Abstract
Background
Oxaliplatin is a platinum-based chemotherapy drug characterized by the development of acute and chronic peripheral neuropathies. The chronic neuropathy is a dose-limiting toxicity. We previously reported that repeated administration of oxaliplatin induced cold hyperalgesia in the early phase and mechanical allodynia in the late phase in rats. In the present study, we investigated the involvement of NR2B-containing N-methyl-D-aspartate (NMDA) receptors in oxaliplatin-induced mechanical allodynia in rats.
Results
Repeated administration of oxaliplatin (4 mg/kg, i.p., twice a week) caused mechanical allodynia in the fourth week, which was reversed by intrathecal injection of MK-801 (10 nmol) and memantine (1 μmol), NMDA receptor antagonists. Similarly, selective NR2B antagonists Ro25-6981 (300 nmol, i.t.) and ifenprodil (50 mg/kg, p.o.) significantly attenuated the oxaliplatin-induced pain behavior. In addition, the expression of NR2B protein and mRNA in the rat spinal cord was increased by oxaliplatin on Day 25 (late phase) but not on Day 5 (early phase). Moreover, we examined the involvement of nitric oxide synthase (NOS) as a downstream target of NMDA receptor. L-NAME, a non-selective NOS inhibitor, and 7-nitroindazole, a neuronal NOS (nNOS) inhibitor, significantly suppressed the oxaliplatin-induced pain behavior. The intensity of NADPH diaphorase staining, a histochemical marker for NOS, in the superficial layer of spinal dorsal horn was obviously increased by oxaliplatin, and this increased intensity was reversed by intrathecal injection of Ro25-6981.
Conclusion
These results indicated that spinal NR2B-containing NMDA receptors are involved in the oxaliplatin-induced mechanical allodynia.
Similar content being viewed by others
Background
Glutamate is a major excitatory transmitter in the spinal cord and N-methyl-D-aspartate (NMDA) receptors are known to be involved in the painful neuropathy [1, 2]. The NMDA receptor antagonist inhibits the pain hypersensitivity in chronic constriction injury (CCI) model. Moreover, the expression of spinal NR2B-containing NMDA receptors is increased with the pain hypersensitivity induced by CCI or chronic compression of the dorsal root ganglia (CCD) [3–6]. Selective NR2B antagonists inhibit mechanical allodynia without causing motor dysfunction in CCI, CCD and spinal nerve-ligated (SNL) neuropathic models [5–8]. In addition, the NR2B subunits are localized to the superficial dorsal horn of the spinal cord [7, 9], suggesting a possible involvement in pain transmission. Thus, the NR2B-containing NMDA receptors may play an important role in the neuropathic pain.
Nitric oxide synthase (NOS) as a downstream target of NMDA receptor also contributes greatly to the incidence of neuropathic pain. In the rat CCI model of neuropathic pain, intrathecal injection of non-selective NOS inhibitor L-NG-nitro-arginine methyl ester (L-NAME) reverses the persistent thermal hyperalgesia [10]. Furthermore, a close correlation between neuronal NOS (nNOS) and neuropathic pain has been documented in CCI model [11].
Oxaliplatin, a third-generation platinum-based chemotherapy drug, has widely been used as a key drug in the treatment of colorectal cancer. However, oxaliplatin causes severe acute and chronic peripheral neuropathies. The acute neuropathy includes acral paresthesias and dysesthesia triggered or enhanced by exposure to cold, and it appears soon after administration [12]. After multiple cycles the patients develop the chronic neuropathy that is characterized by a sensory and motor dysfunction. This chronic neuropathy is a dose-limiting toxicity and a major clinical problem in oxaliplatin chemotherapy [13].
