Abstract
Background
Oxaliplatin is a key drug in the treatment of colorectal cancer, but it causes severe peripheral neuropathy. We previously reported that oxaliplatin (4 mg/kg, i.p., twice a week) induces mechanical allodynia in the late phase in rats, and that spinal NR2B-containig N-methyl-D-aspartate (NMDA) receptors are involved in the oxaliplatin-induced mechanical allodynia. In the present study, we investigated the involvement of Ca2+/calmodulin dependent protein kinase II (CaMKII), which is a major intracellular protein kinase and is activated by NMDA receptor-mediated Ca2+ influx, in the oxaliplatin-induced mechanical allodynia in rats.
Results
An increase of CaMKII phosphorylation was found in the spinal cord (L4-6) of oxaliplatin-treated rats. This increased CaMKII phosphorylation was reversed by intrathecal injection of a selective CaMKII inhibitor KN-93 (50 nmol, i.t.) and a selective NR2B antagonist Ro 25-6981 (300 nmol, i.t.). Moreover, acute administration of KN-93 (50 nmol, i.t.) strongly reversed the oxaliplatin-induced mechanical allodynia in von Frey test, while it did not affect the oxaliplatin-induced cold hyperalgesia in acetone test. Similarly, oral administration of trifluoperazine (0.1 and 0.3 mg/kg, p.o.), which is an antipsychotic drug and inhibits calmodulin, reduced both mechanical allodynia and increased CaMKII phosphorylation. On the other hand, trifluoperazine at the effective dose (0.3 mg/kg) had no effect on the paw withdrawal threshold in intact rats. In addition, trifluoperazine at the same dose did not affect the motor coordination in rota-rod test in intact and oxaliplatin-treated rats.
Conclusions
These results suggest that CaMKII is involved in the oxaliplatin-induced mechanical allodynia, and trifluoperazine may be useful for the treatment of oxaliplatin-induced peripheral neuropathy in clinical setting.
Similar content being viewed by others
Background
Oxaliplatin, a platinum-based chemotherapeutic agent, has widely been used for colorectal cancer. However, oxaliplatin causes severe peripheral neuropathy. After multiple cycles, the patients develop a chronic neuropathy that is characterized by a sensory and motor dysfunction. This chronic neuropathy is a dose-limiting toxicity and a major clinical problem in oxaliplatin-based chemotherapy [1].
We previously reported that repeated administration of oxaliplatin induced cold hyperalgesia in the early phase and mechanical allodynia in the late phase in rats [2]. Recently, we reported that spinal NR2B-containing N-methyl-D-aspartate (NMDA) receptors are involved in the oxaliplatin-induced mechanical allodynia [3]. The NMDA receptor antagonists (MK-801 and memantine) and selective NR2B antagonists (Ro25-6981 and ifenprodil) reverse the oxaliplatin-induced mechanical allodynia. In addition, an expression of NR2B protein and mRNA in the rat spinal cord is increased by oxaliplatin on day 25 (late phase).
Activation of the NMDA receptors leads to an increase in Ca2+ influx into the cytosol. This increased Ca2+ influx initiates cascades of intracellular signaling events involving Ca2+ and various protein kinases [4]. Ca2+/calmodulin dependent protein kinase II (CaMKII) is a major intracellular protein kinase and is activated by Ca2+ signaling [5]. An increase in intracellular Ca2+ initially activates calmodulin by binding to its Ca2+-binding sites, and this interaction induces a change in the conformation of calmodulin. CaMKII is then switched to an activated state by exposure to Ca2+/calmodulin. Several studies showed that an increase of CaMKII activation in the spinal cord is involved in persistent pain by nerve injury [6–9] and inflammation [10, 11]. However, the role of CaMKII in the oxaliplatin-induced mechanical allodynia still remains unclear. In this study, we investigated the involvement of CaMKII in the oxaliplatin-induced mechanical allodynia, and explored novel useful therapeutic drugs for the oxaliplatin-induced neuropathy.
