Abstract
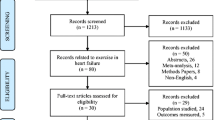
Exercise performance is an essential tool for managing heart failure. Although the benefits of exercise are well documented for people with chronic and stable heart failure, there is still no consensus on their prescription in patients hospitalized with acute heart failure undergoing clinical stabilization. The aim of this study is to identify the literature on exercise programs encompassing the components of aerobic and resistance training for hospitalized patients admitted for acute heart failure. A scoping review was conducted according to the proposed methodology of the Joanna Briggs Institute. Studies with adults over 18 years old, hospitalized, and diagnosed with acute heart failure who participated in aerobic and resistance exercise training programs during their hospital stay were included. Three studies met the inclusion criteria. One was a retrospective, observational analytical cohort study, in which the main outcome of the exercise program was improvement in the previous disabilities of the participants. The other two were multicenter randomized controlled studies that showed greater improvement in physical function, functional capacity, depression, quality of life, and frailty status in the intervention groups. The exercise prescriptions differed according to the principles of the exercise prescription—frequency of exercise, intensity of exercise, exercise time (duration), type (mode), exercise volume, and progression. It is too early to make recommendations based on evidence of the type structure of an exercise program with aerobic and strength-training components in this population. However, in the exercise programs of the reviewed studies, the predominance of light to moderate intensity and the importance of progressively increase the frequency and duration of the training sessions were demonstrated, with bicycle ergometers and walking being the most common types of aerobic exercises. It is recommended that investment and research in this area should continue with more methodologically robust studies.

Similar content being viewed by others
Availability of data and materials
This declaration is not applicable.
References
Long L, Ir M, Bridges C, Va S, Ej D, Ajs C et al (2019) Exercise-based cardiac rehabilitation for adults with heart failure (Review)
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M et al (2021) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 1–128. Available from: https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehab368/6358045
Palmer K, Bowles KA, Paton M, Jepson M, Lane R (2018) Chronic heart failure and exercise rehabilitation: a systematic review and meta-analysis. Arch Phys Med Rehabil 99(12):2570–82. Available from: https://doi.org/10.1016/j.apmr.2018.03.015
Tucker WJ, Beaudry RI, Liang Y, Clark AM, Tomczak CR, Nelson MD et al (2019) Meta-analysis of exercise training on left ventricular ejection fraction in heart failure with reduced ejection fraction: a 10-year update. Prog Cardiovasc Dis 62(2):163–71. Available from: https://doi.org/10.1016/j.pcad.2018.08.006
Fonseca C, Brito D, Cernadas R, Ferreira J, Franco F, Rodrigues T et al (2017) Pela melhoria do tratamento da insuficiência cardíaca em Portugal – documento de consenso. Rev Port Cardiol 36(1):1–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0870255116302979
ACSM (2018) ACSM’s guideline for exercise testing and prescription. Tenth. American College of Sports Medicine; 501 p
Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M et al (2021) ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 42(34):3227–337. Available from: https://academic.oup.com/eurheartj/article/42/34/3227/6358713
Lee CT, Chen LW, Chien MY (2017) Effects of exercise training on anabolic and catabolic markers in patients with chronic heart failure: a systematic review. Heart Fail Rev 22(6):723–730