Recently, we reported that repeated administration of oxaliplatin induced cold hyperalgesia in the early phase and mechanical allodynia in the late phase in rats [14]. Oxaliplatin is metabolized to oxalate and dichloro(1,2-diaminocyclohexane)platinum [Pt(dach)Cl2] [15]. We demonstrated that oxalate and platinum metabolite are involved in the cold hyperalgesia and mechanical allodynia, respectively [14]. Oxalate alters voltage-gated Na+ channels [16] and its effect may be involved in the cold hyperalgesia. On the other hand, the mechanical allodynia may be due to the peripheral nerve injury by platinum metabolite. However, whether the NR2B-containing NMDA receptors are involved still remains largely unclear. In the present study, we investigated the involvement of NR2B-containing NMDA receptors in the oxaliplatin-induced mechanical allodynia in rats.
Results
Effects of NMDA receptor antagonists on oxaliplatin-induced mechanical allodynia
Oxaliplatin (4 mg/kg, i.p., twice a week for 4 weeks) significantly reduced the paw withdrawal thresholds compared with the vehicle in the von Frey test on Day 24 (P < 0.01, Figure 1). Acute administration of a NMDA receptor antagonist MK-801 (10 nmol, i.t.) completely reversed the reduction of paw withdrawal threshold by oxaliplatin at 30 min after administration (P < 0.05, Figure 1A). Similarly, acute administration of another NMDA receptor antagonist memantine (1 μmol, i.t.) completely reversed the reduction of paw withdrawal threshold by oxaliplatin at 30 min after administration (P < 0.05, Figure 1B). These effects of MK-801 and memantine disappeared by 120 min after administration. In addition, MK-801 (10 nmol, i.t.) and memantine (1 μmol, i.t.) had no effect on the paw withdrawal thresholds in intact rats (data not shown).
Effects of MK-801 (A) and memantine (B) on oxaliplatin-induced mechanical allodynia in the von Frey test. Oxaliplatin (4 mg/kg) was administered i.p. twice a week for 4 weeks (Days 1, 2, 8, 9, 15, 16, 22 and 23). We confirmed the incidence of mechanical allodynia on Day 24. We carried out the drug evaluation on the next day. MK-801 (1-10 nmol/body) and memantine (0.1-1 μmol/body) were administered intrathecally. The von Frey test was performed immediately before (0 min) and at 30, 60, 90 and 120 min after administration. Values are expressed as mean ± SEM of 6-10 animals. †† P < 0.01 compared with vehicle, *P < 0.05 compared with oxaliplatin alone.
Effects of NR2B antagonists on oxaliplatin-induced mechanical allodynia
Acute administration of a selective NR2B antagonist Ro 25-6981 (300 nmol, i.t.) significantly inhibited the reduction of paw withdrawal threshold by oxaliplatin at 30 and 60 min after administration (P < 0.01: 30 min, P < 0.05: 60 min, Figure 2A). Similarly, acute administration of another NR2B antagonist ifenprodil (50 mg/kg, p.o.) significantly inhibited the reduction of paw withdrawal threshold by oxaliplatin at 30 and 60 min after administration (P < 0.01: 30 min, P < 0.05: 60 min, Figure 2B). These effects of Ro 25-6981 and ifenprodil disappeared by 120 min after administration. In addition, Ro 25-6981 (300 nmol, i.t.) and ifenprodil (50 mg/kg, p.o.) had no effect on the paw withdrawal thresholds in intact rats (data not shown).
Effects of Ro 25-6981 (A) and ifenprodil (B) on oxaliplatin-induced mechanical allodynia in the von Frey test. Oxaliplatin (4 mg/kg) was administered i.p. twice a week for 4 weeks (Days 1, 2, 8, 9, 15, 16, 22 and 23). We confirmed the incidence of mechanical allodynia on Day 24. We carried out the drug evaluation on the next day. Ro 25-6981 (30-300 nmol/body) was administered intrathecally. Ifenprodil (10-50 mg/kg) was administered orally. The von Frey test was performed immediately before (0 min) and at 30, 60, 90 and 120 min after administration. Values are expressed as mean ± SEM of 6-7 animals. †† P < 0.01 compared with vehicle, *P < 0.05, **P < 0.01 compared with oxaliplatin alone.