Results
Effects of KN-93 and KN-92 on Oxaliplatin-induced mechanical allodynia
Oxaliplatin (4 mg/kg, i.p., twice a week for 4 weeks) significantly reduced the paw withdrawal thresholds compared with the vehicle in the von Frey test on day 24 (p < 0.01, Figure 1). Before administration of KN-93, each group had equivalent paw withdrawal thresholds. The selective CaMKII inhibitor KN-93 (50 nmol, i.t.) completely reversed the reduction of paw withdrawal thresholds by oxaliplatin at 30 min after the administration (p < 0.05, Figure 1A). This effect of KN-93 was disappeared within 120 min after the administration. On the other hand, treatment of KN-92 (50 nmol, i.t.), the negative control of KN-93, had no effect on the oxaliplatin-induced mechanical allodynia (Figure 1B).
Effects of KN-93 and KN-92 on oxaliplatin-induced mechanical allodynia in the von Frey test. Rats were treated with oxaliplatin (4 mg/kg, i.p.) twice a week for 4 weeks (days 1, 2, 8, 9, 15, 16, 22 and 23). We confirmed the incidence of mechanical allodynia on day 24. We carried out the drug evaluation on the next day. KN-93 (10-50 nmol) or KN-92 (50 nmol) was administered intrathecally. The von Frey test was performed immediately before (0 min) and at 30, 60, 90 and 120 min after administration. KN-93 (50 nmol) significantly reversed oxaliplatin-induced mechanical allodynia (A). On the other hand, KN-92 (50 nmol) had no effect on the mechanical allodynia (B).Values are expressed as the mean ± SEM. of 5-8 animals. **p < 0.01 compared with vehicle (Student's t-test). †p < 0.05 compared with oxaliplatin alone (one-way ANOVA followed by Tukey-Kramer post-hoc test).
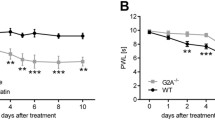
Effect of KN-93 on Oxaliplatin-induced cold hyperalgesia
Oxaliplatin (4 mg/kg, i.p. on days 1 and 2) significantly increased the number of withdrawal responses to cold stimulation by acetone spray on day 5 (p < 0.01, Figure 2). Before administration of KN-93, each group had equivalent number of withdrawal responses. KN-93 (50 nmol, i.t.) did not affect the increase in withdrawal responses by oxaliplatin.
Effect of KN-93 on oxaliplatin-induced cold hyperalgesia in the acetone test. Rats were treated with oxaliplatin (4 mg/kg, i.p.) on days 1 and 2. We confirmed the incidence of cold hyperalgesia on day 5 and we carried out the drug evaluation on the same day. KN-93 (10-50 nmol) was administered intrathecally. The acetone test was performed immediately before (0 min) and at 30, 60, 90 and 120 min after administration. KN-93 had no effect on oxaliplatin-induced cold hyperalgesia. Values are expressed as the mean ± SEM. of 7-8 animals. **p < 0.01 compared with vehicle (Student's t-test).
Effects of KN-93 and Ro 25-6981 on Oxaliplatin-induced increase in spinal CaMKII phosphorylation
To determine the effect of oxaliplatin on spinal CaMKII activity, we investigated the expression of CaMKII phosphorylation (pCaMKII). The pCaMKII in the spinal cord of oxaliplatin treated rats significantly increased compared with that of vehicle-treated rats on day 25 (p < 0.05, Figure 3). This increased pCaMKII was blocked by the selective CaMKII inhibitor KN-93 (50 nmol, i.t.) and the selective NR2B antagonist Ro 25-6981 (300 nmol, i.t.). (KN-93: p < 0.05; Ro 25-6981: p < 0.01, Figure 3).
