Abstract
This article provides a summary of current information on rational postoperative use of the nasogastric tube, based on a review of literature related to postoperative gastrointestinal discomfort and management with the nasogastric tube. Routine gastric decompression after major surgery neither hastens the return of bowel function nor diminishes the incidence of postoperative nausea and vomiting. The multimodal postoperative rehabilitation programme is a modern and more efficient approach. Omission of nasogastric tube decompression does not increase the incidence of anastomotic leakage or wound dehiscence. Conversely, early enteral feeding is feasible and safe, favours local immunity and gut integrity, and improves nutritional status. With the objective to feeding, nasogastric tube could be used in selected patients. To conclude, use of the nasogastric tube to prevent or limit postoperative gastrointestinal discomfort must be challenged. In contrast to gastric decompression, early gastric feeding must be considered within the new concept of fast track surgery.
Similar content being viewed by others
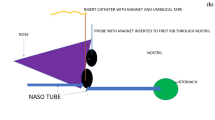
Introduction
Since the 1930s routine use of the nasogastric tube to achieve postoperative gastric decompression has enjoyed widespread acceptance, and for decades patients' complaints were not taken into consideration by anaesthesiologists and surgeons. This strong consensus was based on a traditionally held view, namely that postoperative ileus (POI) should be reduced by nasogastric decompression, although the different specialities had their own reasons to endorse this approach. Anaesthesiologists were mainly concerned with postoperative nausea and vomiting (PONV), whereas surgeons were concerned with preventing wound dehiscence, incisional hernia and anastomotic leakage. It is possible that we have forgotten that the history of the tube began as early as 1790, when it was used to feed and not to decompress, and we must reconsider the role of the nasogastric tube during the postoperative period.
Postoperative gastrointestinal discomfort
Postoperative gastrointestinal discomfort is not new. The earliest written records described an unchanging physiological response following any type of surgery, with greater severity after laparotomy. Clinically, there are three typical consequences of surgery, namely dilatation of the stomach, ileus and PONV.
Dilatation of the stomach is related to the common postoperative increase in swallowing [1]. Air carried into the stomach with each swallow induces gastric discomfort, and when present in great quantities the air passes into the intestine, resulting in abdominal distension. The greatest incidences were found in patients who had undergone surgery to the biliary tract or uterus and adnexa. In the majority of the cases, distension was apparent after 24 hours and the usual duration was 48 to 72 hours [2]. Decompression relieves gastric discomfort, but the irritating presence of the tube promotes swallowing. In any case, these physiological events must be distinguished from acute gastric dilatation and acute colonic pseudo-obstruction, which are responsible for major abdominal distension in very specific circumstances.
In reality, common postoperative gastrointestinal discomfort results predominantly from ileus, and nausea and vomiting. Wells and coworkers [3] stated that, 'After any abdominal operation it is usual for intestinal movements to cease for a time and then to return gradually. This POI usually lasts for up to 48 hours, its duration being related to the amount of intestinal handling at the operation. This period of inactivity of the intestine is presumed to be the response of the intestine to the various surgical manipulations. It is easily recognised clinically because the abdomen is silent when auscultated but is not induly distended.' This assertion, from 1964, has not been challenged since. It became dogma, with universal agreement that ileus should be countered by some form of gastrointestinal suctioning. All patients who underwent surgery of the gastrointestinal tract underwent placement of a nasogastric tube, with various criteria for removal such as normal bowel sounds heard by the surgeon or passage of flatus or stool. Its perceived importance in earlier years was well expressed by WJ Mayo: 'Would rather have a resident with a nasogastric tube in his pocket than a stethoscope.' In this context, gastric decompression was also recommended for the prevention of incisional hernia, wound dehiscence and anastomotic leak. This practice was extended to several other types of surgery, abdominal or otherwise, as secondary indications.
The medical impact of PONV is minor but it clearly is to the detriment of patient comfort. Surgical patients who experienced PONV were willing to pay up to US$100 for a completely effective antiemetic [4]. For the past 40 years, the incidence of PONV has remained constant, involving 20% to 30% of surgical patients. The incidence of nausea is nearly 20% in the postanaesthetic care unit and is over 50% after 24 hours, with corresponding numbers for vomiting being 5% and 25%, respectively. Nausea, retching and vomiting are often analyzed simultaneously and traditionally are related to delayed gastric emptying; however, they are distinct phenomena. In this context, nasogastric decompression was believed to be a logical alternative to prokinetic agents.