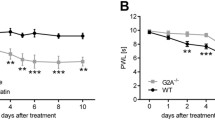
Changes of NR2B protein and mRNA in the spinal cord in oxaliplatin-treated rats
NR2B expression was examined by Western blot and polymerase chain reaction (PCR) analysis on homogenates of the spinal cord from rats. The results of Western blot and PCR showed that NR2B protein and mRNA levels in the spinal cord of oxaliplatin-treated rats significantly increased compared with that of vehicle-treated rats on Day 25 (P < 0.01, Figures 3C, D). On the other hand, oxaliplatin caused no change in NR2B protein and mRNA levels in the spinal cord on Day 5 (Figures 3A, B).
Changes in the NR2B protein (A, C) and mRNA (B, D) levels in the spinal cord in oxaliplatin-treated rats. Oxaliplatin (4 mg/kg) was administered i.p. twice a week for 1 (Days 1 and 2) or 4 weeks (Days 1, 2, 8, 9, 15, 16, 22 and 23). Western blot and PCR were performed to measure NR2B expression at the time points of Days 5 (A, B) and 25 (C, D) in the L4-6 spinal cord. Values are expressed as mean ± SEM of 6-9 animals. **P < 0.01 compared with vehicle.
Effects of NOS inhibitors on oxaliplatin-induced mechanical allodynia
Acute administration of a non-selective NOS inhibitor L-NAME (300 μg, i.t.) completely reversed the reduction of paw withdrawal threshold by oxaliplatin at 30 min after administration (P < 0.05, Figure 4A). Similarly, acute administration of an nNOS inhibitor 7-nitroindazole (100 μg, i.t.) significantly inhibited the reduction of paw withdrawal threshold by oxaliplatin at 30 min after administration (P < 0.05, Figure 4B). These effects of L-NAME and 7-nitroindazole disappeared by 120 min after administration. In addition, L-NAME (300 μg, i.t.) and 7-nitroindazol (100 μg, i.t.) had no effect on the paw withdrawal thresholds in intact rats (data not shown).
Effects of L-NAME (A) and 7-nitroindazole (B) on oxaliplatin-induced mechanical allodynia in the von Frey test. Oxaliplatin (4 mg/kg) was administered i.p. twice a week for 4 weeks (Days 1, 2, 8, 9, 15, 16, 22 and 23). We confirmed the incidence of mechanical allodynia on Day 24. We carried out the drug evaluation on the next day. L-NAME (30-300 μg/body) and 7-nitroindazole (10-100 μg/body) were administered intrathecally. The von Frey test was performed immediately before (0 min) and at 30, 60, 90 and 120 min after administration. Values are expressed as mean ± SEM of 6-10 animals. †† P < 0.01 compared with vehicle, *P < 0.05 compared with oxaliplatin alone.
Change of NOS activity in the spinal cord of oxaliplatin-treated rats
To evaluate change of NOS activity in oxaliplatin-induced mechanical allodynia, we carried out the NADPH diaphorase staining, a histochemical marker for NOS, in rat spinal cord sections. The results of NADPH diaphorase histochemistry revealed that the intensity of NADPH diaphorase staining (blue staining) obviously increased in the superficial layer of spinal dorsal horn in oxaliplatin-treated rats on Day 25 (Figure 5). Moreover, this increased intensity was reversed by intrathecal injection of Ro 25-6981 (300 nmol).
Typical photomicrographs representing NOS histochemistry staining of neurons in the spinal cord. Oxaliplatin (4 mg/kg) was administered i.p. twice a week for 4 weeks (Days 1, 2, 8, 9, 15, 16, 22 and 23). On Day 25, Ro 25-6981 (300 nmol/body) was administered intrathecally, and the L4-6 spinal cord was removed 30 min after administration. NADPH diaphorase staining was performed to confirm NOS activity. The blue staining shows NADPH diaphorase staining. Spinal slices (30 μm) were prepared from rats treated with vehicle (A), oxaliplatin alone (B), and oxaliplatin and Ro 25-6981 (C). Scale bar, 200 μm.
