Abstract
Introduction
The objective was to study the effects of a novel lung volume optimization procedure (LVOP) using high-frequency oscillatory ventilation (HFOV) upon gas exchange, the transpulmonary pressure (TPP), and hemodynamics in a porcine model of surfactant depletion.
Methods
With institutional review board approval, the hemodynamics, blood gas analysis, TPP, and pulmonary shunt fraction were obtained in six anesthetized pigs before and after saline lung lavage. Measurements were acquired during pressure-controlled ventilation (PCV) prior to and after lung damage, and during a LVOP with HFOV. The LVOP comprised a recruitment maneuver with a continuous distending pressure (CDP) of 45 mbar for 2.5 minutes, and a stepwise decrease of the CDP (5 mbar every 5 minute) from 45 to 20 mbar. The TPP level was identified during the decrease in CDP, which assured a change of the PaO2/FIO2 ratio < 25% compared with maximum lung recruitment at CDP of 45 mbar (CDP45). Data are presented as the median (25th–75th percentile); differences between measurements are determined by Friedman repeated-measures analysis on ranks and multiple comparisons (Tukey's test). The level of significance was set at P < 0.05.
Results
The PaO2/FiO2 ratio increased from 99.1 (56.2–128) Torr at PCV post-lavage to 621 (619.4–660.3) Torr at CDP45 (CDP45) (P < 0.031). The pulmonary shunt fraction decreased from 51.8% (49–55%) at PCV post-lavage to 1.03% (0.4–3%) at CDP45 (P < 0.05). The cardiac output and stroke volume decreased at CDP45 (P < 0.05) compared with PCV, whereas the heart rate, mean arterial pressure, and intrathoracic blood volume remained unchanged. A TPP of 25.5 (17–32) mbar was required to preserve a difference in PaO2/FIO2 ratio < 25% related to CDP45; this TPP was achieved at a CDP of 35 (25–40) mbar.
Conclusion
This HFOV protocol is easy to perform, and allows a fast determination of an adequate TPP level that preserves oxygenation. Systemic hemodynamics, as a measure of safety, showed no relevant deterioration throughout the procedure.
Similar content being viewed by others
Introduction
Current ventilatory strategies for 'lung-protective' ventilation in acute respiratory distress syndrome (ARDS) include low tidal volumes to avoid alveolar overdistension, adequate end-expiratory lung volume by positive end-expiratory pressure to prevent end-expiratory alveolar collapse, and inspiratory pressure limitation to minimize further stress and strain to the lung fibrous skeleton [1]. The excessive and nonphysiological strain to lung structures is caused by high transpulmonary pressures (TPP), which in turn depend on the respiratory system elastance [2]. High-frequency oscillatory ventilation (HFOV) offers several advantages over conventional ventilation. Oscillations in HFOV are superimposed on a constant fresh gas flow and induce active inspiratory and expiratory gas movement, resulting in high constant mean airway pressures at low tidal volumes. Atelectatic lung regions are reopened by the continuous distending airway pressure (CDP), and the superimposed small oscillations provide alveolar gas exchange for CO2 removal [3]. Recruitment maneuvers are beneficial at initiation of HFOV to ensure sufficient gas exchange area in the diseased lung [4].
In most clinical studies, HFOV is initiated by an initial lung volume optimization procedure (LVOP) with a CDP level 5 mbar above the effective mean airway pressure previously used at conventional ventilation [5–8]. The CDP is thereafter increased in a stepwise manner (2–5 mbar every 15–30 minutes) up to the maximum increase of PaO2 or up to a predetermined CDP. This maneuver is followed by a stepwise reduction of the CDP (2 mbar every 30 minutes up to 4 hours) to maintain alveolar patency. Recruitment in a stepwise fashion is effective and safe with regard to hemodynamic impairment, but is also time consuming in adjusting an effective CDP.
Preclinical and clinical trials have been presented recently that used a recruitment maneuver with a high CDP, followed by a stepwise decrease of the airway pressure. Sedeek and colleagues used a continuous positive airway pressure of 50 mbar for lung recruitment in lung-lavaged sheep. The CDP was then set according to the maximal compliance on the pressure-volume [9]. The Treatment with Oscillation and an Open Lung Strategy (TOOLS) trial used a standardized HFOV protocol in patients, which showed that the combination of HFOV and a high initial recruitment maneuver (with interrupted HFOV) resulted in a rapid and sustained improvement in oxygenation. The mean airway pressure was then titrated in a decremental fashion according to the oxygenation response [10].
