Abstract
Objective
(1) To assess the impact of high intrathoracic pressure on left ventricular volume and function. (2) To test the hypothesis that right ventricular end-diastolic volume (RVEDV) and intrathoracic blood volume (ITBV) represent cardiac preload and are superior to central venous pressure (CVP) or pulmonary capillary wedge pressure (PCWP). The validity of these parameters was tested by means of correlation with left ventricular end-diastolic volume (LVEDV), the true cardiac preload.
Design
Prospective animal study.
Subjects
Fifteen adult sheep.
Interventions
All animals were studied before and after saline washout-induced lung injury, undergoing volume-controlled ventilation with increasing levels of PEEP (0, 7, 14 and 21 cmH2O, respectively).
Measurements and main results
Left ventricular ejection fraction (LVEF), stroke volume (LVSV) and LVEDV were measured using computed tomography. ITBV and RVEDV were obtained by the thermal dye dilution technique. At PEEP 21 cmH2O, LVSV significantly decreased compared to baseline, PEEP 0 and PEEP 7 cmH2O. LVEDV was maintained except for the highest level of PEEP, while LVEF remained unchanged. RVEDV and RVEF also remained unchanged. The overall correlation of RVEDV and ITBV with LVEDV was satisfactory (r=0.56 and r=0.62, respectively) and clearly superior to cardiac filling pressures.
Conclusion
In the present study, (1) ventilation with increasing levels of PEEP did not alter RV function, while LV function was impaired at the highest level of PEEP; (2) unlike cardiac filling pressures, ITBV and RVEDV both provide valid estimates of cardiac preload even at high intrathoracic pressures.
Similar content being viewed by others
Introduction
Cyclic opening and closing of atelectatic alveoli with tidal breathing is known to be a basic mechanism leading to ventilator-induced lung injury [1]. To prevent alveolar cycling and derecruitment in acute lung injury, high levels of positive end-expiratory pressure (PEEP) have been found necessary in order to counterbalance the increased lung mass resulting from edema, inflammation and infiltrations and to maintain normal functional residual capacity (FRC) [2, 3]. Therefore, the application of high levels of PEEP is recommended [4], even if recent data by Crotti and co-workers [5] suggest that recruitment and derecruitment are not identical in the presence of lung hysteresis and that "threshold closing pressure" is substantially lower than "threshold opening pressure", questioning the routine use of high levels of PEEP.
In addition to the use of high levels of PEEP, fluid restriction is favored in patients with acute lung injury to decrease pulmonary edema [6, 7]. Both high PEEP and fluid restriction can result in significantly decreased venous return, possibly leading to organ hypoperfusion. Therefore, the maintenance of an adequate preload status is crucial in this setting. Cardiac preload is defined by the Frank-Starling relationship as the ventricular fiber length at end-diastole and is described clinically as the left ventricular end-diastolic volume [8]. In clinical practice, cardiac preload is routinely assessed by the measurement of central venous pressure (CVP) and pulmonary capillary wedge pressure (PCWP). However, it has become increasingly clear that both CVP and PCWP can be very poor predictors of preload status in critically ill patients, especially if they are ventilated with high intrathoracic pressures [9, 10, 11, 12, 13, 14].
Right ventricular end-diastolic volume (RVEDV), measured either by a modified pulmonary artery catheter or the thermal dye dilution technique, has been shown to correlate more closely with cardiac index (CI) than CVP or PCWP [9, 10, 11, 12]. Using the thermal dye dilution technique, Lichtwark-Aschoff and colleagues [13] showed that the intrathoracic blood volume (ITBV) is superior to CVP and PCWP for the assessment of the circulatory volume status in critically ill patients. All these studies, however, suffer from one major drawback [15, 16]: they used the correlation with CI to define the suitability of the measured parameters to represent cardiac preload. As CI is also affected by myocardial function and afterload, it would be highly desirable to assess the validity of these parameters by correlating them with the left ventricular end-diastolic volume (LVEDV), the "true cardiac preload" [16].
