Abstract
Background
There is still little information about the long-term results of clinical and radiological evolution in patients older than 65 years with complex proximal humerus fractures (CPHF) treated acutely with reverse shoulder arthroplasty (RSA). The aim of this paper was to evaluate function and results 7 years after surgery.
Material and methods
A prospective cross-sectional cohort study was designed for this purpose. Patients who underwent RSA surgery during 2012 because of a CPHF were included. The surgical approach was randomized (deltopectoral vs anterosuperior). Functional activity, evolution of tuberosities and evidence of scapular notching 7 years after surgery were analyzed.
Results
After evaluating 32 patients, the Constant score improved from 64.83 in the first year to 69.54 at 7 years postoperative. Results were independent of the approach used. Functional outcomes were poorer in patients with scapular notching and when tuberosities were resorbed or displaced.
Conclusions
At 7 years, function in patients undergoing RSA after CPHF demonstrated improvement in all patients except those who developed scapular notching or when tuberosities did not consolidate in an anatomical position. These results are completely independent of the approach used.
Level of evidence
III Controlled cohort study.
Similar content being viewed by others
Introduction
Reverse shoulder arthroplasty (RSA) was first developed as an alternative treatment for rotator cuff arthropathy. Since then, it has proven to be an effective implant for many shoulder disorders. For this reason, there has been a gradual increase in the last decade in its use for proximal humerus fractures in elderly patients [1]. Clinical studies of RSA in this kind of fracture have shown improved outcomes when compared with hemiarthroplasty [2, 3].
However, in the current literature, it is difficult to find long-term data about clinical and radiological results in patients over 65 years with complex fractures of the proximal humerus treated with RSA [4,5,6]. This may be due to many factors. The first of them might be that orthopedic surgeons are still developing in this field and there are no solid long-term results yet. But there are other factors that may influence these results, such as the approach used, the condition of the tuberosities, and the appearance of scapular notching.
The aim of this paper was to evaluate the medium-term functional activity of complex fractures of the proximal humerus treated by a reverse shoulder prosthesis. Moreover, clinical results are compared with the two main approaches used, the final state of the tuberosities and the development of scapular notching.
Material and methods
A prospective cross-sectional cohort study was designed to include patients who were treated at our hospital during 2012 for a complex proximal humerus fracture and treated by reverse shoulder replacement. The cohort for this study was analyzed on two occasions: (1) 12 months postoperatively, and (2) after 7 years, to determine whether or not functional activity decreases with time.
The inclusion and exclusion criteria are shown in Table 1.
The surgery was always performed by the same surgeon and the implant used was the stem-cemented Delta XTEND reverse prosthesis system from DepuySynthes (DePuy Orthopaedics, Warsaw, IN, USA).
The choice of which approach to use was randomized according to the history number of the patient. If the number was even, a deltopectoral approach was used, and if the number was odd, an anterosuperior approach was used. All patients were assessed by the rehabilitation department following surgery.
Functional activity and quality of life were evaluated through the Constant score and the Hospital for Special Surgery (HSS) score, 1 and 7 years after surgery [7, 8]. All of these measures are expressed as mean ± SD (standard deviation).
Radiographic controls were performed by protocol at 3, 6, and 12 months and annually afterwards (true AP, axial and scapular plane projections). For this study, 12-month and 7-year X-rays were used to evaluate scapular notching, the loosening of the prosthetic components, and the condition of the tuberosities. The existence of notching was classified according to the classification of Nérot and Sirveaux [9] as grade 1: limited to the external pillar; grade 2: in contact with the inferior screw; grade 3: extension beyond the inferior screw; and grade 4: extension beyond the baseplate of the prosthesis. The condition of the tuberosities was also determined by X-ray and divided into three groups: normal (N) when the tuberosities consolidated in the normal anatomical location, resorption (R) when the tuberosities were absent, and displaced (D) when the tuberosities consolidated in a poor non-anatomical position [10, 11].