In the present study we investigated the immediate effect of a modified LVOP by means of ongoing HFOV on hemodynamics and oxygenation prior to its clinical application. To demonstrate the feasibility and safety of this lung optimization procedure, HFOV was initiated with the CDP set to 45 mbar (for 2.5 minutes) during ongoing oscillation in six pigs after saline lung lavage, simulating an early-phase ARDS model. The CDP was thereafter reduced in a stepwise fashion of five mbar every five minutes with simultaneous measurement of the TPP. The effects upon gas exchange, systemic hemodynamics, and the pulmonary shunt proportion were observed at each CDP and TPP level.
Methods
Animal preparation
The study protocol was approved by the institutional and state animal care committee. Six pigs were anesthetized after premedication (8 mg/kg azaperone and 0.02 mg/kg atropine intramuscularly) with 0.01 mg/kg fentanyl (Fentanyl; Janssen Pharmaceuticals, Neuss, Germany) and 5 mg/kg thiopentone (Trapanal; Altana Pharma, Konstanz, Germany) intravenously. Anesthesia was maintained by continuous infusion of thiopentone (6–9 mg/kg/hour) and fentanyl (5 μg/kg/hour). The trachea was intubated by tracheotomy (endotracheal tube, ID 9 mm; Ruesch, Kernen, Germany) and the pigs were ventilated in a pressure-controlled mode (PCV) with a FiO2 of 0.3 in air, a positive end-expiratory pressure of 5 mbar, and a variable respiratory rate to achieve an end-tidal carbon dioxide tension of 40 ± 5 Torr (Servo 900 C; Siemens, Erlangen, Germany). Ringer's solution was substituted continuously at a rate of 5 ml/kg/hour intravenously.
Instrumentation included arterial and central venous catheterization by femoral cutdown for blood pressure monitoring (S/5 Monitoring; Datex-Ohmeda, Duisburg, Germany), blood gas analysis, and drug administration. A pulmonary arterial catheter was introduced via the right internal jugular vein for mixed venous blood gas sampling (Radiometer 500 and OSM 3; Radiometer, Copenhagen, Denmark). A left ventricular catheter was introduced through the right internal carotid artery for measurement of the left ventricular end-diastolic pressure (LVEDP). The position of all catheters was verified by transduction of typical pressure waveforms and was verified by autopsy after the experiment. All intravascular pressures were referenced to the mid-chest level. For measurement of the esophageal pressure, a catheter with an inflatable balloon on its tip (Oesophagus Catheter; Jaeger GmbH, Hoechberg, Germany) was placed in the distal esophagus and filled with 1 ml air [11]. A pneumotachymeter (Pneumotachymeter; Jaeger-Toennies, Hoechberg, Germany) was attached to the endotracheal tube. The airway and esophageal pressures were recorded and analyzed with a dedicated monitoring system (MasterScreenIOS; Jaeger-Toennies). After finishing the study protocol, the animals were euthanized (40 mval potassium chloride intravenously) in deep anesthesia.
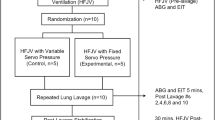
Lung lavage model
A surfactant-depletion model was induced by repetitive lung lavages (4 ± 1) until a PaO2/FiO2 ratio less than 100 Torr was achieved. Isotonic Ringer's solution (20 ml/kg, 38°C) was instilled into the endotracheal tube, and the fluid was retrieved by gravity drainage after 30 seconds of apnoea. To maintain hemodynamic stability, a continuous infusion (mean ± standard deviation) of 3 ± 2 μg/kg/hour epinephrine was administered during the lung lavages and was kept constant during the entire study protocol. After lung lavages, the animals were ventilated with a positive end-expiratory pressure of 5 mbar during PCV (inspiratory pressure = 25 mbar, FiO2 = 1.0, inspiration time:expiration time ratio = 1:1) for 120 minutes prior to initiation of HFOV.
High-frequency oscillatory ventilation
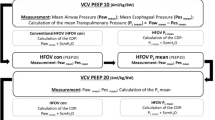
A commercially available HFOV oscillator (Sensormedics 3100 B; Yorba Linda, California, USA) was used. Hemodynamic stability before HFOV initiation was defined by a mean arterial pressure (MAP) > 60 mmHg and a pulmonary artery occlusion pressure (PAOP) > 10 mmHg. If the PAOP was inadequate, repetitive boluses of 5 ml/kg colloids within 10 minutes were applied until hemodynamic stability was achieved. The following HFOV settings were used and kept constant throughout the entire protocol (Figure 1): FiO2 of 1.0, an oscillatory frequency of 6 Hz, an inspiration time of 33% of the respiratory cycle, a bias flow of 30 l/minute, and a pressure amplitude of 40 mbar.
