, admissions to care homes and hospitalisation), are recognized as crucial drivers of the costs of patient management [9, 10].
Walking ability covers a meaningful aspect of health and reflects how a patient functions in daily life. As such, it represents an important outcome for studies on health-prevention and on effects of rehabilitation or surgery. Nonetheless, in the area of pivotal clinical trials, which are essential stages in drug development and marketing authorisation of new medicines, we have shown that assessments of walking parameters are not routinely included [11]. This is regrettable, since improvement in walking performance, in addition to disease-specific clinical efficacy and safety, represents a patient-relevant benefit. A positive effect of a new drug on the patients’ walking performance could also strengthen the manufacturer position in health technology assessments (HTA) or reimbursement negotiations. The constrained budgets of most national health systems mandate a careful allocation of health resources, and improvement or worsening in walking ability as a consequence of treatment could be an interesting additional variable in economic models for cost-effectiveness and cost utility analyses. Yet, a better understanding is still needed of how walking ability and costs are linked at the patient level and which parameters are the best estimators for costs.
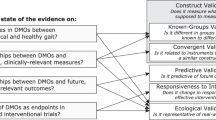
At present, clinical trials assess walking most often as a part of generic quality of life questionnaire scores (e. g. EQ-5D, SF-36) which include some components/questions concerning mobility [11]. Tangible information on actual walking status is difficult to derive from the summary scores. Conventional performance outcomes measuring walking-related mobility (e. g. the 6-min walking distance) may suffer from other limitations, e.g. a moderate external validity [12]. Developments in digital technology have opened up the way for comprehensive real-world measurements of mobility including walking volume, pace, variability, asymmetry and phases [13]. Although the first steps have already been taken to establish walking performance as endpoints in clinical trials (for example using stride velocity as a secondary endpoint in Duchenne Muscular Dystrophy [14]), validation of these novel digital mobility outcomes (DMOs) is an important prerequisite. Mobilise-D (https://www.mobilise-d.eu) [15], an EU-funded collaborative project of academia and industry, is dedicated to promote the acceptance of DMOs by regulatory authorities as endpoints in clinical trials, and by implication its use in labelling and marketing of new medicines.
The role of assessing walking ability for the analysis or prediction of health care expenditure is currently not well understood, as is its potential contribution to economic evaluations of new interventions. The present study aims to identify and synthesize the available primary literature investigating the specific association of walking parameters (conventional and digital) and health care costs.
Methods
This systematic review was conducted according to the Centre for Reviews and Dissemination’s Guidance for undertaking reviews in healthcare, with adherence to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines [16]. The review has been registered in PROSPERO, the international database of prospectively registered systematic reviews (CRD42021261443).
Eligibility criteria
Eligibility criteria were defined using the PICO scheme (see appendix). The population was not restricted to specific indications, ages, gender or geographic location. This review only includes studies assessing the economic consequences of mobility in terms of health care costs. We specifically focused on walking-related mobility parameters including gait speed, walking speed, or the number of steps, among others. Vector magnitude units per minute (VMU) or energy expenditure which are not necessarily derived from walking and questionnaires evaluating additional activity parameters at the same time were excluded. Studies that examined relationships between mobility and quality of life or further clinical factors (e. g. falls or mortality, which could have implications on health care costs), but did not assess economic consequences directly, were excluded. A PRISMA flow chart shows the study selection process, also giving reasons for exclusion (Fig. 1).
Information sources and search strategy
MEDLINE and EMBASE were searched for relevant primary research publications published from database inception until November 2022. The search was supplemented by manual reference screening and cross-referencing. The search strategy comprised two main constructs that refer to walking-related mobility outcomes and the economic implications. The main keywords “mobility”, “walking speed”, and “cost” were searched without restriction, thus not limiting the search strategy to the type of (cost) analysis. Additional search terms included in the search strategy were confined to the title. The search was restricted to studies of human subjects, written in the English language. Editorials, letters, historical articles, abstracts, and reviews were excluded. The full search strategy is presented in the Appendix.