Discussion
In this study, NMDA receptor antagonists completely reverse the oxaliplatin-induced mechanical allodynia when administered after the development of neuropathy. Similarly, selective NR2B antagonists significantly inhibited the oxaliplatin-induced mechanical allodynia. Moreover, the expression of NR2B protein and mRNA in the spinal cord increased in the oxaliplatin-treated rats on Day 25 (late phase) but not on Day 5 (early phase). Oxaliplatin (4 mg/kg, i.p., twice a week) induces cold hyperalgesia in the early phase and mechanical allodynia in the late phase [14]. These findings suggest that the up-regulation of spinal NR2B-containing NMDA receptors is involved in the incidence of mechanical allodynia by repeated administration of oxaliplatin.
To investigate whether spinal cord NOS as the downstream target of NMDA receptor contributes to the incidence of mechanical allodynia, we examined the effects of NOS inhibitors on the oxaliplatin-induced mechanical allodynia. Intrathecal injection of L-NAME, a non-selective NOS inhibitor, and 7-nitroindazole, a selective nNOS inhibitor, inhibited the pain behavior, suggesting that NOS especially nNOS is involved in the oxaliplatin-induced mechanical allodynia. This is further supported by the finding that the intensity of NADPH diaphorase staining in the rat spinal dorsal horn was increased by repeated administration of oxaliplatin, and that this increased intensity was reversed by intrathecal injection of Ro25-6981, which attenuated the oxaliplatin-induced pain behavior. Marked increase of nNOS expression in the dorsal root ganglia (DRG) and spinal cord contributes to spinal sensory processing in CCI model [11]. More recent experiments with selective NOS inhibitors and in NOS-deficient mice revealed the nNOS to be the most important NO-producing enzyme in the spinal cord during the development and maintenance of neuropathic pain in SNL model [17]. In mice with neuropathic pain by transection of spinal nerve, an increase in nNOS activity is visualized in the superficial dorsal horn by NADPH diaphorase histochemistry [18]. Taken together, these findings suggest that NOS especially nNOS contributes to the incidence of oxaliplatin-induced mechanical allodynia.
Interestingly, our results show that both oxaliplatin-induced pain behavior and increase of NOS activity are reversed by intrathecal injection of Ro25-6981, a selective NR2B antagonist. Phosphorylation of NMDA receptor NR2B subunits increases nNOS activity in the superficial dorsal horn of mice with neuropathic pain [18]. The activation of NMDA receptor also induces glutamate release through NOS activity [19]. Thus, the NMDA receptor and NOS comprise a local circuit that amplifies the signal of pain transmission. If sustained production of these factors by repeated administration of oxaliplatin is required for maintenance of mechanical allodynia, and if their treatment-induced increase is likely to cause persistence of pain, blockade of this circuit by the NR2B antagonist would likely reduce pain excitatory neurotransmission in the spinal cord. All of these findings indicate that NR2B antagonists have analgesic effects on the oxaliplatin-induced mechanical allodynia at the spinal level.
Non-competitive NMDA receptor antagonists are used as analgesics in clinical practice, although undesirable side effects limit their utility [20]. In contrast, the restricted distribution of NR2B receptor makes them promising candidates as targets of side effect-free analgesic drugs [21]. Indeed, ifenprodil, traxoprodil (CP-101606) and Ro25-6981 are effective in inflammatory and/or neuropathic pain models in animals at doses that are not accompanied by motor effects [8, 22]. In addition, ifenprodil has been used as analgesic adjuvant in clinical settings. In this study, our results showed that NMDA receptor antagonists, selective NR2B antagonists and NOS inhibitors at the effective dose had no effect on pain behavior in intact rats. Therefore, the ameliorative effects of these drugs were not attributable to non-specific sedative effects or a deficit of motor function, suggesting that the reduced pain behavior reflects a therapeutic effect on oxaliplatin-induced mechanical allodynia. Novel strategies involving NR2B antagonists may be a useful alternative or adjunct therapy for oxaliplatin-induced peripheral neuropathy.