The protocol for lung volume optimization during HFOV comprised three steps: step 1, a lung recruitment maneuver – setting the initial CDP during ongoing oscillations to 45 mbar (CDP45) for 2.5 minutes; step 2, decrease of the CDP – the CDP was reduced in a stepwise manner by 5 mbar every 5 minutes from 45 mbar to 40 mbar, 35 mbar, 30 mbar, 25 mbar, and 20 mbar (CDP20) with simultaneous measurement of the TPP; and step 3, identification of the optimal TPP – the TPP level necessary to maintain lung recruitment was defined as the TPP necessary to prevent a decrease in the PaO2/FiO2 ratio > 25% compared with the PaO2/FiO2 ratio at CDP45 (that is to say, maximum lung recruitment).
Measurements
The following parameters were recorded before and 120 minutes after initiation of lung damage during PCV, and at every CDP level during HFOV: the heart rate, the MAP, the right atrial pressure, the PAOP, the mean pulmonary artery pressure, and the LVEDP. In addition, the intrathoracic blood volume, the extravascular lung water, and the cardiac output (CO), as obtained by the PiCCO®-Technology system (Pulsion Medical Systems, Munich, Germany), were recorded. For blood gas analyses, arterial and mixed venous blood samples were drawn (ABL 500/OSM 3; Radiometer, Copenhagen, Denmark). The pulmonary vascular resistance, the systemic arterial vascular resistance, the stroke volume (SV), oxygen delivery, the oxygenation index, and the pulmonary shunt proportion were calculated according to standard formula.
The TPP was calculated as the difference between the CDP (measured at the proximal end of endotracheal tube) and the esophageal pressure.
Statistical analysis
Data are expressed as the median, and 25th and 75th percentiles (interquartile range). Intraindividual differences before and after induction of lung injury and during the recruitment maneuver (PCV post-lavage and CDP45) were tested nonparametrically using the Wilcoxon signed-rank test. Any differences during the fast CDP deceleration trial were addressed by a Friedman repeated-measures analysis of variance on ranks and multiple comparisons by Tukey's test. P < 0.05 was considered significant (SigmaStat Version 2.03; SPSS Inc., San Raphael, California, USA).
Results
All six animals (25 ± 2 kg bodyweight, mean ± standard deviation) completed the entire study protocol. Hemodynamic and gas exchange variables before and after induction of lung damage are presented in Table 1. The MAP and PAOP before initiation of HFOV complied with the predefined requirements; that is, PAOP of 13 (11–13) mmHg and MAP of 83 (82–85) mmHg. Repetitive lung lavages decreased the PaO2/FiO2 ratio (PCV pre-lavage, 559 (535–658) Torr vs PCV post-lavage, 99 (56–128) Torr; P < 0.05), and increased the pulmonary shunt fraction (PCV pre-lavage, 9.97% (8.8–11%) vs PCV post-lavage, 51.8% (49–55%); P < 0.05). The oxygenation index increased from PCV pre-lavage (1.4 (1.2–2)) to PCV post-lavage (16.3 (14.6–21.3)) (P < 0.05). The extravascular lung water increased from PCV pre-lavage (290 (241–311) ml) to PCV post-lavage (420 (354–463) ml) (P < 0.05).
Hemodynamics
Hemodynamic variables are presented in Table 1 for the lung recruitment maneuver and in Table 2 for the stepwise decrease of the CDP. The MAP, heart rate and intrathoracic blood volume did not change throughout the entire experiment. The right atrial pressure, mean pulmonary artery pressure, PAOP, and LVEDP during the lung recruitment procedure increased significantly from the PCV post-lavage to CDP45 (P < 0.05). The CO and SV decreased from PCV post-lavage (CO, 3.6 (3.1–3.9) l/minute; SV, 32 (31–35) ml) to CDP45 (CO, 2.6 (2.3–3.1) l/minute; SV, 19 (18–24) ml) (P = 0.031).
