Abstract
Background
Inflammatory cascades contribute to secondary injury after intracerebral hemorrhage (ICH) via humoral factors and cell-mediated cytotoxicity. Several experimental models were previously developed to analyze post-hemorrhagic neuroinflammation. However, neuroinflammatory markers have not been compared face-to-face between these models so far, and therefore, pathophysiological conclusions drawn from only one individual model may not be valid.
Methods
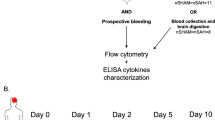
We compared neuroinflammatory pathways in the two most common murine models: striatal injection of autologous blood or collagenase. Expression of pro- and anti-inflammatory cytokines (IL-1, TNF-α, IFN-γ, IL-6, TGF-β and IL-10) as well adhesion molecule expression (VCAM-1, ICAM-1) was analyzed by RT-PCR at several time points after ICH induction. Outcome and physiological parameters were compared between the models.
Results
Both models induced a profound and dynamic increase in the expression of pro-inflammatory cytokines and adhesion molecules. However, blood injection resulted in significantly more pronounced alteration of these markers than collagenase injection. This difference was associated with worse outcome after blood injection compared to the collagenase model despite equal ICH volumes.
Conclusions
This is the first study performing a face-to-face comparison of neuroinflammatory pathways in the two most widely used murine ICH models, revealing substantial differences between the models. This discrepancies need to be taken into account in designing future studies employing experimental ICH models, especially when analyzing neuroinflammatory pathways and therapies.
Similar content being viewed by others
Background
Intracerebral hemorrhage (ICH) represents about 10-15% of all strokes. Compared to ischemic stroke, it is associated with substantially higher morbidity and mortality [1, 2]. In contrast to the major importance of ICH as a health care problem, no specific therapy for ICH is available until now. Moreover, the current understanding of crucial pathophysiological mechanisms is limited [3].
To improve the search for potential therapeutic targets in ICH, several rodent models of ICH have been developed [4–6]. The most widely used techniques are direct injection of either blood or of collagenase, respectively [4, 7, 8]. Collagenase digests the extracellular matrix of small vessels and dose-dependently causes blood extravasation. Although both methods fail to reflect important components of the pathophysiology of ICH in patients [9], they allow to study the impact of extravascular blood on the brain parenchyma. However, differences in signaling cascades of pathophysiologically relevant mechanisms between these models are likely.
Secondary inflammatory damage to brain tissue has emerged as a common link between differing types of central nervous system disorders [3, 10–12]. Several studies using rodent ICH models have suggested a significant contribution of inflammatory pathways to the pathophysiology of ICH [13, 14]. Inflammatory mechanisms have been examined in both the blood and the collagenase injection model [13]. The main inflammatory pathways after ICH are leukocyte migration into the brain, microglial activation, cerebral cytokine expression and production of other neurotoxic factors including matrix metalloproteinases and reactive oxygen species [14]. Unfortunately, specific aspects of neuroinflammation have not been compared face-to-face between these models so far, and therefore, pathophysiological conclusions drawn from only one individual model may not be valid.
The aim of the present study therefore was to compare the dynamic changes in cerebral expression of important cytokines and adhesion molecules as key markers of neuroinflammation in the autologous blood injection and the collagenase injection model of intracerebral hemorrhage.
Materials and methods
Animals
In accordance with national guidelines for the use of experimental animals the study was conducted using age-matched, mature male mice (C57BL/6, Charles River Laboratories, 10-12 weeks of age, body weight 20-25 g). The protocols were approved by the governmental committees (Regierungspraesidium Karlsruhe, Germany).
Animal experiments
Spontaneously breathing mice were anesthetized with halothane (1%-1.5%) in an oxygen/air mixture. After placing the animals in a stereotactic frame (Stoelting, USA) with a mouse adaptor (Model 51625, Stoelting, USA) a borehole was drilled at 2 mm left and 0.5 mm anterior to the bregma as previously described [15, 16].
