Abstract
Background
Atrial fibrillation negatively impacts physical fitness and health-related quality of life. We recently showed that 3 months of physiotherapist-led exercise-based cardiac rehabilitation improves physical fitness and muscle function in elderly patients with permanent atrial fibrillation and concomitant diseases. Little is, however, known about the consequences for physical fitness, physical activity level, and health-related quality of life after ending the rehabilitation period.
Methods
Prospective 3 months follow-up study of 38 patients out of 40 eligible (10 women) who, as part of a randomized controlled trial, had completed a 3 months physiotherapist-led cardiac rehabilitation resulting in improved physical fitness,. In the current study, the participants were instructed to refrain from exercise for 3 months after completion of the rehabilitation period. Primary outcome measure was physical fitness measured as highest achieved workload using an exercise tolerance test. Secondary outcome measures were muscle function (muscle endurance tests), physical activity level (questionnaire and accelerometer), and health-related quality of life, (Short Form-36), as in the preceding intervention study. We used the Wilcoxon Signed Rank test to analyse differences between the end of rehabilitation and at follow-up. The effect size was determined using Cohen’s d .
Results
Exercise capacity and exercise time significantly decresead between end of rehabilitation and at follow-up (p < .0001 for both). A significant reduction in shoulder flexion repetitions (p = .006) was observed as well as reduced health-related quality of life in the Short Form-36 dimensions Physical Function (p = .042), Mental Health (p = .030), and Mental Component Score (p = .035). There were, however, no changes regarding objective and subjective physical activity measurements.
Conclusion
In older patients with permanent atrial fibrillation, previously achieved improvements from physiotherapist-led exercise-based cardiac rehabilitation in physical fitness and muscle function were lost, and health-related quality of life was impaired after ending the rehabilitation period. A strategy for conserving improvements after a rehabilitation period is essential.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is the most common clinically significant arrythmia in adults. AF increases with age, is more common in men, and the prevalence is > 3% in the adult population and > 20% in ages above 80 years; both incidence and prevalence is expected to increase worldwide. The proportion of permanent AF is estimated to 30% [1,2,3]. In older adults, AF has clinically significant negative impact on physical fitness and health-related quality of life (HR-QoL) [4,5,6,7]. Two recent meta-analyses [8, 9] conclude that cardiac rehabilitation in patients with AF can increase physical fitness and improve some aspects of HR-QoL [8]. In line with that conclusion, we recently showed in a randomized controlled trial that 3 months of physiotherapist-led exercise-based cardiac rehabilitation (PT-X) improved physical fitness in older patients with permanent AF and several co-morbidities, while physical activity on prescription did not [10].
Although PT-X improves physical fitness and muscle function in elderly patients with permanent AF and concomitant disease with considerable pharmacotherapy, little is known about the consequences when the rehabilitation period ends. In the present study, our primary aim was therefore to explore the consequences in terms of physical fitness, physical activity level, and HR-QoL among patients with permanent AF after ending a period of PT-X [10].
Methods
We conducted a 3 months follow-up after the cessation of 3 months of PT-X in a randomized controlled study including central circulatory interval exercise and circuit training of muscle function at two 60-min hospital-based sessions, along with two home-based exercise sessions per week, as previously described in detail [10].
Patients
All 40 eligible patients (10 women), who had completed the PT-X part of the randomized controlled study [10], were invited to participate in a follow-up study investigating the effects of 3 months without training. The patients received both written and verbal information, and provided written informed consent to participate. The investigation conformed to the declaration of Helsinki, was approved by the Regional Ethics Committee of Gothenburg, and was retrospectively registred at ClinicalTrials.gov Identifier: NCT02493400. First posted 09/07/2015. Registred in FoUvgr project 124,611. First posted 28/04/2013.
Protocol
During the 3-month period following PT-X, the patients were asked to avoid participation in any organised exercise program that could improve physical fitness (aerobic capacity and muscular function). After this pause the patients were motivated and supported to regain their exercise habits through contact with local gym and patient associations.