Routine nasogastric decompression: an inappropriate measure
Common postoperative ileus is basically a colonic phenomenon
Several animal models have been established to investigate mechanisms of ileus, and the descriptions are consistent [5–8]. Stomach emptying is impaired for about 24 hours after laparotomy. In contrast, the motility and the capacity of absorption of the small intestine is normal within a few hours after surgery. The small bowel, although mobile, contains little fluid or gas and therefore does not generate bowel sounds until the stomach resumes activity after 24 hours, pushing swallowed air and fluid into the gut. Any gas that reaches the small intestine is rapidly passed on into the caecum. However, the colon remains inert for a long time, with differences in times needed for return of activity in caecum (48 hours) and sigmoid colon (72 hours), with the passage of flatus or stool as a marker. Evidently, the profound change in colon motility is a major feature of the postoperative abdomen. It results from differences between the mobility of the ileum and the inertia of the rectosigmoid [9]. The autonomic nervous system undoubtedly plays an important role in POI, with perioperative stimuli inducing an increase in tonic inhibitory sympathetic control, as indicated by the inhibition of bowel function that occurs following surgery not involving the peritoneum. For instance, hip surgery is frequently associated with severe ileus [7].
Postoperative paralytic ileus is a consequence of local factors
Occasionally, ileus is prolonged for days or weeks and is described as postoperative paralytic ileus. The distinction between common POI and postoperative paralytic ileus is important because these phenomena probably result from different pathogenic mechanisms (Figure 1). Indeed, postoperative paralytic ileus affects all segments of the bowel and probably is the consequence of further inhibition of the local intrinsic contractile system. Resulting from bowel manipulation, hypoxia, endotoxin, or hypoperfusion, gut mucosal injury is the initial step inducing local release of nonadrenergic, non-cholinergic inhibitory neurotransmitters such as nitric oxide, vasoactive intestinal peptide, substance P, calcitonin gene-related peptide and prostanoids. Accordingly, a panel of responses may be observed, related to the duration and type of surgery and the degree of injury to the gut mucosa.
As a consequence, minimally invasive surgery could reduce the inflammatory response. In this regard, open and laparoscopic procedures have been compared. Most studies included benign gynaecological disorders or cholecystolithiasis, and a significantly more rapid resolution of ileus was reported with laparoscopic procedures. In a recent meta-analysis involving 6477 children undergoing appendicectomy [10], ileus was significantly reduced with laparoscopic compared with open procedures. However, these findings must be interpreted with caution because laparoscopic procedures are frequently viewed as benign by surgeons and patients, and perioperative management may be simplified as a consequence [11]. In a recent randomized trial [12], laparoscopic colectomy was associated with a shorter delay to first postoperative bowel movement but concurrently with decreased need for opioid analgesics at days 2 and 3. There is a lack of strong, unbiased evidence from human studies, which has stimulated interest in animal models. In a canine model, Davies and coworkers [13] compared three procedures: open colectomy, total laparoscopic and laparoscopically assisted colectomy. They demonstrated a significantly earlier return of gastrointestinal function with a total laparoscopic procedure, but these beneficial effects were not observed with laparoscopically assisted colectomy.
Few studies have investigated the gastrointestinal impact of strategies to protect gut blood flow. Gan and colleagues [14] compared two modes of intraoperative fluid administration in patients undergoing major elective general urological or gynaecological surgery. Continuous intraoperative Doppler-based estimation of ventricular preload to optimize fluid replacement allowed a 48-hour improvement in resolution of ileus.