SPSS software (IBM Inc, Armonk, NY, USA) was used for the statistical analysis. A descriptive analysis of the variables studied was performed and Student’s t-test was used for independent samples (p < 0.05) to determine whether there were any improvements in terms of functionality (Constant and HSS scores). Pearson’s chi-square test was used to determine whether differences in functionality depended on the type of surgical approach. An analysis of variance test (ANOVA) was performed to determine whether the functional results depended on the state of the tuberosities or the appearance of scapular notching. This study was approved by the ethics committee of our hospital, reference number 279-3954 (Protocolo COTINV: ver 3.1).
Results
In 2012, a total of 43 patients underwent reverse shoulder replacement for a complex fracture of the proximal humerus. Of them, 40 patients met the inclusion criteria (35 patients with 3- or 4-part fractures and 5 with fracture-dislocation). During the follow-up period, eight patients were excluded, four due to death and four who were lost to follow-up; therefore, 32 patients remained in the study cohort (3 men and 29 women). The mean age was 74.14 years (range 65–87). A deltopectoral approach was used in 13 patients (40.6%) and an anterosuperior approach was used in 19 patients (59.3%). The primary data can be seen in Tables 2 and 3.
After analyzing the whole cohort the first year, the mean Constant was 64.83 (± 12.01) and the mean HSS was 60.75 (± 11.17). Evaluated independently, patients with an anterosuperior (AS) approach had a mean Constant of 67.69 (± 12.23) and a mean HSS of 62.85 (± 12.09). Patients with a deltopectoral (DP) approach had a mean Constant of 61.45 (± 11.37) and a mean HSS of 58.27 (± 9.95). With a paired Student’s t-test (p < 0.05), there were no statistically significant differences between the two approaches in terms of Constant and HSS (Fig. 1).
When the cohort was reviewed at 7 years, the mean Constant was 69.54 (± 14.82) and the mean HSS was 64.46 (± 12.78). Evaluated independently, patients with an anterosuperior (AS) approach had a mean Constant of 73.31 (± 13.22) and a mean HSS of 68.15 (± 12.74). Patients with a deltopectoral (DP) approach had a mean Constant of 65.09 (± 15.98) and a mean HSS of 60.07 (± 11.94). With a paired Student’s t-test (p < 0.05), there were no statistically significant differences between the two approaches in terms of Constant and HSS (Fig. 2).
In the radiographic assessment at 7 years, eight of the 32 patients had scapular notching (six grade 1 and two grade 2). Patients with no notching had a mean Constant of 64 (± 12.39) and a mean HSS of 60.31 (± 12.18) at 12 months and their function had improved significantly at 7 years (p < 0.05) to a mean Constant of 72.06 (± 12.89) and a mean HSS of 64.69 (± 11.77). On the other hand, patients who developed scapular notching went from a mean Constant of 66.5 (± 11.85) and a mean HSS of 61.63 (± 9.53) at 12 months to a mean Constant of 64.5 (± 17.96) and a mean HSS of 64 (± 15.49) at 7 years, with no statistically significant change. Among patients with notching, 3 underwent surgery by DP approach and 5 by AS approach, with no statistically significant differences between the approach and the existence of scapular notching.
When relating the functional results to the condition of the tuberosities, the mean Constant in the N group (22 patients) was 70.07 (± 17.08) and the mean HSS was 62.91 (± 15.64). The mean Constant in the R group (7 patients) was 67.85 (± 9), with a mean HSS of 67.85 (± 7.9). Finally, the mean Constant in the D group (3 patients) was 71 (± 19.31) with a mean HSS of 63.66 (± 6.65). There were no statistically significant differences (p > 0.05) with respect to the functional results and the condition of the tuberosities (Fig. 3).
During the follow-up period, the following major complications occurred: one periprosthetic fracture (treated with osteosynthesis) and one prosthetic dislocation (resolved through closed reduction with no need for replacement). No signs of component loosening were reported on follow-up control radiographs.