Conclusion
Our results indicate that repeated administration of oxaliplatin induces NR2B and NOS up-regulation in the spinal cord. This up-regulation may contribute to the incidence of mechanical allodynia. Furthermore, NMDA receptor antagonists, selective NR2B antagonists and NOS inhibitors remarkably attenuated the oxaliplatin-induced pain behavior. In addition, the selective NR2B antagonist inhibited the increase of NOS activity in the spinal cord. These results suggest that activation of the NMDA-NOS pathway contributes to the incidence of mechanical allodynia induced by repeated administration of oxaliplatin.
Methods
Animals
Male Sprague-Dawley rats weighing 200-250 g (Kyudo Co., Saga, Japan) were used in the present study. Rats were housed in groups of four to five per cage, with lights on from 7:00 to 19:00 h. Animals had free access to food and water in their home cages. All experiments were approved by the Experimental Animal Care and Use Committee of Kyushu University according to the National Institutes of Health guidelines, and we followed International Association for the Study of Pain (IASP) Committee for Research and Ethical Issues guidelines for animal research [23].
Production of neuropathy
Mechanical allodynia was induced according to the method described previously [24]. Oxaliplatin (Elplat®) was obtained from Yakult Co., Ltd. (Tokyo, Japan). Oxaliplatin was dissolved in 5% glucose solution. The vehicle-treated rats were injected with 5% glucose solution. Oxaliplatin (4 mg/kg) or vehicle (5% glucose) was injected i.p. in volumes of 1 mL/kg twice a week for 4 weeks.
von Frey test
The mechanical allodynia was assessed by von Frey test. Each rat was placed in a clear plastic box (20 × 17 × 13 cm) with a wire mesh floor and allowed to habituate for 30 min prior to testing. von Frey filaments (The Touch Test Sensory Evaluator Set; Linton Instrumentation, Norfolk, UK) ranging 1-15 g bending force were applied to the midplantar skin of each hind paw with each application held for 6 s. The paw withdrawal threshold was determined by a modified up-down method [25].
Pharmacological studies
We confirmed the incidence of mechanical allodynia on Day 24. We carried out the drug evaluation on the next day. The von Frey test was performed immediately before (0 min) and at 30, 60, 90, and 120 min after administration. (+)-MK-801 maleate (Wako Pure Chemical Industries, Ltd., Osaka, Japan), memantine hydrochloride (Alexis Biochemicals, San Diego, CA, USA) and L-NAME (Sigma-Aldrich, Missouri, USA) were dissolved in saline and administered i.t. Ro 25-6981 (Sigma-Aldrich) and 7-nitroindazole were dissolved in 100% dimethyl sulfoxide (DMSO) and administered i.t. Ifenprodil tartrate (Wako Pure Chemical Industries, Ltd.) was suspended in 5% gum arabic solution and administered orally (p.o.). The doses of these drugs were chosen based on previous reports [8, 26–28]. Behavioral test was performed blindly with respect to drug administration.
Western blotting
To investigate the functional changes in protein levels of NR2B, the L4-6 spinal cord was quickly removed on Days 5 and 25. The tissues were homogenized in a solubilization buffer containing 20 mM Tris-HCl (pH7.4, 2 mM EDTA, 0.5 mM EGTA, 10 mM NaF, 1 mM Na3VO4, 1 mM PMSF, 0.32 M Sucrose, 2 mg/ml aprotinine, 2 mg/ml leupeptin), and the homogenates were subjected to 6% SDS-PAGE, and proteins were transferred electrophoretically to PVDF membranes. The membranes were blocked in Tris-buffered saline Tween-20 (TBST) containing 5% BSA (Sigma-Aldrich) for an additional 1 h at room temperature with agitation. The membrane was incubated overnight at 4°C with rabbit polyclonal NR2B antibody (1:5000; Upstate Biotech, NY, USA) and then incubated for 1 h with anti-rabbit IgG horseradish peroxidase (1:5000; Jackson Immuno Research Laboratories, Inc., PA, USA). The immunoreactivity was detected using Enhanced Chemiluminescence (Perkin Elmer, Massachusetts, USA).