Pain and opioids increase the duration of ileus. The major gastrointestinal impact of opioids is related to the μ2 receptors that are present in the presynaptic nerve terminals of the myenteric plexus. Both endogenous opioid peptides and exogenously administered opioid analgesics affect a variety of gastrointestinal functions associated with motility, secretion and visceral pain. Hence, achieving a balance between pain control and abdominal discomfort is a challenge in patients undergoing major surgery. Minimal use of opioid analgesics is recommended, and epidural infusion of a local anaesthetic has been advocated [15]. Epidural analgesia blocks pain transmission through afferent nerve fibres, reducing the need for postoperative opioids; it also inhibits the sympathetic efferent nerves in the thoracolumbar region, increasing gastrointestinal blood flow [16]. Furthermore, efferent parasympathetic tone in the sacral region remains unopposed, promoting gastrointestinal motility. Epidural infusion of local anaesthetics has proved to be more efficient than systemic or epidural opioid analgesia with regard to postoperative recovery of colonic function. Accordingly, a recent meta-analysis including a total of 406 patients [17] found a 44-hour reduction in time to first passage of stool in the group receiving local anaesthesia. Middle thoracic epidural blockade is more consistently effective than a low thoracic or lumbar level one [15]. Moreover, as a pain relief regimen, the combination of epidural local anaesthetic and opioid is not superior to local anaesthetic alone [18].
With the recent development of selective inhibition of gastrointestinal opioid receptors, a simple and appealing approach that is free from the technical demands of thoracic epidural infusion has emerged. Potent oral, peripherally acting antagonists of gastrointestinal opioid receptors are poorly absorbed following oral administration. In an exploratory trial, Taguchi and coworkers [19] found a significantly accelerated recovery of bowel function, without compromised control of analgesia, in patients who underwent partial colectomy or total abdominal hysterectomy. These data were partially confirmed by a recent phase III trial [20], but a number of questions were raised. The time to gastrointestinal recovery was significantly accelerated only for those patients who underwent bowel resection or radical hysterectomy. Furthermore, a clear dose response is not well established, and other studies are needed before widespread use under various postoperative circumstances can be advocated.
Incisional hernia, anastomotic leakage and wound dehiscence are not consequences of ileus
An estimated 10% to 15% of patients undergoing laparotomy incision eventually develop hernias [21]. Intuitively, elevated intra-abdominal pressure was suggested as a risk factor. On the other hand, important roles of surgical technique and biological environment have been demonstrated [22–24]. Abdominal fascial closure of midline laparotomy wounds with a continuous, nonabsorbable suture results in a significantly lower rate of incisional hernia (32% risk reduction) compared with use of either nonabsorbable or interrupted techniques. The impact of biological environment on healing is currently being investigated. Abdominal fascial closure of laparotomy wounds when adjacent to a continuous-release polygalactone polymer rod containing fibroblast growth factor results in a drastic reduction (90% versus 30%) in incisional hernias in animals [24].
Anastomotic leakage after visceral surgery is one of the most important and feared complications. The incidence is 3% to 12%, and it is responsible for 30% of deaths following colorectal surgery. As for incisional hernia, tension was believed to be a risk factor, but no link has been demonstrated and proximal decompression does not protect against anastomotic disruption but only ameliorates its consequences [25]. Reported aetiologic factors in anastomotic failure include male sex, obesity, previous radiotherapy, emergency procedure, low anastomosis, pelvic drainage and transfusion. New concepts in the field of gastrointestinal healing are currently being investigated. In a prospective study involving patients with colorectal anastomosis, the collagen I/III ratio and matrix metalloproteinase profiles of colonic tissues were significantly different between patients suffering anastomotic dehiscence and those with no complications [26]. These data suggest that disturbance in the extracellular matrix may play a role in the pathogenesis of anastomotic leakage.
Postoperative nausea and vomiting are consequences of individual factors
PONV and POI are distinct components of the pathophysiological response to surgery. Regrettably, these entities have been combined in studies conducted during recent decades.
It is still poorly understood why some patients vomit after surgery and others do not. However, it is well known that individual factors as older age, female sex, being a non-smoker, and history of PONV or motion sickness increase the likelihood of PONV. Moreover, exogenous factors such as omitting nitrous oxide, propofol administration, perioperative use of supplemental oxygen, good intravenous hydration, reduction in opioid use and neostigmine have been reported to decrease the incidence of PONV [27, 28]. The duration and type of surgery are other risk factors, but their impact is less marked. The individual risk factor approach has led to formulation of risk scores and made preventative approaches more efficient [29–32].