The aim of this study was to assess left ventricular volumes and function as well as to test the validity of bedside parameters available for monitoring the complex cardiopulmonary interactions during invasive mechanical ventilation. The study therefore focused on (1) measurement of LVEDV and LVEF by means of computed tomography and (2) the correlation of different markers of cardiac preload with LVEDV. We hypothesized that the thermal dye dilution technique, by simultaneously measuring RVEDV, ITBV and CO, could serve as an accurate, integrated cardiopulmonary monitoring device in the setting of acute lung injury.
Materials and methods
Animal preparation and measurements
After approval by the District Governmental Commission on the Care and Use of Animals, 15 anesthetized sheep of mixed breed weighing 41.5±6.5 kg (mean ± SD) were used for the study. The animals were premedicated with xylazine hydrochloride, 5 mg i.v., and anesthetized with ketamine, 6 mg/kg i.v. and midazolam 0.15 mg/kg. Anesthesia and muscle relaxation were maintained by continuous infusion of ketamine (10 mg/kg per h), midazolam (1 mg/kg per h) and by pancuronium bromide (0.12 mg/kg per h) throughout the experiment. Conventional orotracheal intubation was performed using a 9 mm inner-diameter cuffed endotracheal jet tube (Hi-Lo Jet, Mallinckrodt Medical, St. Louis, MO), which provides an additional lumen embedded in the inner wall of the tube. The animals were placed supine in the CT scanner and were ventilated with a Siemens Servo Ventilator 300 (Siemens-Elema, Solna, Sweden) in the volume-controlled (VC) mode with a PEEP of 5 cmH20, an I:E ratio of 1:1 and a FIO2 of 1.0. A tidal volume of 12 ml/kg and a respiratory rate of 12–14 breaths/min were applied to maintain a PCO2 value within the range of 35–40 mmHg. A continuous infusion of lactated Ringer´s solution at a rate of 5 ml/kg per h was given. Gastric emptying was achieved using a large-bore orogastric tube, which was removed thereafter.
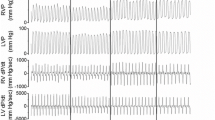
Central venous and pulmonary artery pressures were measured using a 7.5 French flow-directed thermodilution fiberoptic pulmonary artery catheter (Opticath, Abbott Laboratories, North Chicago, IL) advanced into the pulmonary artery under transduced pressure guidance via the left internal jugular vein. The right femoral artery was cannulated with a 6 French percutaneous sheath (Super Arrow-Flex, Arrow, Reading, PA) for arterial pressure monitoring. Continuous ECG monitoring was performed. For hemodynamic monitoring, a Sirecust 1281 monitor (Siemens Medical Electronics, Danvers, MA) and Novotrans II (Medex, Hilliard, OH) pressure transducers referenced to atmospheric pressure at mid thorax level were used. All hemodynamic and ventilatory variables were continuously recorded in 1-min intervals using the graphical programming software Lab-View (National Instruments, Austin, TX).
Cardiac output (CO), intrathoracic blood volume (ITBV), right ventricular end-diastolic volume (RVEDV) and right ventricular ejection fraction (RVEF) were measured via the thermal-green double indicator dilution technique using the COLD Z-021 computer (Pulsion Medizintechnik, Munich, Germany). Dye and thermal dilution were measured using a 4 French fiberoptic catheter (Pulsiocath, Pulsion Medizintechnik) advanced through the 6 French sheath in the femoral artery into the descending aorta. The COLD-derived parameters were determined by injecting 10 ml of 5% glucose solution containing 1 mg/ml of indocyanine green at a temperature between 0 and 10°C into the right atrium via the distal lumen of the pulmonary artery catheter during end-expiratory hold. Densimetric and thermal data were gathered by the fiberoptic catheter in the descending aorta and analyzed on the Pulsion COLD Z-021 computer. ITBV was calculated from the cardiac output and the mean transit time (MTT) of the dye according to the formula:
ITBV = (MTTdye * CO).
