Abstract
Purpose
To compare the clinical results of anterior cruciate ligament (ACL) reconstruction using the single-tunnel single-bundle (STSB) technique versus the single-tunnel double-bundle (STDB) technique.
Methods
This was a retrospective, single-center, single-surgeon study based on data collected from March 2012 to June 2013. According to our inclusion/exclusion criteria, a total of 78 patients (64 males, 14 females; mean age, 25.1 years) who underwent arthroscopic ACL reconstruction with anterior tibialis tendon allografts through either the STSB technique (36 cases) or the STDB technique (42 cases) in our department were recruited. The International Knee Documentation Committee (IKDC), Lysholm, and Tegner scores were used to evaluate the subjective function of the knee joint during the postoperative follow-up. The Lachman test and pivot shift test were used to objectively assess the stability of the knee.
Results
The average follow-up duration was 24.9 ± 1.8 months in the STSB group and 24.6 ± 1.7 months in the STDB group (P > 0.05). Patients in both groups recovered to the preoperative sports level with few complications. The postoperative Lysholm score (86.1 ± 7.5 vs. 47.7 ± 9.0 in the STSB group; 87.0 ± 7.1 vs. 48.2 ± 8.3 in the STDB group), IKDC score (87.8 ± 7.2 vs. 49.3 ± 6.1 in the STSB group; 88.7 ± 6.6 vs. 49.8 ± 6.3 in the STDB group), Tegner score (6.5 ± 1.3 vs. 2.5 ± 1.3 in the STSB group; 6.6 ± 1.2 vs. 2.6 ± 1.2 in the STDB group), Lachman test positive rate (8.3% vs. 89.9% in the STSB group; 7.1% vs. 85.7% in the STDB group), and pivot shift test positive rate (27.8% vs. 63.9% in the STSB group; 7.1% vs. 69.0% in the STDB group) were significantly improved compared to the preoperative status in both groups (P < 0.05). However, no statistically significant difference was observed between the two groups at the final follow-up (P > 0.05), except for the pivot shift test positive rate in the STDB group versus the STSB group (7.1% vs. 27.8%, P < 0.05).
Conclusions
The STDB technique achieved a satisfactory clinical outcome with better rotational stability compared to the traditional STSB technique and therefore provided an effective option for ACL reconstruction.
Level of evidence
Case series, Level IV.
Similar content being viewed by others
Introduction
The anterior cruciate ligament (ACL) is the main stabilizing structure of the knee; it resists anterior translation and maintains forward and rotational stability [1]. The ACL is generally considered to include two functional bundles, i.e., the anteromedial (AM) and posterolateral (PL) bundles, each having a unique function [2, 3]. The AM bundle and PL bundle provide anteroposterior and rotational stability to the knee joint [4]. At present, single-tunnel single-bundle (STSB) and double-tunnel double-bundle (DTDB) reconstructions are two of the main ACL surgical procedures available in clinical practice [5, 6]. However, DTDB is technically difficult to perform for surgeons and more traumatic for patients compared to STSB. It requires a longer operative time, involves an increased risk of graft impingement and lateral femoral condyle and bone bridge fractures, and is challenging in revision surgery [7].
Taking these factors into account, some surgeons have explored single-tunnel double-bundle (STDB) reconstruction with the goal of restoring the anatomical double-bundle (DB) structure of the ACL within a single tunnel [8,9,10,11]. This technique overcomes the shortcomings of both DTDB and STSB reconstruction (i.e., restoring the anteroposterior and rotational stability while avoiding the drawbacks of DTDB reconstruction). Previous publications also reported a DB ACL reconstruction technique with one femoral and two tibial tunnels, which achieved good rotational stability in cadaveric knees [12, 13]. Duncan et al.’s study of fresh-frozen porcine knees with 40 samples concluded that fixation of the ACL with a double-tunnel technique on the tibial side had a biomechanical advantage with no potential deleterious side effects [14]. Another study found that the three-tunnel DB (with two femoral tunnels and a single tibial tunnel or with a single femoral tunnel and two tibial tunnels) could better restore intact knee biomechanics than single-bundle ACL reconstruction in a porcine model [15].