Tests
The testing procedures followed the same protocol as previously described in detail [10]. The tests were performed by physiotherapists blinded to the prior randomisation to PT-X or physical exercise on prescription. The primary outcome measure was maximum exercise capacity, assessed using a symptom-limited ergometer cycle test (Monark ergometer 839e; Monark, Varberg, Sweden) [11]. The workload began at 25 W, and was increased by 25 W every 4.5 min until the patient’s rated perceived exertion was 17 (very heavy) on the Borg scale [12]. At each workload, the patient’s heart rate and blood pressure were measured.
The secondary outcome measures included muscular endurance, physical activity level, and HR-QoL.
The muscular endurance test involved unilateral isoinertial shoulder flexion in a sitting position with a dumbbell (2 kg for women, and 3 kg for men); bilateral isometric shoulder abduction in a sitting position with a dumbbell (1 kg for both women and men); and an unilateral isoinertial heel-lift with a straight knee, on a 10° tilted wedge, with shoes on [13].
Physical activity level was measured using an accelerometer (Actigraph® GT3x+; Actigraph, Pensacola, Florida, USA). Patients were instructed to wear the accelerometer throughout the whole day for 7 days, except when taking a shower or bath [14]. Accelerometer data were calculated using the algorithm validated by Choi et al. [15]. The accelerometer measured the patient’s MET-minutes per week (MET level × minutes of activity × events per week), and one metabolic equivalent of tasks (1 MET) was equal to an oxygen uptake (VO2) of 3.5 mL × kg− 1 × min− 1. Physical activity was also self-reported using the Swedish version of the Short Form International Physical Activity Questionnaire (IPAQ) [16]. IPAQ categories were low (1), medium (2), and high (3) physical activity levels. For self-reported physical activity level during detraining, we also used the Saltin-Grimby’s 6-grade physical activity level scale, which has been previously validated [17].
HR-QoL was measured using the Swedish version of the Short Form-36 Health Survey Questionnaire (SF-36) [18].
Statistics
Statistical analyses were performed using the Statistical Package for Social Science (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 28.0.; Armonk, NY, USA). Ratio and interval data are presented as mean (SD) and median (interquartile range), ordinal data as median (range), and nominal data as absolute and relative numbers. Data distribution was checked with Shapiro-Wilk’s test and normality was assumed if p > .05. Although some variables showed normal distribution, the Wilcoxon Signed Rank test was used to analyse within-group differences. The effect size was calculated using the z-value divided by the square root of N (N = total number of cases). A d value of ~ 0.2 indicated a small effect size, ~ 0.5 medium, and ~ 0.8 large [19, 20]. For changes in SF-36 dimensions, however, a 5-point difference is “clinically and socially relevant”, 10 points a “moderate”, and 20 points “a very large” one [21]. Differences were considered statistically significant when p was <.05.
Results
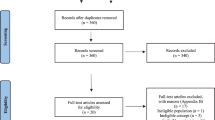
Of the 40 eligible patients 38 (95%) followed instructions and completed follow-up (10 women), while 2 patients withdrew participation due to medical causes or unwillingness. Their mean age (SD) was 75 [4] years.
Table 1 summarizes the patients’ demographic data and clinical characteristics, and Table 2 the patient’s pharmacological therapies. Around 90% received some form of stroke prophylaxis (mainly oral anticoagulation), > 80% required heart rate regulation (mainly beta-blockers), and the majority used renin-angiotensin-inhibiting therapy.
We compared data from the tests performed immediately after the PT-X intervention period with those obtained at the 3-months follow-up.
Primary outcome measure - physical fitness
At follow-up 3 months after the end of the PT-X period there was a significant decrease in physical fitness in terms of maximum workload (on average − 9 W) and exercise time (on average − 102 s); p < .0001 for both measures. The decrease in maximum workload and exercise time showed a moderate effect size (Table 3).
Secondary outcome measures
Muscle endurance in shoulder flexion in the left arm was also significantly reduced by on average − 4 reps; p = .006 (Table 3).
