Abstract
Background
The aim of this study was to investigate the possibility that a decreased mitochondrial ATP synthesis causes muscular and mental fatigue and plays a role in the pathophysiology of the chronic fatigue syndrome (CFS/ME).
Methods
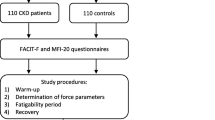
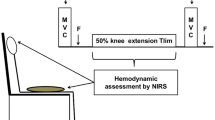
Female patients (n = 15) and controls (n = 15) performed a cardiopulmonary exercise test (CPET) by cycling at a continuously increased work rate till maximal exertion. The CPET was repeated 24 h later. Before the tests, blood was taken for the isolation of peripheral blood mononuclear cells (PBMC), which were processed in a special way to preserve their oxidative phosphorylation, which was tested later in the presence of ADP and phosphate in permeabilized cells with glutamate, malate and malonate plus or minus the complex I inhibitor rotenone, and succinate with rotenone plus or minus the complex II inhibitor malonate in order to measure the ATP production via Complex I and II, respectively. Plasma CK was determined as a surrogate measure of a decreased oxidative phosphorylation in muscle, since the previous finding that in a group of patients with external ophthalmoplegia the oxygen consumption by isolated muscle mitochondria correlated negatively with plasma creatine kinase, 24 h after exercise.
Results
At both exercise tests the patients reached the anaerobic threshold and the maximal exercise at a much lower oxygen consumption than the controls and this worsened in the second test. This implies an increase of lactate, the product of anaerobic glycolysis, and a decrease of the mitochondrial ATP production in the patients. In the past this was also found in patients with defects in the mitochondrial oxidative phosphorylation. However the oxidative phosphorylation in PBMC was similar in CFS/ME patients and controls. The plasma creatine kinase levels before and 24 h after exercise were low in patients and controls, suggesting normality of the muscular mitochondrial oxidative phosphorylation.
Conclusion
The decrease in mitochondrial ATP synthesis in the CFS/ME patients is not caused by a defect in the enzyme complexes catalyzing oxidative phosphorylation, but in another factor.
Trial registration
Clinical trials registration number: NL16031.040.07
Similar content being viewed by others
Background
Chronic fatigue syndrome/myalgic encephalopathy (CFS/ME) as a syndrome was defined in consensus meetings by Fukuda et al [1]. Fatigue was the major criterion in the definition. It was described as suddenly occurring, not explained, not caused by exercise, insufficiently relieved by rest and causing a major reduction in physical capacity. The additional symptoms of the syndrome were headache, pain in muscles and joints, unrefreshing sleep, postexertional malaise, sore throat, painful lymph glands and insufficient concentration. The combination of fatigue and four or more of the additional symptoms lasting at least for 6 months, sufficed for the diagnosis of CFS/ME. The main exclusion criterion for CFS/ME, was the presence of a disease that is generally accepted as an actual cause of fatigue.
Several groups of investigators assume that a defective oxidative phosphorylation and subsequent free radical production and oxidative stress play an important role in the pathophysiology of CFS/ME [2–11]. A well accepted way to test ATP synthesis under increased work rate is the cardiopulmonary exercise test (CPET) [12–16]. The ATP synthesis is measured indirectly by testing for oxygen uptake (V'O2) as a measure for oxygen consumption (Q'O2) in an exercise protocol. Q'O2 can be restricted when mitochondria are insufficiently active, or by a restricted supply line of oxygen that consists of the lungs, both ventilation and perfusion, the heart pump, the blood vessels and the hemoglobin concentration in the blood. Modern equipment and algorisms suggested the exclusion of these latter causes of an inadequate Q'O2, and supported the likelihood of inactivity of the mitochondrial oxidative phosphorylation. This was also suggested by the finding of a decreased anaerobic threshold in the CFS/ME patients, which is determined by CPET. The anaerobic threshold is the rate of oxygen consumption, when the work rate is reached at which blood lactic acid starts to accumulate, and is due to ATP synthesis from anaerobic glycolysis in muscles. In patients with defects in the oxidative phosphorylation, the anaerobic threshold is also reached at a lower oxygen consumption than in controls [17, 18].