Reverse transcriptase-polymerase chain reaction (RT-PCR)
To investigate the functional changes in mRNA levels of NR2B, the L4-6 spinal cord was quickly removed on Days 5 and 25. mRNA was isolated using PolyATtract® System 1000 (Promega, Corp., Wisconsin, USA). cDNA was synthesized using PrimScript® 1st strand cDNA Synthesis Kit (TaKaRa Bio, Inc., Shiga, Japan). PCR was carried out with Gene Taq (Nippon Gene, Co., Ltd., Tokyo, Japan). The oligonucleotide primers for NR2B were designed based on the sequences described by Lau et al. [29]. The sequences of PCR primers were as follows: NR2B, 5'-TCC GTC TTT CTT ATG TGG ATA TGC-3' (sense), 5'-CCT CTA GGC GGA CAG ATT AAG G-3' (antisense); glyceraldehyde-3-phosphate dehydrogenase (G3PDH), 5'-YGC CTG CTT CAC CAC CTT-3' (sense), 5'-TGC MTC CTG CAC CAC CAA CT-3' (antisense) (Sigma-Aldrich). Reactions were run for 40 cycles with 95°C denaturing cycle (30 s), 63°C annealing cycle (1 min) and 72°C extension cycle (30 s) for NR2B or for 30 cycles with 94°C denaturing cycle (45 s), 53°C annealing cycle (45 s) and 72°C extension cycle (1.5 min) for G3PDH, respectively. The PCR products were subjected to electrophoresis on 2% agarose gel, and the DNA was visualized by staining with ethidium bromide under ultraviolet irradiation. Then, the intensities of PCR products were semi-quantified densitometrically by Alpha Imager 2200 (Cell Biosciences, Inc., California, USA).
NADPH diaphorase histochemistry
Animals were anaesthetized with pentobarbital (50 mg/kg) and perfused through the left cardiac ventricle with 50 mL physiological saline followed by a fixative containing 4% paraformaldehyde in 0.1 M sodium phosphate (pH 7.4). The L4-6 spinal cord was removed and immersed in the fixative for 4 h and then cryoprotected overnight in 30% (w/v) sucrose in 0.1 M phosphate-buffered saline (pH 7.4). Transverse frozen sections (30 μm) were cut on a cryostat. These sections were thaw-mounted on slides and NOS activity was determined using NADPH diaphorase histochemistry as described by Mabuchi et al. [30]. The incubation was performed for 1 h at 37°C in a reaction mixture containing 0.5 mg/mL β-NADPH, 0.2 mg/mL nitroblue tetrazolium and 0.25% Triton X-100 in 0.1 M phosphate-buffered saline (pH 7.4).
Statistical analyses
Values were expressed as mean ± SEM. Results were analyzed by Student's t-test or one-way analysis of variance (ANOVA) followed by the Tukey-Kramer post-hoc test to determine differences among the groups. A P value of less than 0.05 is considered as statistically significant.
References
Yamamoto T, Yaksh TL: Spinal pharmacology of thermal hyperesthesia induced by constriction injury of sciatic nerve. Excitatory amino acid antagonists. Pain 1992, 49: 121–128. 10.1016/0304-3959(92)90198-K
Yamamoto T, Shimoyama N, Asano H, Mizuguchi T: Time-dependent effect of morphine and time-independent effect of MK-801, an NMDA antagonist, on the thermal hyperesthesia induced by unilateral constriction injury to the sciatic nerve in the rat. Anesthesiology 1994, 80: 1311–1319. 10.1097/00000542-199406000-00019
Gaunitz C, Schüttler A, Gillen C, Allgaier C: Formalin-induced changes of NMDA receptor subunit expression in the spinal cord of the rat. Amino Acids 2002, 23: 177–182. 10.1007/s00726-001-0125-3
Ma ZL, Zhang W, Gu XP, Yang WS, Zeng YM: Effects of intrathecal injection of prednisolone acetate on expression of NR2B subunit and nNOS in spinal cord of rats after chronic compression of dorsal root ganglia. Ann Clin Lab Sci 2007, 37: 349–355.