Munch GW, Rosenmeier JB, Petersen M, Rinnov AR, Iepsen UW, Pedersen BK et al (2018) Comparative effectiveness of low-volume time-efficient resistance training versus endurance training in patients with heart failure. J Cardiopulm Rehabil Prev 38(3):175–81. Available from: http://journals.lww.com/01273116-201805000-00006
Wang ZQ, Peng X, Li K, Wu CJJ (2019) Effects of combined aerobic and resistance training in patients with heart failure: a meta-analysis of randomized, controlled trials. Nurs Heal Sci 21(2):148–156
Jesus IC De, Menezes Junior FJ de, Bento PCB, Wiens A, Mota J, Leite N (2020) Effect of combined interval training on the cardiorespiratory fitness in heart failure patients: a systematic review and meta-analysis. Brazilian J Phys Ther 24(1):8–19. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1413355518304593
Laoutaris ID (2018) The aerobic / resistance / inspiratory muscle training hypothesis in heart failure
Takada S, Kondo T, Yasunaga M, Watanabe S, Kinoshita H, Fukuhara S et al (2020) Early rehabilitation in older patients hospitalized with acute decompensated heart failure: a retrospective cohort study: early rehabilitation and acute heart failure. Am Heart J 230:44–53. Available from: https://doi.org/10.1016/j.ahj.2020.09.009
Fukuta H, Goto T, Wakami K, Kamiya T, Ohte N (2019) Effects of exercise training on cardiac function, exercise capacity, and quality of life in heart failure with preserved ejection fraction: a meta-analysis of randomized controlled trials. Heart Fail Rev 24(4):535–547
Morris JH, Chen L (2019) Exercise training and heart failure: a review of the literature. Card Fail Rev 5(1):57–61. Available from: https://www.cfrjournal.com/articles/exercise-training-heart-failure
Peters M, Godfrey C, McInerney P, Munn Z, Trico A, Khalil H (2020) Chapter 11: Scoping reviews. In: JBI manual for evidence synthesis. JBI. Available from: https://wiki.jbi.global/display/MANUAL/Chapter+11%3A+Scoping+reviews
Aromataris E, Munn Z, editors (2020) JBI manual for evidence synthesis. JBI. Available from: https://wiki.jbi.global/display/MANUAL
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D et al (2018) PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169(7):467–73. Available from: https://www.acpjournals.org/doi/10.7326/M18-0850
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–9, W64. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19622511
Motoki H, Nishimura M, Kanai M, Kimura K, Minamisawa M, Yamamoto S et al (2019) Impact of inpatient cardiac rehabilitation on Barthel Index score and prognosis in patients with acute decompensated heart failure. Int J Cardiol 293:125–30. Available from: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,shib&db=cmedm&AN=31279661&lang=pt-pt&site=eds-live&scope=site
Kitzman DW, Whellan DJ, Duncan P, Pastva AM, Mentz RJ, Reeves GR et al (2021) Physical rehabilitation for older patients hospitalized for heart failure. N Engl J Med 385(3):203–16. Available from: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,shib&db=cmedm&AN=33999544&lang=pt-pt&site=eds-live&scope=site
Reeves GR, Whellan DJ, O’Connor CM, Duncan P, Eggebeen JD, Morgan TM et al (2017) A novel rehabilitation intervention for older patients with acute decompensated heart failure: the REHAB-HF pilot study. JACC Hear Fail 5(5):359–366
Powell R, McGregor G, Ennis S, Kimani PK, Underwood M (2018) Is exercise-based cardiac rehabilitation effective? A systematic review and meta-analysis to re-examine the evidence. BMJ Open 8
Pelliccia A, Sharma S, Gati S, Bäck M, Börjesson M, Caselli S et al (2020) ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J 42(1):17–96. Available from: https://academic.oup.com/eurheartj/article/42/1/17/5898937