Effects of KN-93 and Ro 25-6981 on oxaliplatin-induced increase in spinal CaMKII phosphorylation. Rats were treated with oxaliplatin (4 mg/kg, i.p.) twice a week for 4 weeks (days 1, 2, 8, 9, 15, 16, 22 and 23). The lumbar sections (L4-6) of the spinal cord were quickly removed at 30 min after administration of KN-93 (50 nmol, i.t.) or Ro 25-6981 (300 nmol, i.t.) on day 25. CaMKII phosphorylation (pCaMKII) in the lumbar sections of the spinal cord was determined by Western blotting. An increase of pCaMKII was found in the spinal cord of oxaliplatin-treated rats. Acute treatment with KN-93 (A) and Ro 25-6981 (B) reduced oxaliplatin-induced increase in the spinal pCaMKII. Values are expressed as mean ± SEM. of 6-8 animals. *p < 0.05 compared with vehicle, †p < 0.05, ††p < 0.01 compared with oxaliplatin alone (one-way ANOVA followed by Tukey-Kramer post-hoc test).
Effect of trifluoperazine on Oxaliplatin-induced mechanical allodynia and increase in CaMKII phosphorylation
Since trifluoperazine, an antipsychotic drug, inhibits calmodulin required for CaMKII phosphorylation [12], we tested the effect of this compound on the oxaliplatin-induced mechanical allodynia. Trifluoperazine (0.1 and 0.3 mg/kg, p.o.) significantly reduced the oxaliplatin-induced mechanical allodynia at 30 min (0.1 mg/kg: p < 0.05; 0.3 mg/kg: p < 0.01) and 120 min (0.3 mg/kg: p < 0.05) after the administration (Figure 4). On the other hand, trifluoperazine at the effective dose (0.3 mg/kg, p.o.) had no effect on the paw withdrawal thresholds in intact rats (Figure 5). Trifluoperazine (0.3 mg/kg, p.o.) strongly reduced the oxaliplatin-induced increase in spinal pCaMKII (p < 0.01, Figure 6).
Effect of trifluoperazine on oxaliplatin-induced mechanical allodynia in the von Frey test. Rats were treated with oxaliplatin (4 mg/kg, i.p.) twice a week for 4 weeks (days 1, 2, 8, 9, 15, 16, 22 and 23). We confirmed the incidence of mechanical allodynia on day 24. We carried out the drug evaluation on the next day. Trifluoperazine (0.05-0.3 mg/kg) was administered orally. The von Frey test was performed immediately before (0 min) and at 30, 120 and 240 min after administration of trifluoperazine. Trifluoperazine (0.1 and 0.3 mg/kg) significantly reversed oxaliplatin-induced mechanical allodynia. Values are expressed as the mean ± SEM. of 8 animals. **p < 0.01 compared with vehicle, †p < 0.05, ††p < 0.01 compared with oxaliplatin alone (one-way ANOVA followed by Tukey-Kramer post-hoc test).
Effect of trifluoperazine on mechanical nociceptive threshold in the von Frey test. Trifluoperazine (0.3 mg/kg) was administered orally in intact rats. The von Frey test was performed immediately before (0 min) and at 30, 120 and 240 min after administration of trifluoperazine. Trifluoperazine did not affect mechanical nociceptive threshold in intact rats. Values are expressed as the mean ± SEM. of 8 animals. No statistical difference was identified (one-way ANOVA followed by Tukey-Kramer post-hoc test).
Effect of trifluoperazine on oxaliplatin-induced increase of spinal CaMKII phosphorylation. Rats were treated with oxaliplatin (4 mg/kg, i.p.) twice a week for 4 weeks (days 1, 2, 8, 9, 15, 16, 22 and 23). The lumbar sections (L4-6) of the spinal cord were quickly removed at 30 min after administration of trifluoperazine (0.3 mg/kg, p.o.) on day 25. CaMKII phosphorylation (pCaMKII) in the lumbar sections of the spinal cord was determined by Western blotting. An increase of pCaMKII was found in the spinal cord of oxaliplatin-treated rats. Acute treatment with trifluoperazine reduced oxaliplatin-induced increase in the spinal pCaMKII. Values are expressed as mean ± SEM. of 6-7 animals. *p < 0.05 compared with vehicle, ††p < 0.01 compared with oxaliplatin alone by Tukey-Kramer post-hoc test.