In this study we compared the CPET [19] with a direct assay of the oxidative phosphorylation in peripheral mononuclear cells (PBMC), attempting to prove an abnormality of this process in the patients. After 24 h these tests were repeated.
Methods
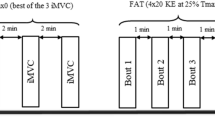
Patients who visited the CFS/ME Clinic Amsterdam and healthy sedentary controls were invited for the study. All patients fulfilled the criteria of Fukuda et al [1] for CFS/ME and reported the start of symptoms after an infectious disease. Exclusion criteria were according to Fukuda et al [1]. Contra indications for the CPET were mainly cardiac diseases, hypertension, or the inability to perform the exercise as in arthrosis of the knee. Medication was discontinued 2 weeks before the first test. All subjects performed a CPET on a cycle ergometer (Excalibur, Lode, Groningen, The Netherlands) according to our protocol: 3 min without activity, 3 min of unloaded pedaling, followed by pedaling against increasing resistance until exhaustion (RAMP protocol) and ended by 3 min pedaling with low resistance. The rate of work rate increase was estimated from history, physical examination, gender, weight and height. The participants performed symptom limited exercise tests as described by Wassermann et al. [13]. Verbal encouragement to perform maximally was used during the last phase of incremental exercise. Exhaustion of the leg muscles was the limiting symptom in all participants. The V'E, V'O2, V'CO2 and oxygen saturation were continuously measured (Metasoft). The ECG was continuously recorded and blood pressure was measured every 2 min. The CPET was repeated after 24 h. The Respiratory Exchange Rate (RER) was used for validation of the repeated CPET.
The exercise ECG of the subjects was analyzed (by FCV). The anaerobic threshold was determined by the V-slope method.
The participants completed questionnaires among others (not shown) about additional symptoms of CFS/ME (Centers for Disease Control and Prevention Symptoms Inventory - Dutch Language Version (CDC Symptom Inventory-DLV)) [20]. The criterion for fatigue was that at least 4 CFS/ME symptoms must be ≥ 7.5 [20].
All subjects were seen and an ECG was approved by the internist (RMK).
The results of the tests were not available to the participants or the investigators until after the last test was performed by the participant.
Before entry into the study, the nature of the study was explained to the participants and written consent was obtained. The STEG independent ethics committee approved the study. The trial was conducted in accordance with the Declaration of Helsinki (1996 revision) and under the principals of good clinical practice, as laid out in the International Conference on Harmonization document Good Clinical Practice Consolidated Guideline.
ATP synthesis assay of PBMC
PBMC were isolated from 20 mL of blood obtained before each CEPT and anti-coagulated with 0.18% EDTA as described in detail elsewhere [21, 22]. For cryostorage in liquid nitrogen, PBMC were suspended at 1 × 107 cells/mL phosphate-buffered saline, pH 7.4, containing 2 mM EDTA, 10% newborn calf serum and 10% dimethyl sulfoxide. To study mitochondrial function, PBMC were thawed and ATP production via reduction of complex I or II was determined exactly as described [22] except that the cell concentration was decreased to only 5 × 104 cells per mL incubation medium. A small sample was used to determine citrate synthase (CS) activity according to Srere [23] and protein concentration by the Bio-Rad DC protein assay (Bio-Rad Laboratories) with bovine serum albumine as a standard. The ATP synthesis rate was expressed as nmol ATP synthesized per 30 min per U citrate synthase (CS) or per mg protein.