Study selection
Two reviewers (MW, SJ) independently screened titles of all identified studies. If either reviewer considered a study to meet the inclusion criteria, its abstract was then screened independently. Upon agreement on inclusion, full texts were retrieved and reviewed independently. Disagreements were resolved in discussions with a third reviewer (MZ). Data merging, deduplication and screening was performed with the open source R package revtools [17].
Data extraction
Data were extracted from selected studies for the following study characteristics: author and year, title of publication, country of investigation, study perspective and comparators, study population and disease area, study design, database and sample size, type of medication, and cost results distributed across sectors (e. g. inpatient, outpatient, emergency, prescriptions, total costs) where reported. To facilitate comparison across studies, all costs from different country sources were inflated to corresponding values for the year 2021, using local inflation rates. These were converted to US dollars (USD) values based on 2021 end of year exchange rates published by the US Federal Reserve [18].
Quality of reporting assessment
We assessed the reporting quality of studies following on the basis of the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) guideline [19] Given that studies are very heterogeneous and do not completely meet type of studies for which CHEERS was initially implemented (cost evaluations of health interventions), individual items from the checklist were adopted based on the notation by Rothfuss et al. [20] (Table 1).
Results
Search results
Results are presented as statistically significant differences of costs in individual studies. Due to heterogeneity in types of cost outcomes, settings, and disease areas, it was not appropriate to synthesize the results or conduct a meta-analysis of the economic findings. The initial search strategy yielded 2,771 titles after the elimination of duplicates. For the final qualitative synthesis, ten studies were included. These studies were conducted in Japan (n = 4), United States (n = 3), Brazil (n = 1), Italy (n = 1), and Germany (n = 1).
Study characteristics
Studies were conducted between 2001 and 2021. Detailed information on the individual studies is shown in Table 2. Six studies were observational cohort studies [21,22,23, 28, 29], two were cross-sectional studies [25, 27], one was a decision analysis using a Markov Model [24], and one was a microsimulation [26]. All studies (n = 10) examined the economic impact of mobility in middle-aged to aged populations. All studies focused on direct healthcare costs (including total costs but also costs by individual health sector).
The description of the source of cost data and the calculation of costs varied considerably across studies. A detailed description was absent in one study [28] but it can be assumed that estimates of hospitalization rates were based on a regional Health Service Registry. Outpatient/emergency room visits or inpatient hospital stays were gathered from institutional electronic health records [21, 25, 29], or insurance databases [22, 23]. Karl et al. [27] directly questioned patients. Hirai et al. [30] used data from the Japan Gerontological Evaluation Study (JAGES), which collected information about the costs from the municipalities that also act as insurers. Kato et al. estimated costs from public statistical data in Japan [24] and the microsimulation study by Kabiri et al. used THEMIS (The Health Economic Medical Innovation Simulation) to estimate how mobility improvements affect medical expenditures through monetized quality adjusted life years including data from MEDICARE, and MEDICAID [26].
Quality of reporting
The assessed quality of reporting is shown in Table 1. All publications outlined the background adequately to understand the research need and the research question. All studies reported cost differences due to a change in walking parameters. Costs that should be included in an analysis depend on the study perspective (refers to the point of view one takes when assessing costs), so failing to state the perspective meant that some of these studies lacked a clear rationale for the types of cost included. Five studies [24, 26, 28, 29] did not adjust costs that occurred at different points in time, and two studies [23, 26] conducted a sensitivity analysis to address a certain variety of their assumptions.
Reported results
Cost results are shown in Table 3. Perkins A, Tsuji I, Purser JL, Kato M, Turi B, Kabiri M. [21,22,23,24,25,26, 28, 29] reported that lower levels of walking ability were associated with higher health care expenditure, and one study [27] reported no statistically significant association between mobility and health care costs. Six studies reported additional associations between walking parameters and health care utilisation [21,22,23, 26, 28, 29].