Impact of routine gastric decompression
Controversy concerning routine postoperative gastric suction emerged as early as 1960 [33]. The suggested beneficial effects were in opposition to the various complications of the nasogastric tube, some of which were even suspected of promoting ileus. The catalogue of possible complications is impressive but not as disturbing as the discomfort it causes to patients [34]. Most complications are related to nasopharyngeal insertion. Irritative rhinitis and pharyngitis are uncomfortable and distressing to the patient [35]. As mentioned above, the simple presence of a nasogastric tube causes significant changes in swallowing behaviour, with concomitant increase in gastric dilatation. A systematic review of 20 clinical studies focusing on routine gastric suction after elective laparotomy [36] demonstrated that routinely decompressed patients suffered more pulmonary complications. In a recent study [37] multivariate analysis revealed that perioperative use of a nasogastric tube was the major risk factor (odds ratio 7.7) for postoperative pulmonary complications.
In the absence of gastric decompression there is a moderate increase in vomiting. However, it is important to note that routine nasogastric decompression does not prevent vomiting in 10% of patients, and it does not preclude the need for tube replacement once it has been removed. In fact, for each patient not routinely decompressed who subsequently requires tube placement for nausea, vomiting, or abdominal distension, at least 20 patients can be managed without the tube [36]. A recent systematic review of prophylactic nasogastric decompression after abdominal operations [38] did not support a beneficial effect of the tube on various aspects of gastric upset during the postoperative period, but it identified more discomfort with routine use of the tube. However, the great heterogeneity of studies does not allow a summary statistic to be calculated. Hence, the hypothesis that gastric decompression during and after surgery will reduce the incidence of vomiting continues to be tested. In a recent study conducted in patients undergoing cardiac surgery with a high PONV score [39], perioperative use of the nasogastric tube did not influence the incidence of nausea, vomiting, or retching.
Nasogastric suction does not interfere with the mechanisms underlying ileus. In a recent meta-analysis [38], which included abdominal operations of any type, emergency or elective, prophylactic nasogastric decompression clearly did not hasten return of bowel function. On the contrary, a significantly earlier return of bowel function – as determined by the time to flatus – was observed without use of the tube.
Clearly, avoidance of nasogastric decompression following elective colorectal surgery does not affect the incidence of anastomotic leakage or incisional hernia. In a prospective study, Cunningham and coworkers [40] randomized 102 patients undergoing small or large bowel anastomosis to either routine nasogastric decompression or no tube. No significant differences in intestinal outcome were observed. Confirmation was recently provided by the meta-analysis conducted by Nelson and coworkers [38] in 2005. Similarly, omission of routine nasogastric decompression after colorectal surgery did not affect the incidence of incisional hernia in a clinical study with 5 years of follow up [41].
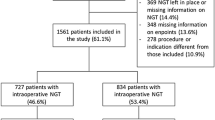
Finally, the two meta-analyses conducted during two distinct trial periods [36, 38] clearly indicated that prophylactic use of nasogastric decompression offers patients no benefit that would offset the discomfort and potential morbidity associated with its use (Figure 2). In all of the studies, at most 10% of patients who were not routinely decompressed required insertion of a nasogastric tube postoperatively. Thus, 90% of patients would have been needlessly decompressed if routine decompression had been used.
Feeding or gastric decompression
In contrast to gastric decompression, early feeding has a favourable effect on major outcomes [42–45]. Although there is a significantly higher incidence of gastric or abdominal distension, and nausea or vomiting, this is not associated with any untoward outcome [46]. However, feeding induces earlier resolution of ileus [47, 48]. Moreover, with early eating, the gastrointestinal tract gains advantages from saliva and gastrointestinal secretions, which possess a multiplicity of healing and antibacterial defence systems. The acidity of the stomach prevents colonization of Gram-negative bacilli and biliary secretions preserve balanced intestinal microflora. Enteral nutrition has proved to protect against postoperative sepsis by supporting mucosal immunity and to modulate the progression from gut ischaemia to systemic inflammatory response syndrome. Studies of animals exposed to brief episodes of mesenteric ischaemia and reperfusion have found that enteral feeding, as compared with parenteral nutrition, reduced mortality rate, abnormal gastric motility and organ permeability. Early oral nutrition reduces catabolism and loss of lean body mass, and enhances visceral blood supply to preserve the integrity of gut structure; hence, the fear of anastomotic dehiscence with early oral nutrition is not rational. In a systematic review of controlled trials, Lewis and coworkers [42] reported a trend toward a reduction in anastomotic dehiscence and wound infection with early feeding.