Using an infusion system containing a 25 G needle connected (1) to a 50 μl microsyringe (Hamilton, Switzerland) for the injection of 30 μL autologous blood (taken from the retro-orbital plexus) or (2) to a 10 μL microsyringe (SGE, Austria) for the injection of 0.5 μL sterile saline containing 0.045 U collagenase type VII (Sigma, Germany) was inserted into the striatum at 3.5 mm depth from scull. The duration of both operations of approximately 45 min was matched to avoid an interference caused by perioperative management including anesthesia. Sham operation was conducted by the same procedure and with the same duration as for ICH induction including placement of the microneedle but without injection of fluid.
Hematoma measurement
In separate experiments, mice were euthanized 24 h after ICH induction (n = 7 per group). 40 μm thick coronal cryosections were cut every 400 μm. Unstained sections were scanned at 600 dpi. The hemorrhagic area was marked and measured using a public domain image analysis program (ImageJ). Total hematoma volume was obtained by integrating measured areas and distance between sections.
RNA isolation and real-time polymerase chain reaction
RNA was isolated from separated cerebral hemispheres using the RNeasy kit (Qiagen). Reverse transcription was performed with the High Capacity complementary DNA Archive Kit and real-time polymerase chain reaction with SYBR-Green assays (on an ABI7500 real-time polymerase chain reaction system (Applied Biosystems). Primers were purchased as ready-to-use primer sets for each gene (all from Super Array, IL-1β: PPM03109E, IL-10: PPM03017B, IL-6: PPM03015A, TNF-α: PPM03113A, IFN-γ: PPM03121A, TGF-β: PPM02991A, VCAM-1: PPM03208B, ICAM-1: PPM03196A). All assays were run in duplicates. A linear dilution-amplification curve was obtained from diluted pooled samples. Using this curve the expression of each gene was quantified relative to the expression of the housekeeping gene encoding for peptidylprolyl isomerase A (cyclophilin), according to the relative standard curve method. Analysis of mRNA expression was performed blinded to treatment groups.
Statistical analysis
All values in bar graphs are expressed as mean ± standard deviation (SD). We used the Mann-Whitney U-Test for comparison of two groups. For three or more groups we applied the Kruskal-Wallis H test with Dunn's post hoc testing, using GraphPad Prism 5 software. P < 0.05 was considered statistically significant.
Results
Differing outcome despite same ICH volume in the autologous blood and colleganase injection model
Both models were optimized to induce ICH of comparable blood volume as used in most previous experimental ICH studies [15–17]. Injection of either 30 μL autologous blood or 0.045 U collagenase VII into the left striatum resulted in an intracerebral hematoma volume of approx. 15-17 mm3 (Figure 1a, b). However, 24 h after ICH induction the hemorrhagic area appeared generally denser in the blood injection model than after collagenase-induced ICH (Figure 1a). Total mortality of mice differed between the experimental models in this study (Figure 1c). While no mice died in the sham group, overall mortality was 6.3% in the collagenase injection model (3/48 operated mice) and 10.1% in the autologous blood injection model (8/79 operated mice). Both ICH models were associated with a pronounced weight loss compared to sham operated mice (Figure 1d). However, only mice undergoing blood-injection ICH showed a significant but transient hypothermia 24 h after ICH compared to the sham group (Figure 1d).
Characterization of the used ICH models. (a) Representative images from the same anatomical region at 24 h after sham operation, intrastriatal injection of 0.045 U collagenase ("Collagenase") or 30 μl autologous blood ("Blood") as used for measurement of hematoma volume. (b) Hemorrhage volume was determined 24 h after ICH by integration of serial coronal sections, no difference between the collagenase and blood injection model was detected (n = 7, 2 individual experiments). (c) Overall mortality was determined for all animals used in this study treated by sham operation or ICH induction by one of both models, respectively. (d) Body weight and rectal body temperature was measured in naïve mice and at the indicated time points after sham operation or ICH induction by the respective model (n = 6-11 per group).* p < 0.05 between Sham and Collagenase; # p < 0.05 between Sham and Blood.