Methods used to assess walking ability
The majority of walking assessments consisted of patient-reported outcomes (PROs) collected via questionnaires. These assessments included the following parameters: walking time [21, 22], and walking during leisure time as part of activities of daily life [25]. Specifically, Perkins et al. examined walking time by documenting the minutes of walking per week, using a newly developed questionnaire [21]. Tsuji et al. obtained mobility data from a survey conducted in 1994, which included a question on walking time asking how long on average patients walk a day [22]. Hirai et al. assessed walking time per day with a single question (“How long do you walk a day, on average?”). The time spent walking was categorized as > 60 min, 30–60 min, and less than 30 min per day. Turi et al. assessed walking during leisure time by using the section ‘physical activity during leisure-time’ of the ‘Baecke12’ questionnaire [25]. Walking ability was also assessed by determining walking speed using performance tests. Purser et al. used the Reubens Physical Performance Test, a supervised performance test [23]. Walking speed was examined by Bonnini et al. using a 1-km treadmill-walking test [28], and by Okayama et al. using the Endurance shuttle walk test [29]. Simulation studies did not assess walking directly. They furthermore examined quantitative risk reduction by walking derived from published studies to calculate the steps taken in their cost simulations [24, 26]. The study by Karl et al. measured the number of steps with a portable accelerometer device (Actigraph GT3X) [27].
Association with health care costs
Walking time and leisure-time walking
In a cohort of community-dwelling adults older than 55 years, Perkins et al. found an association between self-reported walking time of 120 min a week or more, and a significant decrease in emergency room visits and hospital stays in the following year. Annual total ($1,856 vs $6,266 $), inpatient ( $1,184 vs $4,872), and emergency room costs ($253 vs $762) were less for those reporting 60 or more minutes of walking per week compared to those reporting less than 60 min of walking per week [21]. In a four-year-long prospective cohort study in Japanese men and women, aged 40–79 years, Tsuji et al. found that medical costs ($86 vs. $97) were 12% significantly lower per capita and month, for subjects walking for more than one hour/day than for those walking less than one hour/day [22]. Hirai et al. reported that time spent walking was negatively associated with the cumulative costs of long-term care insurance. These cumulative costs were significantly higher in those who walked for less than 30 min than in those who walked for more than 60 min. Turi et al. reported the association of self-reported walking during leisure time with total healthcare expenditure during one year prior to the date of the interview in Brazilian patients (randomly selected users of the Brazilian National Health System) aged ≥ 50 years. Individuals who ‘always walked’ were 41% less likely to be in the highest 25% quantile (an indicator of high expenditure) of incurred health-care cost when compared to individuals who ‘never walked ‘ [25] (Table 2).
Walking speed
In a frail population of hospitalised medical or surgical patients older than 65 years, Purser et al. found that when the baseline walking speed was 0.10 m/s higher, this was associated with $1,334 lower 1-year costs during the index hospitalization [23]. Bonnini et al. conducted an intervention study to evaluate the effects of an unsupervised home program in patients with cardiovascular disease, consisting of 30–60 min of brisk walking at least 3–4 days per week over 3 years, on rates of hospitalization. Between four and six years after baseline, a significant lower hospitalization rate was observed in patients that had highly improved their walking speed compared to those who had only improved their walking speed to a low extent. This resulted in an average cost reduction per patient between high and low improvers in walking between $489 and $882 [28]. Okayama et al. prospectively enrolled patients aged ≥ 70 years with advanced non-small-cell lung cancer to investigate the association of pre-treatment walking capacity with hospitalization rates and medical costs. During the first year of initial therapy, medical costs (the actual revenue the hospital was paid from the health insurance funds) did not differ between less and more mobile groups, but significantly higher additional inpatients costs ($8,076 per person) were reported for the less mobile group [29].
