Abstract
Purpose
Reverse total shoulder arthroplasty (RSA) has revolutionized the management of proximal humerus fractures (PHF) in the elderly patients. There is few or no consensus regarding to management of postoperative rehabilitation in elderly patients. An early rehabilitation from D1 allowed better functional results compared to rehabilitation started to D30 independently from tuberosities consolidation.
Methods
94 patients operated on for PHF were evaluated retrospectively, with a minimum radio-clinical follow-up of 2 years. Clinical evaluation included mobilities and four functional scores: ASES, quick DASH, gross constant, weighted constant. Radiological evaluation was performed on a frontal shoulder X-ray with evaluation of tuberosities’ consolidation.
Results
The mean follow-up was 45 ± 19 months (24–88 months). Early rehabilitation was significantly associated with a better Constant Score (71.1 ± 17.2 vs. 56.4 ± 15.8; p < 0.001), better adjusted Constant score (92.4 ± 14.2 vs. 80.3 ± 19.5; p < 0.001), better quick DASH (22.8 ± 19.8 vs. 36.7 ± 21.3; p < 0.01), better ASES (78.6 ± 20.2 vs. 63 ± 22; p < 0.001).
Conclusion
In traumatology, functional result of RSA seems not related in tuberosities’ union but in rehabilitation in order to limit postoperative stiffness of operated shoulder. An early rehabilitation is related with better clinical and functional results, independently of tuberosities’ union.
Level of evidence
3, control-case study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures of proximal head of humerus (FPH) are the third most common fracture in the elderly with increment of incidence due to aging of the population [1, 2]. Reverse shoulder arthroplasty (RSA) has become gold standard for FPH with better outcomes than hemiarthroplasties [3]. Absence of rotator cuff in elderly patients justify use of RSA. It also provides more predictable results with better function even in cases of tuberosities’ malunion [4,5,6,7,8].
New concepts derived from Grammont’s prosthesis allowed development of dedicated prosthetic device to FPHs. It allows tuberosities’ osteosynthesis on the prosthesis and theoretically their consolidation [9]. It is know that clinical results depend on age, type of implant, surgery approach but rehabilitation protocol have not been evaluated yet [10, 11]. Immobilization is necessary to favorise tuberosities’ union and prevent risk of luxation, nevertheless immobilization is associated with postoperative shoulder stiffness and decrease in functional result [12,13,14,15,16].
Objective was to compare two rehabilitation protocols: one starting to postoperative D1 and one starting to postoperative D30 for elderly patients who have been operated for FPH by RSA [Humelock Reversed (FX Solution, Viriat, FRANCE)]. Main hypothesis was that rehabilitation started at D1 provides better functional results than rehabilitation started at D30 independently from tuberosities’ union.
Material and method
Local Ethics Committee approved the study and the French data protection authority attributed the number ar21-0018v0.
Patients
We conducted a bi-centric, retrospective, multi-operator study. It compared functional outcomes of elderly patients having a FPH who underwent for RSA (Humelock Reversed, FX solutions, Viriat, France). Between January 2013 and December 2019, patients over 60 years old with Neer stage 3 or 4 FPH [17] and for whom RSA (Humelock Reversed) was performed were included. A minimum of 24 months of clinico-radiological follow-up was required. Patients with mental disorders were not eligible to participate to the study. Pathological fractures were excluded.
Surgical technique
The Humelock Reversed prosthesis (Humelock Reversed 1 and 2, FX solutions, Viriat, France) which is a dedicated prothesis for FPH with a cervico-diaphyseal angle of 145° allowing protection of the scapular pillar was used in this study. All surgery was performed by senior surgeons.
A delto-pectoral approach was performed in beachchair position with fluoroscopy. The tendon of longus biceps brachii and tendon of supraspinatus were resected. The humerus has been prepared by successive reamers for diaphysial part and successive rapes for metaphyseal part. A dedicated K-wire was positioned 12 mm from the inferior edge of the glenoid to guide reaming of glenoid. Only, 24-mm metaglene with 4 locking screws was implanted for all patients. Then, the dedicated glenosphere was impacted and screwed in place. Height of humeral component was defined by the pectoralis major tendon marker [18]. The rotation was fixed with a retroversion between 10 and 20° respecting the forearm. The stem was thus stabilized with 2 screws using a specific ancillary. Tuberosities’ osteosuture was systematically performed either by 3 systems of 2 loop wires allowing creation of self-locking lark’s head knots (Fig. 1) [19, 20].