Anderson L, Sharp GA, Norton RJ, Dalal H, Dean SG, Jolly K et al (2017) Home-based versus centre-based cardiac rehabilitation. Cochrane Database of Sys Rev 2017
Davies EJ, Moxham T, Rees K, Singh S, Coats AJS, Ebrahim S et al (2010) Exercise training for systolic heart failure: Cochrane systematic review and meta-analysis. Eur J Heart Fail 12(7):706–15. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-77954936825&doi=10.1093%2Feurjhf%2Fhfq056&partnerID=40&md5=226a35c1d4435c54caca61b7a431b04d
Murad K, Kitzman DW (2012) Frailty and multiple comorbidities in the elderly patient with heart failure: implications for management. Heart Fail Rev 17(4–5):581–8. Available from: http://link.springer.com/10.1007/s10741-011-9258-y
Valenzuela PL, Morales JS, Castillo-García A, Mayordomo-Cava J, García-Hermoso A, Izquierdo M et al (2020) Effects of exercise interventions on the functional status of acutely hospitalised older adults: a systematic review and meta-analysis. Ageing Res Rev 61:101076. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1568163720301288
Loyd C, Markland AD, Zhang Y, Fowler M, Harper S, Wright NC et al (2020) Prevalence of hospital-associated disability in older adults: a meta-analysis. J Am Med Dir Assoc 21(4):455–461.e5. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1525861019306966
Delgado BM, Lopes I, Gomes B, Novo A (2020) Early rehabilitation in cardiology – heart failure: the ERIC-HF protocol, a novel intervention to decompensated heart failure patients rehabilitation. Eur J Cardiovasc Nurs 147451512091380. Available from: http://journals.sagepub.com/doi/10.1177/1474515120913806
Delgado B, Novo A, Lopes I, Rebelo C, Almeida C, Pestana S et al (2022) The effects of early rehabilitation on functional exercise tolerance in decompensated heart failure patients : results of a multicenter randomized controlled trial ( ERIC-HF study ). Clin Rehabil 1–9
Gómez-Cuba M, Perreau de Pinninck-Gaynés A, Planas-Balagué R, Manito N, González-Costello J (2016) Rehabilitation in heart failure: update and new horizons. Curr Phys Med Rehabil Rep 4(3):208–15
Mytinger M, Nelson RK, Zuhl M (2020) Exercise prescription guidelines for cardiovascular disease patients in the absence of a baseline stress test. J Cardiovasc Dev Dis 7(2):15. Available from: https://www.mdpi.com/2308-3425/7/2/15
Haykowsky MJ, Daniel KM, Bhella PS, Sarma S, Kitzman DW (2016) Heart failure: exercise-based cardiac rehabilitation: who, when, and how intense? Can J Cardiol 32(10, Number 10 Supplement 2):S382–7. Available from: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,shib&db=edo&AN=ejs39320249&lang=pt-pt&site=eds-live&scope=site
Author information
Authors and Affiliations
Contributions
Ivo Lopes: conception of the study, study selection and data extraction review, data analysis and interpretation, drafting the article, and critical revision of the article. Bruno Delgado: conception of the study, study selection and data extraction review, and critical revision of the article. Patrício Costa: conception of the study and critical revision of the article. Miguel Padilha: conception of the study and critical revision of the article.
Corresponding author
Ethics declarations
Ethical approval
This declaration is not applicable.
Competing interests
The authors declare no competing interests.
Conflicts of interest
The authors declare that there are no conflicts of interest in this project.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A. Search strategy
Data search: 2022/01/12
Scopus
Search | Query (“Title – Abstract AND Keyword”) | Results |
|---|---|---|
1 | TITLE-ABS-KEY (((“Heart failure” OR “Cardiac Failure” OR “Myocardial Failure” OR “Heart Decompensation”) AND (aerobic OR endurance) AND (resistance OR strength) AND (inpatient OR hospital*))) | 178 |
Web of Science citation database
Search all databases | Query (“Topic”) | Results |