All parameters are expressed in milliliter/kilogram body weight.
In addition to the CO measurements performed using the COLD system, CO and stroke volume were measured in triplicate using the pulmonary artery catheter by injecting 10 ml aliquots of ice-cold saline into the right atrium during end-expiratory hold. Standard formulas were used to calculate transpulmonary shunt, oxygen delivery and oxygen consumption. Arterial and mixed venous blood gases at 37°C were analyzed on an ABL300 (Radiometer A/S, Copenhagen, Denmark).
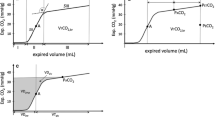
To measure the elastance of the respiratory system and to partition it into its pulmonary and chest wall components, the occlusion method was used [17]. Distal tracheal pressure (Ptrach) was measured by connecting an air-filled pressure transducer (Novotrans II, Medex, Hilliard, OH) to the additional lumen of the Hi-Lo jet tube ending at the tip of the tube. The pressure signals were sampled on-line at a rate of 50 Hz using a Signal Conditioning System (SCXI, National Instruments, Austin, TX) with a four-channel isolation amplifier with excitation. For readout of the pressure waves, a 12-bit analog/digital converter (SCXI-1100 Data Acquisition Module, National Instruments, Austin, TX) was used. The pressure curves were analyzed using the graphical programming software Lab-View (National Instruments, Austin, TX). Expiratory tidal volume was obtained from the Servo Ventilator.
Esophageal pressure (Pes) was measured with a thin-walled latex balloon sealed over one end of a polyethylene catheter (International Medical, Zutphen, Netherlands) inflated with 0.5–1 ml of air. The catheter was positioned at the lower third of the esophagus, as confirmed by computed tomography. The esophageal balloon was connected to a pressure transducer (Novotrans II, Medex, Hilliard, OH) and the signals were sampled and processed as described above for tracheal pressures. Ptrach and Pes were simultaneously recorded during a 5 s airway occlusion at end-inspiration and end-expiration. The end-inspiratory and end-expiratory airway occlusion maneuver was repeated three times at 15 s intervals and mean values were used for calculations of applicable elastances.
Lavage procedure
With the sheep in supine position, the endotracheal tube was disconnected from the ventilator and warmed saline was instilled from a height of 50 cm until a meniscus was seen in the tube. The fluid was retrieved via gravity drainage after 45 s of apnea followed by endotracheal suctioning. Instilled and retrieved volumes were measured. Between the lavages, the sheep were manually ventilated with an FIO2 of 1.0 using an AMBU self-inflating bag. The lavage process was repeated until adequate impairment of gas exchange (defined as PaO2<100 mmHg 15 min after the last lavage) and respiratory mechanics were achieved. After lung lavage, lung injury was established by ventilating the sheep with zero end-expiratory pressure for 60 min.
Determination of left ventricular volumes by rapid acquisition cine computed tomography
The Imatron C-150XP electron beam computed tomography (EBCT) scanner (Imatron, San Francisco, CA) was used for the study. The advantages of the EBCT are sub-second scan times and the ability to produce high-resolution 3D data sets with excellent z-axis resolution [18].
Left ventricular imaging was performed during end-expiratory hold for baseline conditions and each level of PEEP after lung injury. Imaging was carried out in cine mode (modified Multi-Slice-Mode, MSM), a sequence used to evaluate myocardial contractility and ventricular volumes. In this mode, the electron beam sweeps a single target ring a designated number of times to cover one full cardiac cycle before it moves to the next target ring. Two slices per sweep are acquired using the split detector system. Images are acquired at 50-ms intervals with an 8-ms inter-scan delay or a scanning speed of 17 images/s. At a heart rate of 100 beats/min with a cycle length of 600 ms, the cardiac cycle can be completely imaged through end-systole and end-diastole with a 10-frame movie (580 ms acquisition time) [18]. The total scan time for 80 slices is 2.5 s. The sequences are initiated from ECG gating. In order to optimize contrast administration, a circulation time was obtained by injecting 15 ml of contrast media at a rate of 4 ml/s. According to the circulation time obtained, imaging was delayed until maximal opacification was achieved by infusing 30 ml of contrast media at a rate of 4 ml/s via the jugular vein. Left ventricular imaging was followed by CO measurements using the COLD and pulmonary artery catheter. All three measurements were carried out within 5 min.