Neighter self reported physical activity with the IPAQ questionnaire, nor the objective measures with accelerometer were significantly changed (Table 3).
There was a significant reduction of HR-QoL when measured using the SF-36 dimensions Physical Function (PF), on average – 3 points; p = .042, Mental Health (ME), on average – 4 points; p = .030, and the Mental Component Score (MCS), on average - 3 points p = .035 (Table 4).
Discussion
The present study shows that improvements in physical fitness and muscle function gained by a 3-months PT-X period in elderly patients with permanent AF disappeared after a 3-months’ period without organised exercise. In addition, there was a reduction in HR-OoL. A strategy for conserving improvements after a rehabilitation period is thus essential.
Several studies among patients with cardiovascular diseases other than AF show that patients have difficulty continuing exercise and maintaining a sufficient physical activity level after finishing exercise-based cardiac rehabilitation [22,23,24]. The results of the present study both confirms the importance of developing a strategy for preserving achieved improvements and expands the knowledge of what happens when systematic circulatory training is not continued. Such information might strengthen the motivation for continued training both among patients and health care providers.
The physical fitness improvements following PT-X, 2 mL × kg− 1 × min− 1 measured as maximum work load, were comparable to those achieved in patients with chronic heart failure, in whom such improvements were associated with decreased mortality and hospital admissions during the follow-up period [25].
The period following the end of the PT-X period is compatible with the concept of detraining. Detraining is defined as the cessation or reduction of training, or a decrease in physical fitness caused by training cessation or reduction [26]. In the English literature, we have found no previous report addressing the impact of detraining in patients with permanent AF.
Previous investigations have shown that detraining causes central and peripheral alterations in athletes and recently trained healthy individuals [27,28,29]. These alterations are multifactorial, and include a reduced VO2max due to reduced blood volume and higher heart rate response, which reduce stroke volume and affect cardiac output [29]. The peripheral alterations include reduced muscular capillarisation and oxidative enzyme activities, and a decreased arterial-venous oxygen difference and reduced oxygen delivery to the cells, which affect mitochondrial ATP production [27]. We also observed significant loss of muscular endurance, in line with previously reported results of detraining in patients with and without cardiovascular disease [30,31,32]. Our results corroborates those of Volaklis et al. [31] and Ratel et al. [32], which showed that detraining led to reversal of improvements of VO2peak and muscular strength among patients with cardiovascular disease and in older adults [27, 28, 30,31,32]. Our study showed that detraining had similar effects in patients with permanent AF.
Furthermore, the period of detraining led to an impaired HR-QoL, with decreased scores on all SF-36 dimensions, and consequently a significant decrease both in physical function and mental health as well as in the mental component score. In some dimensions, the post-detraining scores were lower than the scores before PT-X. In three of these dimensions (Role Physical, Vitality, and Social Functioning), the SF-36 scores exhibited a reduction of at least 5 points, which is considered a clinically and socially relevant difference. Notably, the patients showed a 13-points deterioration in the Role Emotional dimension, which is considered a moderate change [21].
These findings indicate that both physical fitness and HR-QoL deteriorate if PT-X-induced improvements are not preserved.
Risom et al. [9] found no evidence that PT-X improved HR-QoL. This was also our finding in the first part of our study, in which the patients self-rated scores were similar to in the normative Swedish population of the same age range [10, 33]. Teixeira-Salmela et al. reported that HR-QoL increased with exercise training in the older population, and this increase persisted during detraining [30]. They proposed that patients felt better about their physical abilities and, therefore, adopted a more active lifestyle. That situation differs from the situation in our study, in which patients were asked to avoid organised exercise. Clearly, adherence to these instructions led to a reduction of HR-QoL. Our results are in line with the findings of an observational study, in which older individuals (> 65 years of age) participated in a detraining period after a period of organised exercise [34]. The participants received instructions similar to those given in the present study, and the results showed significant deterioration of all dimensions of the HR-QoL as measured by SF-36, as in our study [34]. These findings clearly confirm that after cessation of PT-X, it is crucial to support patients to maintain their physical fitness and HR-QoL.