Plasma creatine kinase (CK) is usually considered a marker of non-specific muscle damage. In the plasma the activity of CK was measured, as a surrogate measure of a lowered oxidative phosphorylation in skeletal muscle. The rationale of this came from early work by Driessen-Kletter et al. [24]. In a group of seven patients with chronic external ophthalmoplegia a high negative correlation of (R = -0.988; P = 0.0002) was found between plasma CK 24 h after exercise, and the activity of oxidative phosphorylation via reduction of complex I. Plasma CK was tested by the Clinical Chemistry Laboratory (AKC) of Erasmus MC.
Statistical analysis
Statistical analyses were conducted using the Statistical Package for the Social Sciences (17.0 for Windows, Chicago, Ill, US). Kolmogorov-Smirnov tests for normality showed that the data were normally distributed. The results were expressed as the mean ± standard deviation (SD). Differences between groups were tested with multivariate or repeated measures Analysis of Variance (ANOVA) where appropriate; correlations were tested with Pearson's correlation test.
Results
Patients
Inclusion of patients for the study started in May 2007 and the last CPET was in December 2007. Analysis of the blood samples ended in March 2009. At screening 8 of the 23 patients fulfilled exclusion criteria for the study. In the remaining patients, the results of the male participants were significantly different from females. The low number of male patients prevented separate statistical analysis, therefore only the data of the 15 female participants were reported in this study, together with 15 female healthy controls. Demographic data are presented in Table 1 including the scores for the CDC Symptom Inventory-DLV.
CPET1 and CPET2
The V'O2 max in CPET1 and CPET2 in the control group were closely related (R = 0.994; P < 0.001).
Table 2 summarizes the results of CPET1 and CPET2. At rest the Forced Vital Capacity, the Forced Expiratory Volume (in the first second), the heart rate, oxygen consumption and CO2 production were not different between the patient and control group. At the anaerobic threshold the two groups differed for the work rate. (58.6 ± 24.2 W in patients, versus 82.9 ± 29.1 W; P = 0.019, 95% CI: -44.3; -4.3), oxygen uptake (12.8 ± 3.0 mL/kg versus 16.7 ± 4.0 mL/kg; P = 0.006, 95% CI: -6.52; -1.22) and the ventilatory equivalent for CO2 (29.3 ± 2.3 versus 26.9 ± 1.5 in controls; P = 0.002, 95% CI: 0.94; 3.86). At maximal work rate, similar differences were seen: work rate (132 ± 30 W versus 188 ± 46 W; P = 0.001, 95% CI: -85.5; -27.7), oxygen pulse (9.19 ± 2.18 mL/beat versus 12.43 ± 5.25; P = 0.036, 95% CI: -6.25; -0.23) and oxygen uptake (22.3 ± 5.7 mL/kg versus 31.2 ± 7.0; P = 0.001, 95% CI: -13.71; -4.16). The results of the second test showed the same differences between the patients and controls (Table 2). The work rate, oxygen pulse and oxygen uptake at the anaerobic threshold and at maximal work rate in the first and second test were closely correlated (paired t- test, P < 0.001). The oxygen pulse at rest in the first test correlated with oxygen uptake at maximal work rate in the first test (R = 0.63; P < 0.001) and in the second test (R = 0.63; P < 0.001). The results of the CPET1 and CPET2 showed significant correlations of all measures in the 2 tests (Pearson's test, P < 0.001).