However, no patient outcome data have been reported yet. Whether the STDB ACL technique is able to restore knee joint stability and whether the patients can return to sports remain unknown. Therefore, clinical data for patients with an ACL rupture undergoing arthroscopic STSB (one femoral and tibial tunnel with one bundle) or STDB (one femoral and tibial tunnel with two bundles) reconstruction in our department were reviewed to compare the two surgical procedures in terms of the functional outcome, joint stability, complications, and side effects. The hypothesis of this study is that the STDB technique is an effective procedure to restore the knee stability of ACL injury patients and is able to achieve a better clinical outcome without introducing more complications than the traditional STSB technique.
Methods
Inclusion and exclusion criteria
The inclusion criteria were: (1) patients had subjective instability, and abnormal knee laxities were confirmed by the Lachman test and pivot shift test; (2) ACL rupture was confirmed by magnetic resonance imaging (MRI); (3) 18 years of age or over; (4) unilateral primary ACL injury; (5) patients had no or minimal osteochondral degeneration on radiographic examination; (6) patients underwent arthroscopic STDB or STSB ACL reconstruction with anterior tibialis tendon allografts.
The exclusion criteria were: (1) damage to multiple ligaments or injury of the articular cartilage; (2) radiographic evidence of Kellgren–Lawrence grade 3 or 4 osteoarthritis (OA) and/or severe osteoporosis; (3) bilateral ACL injuries; (4) partial ACL rupture; (5) concomitant total or subtotal meniscectomy; (6) young patients with unclosed growth plates.
Patient information
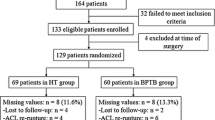
This retrospective study was carried out upon receiving approval from our institution’s ethical review board. Overall, 78 patients who visited our department from March 2012 to June 2013 met our inclusion criteria and were recruited for this study. The duration from injury to surgery ranged from 3 days to 12 months. There were 60 patients with a meniscus injury, for whom the menisci were sutured, shaped, or resected according to the type of injury. All of the surgeries were performed by the same senior surgeon, with either STSB reconstruction (N = 36) or STDB reconstruction (N = 42) performed, which was randomized with closed envelopes. A flowchart of the patient selection process is presented in Fig. 1.
Allograft preparation
The anterior tibialis tendon allografts (Bone Tissue Engineering Library, Shanxi, China) were prepared on a back table after thawing in 37 °C normal saline. The length of the tendon (24–30 cm) was measured and doubled on itself; then the ends of the tendon were whip-stitched for about 35 mm with No. 2 Fiberwire suture (Arthrex). In the STSB group, the allograft was folded and weaved into a single bundle with a length of over 7 cm and a diameter of 8–9 mm. In the STDB group, the allografts were separated into AM and PL bundles. The AM bundle was over 6.5 cm in length and 6–7 mm in diameter, while the PL bundle was over 5.5 cm in length and 5–6 mm in diameter. Then the graft was clamped at either end on the preparation board with 10 lb of tension. The tendon allograft was kept moist until implantation.
Anesthesia and exposure
The surgeries were performed on patients in a supine position, with the affected knee flexing at an angle of 90° to allow the lower leg to naturally droop beside the bed. Epidural anesthesia was administered. A tourniquet was applied around the upper thigh. A routine external anterior approach under arthroscopy was performed in order to confirm the diagnosis of a torn ACL.
STSB ACL reconstruction
The knee was examined by arthroscopy following conventional procedures to confirm the diagnosis (Fig. 2A). In accordance with our previous publication [2], both the lateral intercondylar ridge and the lateral bifurcate ridge were important bony landmarks for the femoral attachments of the ACL. The femoral tunnel, which should not surpass the lateral intercondylar ridge, was created in the center of the lateral bifurcate ridge. A K-wire was placed into the lateral femoral condyle at the 1:30 or 10:30 position through the AM portal using a freehand technique at 120° of knee flexion (Fig. 2B). Using the inserted K-wire as the reference, a femoral tunnel was reamed to the lateral cortex of the distal femur using a 4.5 mm EndoButton drill. A 30 mm femoral socket that matched the prepared graft diameter was then created using a cannulated reamer. The tibial tunnel was placed at the center of the ACL remnant through the AM surface of the tibia at the level of the tibial tubercle using a tibial guide (Smith & Nephew Acufex) (Fig. 2C). The graft was first introduced into the tibial tunnel with a guide wire and then pulled directly into the femoral tunnel and fixed on the femoral side by flipping over the EndoButton (Smith & Nephew) (Fig. 2D, E). The tibial side was fixed using a hydroxyapatite interference screw (DePuy Mitek) with a diameter 1 mm larger than the graft at 3° of knee flexion under 40 N of initial tension.