The cardiac images were stored on magneto-optical discs. Left ventricular end-diastolic and end-systolic volumes as well as left ventricular ejection fraction were calculated as described by Reiter and colleagues [18] using the Imatron software package: end-diastolic and end-systolic frames were chosen for each of the eight levels. End-diastolic volume was visually identified as the frame showing the maximal volume of the left ventricular cavity. End-systole was visually identified as the frame showing the smallest volume of the left ventricular cavity, generally three to four frames (150–200 ms) after the end-diastolic frame. Left ventricular volumes were planimetered with exclusion of the papillary muscles from the left ventricular apex to the left ventricular base, where the left atrium can easily be defined. Measurements of the left ventricular volume were discontinued at the level at which the aortic valve cusps or sinuses were clearly visualized. The tomographic measurements of end-diastolic and end-systolic volume at each level were added. Computer tomographically derived left ventricular stroke volume was determined as the difference between the end-diastolic and end-systolic volumes calculated.
Experimental protocol
The sheep were intubated and placed supine in the CT scanner. After instrumentation had been completed, baseline measurements were obtained, including arterial and mixed venous blood gases, pulmonary artery catheter and COLD catheter-derived parameters (COPAC, SV, PCWPPAC, CVP and COCOLD, SVCOLD, ITBV, RVEDV, RVEF, respectively). Systemic and pulmonary artery pressures, ventilatory parameters and mixed venous saturation were acquired at 1-min intervals. Tidal volumes, tracheal and esophageal pressures were recorded. Computed tomographic images of the left ventricle were performed as described above. After completion of all baseline measurements, lung injury was induced by saline washout. All groups were ventilated in the volume-control mode (VCV) with an I:E time of 1:1, an FIO2 of 1.0 and frequencies between 12–20/min according to the PCO2 value. Peak inspiratory pressure was limited to 45 cmH2O.
Following 60 min of ventilation with zero PEEP in order to establish lung injury, left ventricular imaging was performed, along with the complete set of measurements made at baseline. Thereafter, PEEP was increased in 60-min intervals to 7, 14 and 21 cmH2O, respectively, in order to recruit the collapsed parts of the lung. Measurements were performed before each PEEP increment for ZEEP, PEEP 7 and PEEP 14, and 60 min after PEEP 21, respectively. After completion of the protocol, the animals were killed with high dose thiopental (30 mg/kg) followed by potassium chloride.
Statistical analysis
All values are reported as means ± SD unless otherwise specified. One-way analysis of variance (ANOVA) was used to test for differences between baseline conditions before, and different PEEP levels after, the induction of lung injury. T-tests were used for multiple comparisons. To correct for the amount of tests performed, the level of significance was set at p<0.001. Linear regression analysis was used to evaluate the relationships between CT-derived heart volumes and various bedside parameters. All statistical tests were used in a descriptive manner. Statistical software package SAS 6.12 (SAS Institute, Cary, NC) was used for analysis.
Results
Lung injury
The injury procedure resulted in a substantial decrease in PaO2, an increase in transpulmonary shunt and an increase in static lung elastance (Table 1). All animals survived the experimental protocol. The volume of saline instilled was 6,874±1,443 ml. The volume of saline recovered was 6,596±1,532 ml, resulting in a residual intra-alveolar volume of 278±288 ml.