Cerebral expression patterns of pro-inflammatory cytokines
We analyzed the relative expression of key pro-inflammatory cytokines at 3 h, 24 h, 72 h and 7d after ICH induction in both ICH models and after sham operation (Figure 2). IL-1β and TNF-α have been well characterized as the main neurotoxic cytokines of microglial source after ischemic and traumatic brain injury [18–20]. We detected a significant increase of both cytokines in the hemorrhagic hemispheres of mice undergoing ICH induction in both models compared to the sham group (Figure 2a, b). Increased cytokine expression occurred very early after ICH and peaked already at 3 h for TNF-α and at 24 h for IL-1β. Autologous blood injection, but not collagenase injection, induced a significant increase in IL-1β at 24 h and TNF-α expression 3 h after ICH in the contralateral, non-hemorrhagic hemisphere (Figure 2a, b). IL-6 is a pleiotropic cytokine produced by various cellular sources in the brain after CNS lesions [21]. IL-6 expression was significantly increased 6 h after ICH in both ICH models and at 24 h in the collagenase model compared to sham (Figure 2c). Interestingly, autologous blood injection resulted in significantly higher IL-6 expression than collagenase injection in the hemorrhagic and the non-hemorrhagic hemisphere at 6 h (Figure 2c). Interferon-gamma (IFN-γ) was analyzed as the key neurotoxic cytokine produced by activated lymphocytes [22, 23]. IFN-γ expression did not increase within the first 3d after ICH, but was significantly overexpressed 7d after ICH in both ICH models compared to sham (Figure 2d). Blood injection induced a significantly higher, approx. 5-fold IFN-γ expression compared to the collagenase-injection model and also increased IFN-γ expression in the contralateral hemisphere (Figure 2d).
Expression patterns of pro-inflammatory cytokines after ICH. Relative expression (RE) was determined for (a) IL-1β, (b) TNF-α, (c) IL-6 and (d) IFN-γ at the indicated time points in the hemorrhagic (ipsilateral) and non-hemorrhagic (contralateral) hemispheres after sham operation or ICH induction by the collagenase or autologous blood injection model. Horizontal lines indicate significant statistical differences (p < 0.05) between the indicated groups (n = 5 per group, 2-3 individual experiments).
Cerebral expression patterns of anti-inflammatory cytokines
Previous reports from our and other groups have shown a neuroprotective effect of the anti-inflammatory cytokines IL-10 and TGF-β, respectively, after CNS lesions [20, 24–26]. We detected a significant increase of IL-10 mRNA expression only in the autologous blood injection model (Figure 3a). An up to 3-fold increase in IL-10 expression occurred in the hemorrhagic hemispheres 24 h to 7d after striatal blood injection, while collagenase-induced ICH did not affect IL-10 expression (Figure 3a). In contrast, TGF-β transcription was not altered by any experimental protocol at any time point after ICH induction or sham operation (Figure 3b).
Expression patterns of anti-inflammatory cytokines after ICH. We determined the relative expression (RE) of (a) IL-10 and (b) TGF-β mRNA at the indicated time points in the hemorrhagic (ipsilateral) and non-hemorrhagic (contralateral) hemispheres after sham operation or ICH induction by the collagenase or autologous blood injection model. Horizontal lines indicate significant statistical differences (p < 0.05) between the indicated groups (n = 5 per group, 2-3 individual experiments).
Expression of cerebral adhesion molecules after experimental ICH
The endothelial adhesion molecules VCAM-1 and ICAM-1 have been associated with transendothelial diapedesis of leukocytes and subsequent secondary neuroinflammation in various non-inflammatory CNS disorders and particularly experimental ischemic stroke [27–29]. Significant VCAM-1 upregulation was observed only in the hemorrhagic hemispheres in the autologous blood injection model 3d and 7d after ICH compared to sham and collagenase injection (Figure 4a). Surprisingly, collagenase injection did not significantly alter VCAM-1 expression at any measured time point after ICH induction (Figure 4a). In contrast, ICAM-1 expression was already substantially increased 3 h after ICH induction in both models compared to sham control (Figure 4b). ICAM-1 expression was approx. 12-fold higher than in sham treated animals already 3 h after ICH in the blood injection model and was also significantly higher than in the collagenase group (Figure 4b). A similar pattern, but less pronounced, was observed 24 h after ICH. In contrast, at 3d and 7d after hemorrhage ICAM-1 expression was already normalized again in the collagenase injection model while it remained significantly upregulated in animals with blood-injection ICH.