STDB ACL reconstruction
After confirming the ACL rupture (Fig. 3A), both the femoral and tibial tunnels were created using a method similar to the STSB technique (Fig. 3B, C). The AM and PL bundles were looped over a single strand of suture, and a graft-positioning tool was used to achieve the desired position for each bundle. The graft was placed in the fork of the positioning tool with one bundle on either side of the fork. The single strand of the suture over which the graft was looped was passed through the femoral tunnel until it was out of the lateral thigh, and this suture was used to pull the graft into the tunnel. The graft-positioning tool was advanced through the tibial tunnel until it reached the aperture of the femoral tunnel. At this point, the AM and PL bundles were rotated by rotating the positioning tool to achieve their desired positions before they were advanced into the femoral tunnel (Fig. 3D, E). A femoral INTRAFIX screw (DePuy Mitek) was driven between the strands to separate the two bundles within the single tunnel. For the tibial tunnel fixation, the two bundles were placed in opposite quadrants of the sheath at their anatomical insertion sites on the tibial plateau using the tibial INTRAFIX system (DePuy Mitek). While the graft was secured, 40 N of graft tension were applied by an interference screw at full extension. Illustrative surgical diagrams are presented in Fig. 4.
Postoperative treatment and rehabilitation
Cefoxitin 1 g bid was administered during the first 48 h postoperatively to prevent infection in all the patients. The affected limb was wrapped in cotton pad for 72 h. Three-dimensional computed tomography (3D CT) was performed immediately after surgery to evaluate the bone tunnel and fixation, and MRI was applied to check the ligament healing at the last postsurgical follow-up.
The same postoperative rehabilitation plan was executed in both groups. The affected limb was immobilized with adjustable support. The patients were allowed to walk with crutches while being protected properly by knee braces on the second day after surgery. They were encouraged to flex their knees from 0 to 90° within 2–4 weeks and further to 120° within 6–8 weeks. However, they were instructed not to flex the knee over 120° in the first 3 months postoperatively. The braces were worn for at least 2 months. The patients were allowed to swim and ride a bicycle 6 months after surgery, begin jogging 10 months after surgery, and participate in strenuous exercises 18 months after surgery [16].
Outcome measures
Clinical outcome was assessed based on the International Knee Documentation Committee (IKDC), Lysholm, and Tegner scores and physical examinations performed both before surgery and at the last follow-up for all the patients.
Statistical analysis
Data were expressed as the mean ± standard deviation (SD) and analyzed by SPSS 18.0 software (SPSS Inc., Chicago, IL, USA). The independent-samples t-test and χ2 test were performed on the general data from the patients. Preoperative and postoperative IKDC, Lysholm, and Tegner scores and KT-3000 measurements were tested for Mann–Whitney U rank. Fisher’s exact test was used for the Lachman test and pivot shift test. P < 0.05 was considered statistically significant.
Results
Demographic characteristics and follow-up
The demographic characteristics of the 78 patients included are listed in Table 1. There was no statistical difference between the two groups in terms of gender, age, affected side, injury time interval, and follow-up duration.
Two patients in each group showed extension limitations preoperatively. Loose bodies were detected in the intercondylar fossa and were removed during arthroscopic examination. Postoperatively, all patients showed full extension of the knees. The average follow-up duration was 24.9 ± 1.8 months in the STSB group and 24.6 ± 1.7 months in the STDB group.
Clinical outcomes
Postoperative 3D CT showed accurate bone tunnels and properly positioned screws in both groups, and the low signal intensity of the ACL graft in the T2-weighted MRI at the last follow-up suggested graft maturation in both groups (Figs. 5, 6). No radiograph indicated joint space narrowing or degenerative change at the last follow-up.