Evaluation method
Objective was to compare two rehabilitation protocols: early rehabilitation (ER) and delayed rehabilitation (DR) for patients with FPH underwent RSA considering functional, clinical and radiological outcomes.
The patients in the early rehabilitation (ER) group were all included in the same orthopedic department and the patients in the delayed rehabilitation (DR) group were also all recruited in the second orthopedic department. Patients had standardized physio therapy that was started immediately after surgery or delayed it depending on the group. Need for hospitalization in convalescent centers was decided according to social context. There was no difference in rehabilitation performed in a convalescent center, in hospital or at home.
The only difference between the two compared groups was the delayed for starting rehabilitation and as well immobilization. For ER group, postoperative RSA rehabilitation started à D1 whereas for DR group its started at D30.
In ER group, an immobilization such as a vest elbow to the body was placed for analgesic purposes between the rehabilitation sessions; in RD group, the vest was strictly wear for the first 30 days and then for analgesic purposes once physical therapy had begun.
One hundred and fifty-nine patients were eligible, eleven were excluded, eighteen died before the last follow-up, thirty-six did not have complete reports (clinical or radiological outcomes missing), finally, ninety-four patients (59%) were reassessed at least 24 months after surgery. The mean follow-up was 45 ± 19 months [24–88]. The mean age at surgery was 77 ± 8 years [63–97 years]. We had had 45 patients in ER group versus 49 in the RD group. The characteristics of the two groups are reported in Table 1.
The flow-chart summarizes the population (Fig. 2).
Clinical evaluation
Because of health context (Covid-19), patients review was either physical interview either distancial interview with self-questionnaires sent to patients. Follow-up was standardized with medical evaluation at M1, M3, M6, one year and then every year with radio-clinical follow-up. Absolute and adjusted Constant-Murley score, quick DASH, ASES scores were performed [21,22,23,24]. Active shoulder mobilities: anterior elevation (AE), abduction (ABD), lateral rotation 1 (LR1), and medial rotation (MR) were assessed in each group regarding to rehabilitation protocol.
Radiological evaluation
Radiological follow-up (AP frontal view with neutral rotation, medial rotation, lateral rotation and a Neer view) of operated shoulder was performed at each consultation. At revision, tuberosities’ union, osteolysis, secondary displacement of major tubercule were noted according to X-rays. Notch on scapula was also noted and appreciated by the Sirveaux’s classification [25]. To limit potential biases, radiological analysis had been realized two times two weeks apart by an independent reviewer in each group.
Complications
Peroperative, early and late postoperative complications were collected in both groups.
Statistical analysis
Quantitative variables were described by their mean and standard deviation, their normality was verified by the Shapiro–Wilk test. Univariate analysis of categorical variables was performed using Pearson’s Chi 2 test. For quantitative variables, the two-sample Welch’s t-test was used. A p value < 0.05 was considered significant. Statistical analyses and graphical representations were performed using the R-based software pvalue.io.
Results
The ER and DR groups were comparable on demographic data (Table1).
Anterior elevation was significantly higher in the ER group than in the DR group: 131 ± 27.4 [75–170] versus 123 ± 16.1 [45–150] (p < 0.001), as was abduction: 116 ± 32.0 [30–170] versus 101 ± 23.2 [45–150] (p = 0.011). Concerning the other mobilities, no difference on the sectors of mobilities was found.
The ER group had significantly better functional results than DR on: absolute constant score 71.1 ± 17.2 [30–95] versus 56.4 ± 15.8 [22–83] (p < 0.001) and adjusted constant 92.4 ± 14.2 [46–100] versus 80.3 ± 19.5 [34–100] (p < 0, 001), ASES score 78.6 ± 20.2 [31.6–101] versus 63.0 ± 22.0 [23–96.6] (p < 0.001) and quick DASH 22.8 ± 19.8 [0–70.5] versus 36.7 ± 21.3 [4.5–58.3] (p < 0.01).
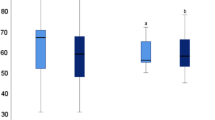
Radiologically, there was significantly less anatomical tuberosities’ union in the ER group than in the DR group (33% of cases vs. 45%, p < 0.01) and significantly more mal union in ER group than in DR group (44% of cases vs. 14%, p < 0.01). Nevertheless, clinical and functional analysis according to tuberosities’ union did not reveal significant differences between the groups (Fig. 3). These results are presented in Table 2.
No intraoperative complications were identified.
Concerning early or late complications rate, there was no significant difference in the two groups. Concerning revision, there were three reinterventions in the ER group (2 for removal of locking screws of the stem and 1 for stem sweeping requiring a new locking) and no revisions in the DR group. A total of 15 patients had postoperative complications, a rate of 16%, with a revision rate of 3%. These results are presented in Table 3.