Discussion
Fractures of the vertebrae, hip, distal radius, and humerus are the most common fractures in osteoporosis. The average risk of suffering a fracture of the humerus has been estimated as 12.9% for women and 4.1% for men over the course of their lives [12]. They represent the third most common fracture in individuals over 65 years of age [13, 14]. Our study shows how complex proximal humerus fractures (CPHF) in the elderly population can be treated by reverse shoulder arthroplasty, obtaining good results in the medium term.
Non-displaced and minimally displaced fractures are usually treated without surgery, with satisfactory outcomes [15,16,17]; meanwhile, displaced fractures, according to Neer’s criteria, usually require surgical intervention [18, 19]. Historically, complex fractures of the humerus include: four-part fractures, three-part fractures in osteoporotic bone, displacement fractures, and fractures that involve 40% to 50% of the joint surface [3].
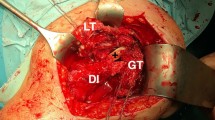
Since Grammont developed the reverse total shoulder arthroplasty (RSA) for cuff tear arthropathies in 1985 [20], its indications have increased, including its use for fractures of the proximal humerus in patients over 65 years old. Many studies recommend the use of RSA in fractures as an appropriate alternative [3, 6, 21,22,23,24]. This study is among the longest follow-up time in patients over 65 with reverse prosthesis due to trauma (complex fractures of the proximal humerus). We aimed to determine the relationship between functional results and important parameters such as the approach used, tuberosities, and scapular notching (Fig. 4).
The superior or anterosuperior (AS) approach was the original recommended approach for RSA by Grammont. As the procedure became more popular and indicated in more complex situations, many shoulder surgerons utilized the deltopectoral (DP) approach in an effort to gain better access to the proximal humerus [25, 26]. While some surgeons feel that the AS approach affords better and less invasive exposure to the glenoid surface, a controversy remains as to which is the best approach and which one to choose depending on the situation [25, 27].
Many authors have compared both approaches for rotator cuff arthropathy [25, 27,28,29]. All of them determined that both approaches have similar results. However, there are two complications that have been described with greater frequency in the AS approach: scapular notching and glenoid loosening [5, 6, 28, 30, 31]. In our study, we found no differences between scapular notching and the approach used and no glenoid loosening was reported, similar to other studies [32,33,34]. However, the number of patients is smaller than in rotator cuff arthropathy studies, so, in our opinion, it is not possible to draw conclusions based on the incidence of notch and the type of approach.
When relating functional outcomes and both the approaches used, results were similar, as reported previously in the literature [32,33,34]. Analyzing more carefully, although no statistically significant differences were found between the two approaches, there did seem to be a tendency for better clinical results with AS; future studies with a larger sample may clarify these results.
One of the greatest difficulties when implanting an RSA after a fracture involves fixation of the tuberosities. In fact, their proper consolidation has been described as one of the main prognostic factors for functional recovery [35]. Many studies show better functional outcomes after correct healing [10, 36,37,38]. In our study, 22 out of 32 patients (68.75%) had normal consolidation of the tuberosities, but this finding was not reflected in a difference of function compared with the rest of the patients (resorption and displaced tuberosities), as has already been described by other authors [6, 36].
Various authors argue that function in patients with an RSA decreases in time due to the micro-loosening of the components and depletion of the deltoid muscle [5, 10, 39]. However, as our study demonstrates, along with others [36, 37], functional results are not only maintained, but even improved over time (measured according to Constant and HSS scores). Moreover, scapular notching is a factor that is usually related to a significant decrease in function [32, 33, 40]. However, in our study, those patients who did not develop notching did improve their function over time, and patients with notching maintained their function at 7 years. The RSA has been shown to be an effective short- and medium-term treatment for a wide variety of shoulder conditions including complex proximal humerus fractures [34, 41,42,43]. The authors believe that the use of RSA instead of osteosynthesis may be an advantage in some patients, and that selected patients should include those with complex proximal humerus fractures over 65 years of age, with more than 3–4 displaced fragments, in which the tuberosities are highly comminuted or the osteosynthesis does not guarantee a good position for them. In such cases, the authors believe that results are more predictable and even better with RSA.