Expression of cerebral endothelial adhesion molecules after ICH. (a) VCAM-1 and (b) ICAM-1 expression was measured at the indicated time points in the hemorrhagic (ipsilateral) and non-hemorrhagic (contralateral) hemispheres after sham operation or ICH induction by the collagenase or autologous blood injection model. Horizontal lines indicate significant statistical differences (p < 0.05) between the indicated groups (n = 5 per group, 2-3 individual experiments).
Discussion
To the best of our knowledge, this is the first study performing a face-to-face comparison of neuroinflammatory pathways in the two most widely used models of murine experimental intracerebral hemorrhage. The major findings of this work are that (1) experimental ICH induces a profound induction of cerebral cytokine expression, (2) ICH increases the expression of cerebral adhesion molecules, (3) autologous blood injection alters these mechanisms generally more pronounced than collagenase injection, (4) blood injection, but not collagenase, induces neuroinflammatory pathways also in the contralateral hemispheres, and (5) the difference in the extent of ICH-induced neuroinflammation between the 2 models is associated with worse outcome in the blood than the collagenase injection model despite equal hematoma volumes.
The kinetics of cytokine expression within the first week after experimental ICH was quite dynamic. The expression pattern differed distinctively between the analyzed cytokines and showed an early peak for IL-1, TNF-α and IL-6 while IFN-γ was significantly increased only at 7d after ICH. The kinetics of cerebral cytokine expression observed in this study resembled the pattern observed after focal cerebral ischemia [30, 31]. There, microglial cells have been identified as the main producers of the early increase in intracerebral IL-1 and TNF-α, while the delayed expression of IFN-γ correlated with the later invasion of lymphocytes-the main source of IFN-γ-to the brain [20, 32–34]. VCAM-1 mRNA expression also showed a delayed increase in parallel to IFN-γ expression. This is especially notable because VCAM-1 has previously been shown to be the key adhesion molecule controlling invasion of lymphocytes to brain lesions after ischemic stroke [23, 28] and might thereby be of relevance in the cascade of lymphocyte invasion and cerebral IFN-γ production after ICH.
Previous studies have investigated microglia/macrophage activation as well as brain leukocyte invasion after experimental ICH [34–36]. Neutrophils have been shown as the earliest subpopulation invading the brain after ICH in preclinical studies [37]. Moreover, lymphocytes migrated to the lesion at approx. 48-72 h after ICH [35]. A report by Loftspring et al. using FACS analyses of brain homogenates after blood injection has documented an early influx of granulocytes and a delayed invasion of CD4+ and CD8+ T cells [34]. Xue and Del Bigio [36] compared the cellular immune reactions in 3 ICH rodent models, including autologous blood injection and collagenase injection. Interestingly, this study detected distinct differences in the kinetics and magnitude of neutrophile and CD8+ lymphocyte brain influx and microglial activation between the blood and the collagenase injection model in rats as blood injection resulted in earlier microglial activation and CD8+ T cell migration to the brain compared to collagenase-induced ICH.
We detected in this study profound differences in neuroinflammatory pathways between the two most common murine ICH models independent of ICH volume. In general, the autologous blood injection model induced more pronounced alterations in the analyzed immunological pathways in the hemorrhagic hemisphere-pro-inflammatory cytokines, anti-inflammatory cytokines and adhesion molecule expression-compared to the collagenase model. Additionally, only ICH induction by the autologous blood injection model (except for IL-6 expression at 3 h) induced significantly the expression of cytokines and adhesion molecules also in the contralateral, non-hemorrhagic hemisphere. Previous reports analyzing intracerebral cytokine expression in murine ICH models have used either autologous blood injection [38, 39] or collagenase-induced ICH [40, 41]. There, both models resulted in increased pro- and anti-inflammatory cytokine expression. However, the present study shows substantial differences in cytokine expression between ICH models.