|---|---|---|
1 | TS = (((“Heart failure” OR “Cardiac Failure” OR “Myocardial Failure” OR “Heart Decompensation”) AND (aerobic OR endurance) AND (Resistance OR Strength) AND (Inpatient OR hospital*))) | 129 |
Query (“Title” OR “Subject Terms” OR “Abstract”) | Databases | Results |
|---|---|---|
TI (((“Heart failure” OR “Cardiac Failure” OR “Myocardial Failure” OR “Heart Decompensation”) AND (aerobic OR endurance) AND (Resistance OR Strength) AND (Inpatient OR hospital*))) OR SU (((“Heart failure” OR “Cardiac Failure” OR “Myocardial Failure” OR “Heart Decompensation”) AND (aerobic OR endurance) AND (Resistance OR Strength) AND (Inpatient OR hospital*))) OR AB (((“Heart failure” OR “Cardiac Failure” OR “Myocardial Failure” OR “Heart Decompensation”) AND (aerobic OR endurance) AND (Resistance OR Strength) AND (Inpatient OR hospital*))) | 66 | |
MEDLINE | 64 | |
MEDLINE with Full Text | 64 | |
OpenAIRE | 57 | |
Complementary Index | 29 | |
CINAHL Complete | 25 | |
Academic Search Complete | 24 | |
Supplemental Index | 18 | |
ScienceDirect | 17 | |
OAIster | 16 | |
Gale Health and Wellness | 15 | |
SPORTDiscus with Full Text | 13 | |
Directory of Open Access Journals | 12 | |
SwePub | 3 | |
Psychology and Behavioral Sciences Collection | 2 | |
Digital Access to Scholarship at Harvard (DASH) | 1 | |
SciELO | 1 | |
Regional Business News | 1 | |
MedicLatina | 1 | |
OpenDissertations | 1 | |
NARCIS | 1 | |
SveMed + | 1 | |
RCAAP | 1 |
OpenGrey
Search | Results | |
|---|---|---|
1 | ((“Heart failure” OR “Cardiac Failure” OR “Myocardial Failure” OR “Heart Decompensation”) AND (aerobic OR endurance) AND (Resistance OR Strength) AND (Inpatient OR hospital*)) | 0 |
Google Scholar
Search | Results | |
|---|---|---|
1 | ((“Heart failure” OR “Cardiac Failure” OR “Myocardial Failure” OR “Heart Decompensation”) AND (aerobic OR endurance) AND (Resistance OR Strength) AND (Inpatient OR hospital*)) | 0 |
Appendix B. Studies ineligible following full-text review
-
1.
Abolahrari-Shirazi, S., Kojuri, J., Bagheri, Z., & Rojhani-Shirazi, Z. (2018). Efficacy of combined endurance-resistance training versus endurance training in patients with heart failure after percutaneous coronary intervention: a randomized controlled trial. Journal of Research in Medical Sciences: The Official Journal of Isfahan University of Medical Sciences, 23, 12. https://doi.org/10.4103/jrms.JRMS_743_17
Reason for exclusion: Ineligible context
-
2.
Ambrosetti, M., Doherty, P., Faggiano, P., Corrà, U., Vigorito, C., Hansen, D., … Pedretti, R. F. E. (2017). Characteristics of structured physical training currently provided in cardiac patients: insights from the Exercise Training in Cardiac Rehabilitation (ETCR) Italian survey. Monaldi Archives for Chest Disease, 87(1). https://doi.org/10.4081/monaldi.2017.778
Reason for exclusion: Ineligible concept
-
3.
Braith, R. W., & Edwards, D. G. (2000). Exercise following heart transplantation. Sports Medicine (Auckland, N.Z.), 30(3), 171–192. https://doi.org/10.2165/00007256-200030030-00003
Reason for exclusion: Ineligible context
-
4.
Carvalho, T. de, Milani, M., Ferraz, A. S., Silveira, A. D. da, Herdy, A. H., Hossri, C. A. C., … Serra, S. M. (2020). Brazilian cardiovascular rehabilitation guideline—2020. Arquivos Brasileiros de Cardiologia, 114(5), 943–987. https://doi.org/10.36660/abc.20200407
Reason for exclusion: Ineligible context
-
5.
Coats, A. J. S. (2011). Clinical utility of exercise training in chronic systolic heart failure. Nature Reviews. Cardiology, 8(7), 380–392. https://doi.org/10.1038/nrcardio.2011.
Reason for exclusion: Ineligible context
-
6.
de Gregorio, C. (2018). Physical training and cardiac rehabilitation in heart failure patientS. Advances in Experimental Medicine and Biology, 1067, 161–181. https://doi.org/10.1007/5584_2018_144
Reason for exclusion: Ineligible context
-
7.