The differences between the CPET2 and CPET1 are shown in table 3. The FVC, the FEV1 and the results of resting heart rate, oxygen consumption and CO2 production did not change in the patient and control group. At the anaerobic threshold the group of patients performed worse and the controls improved. The work rate was 4.40 ± 9.66 W less in the patient group and 7.67 ± 19.50 W higher in the control group (P = 0.002, 95% CI: -23.6; -0.55). Such differences were also found for the oxygen pulse (-0.67 ± 0.93 mL/beat versus 0.25 ± 1.09 mL/beat; P = 0.014, 95% CI: -1.68; -0.16) and oxygen uptake (-0.87 ± 1.07 mL/kg versus 1.07 ± 2.63 mL/kg; P = 0.001, 95% CI: -3.61; -0.26). Similar changes were found at maximal work rate: The work rate was 6.33 ± 11.5 W less in the patient group and 11.1 ± 18.3 W higher in the control group (P < 0.001, 95% CI: -28.8; -5.99). And the changes in the oxygen uptake were likewise (-1.33 ± 1.68 mL/kg versus 0.73 ± 1.39 mL/kg; P < 0.001, 95% CI: -3.22; -0.92). The improvement in the performance of the controls is likely due to the effect of training. In the group of patients the performance is the result of a similar training effect which is counteracted by the effect of the postexertional malaise.
ATP synthesis in PBMC
The results are summarized in table 4. The cells were isolated before the exercise tests. The amount of the mitochondria of PBMC was estimated by the assay of citrate synthase, and the activity was not different between the four groups (patients and controls at CEPT1 and 2).
The ATP synthesis assayed via the reduction of complex I, expressed on basis of protein were similar in the groups, and also when the ATP synthesis rate was expressed on basis of citrate synthase. The same was found for ATP synthesis via complex II.
In the present study, plasma CK was low and not increased before and 24 h after exercise in the patient group, and not different from the control group, suggesting no muscle damage and no major intrinsic abnormalities of muscular oxidative phosphorylation in CFS/ME patients.
Discussion
At rest the cardiopulmonary exercise test 1 and 2 showed no difference between patients and controls. Increasing work rate made the differences obvious. The lower V'O2 at the anaerobic threshold indicated that the difference in V'O2 at maximal work rate was not due to a reduced willingness to perform in the CFS/ME group.
The FEV1 and the FVC were not different, but the higher ventilatory equivalent for CO2 at the anaerobic threshold indicated the possibility of a ventilation-perfusion mismatch in the patient group. The reproducibility of CPET was high, relatively poor performers at the first test ranked low in the second test too. There were significant differences between the patients and controls. Based on the oxygen uptake test, the patients not only performed worse than controls in the first test, but the recovery after 24 h was not completed in this group as well. This indicates an impaired recovery [25], as expressed in the criterion "postexertional malaise" of the CDC Symptom score.
A limited mitochondrial ATP synthesis was the working hypothesis for this investigation. This is probably not true, as the energy production can be limited by other mechanisms as well. The exercise tests with increased work load suggested the possibility that the mitochondrial ATP synthesis was decreased, because the anaerobic threshold was reached. Then the mitochondria were not longer able to produce sufficient ATP to sustain the exercise, and the anaerobic glycolysis in muscle had to produce the extra ATP needed, which is reflected by the lactate production. This is also the case in patients with defects in the oxidative phosphorylation. Peripheral blood mononuclear cells are commonly used to assess the gene expression in CFS/ME [26–34], and the expressions of various genes involved in mitochondrial protein synthesis, energy metabolism, and in free radical metabolism were found to be changed. The results of the present study do not support a physiological effect of these changes, and demonstrated that the oxidative phosphorylation in PCMB of CFS/ME patients is fully normal. And it is likely that also their muscle mitochondria are normal, since 24 h after strenuous exercise CK did not leak to the blood, as is the case in patients with defective oxidative phosphorylation.
A recent publication [6] claimed to have found a defective oxidative phosphorylation in neutrophils of CFS/ME patients, but the flux through this process had not been measured. These investigators performed a so called "ATP profile" test, and determined ATP under five different conditions, and the sum of these was found to be abnormal in 70 of 71 patients. One of us (WS) was involved in an investigation that clearly showed that neutrophils do not catalyze oxidative phosphorylation and the remaining complexes of the respiratory chain maintain the mitochondrial membrane potential [35]. Their mitochondria are only active in apoptosis [36].