Effect of trifluoperazine on motor coordination
We examined the influence of trifluoperazine on motor coordination in rota-rod test. At the time before (0 min) and 30 min after administration of trifluoperazine, there was no difference in the motor coordination among the groups-treated with distilled water, trifluoperazine 0.3 mg/kg or oxaliplatin + trifluoperazine 0.3 mg/kg (Figure 7).
Effect of trifluoperazine on motor coordination in the rota-rod test. Trifluoperazine (0.3 mg/kg) was administered orally in intact and oxaliplatin-treated rats. The rota-rod test was performed immediately before (0 min) and at 30 min after administration of trifluoperazine. Trifluoperazine did not affect motor coordination in intact and oxaliplatin-treated rats. Values are expressed as the mean ± SEM. of 8-11 animals. No statistical difference was identified (one-way ANOVA followed by Tukey-Kramer post-hoc test).
Discussion
In the present study, acute treatment of the CaMKII inhibitor KN-93 reversed the oxaliplatin-induced mechanical allodynia. KN-93 binds directly to calmodulin-binding site of CaMKII and inhibits the enzyme activity [13]. KN-93 also inhibits not only CaMKII but also L-type Ca2+ channels [14], and therefore there is possibility that the effect of KN-93 on the mechanical allodynia depends on blockade of Ca2+ channels. However, its structural analog KN-92, which does not inhibit CaMKII but blocks L-type Ca2+ channels' current, did not reverse the oxaliplatin-induced mechanical allodynia. Moreover, the expression of pCaMKII significantly increased in the spinal cord of oxaliplatin-treated rats on day 25, and this increase of pCaMKII was blocked by KN-93. On the other hand, KN-93 had no effect on the oxaliplatin-induced cold hyperalgesia on day 5. These results indicate that the spinal CaMKII is involved in the oxaliplatin-induced mechanical allodynia but not cold hyperalgesia.
Recently, we reported that repeated administration of oxaliplatin increased the expression of NR2B protein and mRNA in the rat spinal cord on day 25 (late phase) but not on day 5 (early phase), and Ro 25-6981 reversed the oxaliplatin-induced mechanical allodynia [3], suggesting the involvement of NR2B-containing NMDA receptors. These NMDA receptors have been reported to contribute to development of spinal hyperexcitability and chronic pain [15–17]. Ca2+ influx through activated NMDA receptors causes multiple intracellular changes including an activation of CaMKII [18, 19], and the CaMKII co-localizes with NR2B in the nociceptive regions such as the superficial dorsal horn [20]. Furthermore, NR2B mutation, which causes a lower increase in intracellular Ca2+ concentration by glutamate stimulation, leads to the reduction of spinal CaMKII phosphorylation in the neuropathic pain model [8, 9]. In our present study, we found that the increase of pCaMKII in the spinal cord of oxaliplatin-treated rats was blocked by Ro 25-6981, the selective NR2B antagonist. Therefore, oxaliplatin may induce the CaMKII activation by increasing in the expression of NR2B-containing NMDA receptors. These findings indicate an important role of CaMKII as a downstream of NR2B-containing NMDA receptors in pain states.
In this study, we confirmed an inhibition of CaMKII phosphorylation by trifluoperazine, which inhibits calmodulin required for CaMKII activation [12]. Furthermore, we found that trifluoperazine dose-dependently reduced the oxaliplatin-induced mechanical allodynia. Previous studies showed that trifluoperazine reversed complete Freund's adjuvant-induced inflammatory pain and spinal nerve ligation-induced neuropathic pain in mice [7, 11]. On the other hand, we observed that trifluoperazine at the effective dose (0.3 mg/kg) had no effect on the paw withdrawal thresholds in intact rats. In addition, trifluoperazine at the same dose did not affect the motor coordination in rota-rod test in intact and oxaliplatin-treated rats. Ye et al. [21] reported that trifluoperazine (0.125-0.5 mg/kg, i.p.) did not affect spontaneous locomotion in rats. Bhargava and Chandra [22] reported that ED50 (i.p.) of suppression of the conditioned response, an index of tranquilizing effect, is 0.58 mg/kg. Therefore, it is unlikely that the inhibitory effect of trifluoperazine on the oxaliplatin-induced pain behavior is due to its motor dysfunction or sedative effect. Taken together, the inhibitory effect of trifluoperazine on spinal CaMKII activity may be involved in the reduction of pain behavior, and low doses of trifluoperazine may be useful for the treatment of the oxaliplatin-induced neuropathy.