Number of steps
Karl et al. investigated direct medical costs of patients aged between 48 to 68 years. They used cross-sectional data of the population in the German KORA FF4 study. In a subsample of patients for whom daily step count was reported there was no statistically significant difference in costs between those who walked more than 10,000 steps per day and those who did not [27]. Kato et al. 2013 used a Markov model to simulate costs over 10 years for middle-aged Japanese patients with diabetes. They estimated that total medical costs could be 5.2% and 8.4% lower for daily step count increases of 3,000 and 5,000, respectively [24]. Kabiri et al. conducted a microsimulation study of patients aged ≥ 51 years with osteoarthritis, and reported that 554 steps more per day would be associated with a 0.9% reduction in total medical expenditure [26].
Discussion
Loss of walking-related mobility has an impact on the risk of mortality (most recently Maurice et al. [31]), morbidity, and quality of life, especially in older people, and the association of mobility with readmissions and falls is well reported [3,4,5, 32]. The costs of impaired walking ability is a major burden for national health systems. Despite this, the observation from Macera nearly 20 years ago, that ‘quantitative data to make the case that medical care costs are lower among individuals who walk than those who do not is scarce’ [33], still holds in 2022.
In this systematic review, we identified ten studies, most of them recent, that reported a relationship between walking ability and health care costs. With one exception, all studies indicated that better walking performance is associated with significantly lower health care costs. Although it is difficult to derive causal relationships from retrospective studies, the results show that maintaining walking ability can be economically beneficial. It also implies that the accurate measurement and assessment of walking ability could be important. In this regard, this review showed clearly that the calculation and reporting of costs varied considerably between studies. Greater standardisation of cost outcomes would have been needed to allow for a comparison of results in a quantitative synthesis (meta-analysis). In addition, methodically different approaches were used to associate walking ability with monetary values. Further heterogeneity was introduced by the use of different sources of cost data: there was a mix of information from institutional electronic health records, insurance databases, direct questionnaires, and other sources.
In our analysis, we focused on quantitative walking measures, e.g. walking speed, walking distance or the number of steps to enable consistency in decisions regarding the inclusion of studies. Yet, the quantification of walking performance using retrospective questionnaires, as employed in a sizeable part of the included studies, suffers from recall bias and may impact the reported associations with health care costs. For some time now, walking outcomes can be recorded by devices such as mobile phones and wristbands or watches, but in this review, we could include only one study which used such a digital mobility outcome [27]. DMOs can record how a patient functions in the real world, and thus cover a meaningful aspect of health. Assuming that they can be shown to meet necessary requirements in terms of reliability, consistency, sensitivity to change and accuracy [34], they are increasingly recognized as having the potential to contribute important endpoints in clinical trials [14].
Not only clinical but also health economic studies would benefit from the availability of DMOs. Due to their high reliability, accuracy, and simple acquisition, DMOs could be used as a tool for HTA and economic evaluation where cost models could relate a change in the walking ability (e. g. walking speed or number of steps taken) to a monetary value. HTA reports could include the value of the expected cost reduction through improved mobility in cost-effectiveness or cost-utility analyses of new interventions. In such analyses, the willingness to pay threshold is used as an economic decision criterion but the ratios set are often not based on scientific evidence [35]. Future research approaches could address the question of the individual or societal willingness to pay for maintaining certain walking-related mobility levels. Some existing limitations of cost–benefit analysis could be addressed with precise and validated correlations of monetary values and health outcomes such as walking performance and clinically predicted manifestations. Taken together, the use of the association of costs and walking outcomes could become more relevant for health policy research, HTA, budget impact calculations for health insurance companies and the negotiation of reimbursement prices. DMOs may also be of value in the context of generating real-world evidence for monitoring actual costs of therapy.