Pulmonary gas exchange and pulmonary shunt fraction
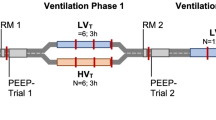
The LVOP increased the PaO2/FiO2 ratio from PCV post-lavage (99 (56–128) Torr) to CDP45 (621 (619–660) Torr) (P < 0.05). The pulmonary shunt fraction decreased from PCV post-lavage (51.8% (49–55%)) to CDP45 (1.03% (0.4–3%)) (P < 0.05). During the stepwise decrease of the CDP, the shunt fraction increased to 20.2% (7.2–52%) at CDP20 compared with 1.03% (0.4–1.4%) at CDP45 and compared with 0.7% (0.1–1.4%) at CDP of 40 mbar (P < 0.05). The PaO2/FiO2 ratio decreased from CDP45 (621 (619–660) Torr) to CDP20 (429 (52–558) Torr) (P < 0.05) (Figure 2). The PaCO2 increased from CDP45 (38.5 (28.3–46) Torr) to CDP20 (54.4 (40.7–68.6) Torr) (P < 0.001).
PaO2/FiO2 ratio and shunt fraction during pressure-controlled ventilation and high-frequency oscillatory ventilation. The PaO2/FiO2 ratio and shunt fraction during pressure-controlled ventilation (PCV) pre-lavage and PCV post-lavage in relation to continuous distending pressure (mbar). CDP, continuous distending pressure.
Identification of the required TPP level
The lung optimization procedure in this study required less than 30 minutes to recruit the lung and to identify the lowest TPP level to maintain adequate oxygenation and gas exchange. The TPP increased from PCV post-lavage (10 (8–11) mbar) to CDP45 (36 (26–43) mbar) (P < 0.05).
A TPP between 32 and 14 mbar prevented a decrease in the PaO2/FiO2 ratio > 25% compared with the PaO2/FiO2 ratio at CDP45. These TPP levels were achieved at CDP settings ranging from 25 to 40 mbar (Figure 3a). In three animals the PaO2/FiO2 ratio did not decrease more than 25% compared with the measurement at CDP45, independently of the applied CDP (Figure 3b). On average, a TPP of 25.5 (17–32) mbar was required to preserve a difference in the PaO2/FiO2 ratio < 25% related to CDP45; this TPP was achieved at a CDP of 35 (25–40) mbar.
Relationship between continuous distending pressure and transpulmonary pressure or changes in PaO2/FiO2 ratio. Relationship (for each animal) between the continuous distending pressure (CDP) (mbar) and: (a) the transpulmonary pressure (TPP) (mbar) (X, shunt fraction > 10%; +, decrease of the PaO2/FiO2 ratio > 25%), and (b) changes in the PaO2/FiO2 ratio (%) (dotted line, decrease of the PaO2/FiO2 ratio of 25% compared with CDP of 45 mbar (CDP45); X, shunt fraction > 10%).
Discussion
The present experimental study investigated the effects upon gas exchange, TPPs, and hemodynamics of a modified HFOV initiation protocol to optimize the lung volume in a porcine model of acute lung injury. The protocol consists of a fast recruitment maneuver followed by a stepwise decrease of CDP. The fast stepwise reduction of CDP allows the identification of the lowest TPP level required to maintain improvement of oxygenation in each animal. This approach therefore offers an effective reduction of pulmonary shunt fraction and improvement in oxygenation without relevant adverse hemodynamic effects within a very short time.
In most clinical and experimental studies, HFOV is initiated with a LVOP with an initial CDP level 5 mbar above the mean airway pressure previously used in conventional ventilation [5, 6, 8, 12]. The CDP is then increased in a stepwise fashion (2–5 mbar steps) every 15–30 minutes until a maximum in PaO2 or a predetermined CDP is reached. Our study presents a fast lung optimization procedure that could be technically applied easily in the clinical scenario. In contrast to recent studies in animals and in patients, the CDP was directly set to 45 mbar for 2.5 minutes. The lowest possible TPP that still assures the improved oxygenation is subsequently titrated.
Recruitment maneuvers are beneficial at the initiation of HFOV to ensure sufficient gas exchange area in the diseased lung [4]. In the Treatment with Oscillation and an Open Lung Strategy trial, the combination of HFOV and a high initial mean airway pressure recruitment maneuver without ongoing HFOV resulted in a rapid and sustained improvement in oxygenation [10]. Although sustained inflation pressures up to 55 mbar are necessary to overcome the opening pressure of collapsed alveoli [13], the criteria of a fully recruited lung, defined as pulmonary shunt proportion < 0.1 [14], was achieved at a CDP of 45 mbar. A CDP of 32 ± 6 mbar in piglets was able to reduce the shunt fraction < 10% [15]. During the present study a single pressure step-up for alveolar recruitment was performed, and therefore no estimate can be made of whether a lower CDP and TPP would have been adequate to reopen the lung, and whether the TPP required to open alveolar units exceeds the TPP required to maintain alveolar patency [15, 16]. Assuming that the TPP stays above a critical closing pressure, a significant alveolar derecruitment cannot be expected [17, 18]. In other experimental studies with the lavage-injury animal model, the mean airway pressures were set according to the pressure-volume curve for the setting of the CDP during HFOV [9, 16, 19]. In their study, Sedeek and colleagues repeated recruitment maneuvers with a continuous positive airway pressure of 50 mbar for 1 minute until the PaO2 was stable with a CDP set according to the maximal compliance on the pressure-volume curve [9].