In line with the present work, Mathew et al [37] discovered by proton magnetic resonance spectroscopy imaging that ventricular cerebrospinal lactate was 3.5-fold increased in CFS/ME patients. McCully and Natelson [38] demonstrated by combined near-infrared spectroscopy and 31P magnetic resonance spectroscopy that during exercise the oxygen delivery to skeletal muscle was delayed. Neary et al [39] established by near-infrared spectrometry that the oxygenation of the prefrontal brain lobe was decreased in exercising patient to 67% of that in controls, confirming the results of a study by Streeten and Bell [40] and Hurwitz et al [41] and in line with a decreased blood volume in CFS patients.
Conclusions
The decrease in mitochondrial ATP production at increasing work rate, detected by the CPET tests in the present well-characterized though small group of CFS/ME patients, is a secondary phenomenon. This was shown by the normality of the oxidative phosphorylation in peripheral blood mononuclear cells. The chain of mechanisms that couple (external) pulmonary to (internal) cellular respiration showed no abnormal differences in this study between CFS patients and healthy controls at the pulmonary, cardiac and circulatory level. Two possible explanations for the insufficient energy production in CFS remained: a lower transport capacity of oxygen as in anemia or a mitochondrial insufficiency. We showed that the mitochondrial ATP production shows no defect. Then the conclusion must be that the transport capacity of oxygen is limited in CFS patients.
Abbreviations
- CDC:
-
US Centers for Disease Control and Prevention
- CFS/ME:
-
chronic fatigue syndrome/myalgic encephalopathy
- CK:
-
creatine kinase
- CPET:
-
cardiopulmonary exercise test
- CS:
-
citrate synthase
- FVC:
-
forced vital capacity
- PBMC:
-
peripheral blood mononuclear cells
- V'CO2:
-
carbondioxyde output
- V'E:
-
minute ventilation
- V'O2:
-
oxygen uptake
- WR:
-
work rate
References
Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A, Schluederberg A, Jones JF, Lloyd AR, Wessely S, International Chronic Fatigue Syndrome Study Group: The chronic fatigue syndrome: A comprehensive approach to its definition and study. Annals of Internal Medicine. 1994, 121: 953-959.
Pieczenik SR, Neustadt J: Mitochondrial dysfunction and molecular pathways of disease. Experimental and Molecular Pathology. 2007, 83: 84-92. 10.1016/j.yexmp.2006.09.008.
Lane RJM, Barrett MC, Taylor DJ, Kemp GJ, Lodi R: Heterogeneity in chronic fatigue syndrome: Evidence from magnetic resonance spectroscopy of muscle. Neuromuscular Disorders. 1998, 8: 204-209. 10.1016/S0960-8966(98)00021-2.
Barnes PRJ, Taylor DJ, Kemp GJ, Radda GK: Skeletal muscle bioenergetics in the chronic fatigue syndrome. Journal of Neurology Neurosurgery and Psychiatry. 1993, 56: 679-683. 10.1136/jnnp.56.6.679.
Bains W: Treating Chronic Fatigue states as a disease of the regulation of energy metabolism. Medical Hypotheses. 2008, 71: 481-488. 10.1016/j.mehy.2008.02.022.
Myhill S, Booth NE, McLaren-Howard J: Chronic fatigue syndrome and mitochondrial dysfunction. International Journal of Clinical and Experimental Medicine. 2009, 2: 1-16.
Chinnery PF, Turnbull DM: Mitochondrial medicine. QJM - Monthly Journal of the Association of Physicians. 1997, 90: 657-667.
Fulle S, Mecocci P, Fano G, Vecchiet I, Vecchini A, Racciotti D, Cherubini A, Pizzigallo E, Vecchiet L, Senin U, Beal MF: Specific oxidative alterations in vastus lateralis muscle of patients with the diagnosis of chronic fatigue syndrome. Free Radical Biology and Medicine. 2000, 29: 1252-1259. 10.1016/S0891-5849(00)00419-6.