Previous reports have documented an increase in cerebral ICAM-1 expression after ICH in the blood injection model [39, 42, 43]. We could reproduce these findings and detected additionally ICAM-1 induction in the collagenase model which was weaker compared to blood injection. VCAM-1 has been proposed as a therapeutic target in ischemic stroke and traumatic brain injury [23, 44]. This is the first study to characterize VCAM-1 expression after ICH. Surprisingly, we observed a significant increase in VCAM-1 expression in the blood injection but not the collagenase injection model. The relevance of this major discrepancy between the two ICH models on leukocyte invasion, neuroinflammation and outcome needs to be further investigated because of the key role of VCAM-1 in the inflammatory cascade after brain injury [28].
Developing new therapies for ICH is the ultimate goal of translational stroke research. So far more than 30 studies have investigated anti-inflammatory therapies targeting various cells and molecules in animal models of ICH [14, 45]. Experiments in these studies were performed in different species, used different methods to induce ICH, and produced different hematoma volumes in relation to the volume of the affected hemisphere. As long as the inflammatory cascades participating in the pathophysiology of human ICH are largely unknown, translational experiments have to take potential discrepancies of experimental models into account and should test hypotheses in different models.
Conflict of interest
The authors declare that they have no competing interests.
References
Ingall T: Stroke--incidence, mortality, morbidity and risk. J Insur Med 2004, 36: 143–152.
Broderick JP, Adams HP Jr, Barsan W, Feinberg W, Feldmann E, Grotta J, Kase C, Krieger D, Mayberg M, Tilley B, et al.: Guidelines for the management of spontaneous intracerebral hemorrhage: A statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke 1999, 30: 905–915. 10.1161/01.STR.30.4.905
Xi G, Keep RF, Hoff JT: Mechanisms of brain injury after intracerebral haemorrhage. Lancet Neurol 2006, 5: 53–63. 10.1016/S1474-4422(05)70283-0
MacLellan CL, Silasi G, Auriat AM, Colbourne F: Rodent models of intracerebral hemorrhage. Stroke 2010, 41: S95–98. 10.1161/STROKEAHA.110.594457
Strbian D, Durukan A, Tatlisumak T: Rodent models of hemorrhagic stroke. Curr Pharm Des 2008, 14: 352–358. 10.2174/138161208783497723
Andaluz N, Zuccarello M, Wagner KR: Experimental animal models of intracerebral hemorrhage. Neurosurg Clin N Am 2002, 13: 385–393. 10.1016/S1042-3680(02)00006-2
James ML, Warner DS, Laskowitz DT: Preclinical models of intracerebral hemorrhage: a translational perspective. Neurocrit Care 2008, 9: 139–152. 10.1007/s12028-007-9030-2
MacLellan CL, Silasi G, Poon CC, Edmundson CL, Buist R, Peeling J, Colbourne F: Intracerebral hemorrhage models in rat: comparing collagenase to blood infusion. J Cereb Blood Flow Metab 2008, 28: 516–525. 10.1038/sj.jcbfm.9600548
Adeoye O, Clark JF, Khatri P, Wagner KR, Zuccarello M, Pyne-Geithman GJ: Do Current Animal Models of Intracerebral Hemorrhage Mirror the Human Pathology? Translational Stroke Research 2011, 2: 17–25. 10.1007/s12975-010-0037-1
Diringer MN: Intracerebral hemorrhage: pathophysiology and management. Crit Care Med 1993, 21: 1591–1603. 10.1097/00003246-199310000-00032
Greve MW, Zink BJ: Pathophysiology of traumatic brain injury. Mt Sinai J Med 2009, 76: 97–104. 10.1002/msj.20104
Dirnagl U, Iadecola C, Moskowitz MA: Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci 1999, 22: 391–397. 10.1016/S0166-2236(99)01401-0
Wang J, Dore S: Inflammation after intracerebral hemorrhage. J Cereb Blood Flow Metab 2007, 27: 894–908.
Wang J: Preclinical and clinical research on inflammation after intracerebral hemorrhage. Prog Neurobiol 2010, 92: 463–477. 10.1016/j.pneurobio.2010.08.001
Illanes S, Zhou W, Heiland S, Markus Z, Veltkamp R: Kinetics of hematoma expansion in murine warfarin-associated intracerebral hemorrhage. Brain Res 2010, 1320: 135–142.