We intended to use an alternative method without the pressure-volume curve. The PaO2/FiO2 ratio was therefore used as a criterion to identify the lowest TPP preventing alveolar derecruitment during the stepwise decrease of CDP. A TPP below this threshold was associated with an increased shunt > 10 and with an increased PaCO2. An increased PaCO2 at unchanged HFOV settings indicates a decreased alveolar surface available for gas exchange.
Previous studies in the lavage animal model showed that CO decreased at high mean airway pressures. Interestingly, better oxygenation values in those studies were found at lower mean airway pressure, suggesting in our study that eventually a lower CDP eventually would have been sufficient [16, 19]. The lung recruitment maneuver had a marked effect on hemodynamics. These effects can easily be corrected by volume or by vasoactive drug usage. There was no relevant decrease of the intrathoracic blood volume as an indicator of reduced venous preload [20]. Also, the fluid regime before initiation of HFOV may have attenuated a reduction of venous return.
At a CDP of 45 mbar, the SV and CO were decreased and, simultaneously, the cardiac filling pressures (LVEDP, right atrial pressure, and PAOP) were elevated. This can be explained by a compression of the heart into the cardiac fossa due to the transmission of high TPPs [21, 22]. Impairment of hemodynamics can therefore be explained by the mechanical restriction of the heart. Systemic afterload did not have a major impact on the impaired SV and CO as measured by the systemic vascular resistance. Right ventricular dysfunction may occur when high airway pressures are applied, and the consecutive right ventricular output and left ventricular filling are impaired leading to SV and CO decreases. As the pulmonary vascular resistance was unaffected by a CDP of 45 mbar and the right ventricle was able to generate a pressure gradient (mean pulmonary artery pressure–right atrial pressure), we excluded right ventricular failure. During the deceleration CDP trial, the cardiac filling pressures returned to similar values as measured before the lung recruitment maneuver. This observation assures us that the hemodynamic effects are related to a pressure transmission of the CDP and the TPP.
The safe window for plateau pressures during conventional ventilation is considered between 30 and 35 mbar, but even those values can lead to a harmful TPP. Depending on the elastance of the respiratory system, volutrauma may occur from cyclic tidal overdistension. No recommendations regarding safe levels for CDP or TPP exist during HFOV. The lowest TPP levels possible, however, should be applied. The measurement and monitoring of the TPP is therefore helpful and of increased interest, as the TPP is the effective distending force of the lung, and ventilator-induced lung injury (VILI) depends on the TPP [23, 24]. By measuring the TPP the mechanical ventilator settings could be set more individually with respect to lung and chest wall mechanical characteristics, which enables the identification of lung recruitment potential in relation to a potential risk of VILI. Such an individual approach may reduce the risk for further lung injury in patients with ARDS undergoing mechanical ventilation [25, 26]. In a clinical scenario, a CDP higher than the safe window for plateau pressures under conventional ventilation should be avoided even if suggested by the LVOP presented in this study. Although the theoretical advantage of HFOV is the avoidance of volutrauma caused by tidal overdistension (due to minimal tidal volumes) in the case of excessive TPP, a compromise between oxygenation and potential VILI should be made to avoid a VILI and to accept lower but adequate oxygenation.
The esophageal pressure measured by an esophageal balloon is used as a surrogate parameter of the pleural pressure for calculation of the TPP. The pleural pressure and therefore the TPP are dependent on the chest wall elastance in experimental patients and ARDS patients. For a given mean airway pressure (CDP) the pleural pressure increases if the chest wall elastance is elevated, and consequently the TPP decreases. Chest wall elastance, however, depends on the pathophysiology of ARDS (for example, high chest wall elastance in extrapulmonary ARDS). The elevated pleural pressure (due to increased chest wall elastance) leads to a lower TPP compared with pulmonary ARDS with normal elastance [1, 27–29].