The standard postoperative nutritional intervention consists of a gradual reintroduction of an oral diet, as tolerated. This sometimes results in several days of insufficient nutrient intake and prolonged use of intravenous infusion. Many perioperative circumstances may widen the gap between requirements and intake. In a broad spectrum of surgical patients, there is no absolute gastrointestinal failure but the oral route is not an option. Typically, the problem emerges in surgical patients who require a few days to wean from mechanical ventilation. The nasogastric tube used intra-operatively is not removed in either the operating room or in the postanaesthesia care unit. In these common circumstances, it is judicious to switch gastric tube to feeding tube, preventing hasty introduction of parenteral nutrition. The nasogastric tube may be a convenient and flexible method to supply energy and pharmacologic treatments, and consequently to allow the withdrawal of central venous catheters. In most patients, careful and gradual increase in tube feeding is tolerated rather well. Specific modalities exist to optimize tolerance such as temporarily lowering or discontinuing the infusion (with selective measures of gastric residual volume, prokinetic agents and semirecumbent position). After a few days, comfort may be increased by a soft, small bore tube. Finally, in some biliary procedures, bile collected in a drainage bag can be infused with the diet in the stomach, inducing a decrease in inflammatory status. Much work challenges the generally held view that gastric delivery of nutriments will cause stimulation of biliary and pancreatic secretions, with adverse consequences when acute pancreatitis occurs or proximal anastomosis is present [49].
Fast track surgery: the physiological response to gastrointestinal discomfort
In recent years the approach to postoperative gastrointestinal dysfunction has improved substantially [50]. Basse and coworkers [51] demonstrated that actions that support faster return of gastrointestinal function can reverse or reduce complications after abdominal surgery. During the preoperative period, patients receive clear and comprehensive explanations of what may happen during their hospital stay. They are informed about pain and PONV control, surgical procedure, choice of incision, postoperative mobilization and food intake. Preoperative stressful experiences such as bowel preparation or fasting are avoided. The use of preoperative oral carbohydrate loading with free access to fluids until 2 hours before induction of anaesthesia is recommended.
Patients who are at high risk for PONV are identified during the preoperative period and receive prophylactic treatment. Avoidance of opioid is advocated, and epidural infusion of a local anaesthetic is favoured. Within the context of opioid-reduced analgesia, patients are encouraged to accept early oral fluids, ideally iso-osmolar or neutral, with the objective of limiting intravenous fluid administration and avoiding positive salt and water balance. Indeed, it has been reported that perioperative over-hydration significantly delays return of gastrointestinal function [52, 53]. Metabolic abnormalities such as hypokalaemia, hypomagnesaemia and hyponatraemia, which can induce ileus, are controlled. Early oral food intake and mobilization are promoted in fast track rehabilitation programmes. These concepts, which improve the cost-effectiveness of perioperative care in minor procedures, are logically expected to have large effects on care in major operations and in patients at high risk (Figure 2).
Postoperative nasogastric tube: a plea for judicious use
Not employing a routine nasogastric tube does not mean never using the tube. Some patients with intractable vomiting, mechanical occlusion, or specific upper surgery need placement of a nasogastric tube. In these cases, careful management is mandatory. The size, material and location of tips merit careful daily consideration. Semirecumbent position is optimal. When a gastric tube is used as a route for feeding or administration of medications, silicone rubber is appropriate to reduce patient discomfort.
Conclusion
As a consequence of the lack of studies dealing with the beneficial effects of prophylactic, routine nasogastric decompression, it is difficult to justify continued use of this procedure. We must turn over a new leaf. New approaches exist to reduce postoperative discomfort. Aimed at improving patient comfort, they induce earlier resolution of ileus. There is no justification for avoiding early attempts at enteral nutrition. On the contrary, with regard to modulation of the acute-phase response, enteral nutrition seems useful for resolution of ileus after major surgery. In some patients there is a need to switch the gastric tube to a feeding tube.
Abbreviations
- POI:
-
POI = postoperative ileus
- PONV:
-
PONV = postoperative nasea and vomiting.
References
French WE: Intra-abdominal surgery without gastrointestinal decompression. J Tenn Med Assoc 1966, 59: 767-768.
McIver MA, Benedict EB, Cline JW: Postoperative gaseous distention of the intestine. Arch Surg 1926, 13: 588-604.