Discussion
Early rehabilitation after RSA for FPH in elderly patients provides better functional results. To our knowledge, this is one of the first studies comparing early and delayed rehabilitation after RSA in traumatology.
The device used in this study is a traumatology dedicated reverse shoulder prosthesis with a locked stem that provides a good primary stability especially in porotic bone. The locking shaft system far from axillary nerve zone avoids lesion of the radial nerve because of 20° retroversion remains an additional advantage compared to other device not dedicated to traumatology [8]. Furthermore, this locking system seems better for adjustment of humeral stem (height and rotational) and its decreases risks associated with cement using in particular in elderly patients. [26, 27].
The RSA is a reliable means of managing fractures of FPH in the elderly RSA is reliable means FPH managing fractures in elderly [28, 29]. It is admitted that tuberosities’ anatomical union is necessary to obtain a functional shoulder and it is accepted that immobilization is necessary to promote that union. However, immobilization seems deleterious for functional recovery of shoulder [30]. It has been demonstrated that immobilization decrease functional recovery in elderly patients. Moreover, it seems to be even more deleterious especially in this population [7]. As we can notice it in our study, ER group had better clinical and functional results despite less tuberosities’ anatomical union. Furthermore, analysis according to tuberosities’ union did not show a statistically significant difference between ER group and DR group, as also reported by Fortané et al. [31].
It seems that FPH is equivalent to proximal femoral fractures for correlation morbidity and mortality after these fractures [32]. As we can notice it, large part of the population died within the 2 years after their fracture, it reflects fragility of the population treated. So, it is essential to provide the best operative treatment and best postoperative management in order to retrieve the best functional function as it is proposed for lower limb fracture [33]. There’s consensus about early mobilization in elderly patients to decrease inconvenient and limitation due to use of sling [34]. A recent review of literature shows no consensus for postoperative rehabilitation protocol after RSA and publications concerning rehabilitation protocol avec RSA in traumatology are very rare [14, 35,36,37]. Both groups have very satisfactory clinical and functional results comparatively to literature [8, 11, 38, 39]. Nevertheless, we found a statistically significant difference in anterior elevation, abduction and for the 4 functional scores with better outcomes in ER group.
Rehabilitation protocols are based on common principles but its differ regarding to several variables: postoperative delay, authorized movements, active/passive work, short and long term precautions which can explication for a part of complications [37, 40, 41]. Concerning complications, only one case of luxation was reported. It belung to DR group which seems paradoxal because immobilization remains a protection for luxation. Other complications were related to prosthetic surgical more than rehabilitation protocol.
Problems related with locking of the stem are about 5% in our series, this rate is similar to data of the Symposium of the French Orthopedic Society in 2019. Nevertheless, early rehabilitation could explain mobilization of stem or locking screws [11, 42].
Main strength of this work remains the follow-up of 45 ± 19 months with a minimum follow-up of 2 years, on a multicenter population of 94 patients, with a single type of surgery. Moreover, it is one of the first study to focus on rehabilitation in elderly. Until now, there is no consensus attitude regarding to the literature for shoulder rehabilitation after RSA in elderly. It is nevertheless a fundamental easily modifiable parameter that remains understudied in traumatology.
Conclusion
Early rehabilitation provides better clinical and functional results than delayed rehabilitation after RSA performed for FPH in the elderly. It appears that tuberosities’ union do not impact on functional results.