Conclusions
Patients over 65 years old with a complex fracture of the proximal humerus who were treated with reverse shoulder arthroplasty, obtained very good results (constant and HSS scores) at 7 years of follow-up, demonstrating its effectiveness in the medium term. Moreover, those patients who did not develop scapular notching improved their function with respect to the first postoperative year. Neither the approach used for RSA implantation (deltopectoral or anterosuperior), nor the state of the tuberosities (normal, absent, or displaced) influenced the final functional outcomes.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Acevedo DC, VanBeek C, Lazarus MD et al (2014) Reverse shoulder arthroplasty for proximal humeral fractures: update on indications, technique, and results. J Shoulder Elb Surg 23:279–289. https://doi.org/10.1016/j.jse.2013.10.003
Baudi P, Campochiaro G, Serafini F et al (2014) Hemiarthroplasty versus reverse shoulder arthroplasty: comparative study of functional and radiological outcomes in the treatment of acute proximal humerus fracture. Musculoskelet Surg. https://doi.org/10.1007/s12306-014-0322-3
Boyle MJ, Youn SM, Frampton CMA, Ball CM (2013) Functional outcomes of reverse shoulder arthroplasty compared with hemiarthroplasty for acute proximal humeral fractures. J Shoulder Elb Surg 22:32–37. https://doi.org/10.1016/j.jse.2012.03.006
Seidl AJ, Sholder D, Warrender W et al (2017) Early vs. late reverse shoulder arthroplasty for proximal humerus fractures: does it matter? J Shoulder Elb Surg 26:e143. https://doi.org/10.1016/j.jse.2016.12.003
Kaisidis A, Pantos PG, Heger H et al (2014) Reverse shoulder arthroplasty for the treatment of three and four part fractures of the proximal humerus in patients older than 75 years old. Acta Orthop Belg 80:99–105
Bufquin T, Hersan A, Hubert L, Massin P (2007) Reverse shoulder arthroplasty for the treatment of three- and four-part fractures of the proximal humerus in the elderly: a prospective review of 43 cases with a short-term follow-up. J Bone Jt Surg Br. 89-B:516–520. https://doi.org/10.1302/0301-620X.89B4.18435
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 160–164
Rozing PM, Nagels J, Rozing MP (2011) Prognostic factors in arthroplasty in the rheumatoid shoulder. HSS J 7:29–36. https://doi.org/10.1007/s11420-010-9172-1
Sirveaux F, Favard L, Oudet D et al (2004) Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Jt Surg Br 86:388–395
Ohl X, Bonnevialle N, Gallinet D et al (2018) How the greater tuberosity affects clinical outcomes after reverse shoulder arthroplasty for proximal humeral fractures. J shoulder Elb Surg 27:2139–2144. https://doi.org/10.1016/j.jse.2018.05.030
Boileau P, Krishnan SG, Tinsi L et al (2002) Tuberosity malposition and migration: reasons for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. J shoulder Elb Surg 11:401–412
Johnell O, Kanis J (2005) Epidemiology of osteoporotic fractures. Osteoporos Int 16(Suppl 2):S3-7. https://doi.org/10.1007/s00198-004-1702-6
Baron JA, Barrett JA, Karagas MR (1996) The epidemiology of peripheral fractures. Bone 18:209S-213S
Roux A, Decroocq L, El Batti S et al (2012) Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res 98:715–719. https://doi.org/10.1016/j.otsr.2012.05.013
Neer CS 2nd (1970) Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 52:1077–1089
Rasmussen S, Hvass I, Dalsgaard J et al (1992) Displaced proximal humeral fractures: results of conservative treatment. Injury 23:41–43