Methodological aspects and limitations
In this study, we investigated the consequences of not pursuing training after a period of PT-X in patients with permanent AF. Due to the high evidence of benefit from improved physical fitness this may seem ethically questionable. It is, however, well known that it is difficult to maintain good exercise habits, and the need for support in lifestyle changes is an important issue. Such a strategy also requires resources and needs to be supported by scientific evidence, which was scarce when this study was initiated in 2013. The results of the present study corroborates the need to continue exercising after a period of successful PT-X, and can thus serve to motivate patients to pursue this goal and health care authorities to allocate suitable resources.
Conclusions
Although PT-X improves physical fitness also in older patients with AF and concomitant diseases, a subsequent period without systematic circulatory training has negative effects not only on physical fitness and muscle function but also on HR-QoL. A strategy for conserving improvements after a period of PT-X rehabilitation is essential.
Availability of data and materials
The dataset used and/or analysed for this current study may be available from the corresponding author upon resenable request. However, this is not applied for in the ethical application and must so be done before data sharing.
Abbreviations
- AF:
-
Atrial fibrillation
- HR-QoL:
-
Health-Related Quality of Life
- IPAQ:
-
Short Form International Physical Activity Questionnaire
- MET:
-
Metabolic equivalent of task
- PT-X:
-
Physiotherapist-led exercise-based cardiac rehabilitation
- PF:
-
The Short Form-36 physical function dimension
- RPE:
-
Rate of perceived exertion (Borg’s scale 6–20)
- SF-36:
-
The Short Form-36 Health Survey Questionnaire
- VO2peak :
-
Highest oxygen uptake achieved
References
Nieuwlaat R, Capucci A, Camm AJ, Olsson SB, Andresen D, Davies DW, et al. Atrial fibrillation management: a prospective survey in ESC member countries: the euro heart survey on atrial fibrillation. Eur Heart J. 2005;26(22):2422–34. https://doi.org/10.1093/eurheartj/ehi505.
Lippi G, Sanchis-Gomar F, Cervellin G. Global epidemiology of atrial fibrillation: an increasing epidemic and public health challenge. Int J Stroke. 2021;16(2):217–21. https://doi.org/10.1177/1747493019897870.
Bjorck S, Palaszewski B, Friberg L, Bergfeldt L. Atrial fibrillation, stroke risk, and warfarin therapy revisited: a population-based study. Stroke. 2013;44(11):3103–8. https://doi.org/10.1161/STROKEAHA.113.002329.
Zhang L, Gallagher R, Neubeck L. Health-related quality of life in atrial fibrillation patients over 65 years: a review. Eur J Prev Cardiol. 2015;22(8):987–1002. https://doi.org/10.1177/2047487314538855.
Ariansena I, Gjesdal K, Abdelnoorb M, Edvardsenc E, Engerd S, Tveitd A. Quality of life, exercise capacity and comorbidity in old patients with permanent atrial fibrillation. J Atr Fibrillation. 2008;1:136.
Stridsman M, Stromberg A, Hendriks J, Walfridsson U. Patients' experiences of living with atrial fibrillation: a mixed methods study. Cardiol Res Pract. 2019;2019:6590358–10. https://doi.org/10.1155/2019/6590358.
Singh SN, Tang XC, Singh BN, Dorian P, Reda DJ, Harris CL, et al. Quality of life and exercise performance in patients in sinus rhythm versus persistent atrial fibrillation: a veterans affairs cooperative studies program substudy. J Am Coll Cardiol. 2006;48(4):721–30. https://doi.org/10.1016/j.jacc.2006.03.051.
Kato M, Kubo A, Nihei F, Ogano M, Takagi H. Effects of exercise training on exercise capacity, cardiac function, BMI, and quality of life in patients with atrial fibrillation: a meta-analysis of randomized-controlled trials. Int J Rehabil Res. 2017;40(3):193–201. https://doi.org/10.1097/MRR.0000000000000232.