Conclusions
Our results indicate that repeated administration of oxaliplatin increases spinal CaMKII activity. This increase of CaMKII activation was reversed by intrathecal injection of the selective CaMKII inhibitor and the selective NR2B antagonist. This CaMKII activation may contribute to the incidence of mechanical allodynia. Furthermore, the selective CaMKII inhibitor and the selective NR2B antagonist reduced the oxaliplatin-induced pain behavior. In addition, trifluoperazine reduced the oxaliplatin-induced mechanical allodynia and CaMKII activation. These results suggest that inhibition of CaMKII or NMDA-CaMKII pathway provides a novel therapeutic target for the treatment of the oxaliplatin-induced peripheral neuropathy.
Methods
Animals
Male Sprague-Dawley rats weighing 200-250 g (Kyudo Co., Saga, Japan) were used in the present study. Animals were housed in groups of four to five per cage, with lights on from 7:00 to 19:00 h. Animals had free access to food and water in their home cages. All experiments were approved by the Experimental Animal Care and Use Committee of Kyushu University according to the National Institutes of Health guidelines, and we followed International Association for the Study of Pain (IASP) Committee for Research and Ethical Issues guidelines for animal research [23].
Drugs
Oxaliplatin (Elplat®) was obtained from Yakult Co., Ltd. (Tokyo, Japan). KN-93, Ro 25-6981 hydrochloride hydrate and trifluoperazine dihydrochloride were purchased from Sigma-Aldrich (Missouri, USA). KN-92 was purchased from Calbiochem (California, USA). Oxaliplatin was dissolved in 5% glucose solution. The vehicle-treated rats were injected with 5% glucose solution. KN-93, KN-92 and Ro 25-6981 were dissolved in 100% dimethyl sulfoxide (DMSO). Trifluoperazine was dissolved in distilled water. The doses of these drugs were chosen based on previous reports [2, 3, 7].
Production of neuropathy
Mechanical allodynia and cold hyperalgesia were induced according to the method described previously [24]. Oxaliplatin (4 mg/kg) or vehicle (5% glucose solution) was administered i.p. twice a week for 4 weeks (on days 1, 2, 8, 9, 15, 16, 22 and 23). The volume of vehicle or drug solution injected was 1 mL/kg for all drugs.
Behavioral studies
Behavioral test was performed blindly with respect to drug administration.
von Frey test for mechanical allodynia
The mechanical allodynia was assessed by von Frey test. Each rat was placed in a clear plastic box (20 × 17 × 13 cm) with a wire mesh floor and allowed to habituate for 30 min prior to testing. von Frey filaments (The Touch Test Sensory Evaluator Set; Linton Instrumentation, Norfolk, UK) ranging from 1- to 15-g bending force were applied to the midplantar skin of each hind paw six times, with each application held for 6 s. The paw withdrawal threshold was determined by a modified up-down method [25].
Acetone test for cold hyperalgesia
The cold hyperalgesia was assessed by acetone test. Each rat was placed in a clear plastic box (20 × 17 × 13 cm) with a wire mesh floor and allowed to habituate for 30 min prior to testing. Fifty microliters of acetone (Wako Pure Chemical Industries, Ltd., Osaka, Japan) was sprayed onto the plantar skin of each hind paw 3 times, and the number of withdrawal responses was counted for 40 s from the start of the acetone spray.
Rota-rod test for motor coordination
The rota-rod test was performed to investigate the change of motor coordination. Rats were placed on a rotating rod (Muromachi Kikai Co., Ltd., Tokyo, Japan) and the latency to falling was measured for up to 2 min according to the method described previously [26]. The test was performed three times, and the rotating speed was 10 rpm.