All the patients had recovered their preoperative activity level at the last follow-up. The IKDC, Lysholm, and Tegner scores at the last follow-up were significantly improved in both groups compared to their preoperative status (P < 0.01), but there was no significant difference between the two groups preoperatively and at the last follow-up (Table 2).
Preoperatively, the Lachman test was positive in 32 patients (positive rate 88.9%) in the STSB group and 36 patients (positive rate 85.7%) in the STDB group (P = 0.74), and the pivot shift test was positive in 23 patients (positive rate 63.9%) in the STSB group and 29 patients (positive rate 69.0%) in the STDB groups (P = 0.63). The positive rates were significantly decreased at the last follow-up when compared to the preoperative status (P < 0.01). No significant difference was found in the Lachman test positive rate at the final follow-up between the two groups (P > 0.05). However, the pivot shift test rate was significantly lower in the STDB group than in the STSB group at the final follow-up (P = 0.01, Table 3).
Complications
There was no statistically significant difference in complications between the two groups (each group reported one case of infection who recovered after systematic anti-infection therapy). There were two cases in the STSB group and three cases in the STDB group who developed occasional pain and residual subjective joint instability. No stiffness, rejection reaction, graft failure, or deep venous thrombosis of the lower extremities was found in either group.
Discussion
Our results across over 2 years of follow-up indicated that the pivot shift test positive rate in the STDB group was significantly lower than that in the STSB group but that there was no significant difference in IKDC, Lysholm, and Tegner scores between the two groups at the final follow-up. Both techniques were found to improve knee joint function significantly compared with the preoperative status.
The argument regarding which technique is better for ACL reconstruction—STSB or DTDB—continues to this day [17, 18]. It has been proven that each of the two bundles of the ACL plays an irreplaceable role. Zantop et al. reported that the tibia shifted forward more significantly after transecting the AM bundle in the knee at 60° and 90° flexion and after transecting the PL bundle in the knee at 30° flexion [3]. Additionally, when flexing at 0° and 30°, the knee revolved more significantly after transecting the PL bundle than after transecting the AM bundle and in the normal situation. Several studies have found that there was no difference in the postoperative functional assessment and complications rate, but STSB reconstruction was inferior at restoring knee stability, particularly rotational stability [19, 20]. Järvelä et al. indicated that there was no significant difference in anterior stability between the two procedures, but DTDB gave significantly superior rotational stability [19], while Siebold et al. reported that DTDB led to superior anterior and rotational stability compared to the STSB procedure [20]. STDB reconstruction, as an alternative treatment option for restoring normal anatomic structures and biomechanical properties [21], involves reconstructing two bundles (AM and PL) with different functions by separating the two bundles of ligaments in the tunnel. This technique is characterized by a simple operation, an ability to simulate DTDB anatomic properties, and excellent anterior and rotational stability, and it can shorten the surgical time and decrease the difficulty and risk of the DBDT pattern [22, 23]. Gadikota et al. measured the biomechanical properties of a cadaveric knee specimen in the action of forward loading and found that STDB was more equivalent to a normal ACL in terms of its biomechanical properties compared to STSB reconstruction [24].
In this study, clinical outcomes, Tegner and Lysholm scores, and IKDC grades were compared between the STSB and STDB reconstruction procedures. Although no significant difference between the procedures in clinical functional scores and Lachman test positive rates was noted, the STDB technique showed a significantly lower pivot shift test positive rate than STSB at the last follow-up, indicating that STDB achieved better rotational stability. Ping et al. compared the therapeutic effects of bioabsorbable interference screws with EndoButtons fixation of the grafts in the treatment of ACL rupture through the STDB technique. No significant difference was found in Lysholm, IKDC, and Larson scores at the last follow-up [12]. In a later cadaveric study by those authors, biomechanical analysis was performed to compare STDB with STSB reconstruction using both methods. The results indicated that similar anterior–posterior stability was achieved using the two techniques, while STDB exhibited better rotational stability tested at 30° and 45° of knee flexion than STSB, which was consistent with our findings [13]. In Meuffels et al.’s study of fresh-frozen porcine knees, no significant difference in maximum failure load was found between the two techniques. However, the stiffness of the tibial tunnel complex was significantly higher in the STDB group [14]. Therefore, our results further strengthened the evidence supporting the application of this new technique in clinical practice.