Fernandes, S. L., Carvalho, R. R., Santos, L. G., Sá, F. M., Ruivo, C., Mendes, S. L., … Morais, J. A. (2020). Pathophysiology and treatment of heart failure with preserved ejection fraction: state of the art and prospects for the future. Arquivos Brasileiros de Cardiologia, 114(1), 120–129. https://doi.org/10.36660/abc.20190111
Reason for exclusion: Ineligible context
-
8.
Gunn, E., Smith, K. M., McKelvie, R. S., & Arthur, H. M. (2006). Exercise and the heart failure patient: aerobic vs strength training–is there a need for both? Progress in Cardiovascular Nursing, 21(3), 146–150. https://doi.org/10.1111/j.0889-7204.2006.04678.x
Reason for exclusion: Ineligible context
-
9.
Jewiss, D., Ostman, C., & Smart, N. A. (2016). The effect of resistance training on clinical outcomes in heart failure: a systematic review and meta-analysis. International Journal of Cardiology, 221, 674–681. https://doi.org/10.1016/j.ijcard.2016.07.046
Reason for exclusion: Ineligible context
-
10.
Knocke, A. (2012). Program description: physical therapy in a heart failure clinic. Cardiopulmonary Physical Therapy Journal, 23(3), 46–48. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22993502
Reason for exclusion: Ineligible context
-
11.
Larsen, A. I. (2018). The muscle hypothesis in heart failure revised: “the multisite training approach”. European Journal of Preventive Cardiology, 25(12), 1252–1256. https://doi.org/10.1177/2047487318789225
Reason for exclusion: Ineligible context
-
12.
Lindgren, M., & Börjesson, M. (2021). The importance of physical activity and cardiorespiratory fitness for patients with heart failure. Diabetes Research and Clinical Practice, 176, 108,833. https://doi.org/10.1016/j.diabres.2021.108833
Reason for exclusion: Ineligible context
-
13.
Miche, E., Roelleke, E., Wirtz, U., Zoller, B., Tietz, M., Huerst, M., & Radzewitz, A. (2008). Combined endurance and muscle strength training in female and male patients with chronic heart failure. Clinical Research in Cardiology: Official Journal of the German Cardiac Society, 97(9), 615–622. https://doi.org/10.1007/s00392-008-0660-y
Reason for exclusion: Ineligible context
-
14.
Schindler, M. J., Adams, V., & Halle, M. (2019). Exercise in heart failure-what is the optimal dose to improve pathophysiology and exercise capacity? Current Heart Failure Reports, 16(4), 98–107. https://doi.org/10.1007/s11897-019-00428-z
Reason for exclusion: Ineligible context
-
15.
Takada, S., Kondo, T., Yasunaga, M., Watanabe, S., Kinoshita, H., Fukuhara, S., & Yamamoto, Y. (2020). Early rehabilitation in older patients hospitalized with acute decompensated heart failure: a retrospective cohort study: early rehabilitation and acute heart failure. American Heart Journal, 230, 44–53. https://doi.org/10.1016/j.ahj.2020.09.009
Reason for exclusion: Ineligible context
-
16.
Van Iterson, E. H., & Olson, T. P. (2017). Therapeutic targets for the multi-system pathophysiology of heart failure: exercise training. Current Treatment Options in Cardiovascular Medicine, 19(11), 87. https://doi.org/10.1007/s11936-017-0585-8
Reason for exclusion: Ineligible context
-
17.