Effects of KN-93, KN-92 and trifluoperazine on Oxaliplatin-induced mechanical allodynia
We confirmed the incidence of mechanical allodynia in the von Frey test on day 24. We carried out the drug evaluation on the next day. KN-93 (10-50 nmol) or KN-92 (50 nmol) was administered i.t. injection by direct lumbar puncture in a volume of 50 µL. The von Frey test was performed immediately before (0 min) and at 30, 60, 90 and 120 min after administration of the drugs. Trifluoperazine (0.05-0.3 mg/kg) was administered p.o. The von Frey test was performed immediately before (0 min) and at 30, 120 and 240 min after oral administration of trifluoperazine.
Effect of KN-93 on Oxaliplatin-induced cold hyperalgesia
We confirmed the incidence of cold hyperalgesia in the acetone test on day 5. KN-93 (10-50 nmol) was administered i.t. injection by direct lumbar puncture in a volume of 50 µL. The acetone test was performed immediately before (0 min) and at 30, 60, 90 and 120 min after administration of the drug.
Effect of trifluoperazine on mechanical nociceptive threshold
We investigated the effect of trifluoperazine on the mechanical nociceptive threshold in the von Frey test. Trifluoperazine (0.3 mg/kg) was administered p.o. in intact rats. The von Frey test was performed immediately before (0 min) and at 30, 120 and 240 min after oral administration of trifluoperazine.
Effect of trifluoperazine on motor coordination
We investigated the effect of trifluoperazine on the motor coordination in the rota-rod test. Trifluoperazine (0.3 mg/kg) was administered p.o. in intact and oxaliplatin-treated rats. The rota-rod test was performed immediately before (0 min) and at 30 min after oral administration of trifluoperazine.
Western blotting analysis
The lumbar sections (L4-6) of the spinal cord were quickly removed at 30 min after administration of KN-93 (50 nmol, i.t.), Ro 25-6981 (300 nmol, i.t.) or trifluoperazine (0.3 mg/kg, p.o.) on day 25. The tissues were homogenized in a solubilization buffer containing 20 mM Tris-HCl (pH 7.4, 2 mM EDTA, 0.5 mM EGTA, 10 mM NaF, 1 mM Na3VO4, 1 mM PMSF, 0.32 M Sucrose, 2 mg/ml aprotinine, 2 mg/ml leupeptin), and the homogenates were subjected to 12.5% SDS-PAGE, and proteins were transferred electrophoretically to PVDF membranes. The membranes were blocked in Tris-buffered saline Tween-20 (TBST) containing 5% BSA (Sigma-Aldrich) for an additional 1 h at room temperature with agitation. The membrane was incubated overnight at 4°C with mouse polyclonal anti-CaMKIIα antibody or rabbit polyclonal anti-(Thr286)pCaMKII (1:5000; Santa Cruz Biotechnology, California, USA) and then incubated for 1 h with corresponding horseradish peroxidase conjugate secondary antibodies (1:5000; Jackson Immuno Research Laboratories, Inc., PA, USA). The immunoreactivity was detected using Enhanced Chemiluminescence (Perkin Elmer, Massachusetts, USA). Ratios of the optical densities of pCaMKII to those of CaMKII were calculated for each sample.
Data analysis
Values were expressed as the means ± SEM. The values were analyzed by the Student's t-test or one-way analysis of variance (ANOVA) followed by the Tukey-Kramer post-hoc test (StatView; Abacus Concepts, Berkely, CA, USA) to determine differences among the groups. A p value of less than 0.05 is considered as statistically significant.
References
Saif MW, Reardon J: Management of oxaliplatin-induced peripheral neuropathy. Ther Clin Risk Manag 2005, 1: 249–258.