Koval KJ, Gallagher MA, Marsicano JG et al (1997) Functional outcome after minimally displaced fractures of the proximal part of the humerus. J Bone Joint Surg Am 79:203–207
Neer CS 2nd (1970) Displaced proximal humeral fractures. II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am 52:1090–1103
Young SW, Segal BS, Turner PC, Poon PC (2010) Comparison of functional outcomes of reverse shoulder arthroplasty versus hemiarthroplasty in the primary treatment of acute proximal humerus fracture. ANZ J Surg 80:789–793. https://doi.org/10.1111/j.1445-2197.2010.05342.x
Grammont P, Trouilloud P, Laffay J, Deries (1987) Etude et realisation d’une nouvelle prothese d’epaule. Rheumatologie 39:17–22
Jobin CM, Galdi B, Anakwenze OA et al (2015) Reverse shoulder arthroplasty for the management of proximal humerus fractures. J Am Acad Orthop Surg 23:190–201. https://doi.org/10.5435/JAAOS-D-13-00190
Mattiassich G, Marcovici LL, Krifter RM et al (2013) Delta III reverse shoulder arthroplasty in the treatment of complex 3- and 4-part fractures of the proximal humerus: 6 to 42 months of follow up. BMC Musculoskelet Disord 14:231. https://doi.org/10.1186/1471-2474-14-231
Lenarz C, Shishani Y, McCrum C et al (2011) Is reverse shoulder arthroplasty appropriate for the treatment of fractures in the older patient? Early observations. Clin Orthop Relat Res 469:3324–3331. https://doi.org/10.1007/s11999-011-2055-z
Anakwenze OA, Zoller S, Ahmad CS, Levine WN (2014) Reverse shoulder arthroplasty for acute proximal humerus fractures: a systematic review. J Shoulder Elb Surg 23:e73–e80. https://doi.org/10.1016/j.jse.2013.09.012
Gillespie RJ, Garrigues GE, Chang ES et al (2015) Surgical exposure for reverse total shoulder arthroplasty. differences in approaches and outcomes. Orthop Clin North Am 46:49–56. https://doi.org/10.1016/j.ocl.2014.09.015
Uct SRM, Ortho FCSSA (2015) Reverse total shoulder arthroplasty for complex proximal humeral fractures in the elderly: how to improve outcomes. Correspondence 14:25–33
Ladermann A, Lubbeke A, Collin P et al (2011) Influence of surgical approach on functional outcome in reverse shoulder arthroplasty. Orthop Traumatol Surg Res 97:579–582. https://doi.org/10.1016/j.otsr.2011.04.008
Levigne C, Boileau P, Favard L et al (2008) Scapular notching in reverse shoulder arthroplasty. J Shoulder Elb Surg 17:925–935. https://doi.org/10.1016/j.jse.2008.02.010
Melis B, DeFranco M, Ladermann A et al (2011) An evaluation of the radiological changes around the Grammont reverse geometry shoulder arthroplasty after eight to 12 years. J Bone Joint Surg Br 93:1240–1246. https://doi.org/10.1302/0301-620X.93B9.25926
Cheung E, Willis M, Walker M et al (2011) Complications in reverse total shoulder arthroplasty. J Am Acad Orthop Surg 19:439–449
Aibinder WR, Clark NJ, Schoch BS, Steinmann SP (2018) Assessing glenosphere position: superior approach versus deltopectoral for reverse shoulder arthroplasty. J Shoulder Elb Surg 27:455–462. https://doi.org/10.1016/j.jse.2017.10.013
Friedman RJ, Barcel DA, Eichinger JK (2019) Scapular notching in reverse total shoulder arthroplasty. J Am Acad Orthop Surg 27:200–209. https://doi.org/10.5435/JAAOS-D-17-00026
Mollon B, Mahure SA, Roche CP, Zuckerman JD (2017) Impact of scapular notching on clinical outcomes after reverse total shoulder arthroplasty: an analysis of 476 shoulders. J shoulder Elb Surg 26:1253–1261. https://doi.org/10.1016/j.jse.2016.11.043
Wall B, Nove-Josserand L, O’Connor DP et al (2007) Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am 89:1476–1485. https://doi.org/10.2106/JBJS.F.00666