Hemodynamic effects of positive end-expiratory pressure
The main results are shown in Table 1. Stroke volume was maintained up to high levels of PEEP. Left ventricular stroke volume, as measured by EBCT, only decreased significantly compared to baseline, zero PEEP and PEEP of 7 cmH2O (p<0.001) at a PEEP level of 21 cmH2O. The decrease in left ventricular end-diastolic volume (LVEDV) observed under increasing levels of PEEP was significant only when comparing PEEP 21 and ZEEP (1.7±0.3 vs 2.2±0.4 ml/kg, at a PEEP level of 21 cmH2O p=0.0006). Left ventricular ejection fraction, an estimate for cardiac contractility, was preserved and the decrease observed at the highest level of PEEP did not reach a level of statistical significance. Of note, RVEDV and RVEF, as well as ITBV, did not change significantly throughout the experiment.
Cardiac output and oxygen delivery were maintained at all levels of PEEP. Taking into account that stroke volumes and COs measured by EBCT, pulmonary artery catheter (PAC) and COLD could not be obtained simultaneously, but spanned a 5-min interval, correlations between the different measurements were good (COPAC versus COEBCT: r=0.91, p<0.0001, COCOLD versus COEBCT: r=0.89, p<0.0001 and COCOLD versus COPAC: r=0.94, p<0.0001; Pearson correlation coefficients).
Correlation of bedside parameters of cardiac preload with left ventricular end-diastolic volume and cardiac output
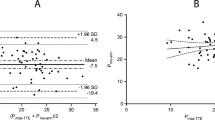
The overall correlation of RVEDV and ITBV with LVEDV was significant (RVEDV vs LVEDV: r=0.56; ITBV vs LVEDV: r=0.62, Fig.1). In contrast, no positive correlation between CVP and PCWP with LVEDV could be found (CVP vs LVEDV: r= −0.34; PCWP vs LVEDV: r= −0.37) (Table 2).
Despite the relatively small sample size, statistical significance for most levels of PEEP was reached for the correlations of ITBV and RVEDV with LVEDV. Of note, CVP and PCWP failed to correlate with LVEDV even under baseline conditions. In a second step, transmural pressures (PCWPtrm = PCWP−Pes; CVPtrm = CVP−Pes) were calculated, but failed to improve correlation (CVP vs LVEDV: r= −0.37; CVPtrm vs LVEDV: r= −0.17; PCWP vs LVEDV: r= −0.34; PCWPtrm vs LVEDV: r= −0.10; Pearson correlation coefficients).
Left ventricular end-diastolic volume, RVEDV and ITBV showed good correlations with CO ( LVEDV vs CO: r=0.48; RVEDV vs CO: r=0.56; ITBV vs CO: r=0.64) (Table 3).
Discussion
The main findings of this study are as follows: first, in an ovine saline washout model of acute lung injury, ventilation with high levels of PEEP did not significantly compromise right ventricular function, while left ventricular function was impaired at a PEEP of 21 cmH2O, as indicated by a decrease in LVSV. Second, ITBV and RVEDV are clearly superior to cardiac filling pressures in the assessment of cardiac preload at high intrathoracic pressures.
Ventricular volumes and function under increasing levels of positive end-expiratory pressure
Although mechanical ventilation and ventilatory maneuvers like PEEP have profound hemodynamic effects, a practical clinical approach to understanding the interaction between ventilation and cardiac ejection performance is still not feasible, primarily because of difficulties in estimating LVEDV [19]. Therefore, the effects of increasing levels of PEEP on LVEDV and LVEF were studied in this experimental setting using electron beam computed tomography.
In this study, increasing levels of PEEP up to 14 cmH2O did not compromise LVEDV or LVEF. The small, yet significant, decrease in LVEDV and LVSV seen at the highest level of PEEP may indicate impairment of LV function and may be, at least in part, due to direct mechanical compression of the cardiac fossa [19, 20] caused by the significant increase in total lung volume (data not shown). Right ventricular function, as estimated by measuring RVEDV and RVEF, also was not compromised. This finding is in accordance with the results from Cheatham and colleagues [12], who also found RV function to be well preserved in patients treated with high levels of PEEP due to acute respiratory failure, and they therefore concluded that ventricular dysfunction is not an inevitable result of therapy with PEEP.