Vuckovic, K. M., Piano, M. R., & Phillips, S. A. (2013). Effects of exercise interventions on peripheral vascular endothelial vasoreactivity in patients with heart failure with reduced ejection fraction. Heart, Lung and Circulation, 22(5), 328–340. https://doi.org/10.1016/j.hlc.2012.12.006
Reason for exclusion: Ineligible context
Appendix C. Characteristics of included studies
Author(s), year of publication, country | Study objective(s) | Population and sample size | Frequency of the implemented exercise training program | Intensity of the implemented exercise training program | Time (duration) of the implemented exercise training program | Type of the implemented exercise training program | Volume of the implemented exercise training program | Rate of progression of the implemented exercise training program |
|---|---|---|---|---|---|---|---|---|
Kitzman et al. (2021), USA [21] | To evaluate the effect of a multi-domain structured physical rehabilitation intervention the on the physical function and on the 6-month rate of rehospitalization for any cause | Patients ≥ 60 years hospitalized with acute decompensated heart failure N = 349 (experimental group: 175; control group: 174) | One session of exercise per day | Borg RPE scale (6 to 20), ≤ 12 | Up to 45 min | Aerobic component: walking and bicycle ergometer; Resistance component: sit to stand, step-up and side step-up, calf raise, stand to squat, proprioceptive neuromuscular facilitation patterns, open chain standing upper and lower extremities exercises using theraband (hip abductors, hip flexors, hip extensors, knee flexors, knee extensors, shoulder press, shoulder abductors, elbow flexors, elbow extensors | Not described; Average number of sessions per participant of 1.8 sessions | Assessment of the participants’ functional performance level (levels 1 to 4, from lowest to highest)—In the aerobic component, the time at which each participant could walk continuously without stopping was counted, with level 1 corresponding to the ability to walk at the usual pace for less than 2 min, level 2 corresponding to the ability to walk at the usual pace for 2 or more min but less than 10 min, level 3 corresponding to the ability to walk at the usual pace for 10 min or more but less than 20 min, and level 4 corresponding to the ability to walk at the usual pace for 20 min or more. Regarding the resistance component, the participant’s ability to get up from a chair without hand support was evaluated, with level 1 corresponding to the inability of this action, level 2 corresponding to the ability to rise from a chair at least once, level 3 corresponding to the ability to rise from a chair five times between 15 and 60 s, and level 4 corresponding to the ability to rise from a chair five times in less than 15 s Aerobic component: level 1: 5–9 min, level 2: 10–19 min, level 3: 20–29 min, level 4: 30–35 min (the participant should be encouraged to exceed the goal duration if able and then progressed to the next level at the subsequent session); Resistance component: once the participant can perform 1 set of 10 repetitions for each exercise without exceeding the target RPE in 2 consecutive sessions, the resistance is to be increased; proprioceptive neuromuscular facilitation patterns will be assisted or resisted by the study therapist to match the participant’s ability (1 set of 10 reps.); therabands with increasing resistance |
Reeves et al. (2017), USA [22] | To determine the feasibility, reasonableness, adherence and potential for efficacy of an intervention, as well as the potential safety, and to estimate the intervention effect size | Patients ≥ 60 years hospitalized with acute decompensated heart failure N = 27 (experimental group: 15; control group: 12) | The same data as in the study by Kitzman et al. (21) | The same data as in the study by Kitzman et al. (21) | The same data as in the study by Kitzman et al. (21) | The same data as in the study by Kitzman et al. (21) | Not described | The same data as in the study by Kitzman et al. (21) |
Motoki et al. (2019), Japan [20] | To evaluate the impact of a cardiac rehabilitation intervention on disability and prognosis | Patients hospitalized with acute decompensated heart failure N = 171 | Five sessions of exercise per week carried out during 2 weeks | Borg RPE scale (6 to 20 between the values 11 to 13 or target heart rate training zone between 30 and 50% | 30 min | Aerobic component: walking and bicycle ergometer; Resistance component: squats, calf raises, and weight training | Not described | Progression from the first stage (“sitting up in bed, sit-to-stand motions, self-care, and walking within the ward) to the second stage (exercise with the aerobic and resistance components) |
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lopes, I., Delgado, B., Costa, P. et al. Aerobic and resistance exercise in heart failure inpatients: a scoping review. Heart Fail Rev 28, 1077–1089 (2023). https://doi.org/10.1007/s10741-023-10311-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-023-10311-8