Kralinger F, Schwaiger R, Wambacher M et al (2004) Outcome after primary hemiarthroplasty for fracture of the head of the humerus. A retrospective multicentre study of 167 patients. J Bone Joint Surg Br 86:217–219
Torrens C, Alentorn-Geli E, Mingo F et al (2018) Reverse shoulder arthroplasty for the treatment of acute complex proximal humeral fractures: influence of greater tuberosity healing on the functional outcomes. J Orthop Surg (Hong Kong) 26:2309499018760132. https://doi.org/10.1177/2309499018760132
Jain NP, Mannan SS, Dharmarajan R, Rangan A (2019) Tuberosity healing after reverse shoulder arthroplasty for complex proximal humeral fractures in elderly patients—does it improve outcomes? A systematic review and meta-analysis. J Shoulder Elb Surg 28:e78–e91. https://doi.org/10.1016/j.jse.2018.09.006
Simovitch RW, Roche CP, Jones RB et al (2019) Effect of tuberosity healing on clinical outcomes in elderly patients treated with a reverse shoulder arthroplasty for 3- and 4-part proximal humerus fractures. J Orthop Trauma 33:e39–e45. https://doi.org/10.1097/BOT.0000000000001348
Wright JO, Ho A, Kalma J et al (2019) Uncemented reverse total shoulder arthroplasty as initial treatment for comminuted proximal humerus fractures. J Orthop Trauma 33:e263–e269. https://doi.org/10.1097/BOT.0000000000001465
Simovitch RW, Zumstein MA, Lohri E et al (2007) Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J Bone Joint Surg Am 89:588–600. https://doi.org/10.2106/JBJS.F.00226
Boileau P, Gonzalez J-F, Chuinard C et al (2009) Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elb Surg 18:600–606. https://doi.org/10.1016/j.jse.2009.03.011
Drake GN, O’Connor DP, Edwards TB (2010) Indications for reverse total shoulder arthroplasty in rotator cuff disease. Clin Orthop Relat Res 468:1526–1533. https://doi.org/10.1007/s11999-009-1188-9
Frankle M, Levy JC, Pupello D et al (2006) The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. a minimum two-year follow-up study of sixty patients surgical technique. J Bone Joint Surg Am 88(1):178–190. https://doi.org/10.2106/JBJS.F.00123
Acknowledgements
The authors would like to thank Maite Urbano Luque, Juan Carlos Díaz Alcaide, and María de los Ángeles Miñarro del Moral for their continous help and support. Life is better thanks to them.
Funding
The authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Author information
Authors and Affiliations
Contributions
AIF: surgeon. MGR: patient data recording. MUL: statistical analysis. MGC: patient data recording. RQR: patient data recording. JCM: surgeon and major contributor to writing the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
During the study, national and international guidelines for biomedical research in human beings was followed (code of ethics, declaration of Helsinki). The study complied with legal regulations about confidentiality of patient data, the Spanish Personal Data Protection Act (Organic law 15/1999 of 13 December) according to the legislation compliance control body of the Spanish Data Protection Agency (AEPD). Institutional Review Board approval was obtained for this study (COTINV.ver3.1). All patients signed an informed consent form prior to their inclusion in the study
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Izquierdo-Fernández, A., Gómez-Rodríguez, M., Urbano-Luque, M. et al. Reverse shoulder arthroplasty in complex fractures of the proximal humerus: results after 7 years of follow-up. J Orthop Traumatol 22, 38 (2021). https://doi.org/10.1186/s10195-021-00597-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10195-021-00597-5