Sakurai M, Egashira N, Kawashiri T, Yano T, Ikesue H, Oishi R: Oxaliplatin-induced neuropathy in the rat: Involvement of oxalate in cold hyperalgesia but not mechanical allodynia. Pain 2009, 147: 165–174. 10.1016/j.pain.2009.09.003
Mihara Y, Egashira N, Sada H, Kawashiri T, Ushio S, Yano T, Ikesue H, Oishi R: Involvement of spinal NR2B-containing NMDA receptors in oxaliplatin-induced mechanical allodynia in rats. Mol Pain 2011, 7: 8. 10.1186/1744-8069-7-8
Womack MD, MacDermott AB, Jessell TM: Sensory transmitters regulate intracellular calcium in dorsal horn neurons. Nature 1988, 334: 351–353. 10.1038/334351a0
Lisman J, Schulman H, Cline H: The molecular basis of CaMKII function in synaptic and behavioural memory. Nat Rev Neurosci 2002, 3: 175–190. 10.1038/nrn753
Dai Y, Wang H, Ogawa A, Yamanaka H, Obata K, Tokunaga A, Noguchi K: Ca2+ /calmodulin-dependent protein kinase II in the spinal cord contributes to neuropathic pain in a rat model of mononeuropathy. Eur J Neurosci 2005, 21: 2467–2474. 10.1111/j.1460-9568.2005.04091.x
Chen Y, Luo F, Yang C, Kirkmire CM, Wang ZJ: Acute inhibition of Ca2+ /calmodulin-dependent protein kinase II reverses experimental neuropathic pain in mice. J Pharmacol Exp Ther 2009, 330: 650–659. 10.1124/jpet.109.152165
Katano T, Nakazawa T, Nakatsuka T, Watanabe M, Yamamoto T, Ito S: Involvement of spinal phosphorylation cascade of Tyr1472-NR2B, Thr286-CaMKII, and Ser831-GluR1 in neuropathic pain. Neuropharmacology 2010, 60: 609–616.
Matsumura S, Kunori S, Mabuchi T, Katano T, Nakazawa T, Abe T, Watanabe M, Yamamoto T, Okuda-Ashitaka E, Ito S: Impairment of CaMKII activation and attenuation of neuropathic pain in mice lacking NR2B phosphorylated at Tyr1472. Eur J Neurosci 2010, 32: 798–810. 10.1111/j.1460-9568.2010.07348.x
Choi SS, Seo YJ, Shim EJ, Kwon MS, Lee JY, Ham YO, Suh HW: Involvement of phosphorylated Ca2+ /calmodulin-dependent protein kinase II and phosphorylated extracellular signal-regulated protein in the mouse formalin pain model. Brain Res 2006, 1108: 28–38. 10.1016/j.brainres.2006.06.048
Luo F, Yang C, Chen Y, Shukla P, Tang L, Wang LX, Wang ZJ: Reversal of chronic inflammatory pain by acute inhibition of Ca2+ /calmodulin-dependent protein kinase II. J Pharmacol Exp Ther 2008, 325: 267–275. 10.1124/jpet.107.132167
Prozialeck WC, Weiss B: Inhibition of calmodulin by phenothiazines and related drugs: structure-activity relationships. J Pharmacol Exp Ther 1982, 222: 509–516.