Foerch C, Arai K, Jin G, Park KP, Pallast S, van Leyen K, Lo EH: Experimental model of warfarin-associated intracerebral hemorrhage. Stroke 2008, 39: 3397–3404. 10.1161/STROKEAHA.108.517482
Illanes S, Liesz A, Sun L, Dalpke A, Zorn M, Veltkamp R: Hematoma size as major modulator of the cellular immune system after experimental intracerebral hemorrhage. Neurosci Lett 2011, 490: 170–174. 10.1016/j.neulet.2010.11.065
Rooker S, Jander S, Van Reempts J, Stoll G, Jorens PG, Borgers M, Verlooy J: Spatiotemporal pattern of neuroinflammation after impact-acceleration closed head injury in the rat. Mediators Inflamm 2006, 2006: 90123.
Barone FC, Arvin B, White RF, Miller A, Webb CL, Willette RN, Lysko PG, Feuerstein GZ: Tumor necrosis factor-alpha. A mediator of focal ischemic brain injury. Stroke 1997, 28: 1233–1244. 10.1161/01.STR.28.6.1233
Liesz A, Suri-Payer E, Veltkamp C, Doerr H, Sommer C, Rivest S, Giese T, Veltkamp R: Regulatory T cells are key cerebroprotective immunomodulators in acute experimental stroke. Nat Med 2009, 15: 192–199. 10.1038/nm.1927
Harden LM, du Plessis I, Poole S, Laburn HP: Interleukin (IL)-6 and IL-1 beta act synergistically within the brain to induce sickness behavior and fever in rats. Brain Behav Immun 2008, 22: 838–849. 10.1016/j.bbi.2007.12.006
Baird AE: The forgotten lymphocyte: immunity and stroke. Circulation 2006, 113: 2035–2036. 10.1161/CIRCULATIONAHA.105.620732
Liesz A, Zhou W, Mracsko E, Karcher S, Bauer H, Schwarting S, Sun L, Bruder D, Stegemann S, Cerwenka A, et al.: Inhibition of lymphocyte trafficking shields the brain against deleterious neuroinflammation after stroke. Brain 2011, 134: 704–720. 10.1093/brain/awr008
O'Garra A, Vieira PL, Vieira P, Goldfeld AE: IL-10-producing and naturally occurring CD4+ Tregs: limiting collateral damage. J Clin Invest 2004, 114: 1372–1378.
Strle K, Zhou JH, Shen WH, Broussard SR, Johnson RW, Freund GG, Dantzer R, Kelley KW: Interleukin-10 in the brain. Crit Rev Immunol 2001, 21: 427–449.
Allan SM, Rothwell NJ: Cytokines and acute neurodegeneration. Nat Rev Neurosci 2001, 2: 734–744. 10.1038/35094583
Jander S, Kraemer M, Schroeter M, Witte OW, Stoll G: Lymphocytic infiltration and expression of intercellular adhesion molecule-1 in photochemically induced ischemia of the rat cortex. J Cereb Blood Flow Metab 1995, 15: 42–51. 10.1038/jcbfm.1995.5
Engelhardt B: Molecular mechanisms involved in T cell migration across the blood-brain barrier. J Neural Transm 2006, 113: 477–485. 10.1007/s00702-005-0409-y
Ley K, Laudanna C, Cybulsky MI, Nourshargh S: Getting to the site of inflammation: the leukocyte adhesion cascade updated. Nat Rev Immunol 2007, 7: 678–689. 10.1038/nri2156
Lakhan SE, Kirchgessner A, Hofer M: Inflammatory mechanisms in ischemic stroke: therapeutic approaches. J Transl Med 2009, 7: 97. 10.1186/1479-5876-7-97
Arvin B, Neville LF, Barone FC, Feuerstein GZ: The role of inflammation and cytokines in brain injury. Neuroscience and Biobehavioral Reviews 1996, 20: 445–452. 10.1016/0149-7634(95)00026-7
Wang Q, Tang XN, Yenari MA: The inflammatory response in stroke. J Neuroimmunol 2006.