Preservation of RV function in our model may have been facilitated by the fact that a rather liberal fluid regimen (lactated Ringer´s solution at a rate of 5 ml/kg per h) was used, thus maintaining adequate venous return despite high levels of PEEP. This may be a limitation of the study, as fluid restriction is generally favored in acute lung injury in clinical settings. In hemodynamically stable postoperative, fluid-resuscitated patients, increasing positive pressure also had only minimal effects on venous return, primarily because of an in-phase-associated pressurization of the abdominal compartment [21]. Furthermore, saline washout only moderately increased MPAP. Brunet and colleagues [22] emphasized the importance of right ventricular afterload by showing an inverse correlation between changes in RVEDV and RVEF and the increase in MPAP. As RVEDV did not significantly increase, we do not believe that ventricular interdependence played a major role in this model.
Finally, and maybe most importantly, the PEEP-induced increase in intrathoracic pressure might have been blunted by the high lung elastance, resulting in relatively low pericardial pressures. Indicators of a very limited transmission, by PEEP, of intrapulmonary pressures and increases thereof to the mediastinal area are the relatively small increases of esophageal pressure, CVP and PCWP between PEEP zero and 21 cmH2O. All measurements of ventricular volumes and function were taken during end-expiratory hold. While this allows for comparison of static PEEP-induced left and right ventricular changes, no conclusions can be made about the dynamic effects of the ventilatory cycle on ventricular performance.
This may pose some limitations on our findings, as Groeneveld et al. [23] demonstrated significant inspiratory decreases in RVEF and increases in right ventricular end-systolic volume (RVESV) and RVEDV during ventilation with relatively large pressure amplitudes (Ppeak 32±7 cmH2O at 5 cmH2O of PEEP). Therefore, they concluded that cyclic RV afterloading necessitates multiple thermodilution measurements equally spaced in the ventilatory cycle for reliable assessment of RV performance during mechanical ventilation. Unfortunately, this approach is not feasible for CT-based ventricular imaging due to the large amount of contrast media necessary. Concluding, we cannot rule out the possibility that cardiac performance in our model was somewhat compromised during inspiration. Vieillard-Baron and co-workers [24], however, showed that tidal volume (which was kept constant during PEEP increase in our study), but not airway pressure, was the main determinant factor of RV afterloading during mechanical ventilation. Therefore, the potential inspiratory compromise should have been comparable among the different levels of PEEP studied.
Correlation of bedside parameters of cardiac preload with left ventricular end-diastolic volume and cardiac output
In the model studied, RVEDV and ITBV were superior to cardiac filling pressures for the assessment of cardiac preload, confirming the finding of former studies [9, 10, 11, 12, 13]. Durham et al. [9] studied 38 critically ill patients using a fast response thermodilution catheter, allowing for RVEDV measurements. While correlation between cardiac index (CI) and PCWP was poor (r=0.10), correlation between CI and the RVEDV index was significant (r=0.60) and very similar to the findings in 29 critically ill patients studied by Diebel et al. (r=0.61) [10]. Interestingly, our data, obtained in an experimental setting, yielded almost identical results (r=0.56). It should be emphasized, however, that RVEDV becomes a poor reflector of left ventricular preload whenever the right ventricle is the limiting factor in circulatory failure. In five out of eighteen patients with septic shock accompanied by pulmonary hypertension, for example, the right ventricle was found to be systolic and/or diastolic overloaded, explaining the left ventricular preload decrease and the inability of blood volume expansion to restore it [25]. Right ventricular failure might also have been the reason for the absence of correlation between RVEDV and CI in 11 out of the 38 patients studied by Durham et al. [9].