Some limitations to our review apply. Our systemic literature search includes the most relevant databases (PUBMED and EMBASE) for primary research publications in the field of health economic studies, but did not include reviews by HTA bodies or governmental reports. A search in NHSEED and DARE database was not included as these have been discontinued. The search strategy used the main keywords “mobility”, “walking speed”, and “cost” without restriction, while including additional search terms with a title search only. We acknowledge that publications might have been missed that did not include either of those elements in the title. Yet, the framework of the CHEERS checklist clearly recommends that cost analyses should already be identifiable as such in the title. It should also be mentioned that several studies could not be included in the results although they reported cost effects related to general physical activity. In these cases, it was not possible to explicitly extract walking-related mobility outcomes. Moreover, the reported cost effects are based on direct health care costs, originating from different sectors and payers. This means that the studies are very heterogeneous and our review provides no information about the relationship of walking ability to costs beyond this perspective (e.g., indirect costs due to the loss of productivity). Although cost values were converted to USD and inflated to 2021 equivalent values, data were collected in different countries, at various points in time, and against a background of different health care settings. The presence/absence of chronic conditions varied between studies and most of the studies included enrolled middle-aged to older populations. As a consequence, this review cannot inform about the association of walking ability and health care cost in young individuals.
Conclusion
Our systematic review demonstrates the specific relevance of walking-related mobility for health care costs. Regardless of the type of assessment of walking ability (walking time, leisure-time walking, walking speed, number of steps), the studies show that better walking ability was significantly associated with lower health care costs. Future health economic research and health technology assessments should use quantifiable mobility outcomes when evaluating new drugs or non-pharmacological interventions. Walking parameters such as number of steps or walking speed appear to be particularly well suited for use in economic cost evaluations due to their scalability. They might help to quantify the monetary value of a new therapy in terms of improvement in walking performance as an additional source of information. Further studies are needed, starting with a clear prospective definition of the mobility outcome and greater standardisation of the costing perspective, study design, and analyses. In the future, digital mobility outcomes can provide objective measures of walking ability to inform health technology assessments and payer’s decisions more reliably.
Availability of data and materials
For all inquiries regarding data access, please contact the corresponding author.
References
Laugesen SKN, Nissen SK, Kellett J, Brabrand M, Cooksley T, Nickel CH. Impaired Mobility, Rather Than Frailty. Should Be a Vital Sign Chest. 2019;155:877–8.
Middleton A, Fritz SL, Lusardi M. Walking speed: the functional vital sign. J Aging Phys Act. 2015;23:314–22.
Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait Speed and Survival in Older Adults. JAMA. 2011;305:50–8.
Perera S, Patel K, Rosano C, Rubin S, Satterfield S, Harris T, et al. Gait Speed Predicts Incident Disability: A Pooled Analysis. J Gerontol A Biol Sci Med Sci. 2016;71:63–71.
Ekelund U, Tarp J, Steene-Johannessen J, Hansen B, Jefferis B, Fagerland MW, et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis. BMJ. 2019;366:l4570.
Saint-Maurice PF, Troiano RP, Bassett DR, Graubard BI, Carlson SA, Shiroma EJ, et al. Association of Daily Step Count and Step Intensity With Mortality Among US Adults. JAMA. 2020;323:1151.
Iosifidis M, Iliopoulos E, Panagiotou A, Apostolidis K, Traios S, Giantsis G. Walking ability before and after a hip fracture in elderly predict greater long-term survivorship. J Orthop Sci. 2016;21:48–52.
Contreras A, Grandas F. Risk of Falls in Parkinson’s Disease: A Cross-Sectional Study of 160 Patients. Parkinsons Dis. 2012;2012.
Urbich M, Globe G, Pantiri K, Heisen M, Bennison C, Wirtz HS, et al. A Systematic Review of Medical Costs Associated with Heart Failure in the USA (2014–2020). Pharmacoeconomics. 2020;38:1219.
Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. The Medical Costs of Fatal Falls and Fall Injuries among Older Adults. J Am Geriatr Soc. 2018;66:693.
Jaeger SU, Wohlrab M, Schoene D, Tremmel R, Chambers M, Leocani L, et al. Mobility endpoints in marketing authorisation of drugs: What gets the European medicines agency moving? Age Ageing. 2022;51:1–10.