Sumi M, Kiuchi K, Ishikawa T, Ishii A, Hagiwara M, Nagatsu T, Hidaka H: The newly synthesized selective Ca2+ /calmodulin dependent protein kinase II inhibitor KN-93 reduces dopamine contents in PC12h cells. Biochem Biophys Res Commun 1991, 181: 968–975. 10.1016/0006-291X(91)92031-E
Gao L, Blair LA, Marshall J: CaMKII-independent effects of KN93 and its inactive analog KN92: reversible inhibition of L-type calcium channels. Biochem Biophys Res Commun 2006, 345: 1606–1610. 10.1016/j.bbrc.2006.05.066
Qu XX, Cai J, Li MJ, Chi YN, Liao FF, Liu FY, Wan Y, Han JS, Xing GG: Role of the spinal cord NR2B-containing NMDA receptors in the development of neuropathic pain. Exp Neurol 2009, 215: 298–307. 10.1016/j.expneurol.2008.10.018
Abe T, Matsumura S, Katano T, Mabuchi T, Takagi K, Xu L, Yamamoto A, Hattori K, Yagi T, Watanabe M, Nakazawa T, Yamamoto T, Mishina M, Nakai Y, Ito S: Fyn kinase-mediated phosphorylation of NMDA receptor NR2B subunit at Tyr1472 is essential for maintenance of neuropathic pain. Eur J Neurosci 2005, 22: 1445–1454. 10.1111/j.1460-9568.2005.04340.x
Wilson JA, Garry EM, Anderson HA, Rosie R, Colvin LA, Mitchell R, Fleetwood-Walker SM: NMDA receptor antagonist treatment at the time of nerve injury prevents injury-induced changes in spinal NR1 and NR2B subunit expression and increases the sensitivity of residual pain behaviours to subsequently administered NMDA receptor antagonists. Pain 2005, 117: 421–432. 10.1016/j.pain.2005.07.005
Hardingham GE, Bading H: Synaptic versus extrasynaptic NMDA receptor signalling: implications for neurodegenerative disorders. Nat Rev Neurosci 2010, 11: 682–696. 10.1038/nrn2911
Yashiro K, Philpot BD: Regulation of NMDA receptor subunit expression and its implications for LTD, LTP, and metaplasticity. Neuropharmacology 2008, 55: 1081–1094. 10.1016/j.neuropharm.2008.07.046
Petrenko AB, Yamakura T, Baba H, Shimoji K: The role of N-methyl-D-aspartate (NMDA) receptors in pain: a review. Anesth Analg 2003, 97: 1108–1116.
Ye XF, Lu Y, Zhang P, Liang JH: Calmodulin inhibitor trifluoperazine attenuates the development and expression of morphine-induced conditioned place preference in rats. Eur J Pharmacol 2004, 486: 265–271. 10.1016/j.ejphar.2004.01.002
Bhargava KP, Chandra OM: Tranquillizing and hypotensive activities of twelve phenothiazines. Br J Pharmacol Chemother 1964, 22: 154–161.
Zimmermann M: Ethical guidelines for investigations of experimental pain in conscious animals. Pain 1983, 16: 109–110. 10.1016/0304-3959(83)90201-4
Egashira N, Hirakawa S, Kawashiri T, Yano T, Ikesue H, Oishi R: Mexiletine reverses oxaliplatin-induced neuropathic pain in rats. J Pharmacol Sci 2010, 112: 473–476. 10.1254/jphs.10012SC
Kawashiri T, Egashira N, Watanabe H, Ikegami Y, Hirakawa S, Mihara Y, Yano T, Ikesue H, Oishi R: Prevention of oxaliplatin-induced mechanical allodynia and neurodegeneration by neurotropin in the rat model. Eur J Pain 2011, 15: 344–350. 10.1016/j.ejpain.2010.08.006
Egashira N, Tanoue A, Higashihara F, Mishima K, Fukue Y, Takano Y, Tsujimoto G, Iwasaki K, Fujiwara M: V1a receptor knockout mice exhibit impairment of spatial memory in an eight-arm radial maze. Neurosci Lett 2004, 356: 195–198. 10.1016/j.neulet.2003.11.050
Acknowledgements
Part of this study was supported by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (Nos. 21590285 and 22590242). We appreciate the technical support from the Research Support Center, Graduate School of Medical Sciences, Kyushu University.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
NE and TK are responsible for experimental design. MS, SU and HS are responsible for performance of behavioral tests. MS, SU, SY, HS and KM are responsible for performance of Western blotting. NE, MS and RO are responsible for writing the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Shirahama, M., Ushio, S., Egashira, N. et al. Inhibition of Ca2+/Calmodulin-dependent protein kinase II reverses oxaliplatin-induced mechanical allodynia in Rats. Mol Pain 8, 26 (2012). https://doi.org/10.1186/1744-8069-8-26
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1744-8069-8-26