Wells C, Tinckler L, Rawlinson K, Jones H, Saunders J: Postoperative gastrointestinal motility. Lancet 1964, 41: 4-10. 10.1016/S0140-6736(64)92156-7
Gan T, Sloan F, Dear Gde L, El-Moalem HE, Lubarsky DA: How much are patients willing to pay to avoid postoperative nausea and vomiting? Anesth Analg 2001, 92: 393-400. 10.1097/00000539-200102000-00022
Smith J, Kelly KA, Weinshilboum RM: Pathophysiology of postoperative ileus. Arch Surg 1977, 112: 203-209.
Woods JH, Erickson LW, Condon RE, Schulte WJ, Sillin LF: Postoperative ileus: a colonic problem? Surgery 1978, 84: 527-533.
Livingston EH, Passaro EP Jr: Postoperative ileus. Dig Dis Sci 1990, 35: 121-132. 10.1007/BF01537233
Hotokezaka M, Mentis EP, Patel SP, Combs MJ, Teates CD, Schirmer BD: Recovery of gastrointestinal tract motility and myoelectric activity change after abdominal surgery. Arch Surg 1997, 132: 410-417.
Resnick J, Greenwald DA, Brandt LJ: Delayed gastric emptying and postoperative ileus after nongastric abdominal surgery: part I. Am J Gastroenterol 1997, 92: 751-762.
Aziz O, Athanasiou T, Tekkis PP, Purkayastha S, Haddow J, Malinovski V, Paraskeva P, Darzi A: Laparoscopic versus open appendectomy in children: a meta-analysis. Ann Surg 2006, 243: 17-27. 10.1097/01.sla.0000193602.74417.14
Ortiz H, Armendariz P, Yarnoz C: Early postoperative feeding after elective colorectal surgery is not a benefit unique to laparoscopy-assisted procedures. Int J Colorectal Dis 1996, 11: 246-249. 10.1007/s003840050055
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Pahlman L, Cuesta MA, Msika S, et al.: Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 2005, 6: 477-484. 10.1016/S1470-2045(05)70221-7
Davies W, Kollmorgen CF, Tu QM, Donohue JH, Thompson GB, Nelson H, Sarr MG: Laparoscopic colectomy shortens postoperative ileus in a canine model. Surgery 1997, 121: 550-555. 10.1016/S0039-6060(97)90110-0
Gan TJ, Soppitt A, Maroof M, el-Moalem H, Robertson KM, Moretti E, Dwane P, Glass PS: Goal-directed intraoperative fluid administration reduces length of hospital stay after major surgery. Anesthesiology 2002, 97: 820-826. 10.1097/00000542-200210000-00012
Steinbrook RA: Epidural anesthesia and gastrointestinal motility. Anesth Analg 1998, 86: 837-844. 10.1097/00000539-199804000-00029
Schulz-Stubner S, Boezaart A, Hata JS: Regional analgesia in the critically ill. Crit Care Med 2005, 33: 1400-1407. 10.1097/01.CCM.0000165843.39713.AE
Jorgensen H, Wetterslev J, Moiniche S, Dahl JB: Epidural local anaesthetics versus opioid-based analgesic regimens on postoperative gastrointestinal paralysis, PONV and pain after abdominal surgery. Cochrane Database Syst Rev 2000, 4: CD001893.