We found a pressure difference of about 10 mbar between the applied CDP and the resulting TPP. The difference in mean intrathoracic pressure and CDP in HFOV increases with the oscillatory frequency, decreasing the tracheal tube diameter and the relative duration of the inspiratory time [30]. The inspiration time:expiration time ratio of 33% in our study results in an increased tracheal tube resistance and, consequently, in a decreased mean intrathoracic pressure and TTP.
Limitations
A major limitation of this study is that it was performed in a lavage animal model of ARDS and not in patients. Large-animal models, however, have contributed greatly to the understanding of the basic physiology of HFOV and its clinical application during severe lung injury [31]. ARDS in patients is rarely and solely a result of surfactant deficiency only. Early institution of HFOV, however, and institution of HFOV in patients with high potential for recruitment is theoretically beneficial to outcome in ARDS [32–34]. The lavage model is easily recruitable and is probably the most comparable experimental ARDS model for early-phase ARDS. Although it is primarily a model of surfactant depletion, it has been shown that mechanical ventilation after lavages leads to neutrophil infiltration, cytokine expression, and capillary-alveolar protein leak (as indicated by the increased extravascular lung water in this study) [35–37]. The present study only observed immediate changes of hemodynamics and lung oxygenation. High airway pressures and subsequent lung overdistension may lead to mediator release and to VILI. These adverse events were not accessible in the present study. Also, we cannot report whether the optimized gas exchange remained stable over a longer time period. This raises the question of how often such recruitment maneuvers should be applied in clinical practice.
Conclusion
This short-term experimental observation study demonstrates the feasibility of a fast and safe lung optimization procedure during uninterrupted HFOV. This lung optimization procedure was well tolerated and resulted in a dramatic improvement of oxygenation. No clinically relevant adverse effects on hemodynamics or barotrauma occurred during the time period of approximately 1 hour. The stepwise decrease of CDP allowed the determination of the lowest TPP level necessary to maintain adequate oxygenation.
Key messages
-
A novel lung optimization procedure in uninterrupted HFOV is presented.
-
The LVOP consists of a single CDP recruitment maneuver during uninterrupted HFOV, followed by a stepwise decrease of the CDP.
-
This LVOP allows the determination of the lowest TPP that still maintains adequate pulmonary gas exchange.
-
This LVOP shows no adverse effects in hemodynamics and oxygenation during its intervention in a porcine lavage ARDS model.
Abbreviations
- ARDS:
-
ARDS = acute respiratory distress syndrome
- CDP:
-
CDP = continuous distending pressure
- CDP20:
-
CDP20 = continuous distending pressure of 20 mbar
- CDP45:
-
CDP45 = continuous distending pressure of 45 mbar
- CO:
-
CO = cardiac output
- FiO:
-
FiO2 = fraction of inspired oxygen
- HFOV:
-
HFOV = high-frequency oscillatory ventilation
- LVEDP:
-
LVEDP = left ventricular end-diastolic pressure
- LVOP:
-
LVOP = lung volume optimization procedure
- MAP:
-
MAP = mean arterial pressure
- PaCO:
-
PaCO2 = arterial partial pressure of carbon dioxide
- PaO:
-
PaO2 = arterial partial pressure of oxygen
- PAOP:
-
PAOP = pulmonary occlusion pressure
- PCV:
-
PCV = pressure-controlled ventilation
- SV:
-
SV = stroke volume
- TPP:
-
TPP = transpulmonary pressure
- VILI:
-
VILI = ventilator-induced lung injury.
References
Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network N Engl J Med 2000, 342: 1301-1308. 10.1056/NEJM200005043421801
Gattinoni L, Carlesso E, Cadringher P, Valenza F, Vagginelli F, Chiumello D: Physical and biological triggers of ventilator-induced lung injury and its prevention. Eur Respir J Suppl 2003, 47: 15s-25s. 10.1183/09031936.03.00021303
Imai Y, Nakagawa S, Ito Y, Kawano T, Slutsky AS, Miyasaka K: Comparison of lung protection strategies using conventional and high-frequency oscillatory ventilation. J Appl Physiol 2001, 91: 1836-1844.