Gijbels D, Alders G, Van Hoof E, Charlier C, Roelants M, Broekmans T, et al. Predicting habitual walking performance in multiple sclerosis: Relevance of capacity and self-report measures. Mult Scler. 2010;16:618–26.
Kluge F, Del Din S, Cereatti A, Gaßner H, Hansen C, Helbostad JL, et al. Consensus based framework for digital mobility monitoring. PLoS ONE. 2021;16:e0256541.
Medicines Agency E. Committee for Medicinal Products for Human Use (CHMP) Qualification opinion on stride velocity 95th centile as a secondary endpoint in Duchenne Muscular Dystrophy measured by a valid and suitable wearable device*. 2019.
Rochester L, Mazzà C, Mueller A, Caulfield B, McCarthy M, Becker C, et al. A Roadmap to Inform Development, Validation and Approval of Digital Mobility Outcomes: The Mobilise-D Approach. Digit Biomarkers. 2020;4(Suppl 1):13–27.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372.
Westgate MJ. revtools: An R package to support article screening for evidence synthesis. Res Synth Methods. 2019;10:606–14.
Inflation Calculator | Federal Reserve Bank of Minneapolis. https://www.minneapolisfed.org/about-us/monetary-policy/inflation-calculator.
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) Statement. Value Heal. 2013;16:e1-5.
Rothfuss J, Mau W, Zeidler H, Brenner MH. Socioeconomic evaluation of rheumatoid arthritis and osteoarthritis: A literature review. Semin Arthritis Rheum. 1997;26:771–9.
Perkins A, Clark D. Assessing the association of walking with health services use and costs among socioeconomically disadvantaged older adults. Prev Med (Baltim). 2001;32:492–501.
Tsuji I, Takahashi K, Nishino Y, Ohkubo T, Kuriyama S, Watanabe Y, et al. Impact of walking upon medical care expenditure in Japan: the Ohsaki Cohort Study. Int J Epidemiol. 2003;32:809–14.
Purser JL, Weinberger M, Cohen HJ, Pieper CF, Morey MC, Li T, et al. Walking speed predicts health status and hospital costs for frail elderly male veterans. J Rehabil Res Dev. 2005;42:535.
Kato M, Goto A, Tanaka T, Sasaki S, Igata A, Noda M. Effects of walking on medical cost: A quantitative evaluation by simulation focusing on diabetes. J Diabetes Investig. 2013;4:667–72.
Turi B, Codogno J, Fernandes R, Monteiro H. Walking and health care expenditures among adult users of the Brazilian public healthcare system: retrospective cross-sectional study. Cien Saude Colet. 2015;20:3561–8.
Kabiri M, Brauer M, Shafrin J, Sullivan J, Gill TM, Goldman DP. The Long-Term Health and Economic Value of Improved Mobility Among Older Adults in the United States. Value Health. 2018;21:792.
Karl FM, Tremmel M, Luzak A, Schulz H, Peters A, Meisinger C, et al. Direct healthcare costs associated with device assessed and self-reported physical activity: results from a cross-sectional population-based study. BMC Public Heal. 2018;18:1–11.
Bonnini S, Mazzoni G, Borghesi M, Chiaranda G, Myers J, Mandini S, et al. Improving walking speed reduces hospitalization costs in outpatients with cardiovascular disease. An analysis based on a multistrata non-parametric test. BMC Health Serv Res. 2020;20(1):1048.
Okayama T, Naito T, Yonenaga Y, Ohashi T, Kitagawa M, Mitsuhashi N, et al. Clinical impact of walking capacity on the risk of disability and hospitalizations among elderly patients with advanced lung cancer. Support Care Cancer. 2021;29:3961–70.
Hirai H, Saito M, Kondo N, Kondo K. Ojima T. Physical activity and cumulative long-term care cost among older japanese adults: A prospective study in jages. Int J Environ Res Public Health; 2021. p. 18.