Wu CL, Cohen SR, Richman JM, Rowlingson AJ, Courpas GE, Cheung K, Lin EE, Liu SS: Efficacy of postoperative patient-controlled and continuous infusion epidural analgesia versus intravenous patient-controlled analgesia with opioids: a meta-analysis. Anesthesiology 2005, 103: 1079-1088. quiz 1109–1010 10.1097/00000542-200511000-00023
Taguchi A, Sharma N, Saleem RM, Sessler DI, Carpenter RL, Seyedsadr M, Kurz A: Selective postoperative inhibition of gastrointestinal opioid receptors. N Engl J Med 2001, 345: 935-940. 10.1056/NEJMoa010564
Delaney CP, Weese JL, Hyman NH, Bauer J, Techner L, Gabriel K, Du W, Schmidt WK, Wallin BA: Phase III trial of alvimopan, a novel, peripherally acting, mu opioid antagonist, for postoperative ileus after major abdominal surgery. Dis Colon Rectum 2005, 48: 1114-1125. discussion 1125–1116; author reply 1127–1119 10.1007/s10350-005-0035-7
Kingsnorth A, LeBlanc K: Hernias: inguinal and incisional. Lancet 2003, 362: 1561-1571. 10.1016/S0140-6736(03)14746-0
Hodgson NC, Malthaner RA, Ostbye T: The search for an ideal method of abdominal fascial closure: a meta-analysis. Ann Surg 2000, 231: 436-442. 10.1097/00000658-200003000-00018
van 't Riet M, Steyerberg EW, Nellensteyn J, Bonjer HJ, Jeekel J: Meta-analysis of techniques for closure of midline abdominal incisions. Br J Surg 2002, 89: 1350-1356. 10.1046/j.1365-2168.2002.02258.x
Dubay DA, Wang X, Kuhn MA, Robson MC, Franz MG: The prevention of incisional hernia formation using a delayed-release polymer of basic fibroblast growth factor. Ann Surg 2004, 240: 179-186. 10.1097/01.sla.0000131576.12153.ab
Matthiessen P, Hallbook O, Andersson M, Rutegard J, Sjodahl R: Risk factors for anastomotic leakage after anterior resection of the rectum. Colorectal Dis 2004, 6: 462-469. 10.1111/j.1463-1318.2004.00657.x
Stumpf M, Klinge U, Wilms A, Zabrocki R, Rosch R, Junge K, Krones C, Schumpelick V: Changes of the extracellular matrix as a risk factor for anastomotic leakage after large bowel surgery. Surgery 2005, 137: 229-234. 10.1016/j.surg.2004.07.011
Greif R, Laciny S, Rapf B, Hickle RS, Sessler DI: Supplemental oxygen reduces the incidence of postoperative nausea and vomiting. Anesthesiology 1999, 91: 1246-1252. 10.1097/00000542-199911000-00014
Marret E, Kurdi O, Zufferey P, Bonnet F: Effects of nonsteroidal antiinflammatory drugs on patient-controlled analgesia morphine side effects: meta-analysis of randomized controlled trials. Anesthesiology 2005, 102: 1249-1260. 10.1097/00000542-200506000-00027
Apfel CC, Greim CA, Haubitz I, Goepfert C, Usadel J, Sefrin P, Roewer N: A risk score to predict the probability of postoperative vomiting in adults. Acta Anaesthesiol Scand 1998, 42: 495-501.
Apfel CC, Greim CA, Haubitz I, Grundt D, Goepfert C, Sefrin P, Roewer N: The discriminating power of a risk score for postoperative vomiting in adults undergoing various types of surgery. Acta Anaesthesiol Scand 1998, 42: 502-509.
Sinclair DR, Chung F, Mezei G: Can postoperative nausea and vomiting be predicted? Anesthesiology 1999, 91: 109-118. 10.1097/00000542-199907000-00018
Pierre S, Corno G, Benais H, Apfel CC: A risk score-dependent antiemetic approach effectively reduces postoperative nausea and vomiting – a continuous quality improvement initiative. Can J Anaesth 2004, 51: 320-325.
Gerber A: An appraisal of paralytic ileus and the necessity for postoperative gastrointestinal suction. Surg Gynecol Obstet 1963, 117: 294-296.
Hafner CD, Wylie JH Jr, Brush BE: Complications of gastrointestinal intubation. Arch Surg 1961, 83: 147-160.
Desmond P, Raman R, Idikula J: Effect of nasogastric tubes on the nose and maxillary sinus. Crit Care Med 1991, 19: 509-511. 10.1097/00003246-199104000-00009
Cheatham ML, Chapman WC, Key SP, Sawyers JL: A meta-analysis of selective versus routine nasogastric decompression after elective laparotomy. Ann Surg 1995, 221: 469-476. discussion 476–468 10.1097/00000658-199505000-00004
McAlister FA, Bertsch K, Man J, Bradley J, Jacka M: Incidence of and risk factors for pulmonary complications after nonthoracic surgery. Am J Respir Crit Care Med 2005, 171: 514-517. 10.1164/rccm.200408-1069OC
Nelson R, Tse B, Edwards S: Systematic review of prophylactic nasogastric decompression after abdominal operations. Br J Surg 2005, 92: 673-680. 10.1002/bjs.5090
Burlacu CL, Healy D, Buggy DJ, Twomey C, Veerasingam D, Tierney A, Moriarty DC: Continuous gastric decompression for postoperative nausea and vomiting after coronary revascularization surgery. Anesth Analg 2005, 100: 321-326. 10.1213/01.ANE.0000143567.51304.1A
Cunningham J, Temple WJ, Langevin JM, Kortbeek J: A prospective randomized trial of routine postoperative nasogastric decompression in patients with bowel anastomosis. Can J Surg 1992, 35: 629-632.