Wilson JA, Garry EM, Anderson HA, Rosie R, Colvin LA, Mitchell R, Fleetwood-Walker SM: NMDA receptor antagonist treatment at the time of nerve injury prevents injury-induced changes in spinal NR1 and NR2B subunit expression and increases the sensitivity of residual pain behaviours to subsequently administered NMDA receptor antagonists. Pain 2005, 117: 421–432. 10.1016/j.pain.2005.07.005
Zhang W, Shi CX, Gu XP, Ma ZL, Zhu W: Ifenprodil induced antinociception and decreased the expression of NR2B subunits in the dorsal horn after chronic dorsal root ganglia compression in rats. Anesth Analg 2009, 108: 1015–1020. 10.1213/ane.0b013e318193ffd2
Boyce S, Wyatt A, Webb JK, O'Donnell R, Mason G, Rigby M, Sirinathsinghji D, Hill RG, Rupniak NM: Selective NMDA NR2B antagonists induce antinociception without motor dysfunction: correlation with restricted localisation of NR2B subunit in dorsal horn. Neuropharmacology 1999, 38: 611–623. 10.1016/S0028-3908(98)00218-4
Qu XX, Cai J, Li MJ, Chi YN, Liao FF, Liu FY, Wan Y, Han JS, Xing GG: Role of the spinal cord NR2B-containing NMDA receptors in the development of neuropathic pain. Exp Neurol 2009, 215: 298–307. 10.1016/j.expneurol.2008.10.018
Nagy GG, Watanabe M, Fukaya M, Todd AJ: Synaptic distribution of the NR1, NR2A and NR2B subunits of the N-methyl-d-aspartate receptor in the rat lumbar spinal cord revealed with an antigen-unmasking technique. Eur J Neurosci 2004, 20: 3301–3312. 10.1111/j.1460-9568.2004.03798.x
Meller ST, Pechman PS, Gebhart GF, Maves TJ: Nitric oxide mediates the thermal hyperalgesia produced in a model of neuropathic pain in the rat. Neuroscience 1992, 50: 7–10. 10.1016/0306-4522(92)90377-E
Cízková D, Lukácová N, Marsala M, Marsala J: Neuropathic pain is associated with alterations of nitric oxide synthase immunoreactivity and catalytic activity in dorsal root ganglia and spinal dorsal horn. Brain Res Bull 2002, 58: 161–171.
Pasetto LM, D'Andrea MR, Rossi E, Monfardini S: Oxaliplatin-related neurotoxicity: how and why? Crit Rev Oncol Hematol 2006, 59: 159–168. 10.1016/j.critrevonc.2006.01.001
Saif MW, Reardon J: Management of oxaliplatin-induced peripheral neuropathy. Ther Clin Risk Manag 2005, 1: 249–258.
Sakurai M, Egashira N, Kawashiri T, Yano T, Ikesue H, Oishi R: Oxaliplatin-induced neuropathy in the rat: involvement of oxalate in cold hyperalgesia but not mechanical allodynia. Pain 2009, 147: 165–174. 10.1016/j.pain.2009.09.003
Graham MA, Lockwood GF, Greenslade D, Brienza S, Bayssas M, Gamelin E: Clinical pharmacokinetics of oxaliplatin: a critical review. Clin Cancer Res 2000, 6: 1205–1218.
Grolleau F, Gamelin L, Boisdron-Celle M, Lapied B, Pelhate M, Gamelin E: A possible explanation for a neurotoxic effect of the anticancer agent oxaliplatin on neuronal voltage-gated sodium channels. J Neurophysiol 2001, 85: 2293–2297.