Froese AB: The incremental application of lung-protective high-frequency oscillatory ventilation. Am J Respir Crit Care Med 2002, 166: 786-787. 10.1164/rccm.2206005
Derdak S, Mehta S, Stewart TE, Smith T, Rogers M, Buchman TG, Carlin B, Lowson S, Granton J: High-frequency oscillatory ventilation for acute respiratory distress syndrome in adults: a randomized, controlled trial. Am J Respir Crit Care Med 2002, 166: 801-808. 10.1164/rccm.2108052
Derdak S: High-frequency oscillatory ventilation for acute respiratory distress syndrome in adult patients. Crit Care Med 2003, 31: S317-S323. 10.1097/01.CCM.0000057910.50618.EB
David M, Karmrodt J, Weiler N, Scholz A, Markstaller K, Eberle B: High-frequency oscillatory ventilation in adults with traumatic brain injury and acute respiratory distress syndrome. Acta Anaesthesiol Scand 2005, 49: 209-214. 10.1111/j.1399-6576.2004.00570.x
David M, Weiler N, Heinrichs W, Neumann M, Joost T, Markstaller K, Eberle B: High-frequency oscillatory ventilation in adult acute respiratory distress syndrome. Intensive Care Med 2003, 29: 1656-1665. 10.1007/s00134-003-1897-6
Sedeek KA, Takeuchi M, Suchodolski K, Vargas SO, Shimaoka M, Schnitzer JJ, Kacmarek RM: Open-lung protective ventilation with pressure control ventilation, high-frequency oscillation, and intratracheal pulmonary ventilation results in similar gas exchange, hemodynamics, and lung mechanics. Anesthesiology 2003, 99: 1102-1111. 10.1097/00000542-200311000-00016
Ferguson ND, Chiche JD, Kacmarek RM, Hallett DC, Mehta S, Findlay GP, Granton JT, Slutsky AS, Stewart TE: Combining high-frequency oscillatory ventilation and recruitment maneuvers in adults with early acute respiratory distress syndrome: the Treatment with Oscillation and an Open Lung Strategy (TOOLS) trial pilot study. Crit Care Med 2005, 33: 479-486. 10.1097/01.CCM.0000155785.23200.9E
Baydur A, Cha EJ, Sassoon CS: Validation of esophageal balloon technique at different lung volumes and postures. J Appl Physiol 1987, 62: 315-321. 10.1063/1.339151
Mehta S, Lapinsky SE, Hallett DC, Merker D, Groll RJ, Cooper AB, MacDonald RJ, Stewart TE: Prospective trial of high-frequency oscillation in adults with acute respiratory distress syndrome. Crit Care Med 2001, 29: 1360-1369. 10.1097/00003246-200107000-00011
Sjostrand UH, Lichtwarck-Aschoff M, Nielsen JB, Markstrom A, Larsson A, Svensson BA, Wegenius GA, Nordgren KA: Different ventilatory approaches to keep the lung open. Intensive Care Med 1995, 21: 310-318. 10.1007/BF01705409
Lachmann B: Open up the lung and keep the lung open. Intensive Care Med 1992, 18: 319-321. 10.1007/BF01694358
van Genderingen HR, van Vught JA, Jansen JR, Duval EL, Markhorst DG, Versprille A: Oxygenation index, an indicator of optimal distending pressure during high-frequency oscillatory ventilation? Intensive Care Med 2002, 28: 1151-1156. 10.1007/s00134-002-1368-5
Luecke T, Meinhardt JP, Herrmann P, Weisser G, Pelosi P, Quintel M: Setting mean airway pressure during high-frequency oscillatory ventilation according to the static pressure-volume curve in surfactant-deficient lung injury: a computed tomography study. Anesthesiology 2003, 99: 1313-1322. 10.1097/00000542-200312000-00012
Kolton M, Cattran CB, Kent G, Volgyesi G, Froese AB, Bryan AC: Oxygenation during high-frequency ventilation compared with conventional mechanical ventilation in two models of lung injury. Anesth Analg 1982, 61: 323-332. 10.1213/00000539-198204000-00003
Rimensberger PC, Pache JC, McKerlie C, Frndova H, Cox PN: Lung recruitment and lung volume maintenance: a strategy for improving oxygenation and preventing lung injury during both conventional mechanical ventilation and high-frequency oscillation. Intensive Care Med 2000, 26: 745-755. 10.1007/s001340051242
Goddon S, Fujino Y, Hromi JM, Kacmarek RM: Optimal mean airway pressure during high-frequency oscillation: predicted by the pressure-volume curve. Anesthesiology 2001, 94: 862-869. 10.1097/00000542-200105000-00026
Luecke T, Roth H, Herrmann P, Joachim A, Weisser G, Pelosi P, Quintel M: Assessment of cardiac preload and left ventricular function under increasing levels of positive end-expiratory pressure. Intensive Care Med 2004, 30: 119-126. 10.1007/s00134-003-1993-7
Pinsky MR: The hemodynamic consequences of mechanical ventilation: an evolving story. Intensive Care Med 1997, 23: 493-503. 10.1007/s001340050364
Butler J: The heart is not always in good hands. Chest 1990, 97: 453-460.