Risom SS, Zwisler AD, Johansen PP, Sibilitz KL, Lindschou J, Gluud C, et al. Exercise-based cardiac rehabilitation for adults with atrial fibrillation. Cochrane Database Syst Rev. 2017;2:Cd011197.
Borland M, Bergfeldt L, Nordeman L, Bollano E, Andersson L, Rosenkvist A, et al. Exercise-based cardiac rehabilitation improves physical fitness in patients with permanent atrial fibrillation – a randomized controlled study. Transl Sports Med. 2020;00:1–11.
World Health Organization. Exercise tests in relation to cardiovascular function. Report of a WHO meeting. World Health Organ Tech Rep Ser. 1968;388:1–30.
Borg G. Borg's perceived exertion and pain scales. Leeds: Human Kinetics; 1998.
Cider A, Carlsson S, Arvidsson C, Andersson B, Sunnerhagen KS. Reliability of clinical muscular endurance tests in patients with chronic heart failure. Eur J Cardiovasc Nurs. 2006;5(2):122–6. https://doi.org/10.1016/j.ejcnurse.2005.10.001.
Corder K, Brage S, Ekelund U. Accelerometers and pedometers: methodology and clinical application. Curr Opin Clin Nutr Metab Care. 2007;10(5):597–603. https://doi.org/10.1097/MCO.0b013e328285d883.
Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011;43(2):357–64. https://doi.org/10.1249/MSS.0b013e3181ed61a3.
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–95. https://doi.org/10.1249/01.MSS.0000078924.61453.FB.
Grimby G, Frandin K. On the use of a six-level scale for physical activity. Scand J Med Sci Sports. 2018;28:819–25.
Sullivan M, Karlsson J, Ware JJ. The Swedish SF-36 health survey--I. evaluation of data quality, scaling assumptions, reliability and construct validity across general populations in Sweden. Soc Sci Med. 1995;41(10):1349–58. https://doi.org/10.1016/0277-9536(95)00125-Q.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: L. Erlbaum Associates; 1988.
Pallant J. SPSS survival manual: a step by step guide to data analysis using IBM SPSS. 6th ed: Maidenhead: Open University Press: McGraw-Hill; 2016.
Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 health survey: manual and interpretation guide. Boston: Nimord Press; 1993.
Pinto BM, Goldstein MG, Papandonatos GD, Farrell N, Tilkemeier P, Marcus BH, et al. Maintenance of exercise after phase II cardiac rehabilitation: a randomized controlled trial. Am J Prev Med. 2011;41(3):274–83. https://doi.org/10.1016/j.amepre.2011.04.015.
Moore SM, Dolansky MA, Ruland CM, Pashkow FJ, Blackburn GG. Predictors of women's exercise maintenance after cardiac rehabilitation. J Cardpulm Rehabil. 2003;23(1):40–9. https://doi.org/10.1097/00008483-200301000-00008.
Reid RD, Wooding EA, Blanchard CM, Moghei M, Harris J, Proulx GA, et al. A randomized controlled trial of an exercise maintenance intervention in men and women after cardiac rehabilitation (ECO-PCR trial). Can J Cardiol. 2021;37(5):794–802. https://doi.org/10.1016/j.cjca.2020.10.015.
Gielen S, Laughlin MH, O'Conner C, Duncker DJ. Exercise training in patients with heart disease: review of beneficial effects and clinical recommendations. Prog Cardiovasc Dis. 2015;57(4):347–55. https://doi.org/10.1016/j.pcad.2014.10.001.
Kraemer WJ, Fleck SJ. Optimizing strength training: designing nonlinear periodization workouts: human kinetics; 2007.
Mujika I, Padilla S. Detraining: loss of training-induced physiological and performance adaptations. Part II: long term insufficient training stimulus. Sports Med. 2000;30(3):145–54. https://doi.org/10.2165/00007256-200030030-00001.