Guan Y, Yaster M, Raja SN, Tao YX: Genetic knockout and pharmacologic inhibition of neuronal nitric oxide synthase attenuate nerve injury-induced mechanical hypersensitivity in mice. Mol Pain 2007, 3: 29. 10.1186/1744-8069-3-29
Abe T, Matsumura S, Katano T, Mabuchi T, Takagi K, Xu L, Yamamoto A, Hattori K, Yagi T, Watanabe M, Nakazawa T, Yamamoto T, Mishina M, Nakai Y, Ito S: Fyn kinase-mediated phosphorylation of NMDA receptor NR2B subunit at Tyr1472 is essential for maintenance of neuropathic pain. Eur J Neurosci 2005, 22: 1445–1454. 10.1111/j.1460-9568.2005.04340.x
Nei K, Matsuyama S, Shuntoh H, Tanaka C: NMDA receptor activation induces glutamate release through nitric oxide synthesis in guinea pig dentate gyrus. Brain Res 1996, 728: 105–110. 10.1016/0006-8993(96)00394-0
Martin TJ, Eisenach JC: Pharmacology of opioid and nonopioid analgesics in chronic pain states. J Pharmacol Exp Ther 2001, 299: 811–817.
Gurwitz D, Weizman A: The NR2B subunit of glutamate receptors as a potential target for relieving chronic pain: prospects and concerns. Drug Discov Today 2002, 7: 403–406. 10.1016/S1359-6446(02)02242-0
Chizh BA, Headley PM: NMDA antagonists and neuropathic pain--multiple drug targets and multiple uses. Curr Pharm Des 2005, 11: 2977–2994. 10.2174/1381612054865082
Zimmermann M: Ethical guidelines for investigations of experimental pain in conscious animals. Pain 1983, 16: 109–110. 10.1016/0304-3959(83)90201-4
Egashira N, Hirakawa S, Kawashiri T, Yano T, Ikesue H, Oishi R: Mexiletine reverses oxaliplatin-induced neuropathic pain in rats. J Pharmacol Sci 2010, 112: 473–6. 10.1254/jphs.10012SC
Kawashiri T, Egashira N, Watanabe H, Ikegami Y, Hirakawa S, Mihara Y, Yano T, Ikesue H, Oishi R: Prevention of oxaliplatin-induced mechanical allodynia and neurodegeneration by neurotropin in rat model. Eur J Pain 2010, in press.
Chaplan SR, Malmberg AB, Yaksh TL: Efficacy of spinal NMDA receptor antagonism in formalin hyperalgesia and nerve injury evoked allodynia in the rat. J Pharmacol Exp Ther 1997, 280: 829–238.
Chizh BA, Reissmüller E, Schlütz H, Scheede M, Haase G, Englberger W: Supraspinal vs spinal sites of the antinociceptive action of the subtype-selective NMDA antagonist ifenprodil. Neuropharmacology 2001, 40: 212–220. 10.1016/S0028-3908(00)00148-9
Osborne MG, Coderre TJ: Effects of intrathecal administration of nitric oxide synthase inhibitors on carrageenan-induced thermal hyperalgesia. Br J Pharmacol 1999, 126: 1840–1846. 10.1038/sj.bjp.0702508
Lau WK, Yeung CW, Lui PW, Cheung LH, Poon NT, Yung KK: Different trends in modulation of NMDAR1 and NMDAR2B gene expression in cultured cortical and hippocampal neurons after lead exposure. Brain Res 2002, 932: 10–24. 10.1016/S0006-8993(01)03395-9
Mabuchi T, Matsumura S, Okuda-Ashitaka E, Kitano T, Kojima H, Nagano T, Minami T, Ito S: Attenuation of neuropathic pain by the nociceptin/orphanin FQ antagonist JTC-801 is mediated by inhibition of nitric oxide production. Eur J Neurosci 2003, 17: 1384–1392. 10.1046/j.1460-9568.2003.02575.x
Acknowledgements
Part of this study was supported by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (Nos. 21590285 and 22590242).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
YM, NE, TK, TY, HI and RO are responsible for experimental design. YM and HS are responsible for performance of behavioral test. YM, HS, TK and SU are responsible for performance of Western blot, PCR and NADPH diaphorase staining. YM, NE, HS, TK and RO are responsible for writing the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Mihara, Y., Egashira, N., Sada, H. et al. Involvement of spinal NR2B-containing NMDA receptors in oxaliplatin-induced mechanical allodynia in rats. Mol Pain 7, 8 (2011). https://doi.org/10.1186/1744-8069-7-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1744-8069-7-8