The effect of end-expiratory pressure on the assessment of cardiac preload was examined by the same group [11] and by Cheatham et al. [12]: both studies agreed that, unlike the PCWP, RVEDV represents a reliable indicator in the mechanically ventilated patient. Lichtwark-Aschoff and colleagues [13] investigated ITBV as a marker for the circulatory volume status in critically ill patients: ITBV showed good correlation with CI (r=0.488) and oxygen delivery (r=0.46), while CVP and PCWP did not indicate the volume status in mechanically ventilated patients. The authors stated that, being a pure volume indicator, ITBV correlates only with the preload component of CI. These findings were basically repeated in the study of Wiesenack et al. [26], who found a significant correlation between ITBV and CO (r=0.55). Again, neither CVP nor PCWP showed significant correlation with CO ( r=0.09 and r=-0.27, respectively).
While all these data strongly suggest that volume parameters like RVEDV or ITBV are reliable markers of cardiac preload, that hypothesis had not been specifically tested yet. For the first time, therefore, this study correlates the various bedside parameters with LVEDV, the true cardiac preload. Due to the small sample size, we did not try to look for statistical differences between the correlations for RVEDV and ITBV with LVEDV, respectively, and believe that—from a clinical point of view—both parameters are equally well suited to estimate cardiac preload. As in the studies cited above, cardiac filling pressures did not reflect cardiac preload. In accordance with data from Safcsak and colleagues [27], the correction of filling pressures for esophageal pressures (transmural filling pressures) did not improve correlation with LVEDV.
Correlations of LVEDV, RVEDV and ITBV with cardiac output were satisfactory (overall Pearson correlation coefficients ranging from 0.48 to 0.64), but showed large variations. Again, this emphasizes the fact that CO is influenced by contractility, afterload and heart rate, in addition to preload [15, 16]. Therefore, we conclude that the validity of "bedside" parameters of cardiac preload should be tested primarily against LVEDV, while their correlation with CO may be misleading.
Summarizing, the main findings of this study are as follows: first, in this model of acute lung injury ventilation with increasing levels of PEEP did not alter RV function, while LV function was impaired at the highest level of PEEP studied. Second, ITBV and RVEDV reliably reflect cardiac preload even at high intrathoracic pressures and are clearly superior to cardiac filling pressures.
References
Dreyfuss D, Saumon G (1998) Ventilator-induced lung injury. Lessons from experimental studies [State of the art]. Am J Respir Crit Care Med 157:294–330
Maggiore SM, Jonson B, Richard JC, Jaber S, Lemaire F, Brocahrd L (2001) Alveolar derecruitment at decremental positive end-expiratory pressure levels in acute lung injury. Am J Respir Crit Care Med 164:795–801
Gattinoni L, D'Andrea L, Pelosi P, Vitale G, Pesenti A, Fumagalli F (1993) Regional effects and mechanisms of positive end-expiratory pressure in early adult respiratory distress syndrome. JAMA 269:2122–2127
Rouby JJ, Lu Q, Goldstein I (2002) Selecting the right level of positive end-expiratory pressure in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 165:1182–1186
Crotti S, Mascheroni D, Caironi P, Pelosi P, Ronzoni G, Mondino M, Marini JJ, Gattinoni L (2001) Recruitment and derecruitment during acute respiratory failure. Am J Respir Crit Care Med 164:131–140
Mitchell JP, Schuller D, Calandrino FS, Schuster DP (1992) Improved outcome based on fluid management in critically ill patients requiring pulmonary artery catheterization. Am Rev Respir Dis 145:990–998
Humphrey H, Hall J, Sznajder I, Silverstein M, Wood L (1990) Improved survival in ARDS patients associated with a reduction in pulmonary capillary wedge pressure. Chest 97:1176–1183
Starling EH (1918) The Linacre lecture on the law of the heart given at Cambridge, 1915. Longmans, Green & Co, London