Mujika I, Padilla S. Detraining: loss of training-induced physiological and performance adaptations. Part I: short term insufficient training stimulus. Sports Med. 2000;30(2):79–87. https://doi.org/10.2165/00007256-200030020-00002.
Mujika I, Padilla S. Cardiorespiratory and metabolic characteristics of detraining in humans. Med Sci Sports Exerc. 2001;33(3):413–21. https://doi.org/10.1097/00005768-200103000-00013.
Teixeira-Salmela LF, Santiago L, Lima RC, Lana DM, Camargos FF, Cassiano JG. Functional performance and quality of life related to training and detraining of community-dwelling elderly. Disabil Rehabil. 2005;27(17):1007–12. https://doi.org/10.1080/09638280500030688.
Volaklis KA, Douda HT, Kokkinos PF, Tokmakidis SP. Physiological alterations to detraining following prolonged combined strength and aerobic training in cardiac patients. Eur J Cardiovasc Prev Rehabil. 2006;13(3):375–80. https://doi.org/10.1097/01.hjr.0000198922.42437.39.
Ratel S, Gryson C, Rance M, Penando S, Bonhomme C, Le Ruyet P, et al. Detraining-induced alterations in metabolic and fitness markers after a multicomponent exercise-training program in older men. Appl Physiol Nutr Metab. 2012;37(1):72–9. https://doi.org/10.1139/h11-130.
Sullivan M, Karlsson J, Taft C. SF-36 Hälsoenkät: Swedish manual och Tolkningsguide, 2 upplagan (Swedish manual and interpretation guide 2nd edition ). Gothenburg: Sahlgrenska University Hospital; 2002.
Esain I, Rodriguez-Larrad A, Bidaurrazaga-Letona I, Gil SM. Health-related quality of life, handgrip strength and falls during detraining in elderly habitual exercisers. Health Qual Life Outcomes. 2017;15(1):226. https://doi.org/10.1186/s12955-017-0800-z.
Acknowledgements
The authors would like to thank their colleagues at Alingsås Hospital, Närhälsan Sörhaga rehabilitation center, and Sahlgrenska University Hospital for their support.
Funding
Open access funding provided by University of Gothenburg. This work was supported by the HealthCare Board, Region Västra Götaland (VGFOUREG-383951 and VGFOUREG-551731), and by the Local Research and Development Council Södra Älvsborg (VGFOUSA-601851 and VGFOUSA-344441).
Author information
Authors and Affiliations
Contributions
Maria Borland, Lennart Bergfeldt, Åsa Cider, Lars Andersson and Lena Nordeman, contributed to the conception and design of the work. Maria Borland, Agneta Rosenkvist, Marika Jakobsson, Kristin Olsson, Adam Lundwall contributed to the acquisition of the work, Maria Borland, Lennart Bergfeldt, Åsa Cider and Lena Nordeman, made the analysis and interpretation of the data. Maria Borland, Lennart Bergfeldt, Åsa Cider and Lena Nordeman drafted the manuscript, Maria Borland, Lennart Bergfeldt, Åsa Cider Agneta Rosenkvist, Marika Jakobsson, Kristin Olsson, Adam Lundwall, Lars Andersson and Lena Nordeman, critically revised the manuscript. All gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
In compliance with the Declaration of Helsinki, the protocol was approved by the Regional Ethics Committee of Gothenburg with registration number DNR 074–13. ClinicalTrials.gov Identifier: NCT02493400. All participants signed informed consent.
Registered in researchweb, FoUvgr project 124611. First posted 28/04/2013.
Retrospectively registered in ClinicalTrials.gov Identifier: NCT02493400. First posted 09/07/2015.
Consent for publication
Not applicable.
Competing interests
The authors declare that there is no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Borland, M., Bergfeldt, L., Cider, Å. et al. Effects of 3 months of detraining following cardiac rehabilitation in patients with atrial fibrillation. Eur Rev Aging Phys Act 19, 14 (2022). https://doi.org/10.1186/s11556-022-00293-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s11556-022-00293-1