Despite the merits shown, this study presents some limitations as well. Firstly, as it is a retrospective study, more prospective research, including randomized controlled trials, should be performed to provide further evidence. Secondly, the sample size was relatively small and there was a relatively short follow-up duration. More cases will be included and longer-term investigations will be conducted in the future. Moreover, previous cadaveric studies reported that the STDB technique might achieve better rotational stability [12, 13]. However, no quantitative data on the difference between the two methods could be collected from the patients. Only the clinical physical examination and the patient’s objective feeling of stability were measured in this study. Last but not least, the clinical outcome was not compared between STDB and DTDB, which points to a future direction for our research.
Conclusions
The stability and function of the knee joint can be restored well using either STSB or STDB ACL reconstruction with allograft. The STDB technique showed superior rotational stability at the final follow-up, accompanied by a satisfactory short-term curative effect.
Availability of data and materials
All relevant data for the research are included in the manuscript.
Abbreviations
- 3D CT:
-
Three-dimensional computed tomography
- ACL:
-
Anterior cruciate ligament
- AM:
-
Anteromedial
- DB:
-
Double-bundle
- DTDB:
-
Double-tunnel double-bundle
- IKDC:
-
International Knee Documentation Committee
- MRI:
-
Magnetic resonance imaging
- OP:
-
Osteoporosis
- OA:
-
Osteoarthritis
- PL:
-
Posterolateral
- STDB:
-
Single-tunnel double-bundle
- STSB:
-
Single-tunnel single-bundle
- SB:
-
Single-bundle
- SD:
-
Standard deviation
References
Kraeutler MJ, Wolsky RM, Vidal AF, Bravman JT (2017) Anatomy and biomechanics of the native and reconstructed anterior cruciate ligament: surgical implications. J Bone Joint Surg Am 99:438–445
Chen K, Zhu W, Zheng Y, Zhang F, Ouyang K, Peng L et al (2020) A retrospective study to compare the clinical effects of individualized anatomic single- and double-bundle anterior cruciate ligament reconstruction surgery. Sci Rep 10:14712
Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W (2007) The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med 35:223–227
Buoncristiani AM, Tjoumakaris FP, Starman JS, Ferretti M, Fu FH (2006) Anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy 22:1000–1006
Sundemo D, Sernert N, Kartus J, Hamrin SE, Svantesson E, Karlsson J et al (2018) Increased postoperative manual knee laxity at 2 years results in inferior long-term subjective outcome after anterior cruciate ligament reconstruction. Am J Sports Med 46:2632–2645
Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH (2012) Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am J Sports Med 40:512–520
Harner CD, Poehling GG (2004) Double bundle or double trouble? Arthroscopy 20:1013–1014
Caborn DN, Chang HC (2005) Single femoral socket double-bundle anterior cruciate ligament reconstruction using tibialis anterior tendon: description of a new technique. Arthroscopy 21:1273
Marcacci M, Molgora AP, Zaffagnini S, Vascellari A, Iacono F, Presti ML (2003) Anatomic double-bundle anterior cruciate ligament reconstruction with hamstrings. Arthroscopy 19:540–546
Takeuchi R, Saito T, Mituhashi S, Suzuki E, Yamada I, Koshino T (2002) Double-bundle anatomic anterior cruciate ligament reconstruction using bone-hamstring-bone composite graft. Arthroscopy 18:550–555
Kubo T, Hara K, Suginoshita T, Shimizu C, Tsujihara T, Honda H et al (2000) Anterior cruciate ligament reconstruction using the double bundle method. J Orthop Surg 8:59–63 (Hong Kong)
Ping LW, Bin S, Rui Y, Yang S, Zheng ZZ, Yue D (2012) Arthroscopic ACL reconstruction with reverse “Y”-plasty grafts and fixation in the femur with either a bioabsorbable interference screw or an endobutton. Knee 19:78–83
Li W, Song Y, Song B, Yang R, Xing T, Chen Z et al (2018) Comparison of anterior cruciate ligament reconstruction methods between reverse “Y” plasty reconstruction and traditional single-bundle technique—a cadaveric study. J Orthop Translat 14:1–7