Durham R, Neuaber K, Vogler G, Shapiro M, Mazuski J (1995) Right ventricular end-diastolic volume as a measure of preload. J Trauma. 39:218–223
Diebel LN, Wilson RF, Tagett MG, Kline RA (1992) End-diastolic volume—a better indicator of preload in the critically ill. Arch Surg 127:817–821
Diebel LN, Myers T, Dulchavsky S (1997) Effects of increasing airway pressure and PEEP on the assessment of cardiac preload. J Trauma 42:585–590
Cheatham ML, Nelson LD, Chang MC, Safcsak K (1998) Right ventricular end-diastolic volume index as a predictor of preload status in patients with positive end-diastolic pressure. Crit Care Med 26:1801–1806
Lichtwark-Aschoff M, Zeravik J, Pfeiffer UJ (1992) Intrathoracic blood volume accurately reflects circulatory volume status in critically ill patients with mechanical ventilation. Intensive Care Med 18:142–147
Jardin F, Farcot JC, Boisante L, Curien N, Margairaz A, Bourdarias JP (1981) Influence of positive end-expiratory pressure on left ventricular performance. N Engl J Med 304:387–392
Edwards JD (1998) Time for a reappraisal of the use of right ventricular ejection fraction catheters? Crit Care Med 26:1769–1770
Hedenstierna G (1992) What value does the recording of intrathoracic blood volume have in clinical practice? Intensive Care Med 18:137–138
Gattinoni L, Pelosi P, Suter PM, Pedoto A, Vercesi P, Lissoni A (1998) Acute respiratory distress syndrome caused by pulmonary and extrapulmonary disease. Am J Respir Crit Care Med 158:3–11
Reiter SJ, Rumberger JA, Feiring AJ, Stanford W, Marcus ML (1986) Precision of measurements of right and left ventricular volume by cine computed tomography. Circulation 74:890–900
Pinsky MR (1997) The hemodynamic consequences of mechanical ventilation: an evolving study. Intensive Care Med 23:493–503
Marini JJ, Culver BN, Butler J (1981) Mechanical effects of lung distention with positive pressure in cardiac function. Am Rev Respir Dis 124:382–386
Van Den Berg PCM, Jansen JRC, Pinsky MR (2002) Effect of positive pressure on venous return in volume-loaded cardiac surgical patients. J Appl Physiol 92:1223–1231
Brunet F, Gueret P, Dubourg O, Farcot JC, Margairaz A, Bourdarias JP (1988) Right ventricular performance in patients with acute respiratory failure. Intensive Care Med 14:474–477
Groeneveld AB, Berendsen RR, Schneider AJ, Pneumatikos IA, Stokkel LA, Thijs LG (2000) Effect of the mechanical ventilatory cycle on thermodilution right ventricular volumes and cardiac output. J Appl Physiol 89:89–96
Vieillard-Baron A, Loubieres Y, Schmitt JM, Page B, Dubourg O, Jardin F (1999) Cyclic changes in right ventricular output impedance during mechanical ventilation. J Appl Physiol 87:1644–1650
Schneider AJ, Teule GJ, Groeneveld AB, Nauta J, Heidendal GA, Thijs LG (1988) Biventricular performance during volume loading in patients with septic shock, with emphasis on the right ventricle: a combined hemodynamic and radionuclide study. Am Heart J 116:103–112
Wiesenack C, Prasser C, Keyl C, Roedig G (2001) Assessment of intrathoracic blood volume as an indicator of cardiac preload: single transpulmonary thermodilution technique versus assessment of pressure preload parameters derived from a pulmonary artery catheter. J Cardiothorac Vasc Anesth 15:584–588
Safcsak K, Fusco MA, Miles WS, Cheatham ML, Nelson LD (1995) Does transmural pulmonary artery occlusion pressure (PAOP) via esophageal balloon improve prediction of ventricular preload in patients receiving positive end-expiratory pressure (PEEP)? Crit Care Med 23 (Suppl):A244
Acknowledgements
The authors wish to thank Thomas Bruckner, Dipl. Math., Schwetzingen, Germany, for statistical advice.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by a grant from the Faculty of Clinical Medicine, University of Mannheim.
Rights and permissions
About this article
Cite this article
Luecke, T., Roth, H., Herrmann, P. et al. Assessment of cardiac preload and left ventricular function under increasing levels of positive end-expiratory pressure. Intensive Care Med 30, 119–126 (2004). https://doi.org/10.1007/s00134-003-1993-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-1993-7