Otchy DP, Wolff BG, van Heerden JA, Ilstrup DM, Weaver AL, Winter LD: Does the avoidance of nasogastric decompression following elective abdominal colorectal surgery affect the incidence of incisional hernia? Results of a prospective, randomized trial. Dis Colon Rectum 1995, 38: 604-608. 10.1007/BF02054119
Lewis SJ, Egger M, Sylvester PA, Thomas S: Early enteral feeding versus 'nil by mouth' after gastrointestinal surgery: systematic review and meta-analysis of controlled trials. BMJ 2001, 323: 773-776. 10.1136/bmj.323.7316.773
Bozzetti F, Braga M, Gianotti L, Gavazzi C, Mariani L: Postoperative enteral versus parenteral nutrition in malnourished patients with gastrointestinal cancer: a randomised multicentre trial. Lancet 2001, 358: 1487-1492. 10.1016/S0140-6736(01)06578-3
Braga M, Gianotti L, Gentilini O, Parisi V, Salis C, Di Carlo V: Early postoperative enteral nutrition improves gut oxygenation and reduces costs compared with total parenteral nutrition. Crit Care Med 2001, 29: 242-248. 10.1097/00003246-200102000-00003
Marik PE, Zaloga GP: Early enteral nutrition in acutely ill patients: a systematic review. Crit Care Med 2001, 29: 2264-2270. 10.1097/00003246-200112000-00005
Schilder JM, Hurteau JA, Look KY, Moore DH, Raff G, Stehman FB, Sutton GP: A prospective controlled trial of early postoperative oral intake following major abdominal gynecologic surgery. Gynecol Oncol 1997, 67: 235-240. 10.1006/gyno.1997.4860
Cutillo G, Maneschi F, Franchi M, Giannice R, Scambia G, Benedetti-Panici P: Early feeding compared with nasogastric decompression after major oncologic gynecologic surgery: a randomized study. Obstet Gynecol 1999, 93: 41-45. 10.1016/S0029-7844(98)00401-3
Kaur N, Gupta MK, Minocha VR: Early enteral feeding by nasoenteric tubes in patients with perforation peritonitis. World J Surg 2005, 29: 1023-1027. discussion 1027–1028 10.1007/s00268-005-7491-z
Eatock FC, Chong P, Menezes N, Murray L, McKay CJ, Carter CR, Imrie CW: A randomized study of early nasogastric versus nasojejunal feeding in severe acute pancreatitis. Am J Gastroenterol 2005, 100: 432-439. 10.1111/j.1572-0241.2005.40587.x
Kehlet H, Wilmore DW: Fast-track surgery. Br J Surg 2005, 92: 3-4. 10.1002/bjs.4841
Basse L, Raskov HH, Hjort Jakobsen D, Sonne E, Billesbolle P, Hendel HW, Rosenberg J, Kehlet H: Accelerated postoperative recovery programme after colonic resection improves physical performance, pulmonary function and body composition. Br J Surg 2002, 89: 446-453. 10.1046/j.0007-1323.2001.02044.x
Lobo DN, Bostock KA, Neal KR, Perkins AC, Rowlands BJ, Allison SP: Effect of salt and water balance on recovery of gastrointestinal function after elective colonic resection: a randomised controlled trial. Lancet 2002, 359: 1812-1818. 10.1016/S0140-6736(02)08711-1
Nisanevich V, Felsenstein I, Almogy G, Weissman C, Einav S, Matot I: Effect of intraoperative fluid management on outcome after intraabdominal surgery. Anesthesiology 2005, 103: 25-32. 10.1097/00000542-200507000-00008
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
About this article
Cite this article
Tanguy, M., Seguin, P. & Mallédant, Y. Bench-to-bedside review: Routine postoperative use of the nasogastric tube – utility or futility?. Crit Care 11, 201 (2007). https://doi.org/10.1186/cc5118
Published:
DOI: https://doi.org/10.1186/cc5118