Gregersen R, Lambertsen K, Finsen B: Microglia and macrophages are the major source of tumor necrosis factor in permanent middle cerebral artery occlusion in mice. J Cereb Blood Flow Metab 2000, 20: 53–65. 10.1097/00004647-200001000-00009
Loftspring MC, McDole J, Lu A, Clark JF, Johnson AJ: Intracerebral hemorrhage leads to infiltration of several leukocyte populations with concomitant pathophysiological changes. J Cereb Blood Flow Metab 2009, 29: 137–143. 10.1038/jcbfm.2008.114
Xue M, Del Bigio MR: Intracerebral injection of autologous whole blood in rats: time course of inflammation and cell death. Neurosci Lett 2000, 283: 230–232. 10.1016/S0304-3940(00)00971-X
Xue M, Del Bigio MR: Comparison of brain cell death and inflammatory reaction in three models of intracerebral hemorrhage in adult rats. J Stroke Cerebrovasc Dis 2003, 12: 152–159. 10.1016/S1052-3057(03)00036-3
Wang J, Dore S: Heme oxygenase-1 exacerbates early brain injury after intracerebral haemorrhage. Brain 2007, 130: 1643–1652. 10.1093/brain/awm095
Zhao X, Zhang Y, Strong R, Zhang J, Grotta JC, Aronowski J: Distinct patterns of intracerebral hemorrhage-induced alterations in NF-kappaB subunit, iNOS, and COX-2 expression. J Neurochem 2007, 101: 652–663.
Zhang X, Li H, Hu S, Zhang L, Liu C, Zhu C, Liu R, Li C: Brain edema after intracerebral hemorrhage in rats: the role of inflammation. Neurol India 2006, 54: 402–407. 10.4103/0028-3886.28115
Wasserman JK, Zhu X, Schlichter LC: Evolution of the inflammatory response in the brain following intracerebral hemorrhage and effects of delayed minocycline treatment. Brain Res 2007, 1180: 140–154.
Lee ST, Chu K, Sinn DI, Jung KH, Kim EH, Kim SJ, Kim JM, Ko SY, Kim M, Roh JK: Erythropoietin reduces perihematomal inflammation and cell death with eNOS and STAT3 activations in experimental intracerebral hemorrhage. J Neurochem 2006, 96: 1728–1739. 10.1111/j.1471-4159.2006.03697.x
Gong C, Hoff JT, Keep RF: Acute inflammatory reaction following experimental intracerebral hemorrhage in rat. Brain Res 2000, 871: 57–65. 10.1016/S0006-8993(00)02427-6
Ma Q, Manaenko A, Khatibi NH, Chen W, Zhang JH, Tang J: Vascular adhesion protein-1 inhibition provides antiinflammatory protection after an intracerebral hemorrhagic stroke in mice. J Cereb Blood Flow Metab 31: 881–893.
Clausen F, Lorant T, Lewen A, Hillered L: T lymphocyte trafficking: a novel target for neuroprotection in traumatic brain injury. J Neurotrauma 2007, 24: 1295–1307. 10.1089/neu.2006.0258
Katsuki H: Exploring neuroprotective drug therapies for intracerebral hemorrhage. J Pharmacol Sci 2010, 114: 366–378. 10.1254/jphs.10R05CR
Acknowledgements
This study was supported by grants from the Else-Kröner Fresenius Stiftung and the German federal and state governments' Excellence initiative to R.V.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
AL designed and performed experiments, analyzed data, and wrote the manuscript; MM, WZ, SK and SI. performed experiments and analyzed data; RV. initiated and directed the entire study, designed experiments, analyzed data, and wrote the manuscript.
All authors have read and approved the final version of the manuscript.
Arthur Liesz, Moritz Middelhoff contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Liesz, A., Middelhoff, M., Zhou, W. et al. Comparison of humoral neuroinflammation and adhesion molecule expression in two models of experimental intracerebral hemorrhage. Exp & Trans Stroke Med 3, 11 (2011). https://doi.org/10.1186/2040-7378-3-11
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2040-7378-3-11