References
Roux A, Decroocq L, El Batti S, Bonnevialle N, Moineau G, Trojani C et al (2012) Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Res Surg 98(6):715–719
Court-Brown C, Duckworth A, Biant L, McQueen M (2017) The changing epidemiology of fall-related fractures in adults. Injury 48(4):819–824
Gallinet D, Ohl X, Decroocq L, Dib C, Valenti P, Boileau P (2018) Is reverse total shoulder arthroplasty more effective than hemiarthroplasty for treating displaced proximal humerus fractures in older adults? A systematic review and meta-analysis. Orthop Traumatol Res Surg 104(6):759–766
Gallinet D, Clappaz P, Garbuio P, Tropet Y, Obert L (2009) Three or four parts complex proximal humerus fractures: hemiarthroplasty versus reverse prosthesis: a comparative study of 40 cases. Orthop Traumatol Res Surg 95(1):48–55
Garrigues G, Johnston P, Pepe M, Tucker B, Ramsey M, Austin L (2012) Hemiarthroplasty versus reverse total shoulder arthroplasty for acute proximal humerus fractures in elderly patients. Orthopedics 35(5):e703–e708
Cuff D, Pupello D (2013) Comparison of hemiarthroplasty and reverse shoulder arthroplasty for the treatment of proximal humeral fractures in elderly patients. J Bone Joint Surg 95(22):2050–2055
Schumaier A, Grawe B (2018) Proximal humerus fractures: evaluation and management in the elderly patient. Geriatr Orthop Surg Rehabil 9:2151458517750516
Bufquin T, Hersan A, Hubert L, Massin P (2007) Reverse shoulder arthroplasty for the treatment of three-and four-part fractures of the proximal humerus in the elderly: a prospective review of 43 cases with a short-term follow-up. J Bone Joint Surg Br 89(4):516–520
Grammont P, Laffay J, Deries X (1987) Étude et réalisation d’une nouvelle prothèse d’épaule. Rhumatologie 239:407–418
Boudreau S, Boudreau E, Higgins LD, Wilcox B (2007) Rehabilitation following reverse total shoulder arthroplasty. J Orthop Sport Phys Ther 37(12):734–743
Gallinet D, Cazeneuve J-F, Boyer E, Menu G, Obert L, Ohl X et al (2019) Reverse shoulder arthroplasty for recent proximal humerus fractures: outcomes in 422 cases. Orthop Traumatol Res Surg 105(5):805–811
Cheung E, Sarkissian E, Sox-Harris A, Comer GC, Saleh J, Diaz R et al (2018) Instability after reverse total shoulder arthroplasty. J Shoulder Elb Surg 27(11):1946–1952
Villacis D, Sivasundaram L, Pannell W, Heckmann N, Omid R, George F (2016) Complication rate and implant survival for reverse shoulder arthroplasty versus total shoulder arthroplasty: results during the initial 2 years. J Shoulder Elb Surg 25(6):927–935
Wolff AL, Rosenzweig L (2017) Anatomical and biomechanical framework for shoulder arthroplasty rehabilitation. J Hand Ther 30(2):167–174
Alentorn-Geli E, Clark N, Assenmacher A, Samuelsen B, Sánchez-Sotelo J, Cofield R et al (2017) What are the complications, survival, and outcomes after revision to reverse shoulder arthroplasty in patients older than 80 years? Clinic Orthop Relat Res 475(11):2744–2751
Singh J, Ramachandran R (2015) Age-related differences in the use of total shoulder arthroplasty over time: use and outcomes. Bone Joint 97(10):1385–1389
Neer C (1970) Displaced proximal humeral fractures: part II. Treatment of three-part and four-part displacement. J Bone Joint Surg 52(6):1090–1103
Murachovsky J, Ikemoto RY, Nascimento LG, Fujiki EN, Milani C, Warner JJ (2006) Pectoralis major tendon reference (PMT): a new method for accurate restoration of humeral length with hemiarthroplasty for fracture. J Shoulder Elb Surg 15(6):675–678
Lascar T, Vidil A, Hery J-Y, Juvanspan M, Bellumore Y et al (2012) Dedicated anatomic prostheses for proximal humerus fracture. Technical solutions to improve tuberosity consolidation, with radiological and clinical analysis of results. Orthop Traumatol Surg Res 98:S68–S72
Boileau P, Winter M, Cikes A, Han Y, Carles M, Walch G et al (2013) Can surgeons predict what makes a good hemiarthroplasty for fracture? J Shoulder Elb Surg 22(11):1495–1506
Chelli M, Levy Y, Lavoué V, Clowez G, Gonzalez J-F, Boileau P (2019) The “Auto-Constant”: can we estimate the Constant-Murley score with a self-administered questionnaire? A pilot study. Orthop Traumatol Res Surg 105(2):251–256
Constant C, Murley A (1987) A clinical method of functional assessment of the shoulder. Clinic Orthop Relat Res 214:160–164
Hudak P, Amadio P, Bombardier C, Beaton D, Cole D, Davis A et al (1996) Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder, and head). Am J Ind Med 29(6):602–608
Sallay P, Reed L (2003) The measurement of normative American shoulder and elbow surgeons scores. J Shoulder Elb Surg 12(6):622–627
Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D (2004) Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff: results of a multicentre study of 80 shoulders. J Bone Joint Surg Br 86(3):388–395
Soleimanha M, Sedighinejad A, Haghighi M, Nabi B, Mirbolook A, Mardani-Kivi M (2014) Hemodynamic and arterial blood gas parameters during cemented hip hemiarthroplasty in elderly patients. Arch Bone Joint Surg 2(3):163
Boyer E, Menu G, Loisel F, Saadnia R, Uhring J, Adam A et al (2017) Cementless and locked prosthesis for the treatment of 3-part and 4-part proximal humerus fractures: prospective clinical evaluation of hemi-and reverse arthroplasty. Eur J Orthop Surg Traumatol 27(3):301–308
Cazeneuve J-F, Cristofari D-J (2011) Long term functional outcome following reverse shoulder arthroplasty in the elderly. Orthop Traumatol Res Surg 97(6):583–589
Ross M, Hope B, Stokes A, Peters S, McLeod I, Duke P (2015) Reverse shoulder arthroplasty for the treatment of three-part and four-part proximal humeral fractures in the elderly. J Shoulder Elb Surg 24(2):215–222
O’Sullivan J, Lädermann A, Parsons B, Werner B, Steinbeck J, Tokish J et al (2020) A systematic review of tuberosity healing and outcomes following reverse shoulder arthroplasty for fracture according to humeral inclination of the prosthesis. J Should Elbow Surg 29(9):1938–1949
Fortané T, Beaudouin E, Lateur G, Giraudo P, Kerschbaumer G, Boudhissa M et al (2020) Tuberosity healing in reverse shoulder arthroplasty in traumatology: use of an offset modular system with bone graft. Orthop Traumatol Res Surg 106(6):1113–1118
Fernández-Cortiñas A, Vidal CJ, Paredes-Carnero X, Marco MF (2019) Is the Charlson comorbidity index a good predictor of mortality and adverse effects in proximal humerus fractures? Orthop Traumatol Res Surg 105(2):301–315
Kulakli-Inceleme E, Tas D, Smeeing D, Houwert R, van Veelen N, Link B-C et al (2021) Tibiotalocalcaneal intramedullary nailing for unstable geriatric ankle fractures. Geriatr Orthop Surg Rehabil 12:21514593211020704
Hagen M, Allahabadi S, Zhang A, Feeley B, Grace T, Ma C (2020) A randomized single-blinded trial of early rehabilitation versus immobilization after reverse total shoulder arthroplasty. J Should Elbow Surg 29(3):442–450
Bullock G, Garrigues G, Ledbetter L, Kennedy J (2019) A systematic review of proposed rehabilitation guidelines following anatomic and reverse shoulder arthroplasty. J Orthop Sport Phys Ther 49(5):337–346
Blacknall J, Neumann L (2011) Rehabilitation following reverse total shoulder replacement. Shoulder Elb 3(4):232–240
van Essen T, Kornuijt A, de Vries L, Stokman R, van der Weegen W, Bogie R et al (2020) Fast track rehabilitation after reversed total shoulder arthroplasty: a protocol for an international multicentre prospective cohort study. BMJ Open 10(8):e034934
Cazeneuve J, Cristofari D-J (2010) The reverse shoulder prosthesis in the treatment of fractures of the proximal humerus in the elderly. J Bone Joint Surg Br 92(4):535–539
Garofalo R, Flanagin B, Castagna A, Lo E, Krishnan S (2015) Reverse shoulder arthroplasty for proximal humerus fracture using a dedicated stem: radiological outcomes at a minimum 2 years of follow-up—case series. J Orthop Surg Res 10(1):1–8
Denard P, Lädermann A (2016) Immediate versus delayed passive range of motion following total shoulder arthroplasty. J Should Elbow Surg 25(12):1918–1924
Choate W, Kwapisz A, Momaya A, Hawkins R, Tokish J (2018) Outcomes for subscapularis management techniques in shoulder arthroplasty: a systematic review. J Should Elbow Surg 27(2):363–370
Dolci A, Melis B, Verona M, Capone A, Marongiu G (2021) Complications and intraoperative fractures in reverse shoulder arthroplasty: a systematic review. Geriatr Orthop Surg Rehabil 12:21514593211059864
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Laurent Obert has no conflicts of interest in this work but has ties of interest with the following organizations: FX solutions, Medartis, Evolutis, Keri medical, Elsevier, Springer, CHU de Besancon, Université de Bourgogne Franche Comté. The authors declare that they have no competing interest.
Ethical approval
Local Ethics Committee approved the study and the French Data Protection.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tuphe, P., Caubriere, M., Hubert, L. et al. Early rehabilitation after reverse total shoulder prosthesis on fracture of proximal humerus in elderly patients provides better functional outcome. Eur J Orthop Surg Traumatol 33, 2951–2957 (2023). https://doi.org/10.1007/s00590-023-03505-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03505-1