Saint-Maurice PF, Graubard BI, Troiano RP, Berrigan D, Galuska DA, Fulton JE, et al. Estimated Number of Deaths Prevented Through Increased Physical Activity Among US Adults. JAMA Intern Med. 2022. https://doi.org/10.1001/JAMAINTERNMED.2021.7755.
Montero-Odasso M, Schapira M, Soriano E, Varela M, Kaplan R, Camera L, et al. Gait velocity as a single predictor of adverse events in healthy seniors aged 75 years and older. J Gerontol A Biol Sci Med Sci. 2005;60:1304–9.
Macera CA. Commentary: Can walking lower medical care costs? Int J Epidemiol. 2003;32:814–5.
Mazzà C, Alcock L, Aminian K, Becker C, Bertuletti S, Bonci T, et al. Technical validation of real-world monitoring of gait: a multicentric observational study. BMJ Open. 2021;11:e050785.
Shiroiwa T, Sung YK, Fukuda T, Lang HC, Bae SC, Tsutani K. International survey on willingness-to-pay (WTP) for one additional QALY gained: what is the threshold of cost effectiveness? Health Econ. 2010;19:422–37.
Acknowledgements
Not applicable.
Funding
This work was supported by the Mobilise-D project, which has received funding from the Innovative Medicines Initiative 2 Joint Undertaking (JU) under grant agreement No. 820820. This JU receives support from the European Union's Horizon 2020 research and innovation program and the European Federation of Pharmaceutical Industries and Associations (EFPIA). The content of this study reflects the authors’ views. Neither IMI nor the European Union, EFPIA, nor any Associated Partners are responsible for any use that may be made of the information contained herein. ISGlobal acknowledges support from the Spanish Ministry of Science, Innovation, and Universities through the “Centro de Excelencia Severo Ochoa 2019–2023” Program (CEX2018- 000806-S), and support from the Generalitat de Catalunya through the CERCA Program. LR acknowledges support from the National Institute for Health Research (NIHR) Newcastle Biomedical Research Centre and the Clinical Ageing Research Unit based at Newcastle upon Tyne Hospitals NHS Foundation Trust.
Author information
Authors and Affiliations
Contributions
MW, SJ and CB conceived the paper. MW was responsible for data management and coordinated the review process. MW and SJ screen titles, abstracts and full texts. MW and SJ drafted the manuscript. JK contributed to development of search strategy and provided access to Embase. LD, JK, MZ, MS, MC, LR and CB critically revised the manuscript and all authors gave their final approval of the version to be published.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
MW reports grants from HORIZON 2020 IMI No. 820820, during the conduct of the study. SJ is partly supported by the Robert Bosch Stiftung Stuttgart. J.K. reports grants from HORIZON2020 IMI No.820820, during the conduct of the study. M.C. reports personal fees from Takeda Pharmaceuticals, during the conduct of the study; personal fees from Takeda Pharmaceuticals, outside the submitted work. MS is supported by the Robert Bosch Stiftung Stuttgart and reports grants from HORIZON 2020 IMI 2 Mobilise-D, during the conduct of the study, and grants and non-financial support from Green Cross WellBeing Co. Ltd., Gilead Sciences Inc., Robert Bosch GmbH, and CORAT Therapeutics GmbH, as well as other from Agena Bioscience GmbH, outside the submitted work. CB disclosed consultation fees from E. Lilly and speaker fees from Amgen, Nutricia and Pfizer, and reports grants from HORIZON 2020 IMI No. 820820, during the conduct of the study. LR reports grants from HORIZON2020 IMI 2 Mobilise-D and IDEA-FAST, National Institute for Health Research, Medical Research Council, Dunhill Medical Trust, Parkinson’s UK, and Cure Parkinson’s Trust.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wohlrab, M., Klenk, J., Delgado-Ortiz, L. et al. The value of walking: a systematic review on mobility and healthcare costs. Eur Rev Aging Phys Act 19, 31 (2022). https://doi.org/10.1186/s11556-022-00310-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s11556-022-00310-3