Meuffels DE, Docter PT, van Dongen RA, Kleinrensink GJ, Verhaar JA, Reijman M (2010) Stiffer fixation of the tibial double-tunnel anterior cruciate ligament complex versus the single tunnel: a biomechanical study. Arthroscopy 26:S35-40
Debandi A, Maeyama A, Lu S, Hume C, Asai S, Goto B et al (2011) Biomechanical comparison of three anatomic ACL reconstructions in a porcine model. Knee Surg Sports Traumatol Arthrosc 19:728–735
Zhu W, Wang D, Han Y, Zhang N, Zeng Y (2013) Anterior cruciate ligament (ACL) autograft reconstruction with hamstring tendons: clinical research among three rehabilitation procedures. Eur J Orthop Surg Traumatol 23:939–943
Hantes ME, Tsarouhas A, Giakas G, Spiropoulos G, Sideris V, Christel P et al (2012) Effect of fatigue on tibial rotation after single- and double-bundle anterior cruciate ligament reconstruction: a 3-dimensional kinematic and kinetic matched-group analysis. Am J Sports Med 40:2045–2051
Gobbi A, Whyte GP (2019) Anatomic double-bundle and single-bundle ACL reconstruction after ACL rupture did not differ for quality of life at 2 years. J Bone Joint Surg Am 101:943
Järvelä T (2007) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc 15:500–507
Siebold R, Dehler C, Ellert T (2008) Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy 24:137–145
Lee BI, Kwon SW, Kim JB, Choi HS, Min KD (2008) Comparison of clinical results according to amount of preserved remnant in arthroscopic anterior cruciate ligament reconstruction using quadrupled hamstring graft. Arthroscopy 24:560–568
Zhu W, Lu W, Han Y, Hui S, Ou Y, Peng L et al (2013) Application of a computerised navigation technique to assist arthroscopic anterior cruciate ligament reconstruction. Int Orthop 37:233–238
Xiang X, Qu Z, Sun H, Ma X, Wang W, Huang L (2019) Single-tunnel anatomic double-bundle anterior cruciate ligament reconstruction has the same effectiveness as double femoral, double tibial tunnel: a prospective randomized study. Medicine 98:e14851
Gadikota HR, Wu JL, Seon JK, Sutton K, Gill TJ, Li G (2010) Single-tunnel double-bundle anterior cruciate ligament reconstruction with anatomical placement of hamstring tendon graft: can it restore normal knee joint kinematics? Am J Sports Med 38:713–720
Acknowledgements
None.
Funding
This research was funded by the National Natural Science Foundation of China (81902303, 81902682, 81672234), the Guangdong Basic and Applied Basic Research Foundation (2021A1515220030, 2021A1515011122, 2020A151501048), the Shenzhen Double Chain Project for Innovation and Development Industry supported by the Bureau of Industry and Information Technology of Shenzhen (201806081524201510), the Shenzhen Science and Technology Project (RCYX20210609103902019, RCBS20200714114856299, JCYJ20190806164216661, GJHZ20180416164801042, JCYJ20180305124912336), the Science and Technology Commission of Shanghai Municipality (Shanghai Sailing Program 19YF1408900), and the Clinical Research Project of Shenzhen Second People’s Hospital (20173357201814, 20203357028, 20203357007).
Author information
Authors and Affiliations
Contributions
ZD and WZ designed the research study. ZD performed the research. YZ, ZD, CL, YW, and KC provided help in data collection. ZF, HZ, and WL analyzed the data. ZD wrote the manuscript. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethical Committee of the First Affiliated Hospital of Shenzhen University, Shenzhen Second People’s Hospital. Written informed consent was obtained from the patients for the publication of this study and any accompanying images.
Consent for publication
Consent to publish was obtained from all the participants.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Deng, Z., Zheng, Y., Deng, Z. et al. Arthroscopic reconstruction of anterior cruciate ligaments with allograft: single-tunnel single-bundle versus single-tunnel double-bundle techniques. J Orthop Traumatol 23, 26 (2022). https://doi.org/10.1186/s10195-022-00649-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10195-022-00649-4