Talmor D, Sarge T, O'Donnell CR, Ritz R, Malhotra A, Lisbon A, Loring SH: Esophageal and transpulmonary pressures in acute respiratory failure. Crit Care Med 2006, 34: 1389-1394. 10.1097/01.CCM.0000215515.49001.A2
Brander L, Ranieri VM, Slutsky AS: Esophageal and transpulmonary pressure help optimize mechanical ventilation in patients with acute lung injury. Crit Care Med 2006, 34: 1556-1558. 10.1097/01.CCM.0000216146.51250.8D
Terragni PP, Rosboch GL, Lisi A, Viale AG, Ranieri VM: How respiratory system mechanics may help in minimising ventilator-induced lung injury in ARDS patients. Eur Respir J Suppl 2003, 42: 15s-21s. 10.1183/09031936.03.00420303
de Chazal I, Hubmayr RD: Novel aspects of pulmonary mechanics in intensive care. Br J Anaesth 2003, 91: 81-91. 10.1093/bja/aeg146
Tobin MJ: Culmination of an era in research on the acute respiratory distress syndrome. N Engl J Med 2000, 342: 1360-1361. 10.1056/NEJM200005043421808
Pelosi P, D'Onofrio D, Chiumello D, Paolo S, Chiara G, Capelozzi VL, Barbas CS, Chiaranda M, Gattinoni L: Pulmonary and extrapulmonary acute respiratory distress syndrome are different. Eur Respir J Suppl 2003, 42: 48s-56s. 10.1183/09031936.03.00420803
Gattinoni L, Chiumello D, Carlesso E, Valenza F: Bench-to-bedside review: chest wall elastance in acute lung injury/acute respiratory distress syndrome patients. Crit Care 2004, 8: 350-355. 10.1186/cc2854
Pillow JJ, Neil H, Wilkinson MH, Ramsden CA: Effect of I/E ratio on mean alveolar pressure during high-frequency oscillatory ventilation. J Appl Physiol 1999, 87: 407-414.
Kacmarek RM, Malhotra A: High-frequency oscillatory ventilation: what large-animal studies have taught us! Crit Care Med 2005, 33: S148-S154. 10.1097/01.CCM.0000156786.43935.A0
Higgins J, Estetter B, Holland D, Smith B, Derdak S: High-frequency oscillatory ventilation in adults: respiratory therapy issues. Crit Care Med 2005, 33: S196-S203. 10.1097/01.CCM.0000155922.78943.2D
Mehta S, Granton J, MacDonald RJ, Bowman D, Matte-Martyn A, Bachman T, Smith T, Stewart TE: High-frequency oscillatory ventilation in adults: the Toronto experience. Chest 2004, 126: 518-527. 10.1378/chest.126.2.518
Ferguson ND, Stewart TE: New therapies for adults with acute lung injury. High-frequency oscillatory ventilation. Crit Care Clin 2002, 18: 91-106. 10.1016/S0749-0704(03)00067-8
Lachmann B, Robertson B, Vogel J: In vivo lung lavage as an experimental model of the respiratory distress syndrome. Acta Anaesthesiol Scand 1980, 24: 231-236.
Rotta AT, Gunnarsson B, Fuhrman BP, Hernan LJ, Steinhorn DM: Comparison of lung protective ventilation strategies in a rabbit model of acute lung injury. Crit Care Med 2001, 29: 2176-2184. 10.1097/00003246-200111000-00021
Sugiura M, McCulloch PR, Wren S, Dawson RH, Froese AB: Ventilator pattern influences neutrophil influx and activation in atelectasis-prone rabbit lung. J Appl Physiol 1994, 77: 1355-1365.
Acknowledgements
This study was funded by the German Research Foundation (DFG) Grant Ma 2398/3-2. All other sources of financial support for the work contained in the article have been disclosed. The high-frequency oscillatory ventilator was provided by Viasys Healthcare (Hoechberg, Germany). The authors thank Mr Jeffrey Crowder for his editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
JK designed the study protocol, collected data, and drafted the protocol. MD designed and participated in the study protocol, collected data, and performed statistical analysis. SY collected data. KM coordinated the study and revised the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Karmrodt, J., David, M., Yuan, S. et al. Alternative protocol to initiate high-frequency oscillatory ventilation: an experimental study. Crit Care 10, R138 (2006). https://doi.org/10.1186/cc5052
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc5052