Chaudhuri A, Behan PO: In vivo magnetic resonance spectroscopy in chronic fatigue syndrome. Prostaglandins Leukotrienes and Essential Fatty Acids. 2004, 71: 181-183. 10.1016/j.plefa.2004.03.009.
Jammes Y, Steinberg JG, Mambrini O, Bregeon F, Delliaux S: Chronic fatigue syndrome: assessment of increased oxidative stress and altered muscle excitability in response to incremental exercise. Journal of Internal Medicine. 2005, 257: 299-310. 10.1111/j.1365-2796.2005.01452.x.
Kennedy G, Spence VA, McLaren M, Hill A, Underwood C, Belch JJF: Oxidative stress levels are raised in chronic fatigue syndrome and are associated with clinical symptoms. Free Radical Biology and Medicine. 2005, 39: 584-589. 10.1016/j.freeradbiomed.2005.04.020.
Agostoni P, Bianchi M, Moraschi A, Palermo P, Cattadori G, La Gioia R, Bussotti M, Wasserman K: Work-rate affects cardiopulmonary exercise test results in heart failure. European Journal of Heart Failure. 2005, 7: 498-504. 10.1016/j.ejheart.2004.06.007.
Wasserman K, Hansen JE, Sue DY, Stringer WW, Whipp BJ: Principles of exercise testing and interpretation. 2005, Philadelphia: Lippincott Williams & Wilkins, 4
VanNess JM, Stevens SR, Bateman L, Stiles TL, Snell CR: Postextertional malaise in women with chronic fatigue syndrome. Journal of Women's Health. 2010, 19: 239-244. 10.1089/jwh.2009.1507.
Nijs J, van Oosterwijck J, Meeus M, Lambrecht L, Metzger K, Frémont M, Paul L: Unravelling the nature of postexertional malaise in myalgic encephalomyelitis/chronic fatigue syndrome: the role of elastase, complement C4a and interleukin-1β. Journal of Internal Medicine. 2010, 267: 418-435. 10.1111/j.1365-2796.2009.02178.x.
Van Oosterwijck J, Nijs J, Meeus M, Lefever I, Huybrechts L, Lambrecht L, Paul L: Pain inhibition and postexertional malaise in myalgic encephalomyelitis/chronic fatigue syndrome: An experimental study. Journal of Internal Medicine. 2010, 268: 265-278. 10.1111/j.1365-2796.2010.02228.x.
Bogaard JM, Scholte HR, Busch HFM, Stam H, Versprille A: Anaerobic threshold as detected from ventilatory and metabolic exercise responses in patients with mitochondrial respiratory chain defect. Advances in Cardiology. 1986, 35: 135-145.
Wallace DC, Zheng X, Lott MT, Shoffner JM, Hodge JA, Kelley RI, Epstein CM, Hopkins LC: Familial mitochondrial encephalomyopathy (MERRF): Genetic, pathophysiological, and biochemical characterization of a mitochondrial DNA disease. Cell. 1988, 55: 601-610. 10.1016/0092-8674(88)90218-8.
VanNess JM, Snell CR, Stevens SR: Diminished cardiopulmonary capacity during post-exertional malaise. Journal of Chronic Fatigue Syndrome. 2008, 14: 77-85. 10.1300/J092v14n02_07.
Vermeulen RCW: Translation and validation of the Dutch language version of the CDC Symptom Inventory for assessment of Chronic Fatigue Syndrome (CFS). Population Health Metrics. 2006, 4: 10.1186/1478-7954-4-12.
de Wit LEA, Sluiter W: Reliable assay for measuring complex I activity in human blood lymphocytes and skin fibroblasts. Methods in Enzymology. 2009, 456: 169-181. full_text.
Korsten A, de Coo IFM, Spruijt L, de Wit LEA, Smeets HJM, Sluiter W: Patients with Leber hereditary optic neuropathy fail to compensate impaired oxidative phosphorylation. Biochimica Biophysica Acta. 2010, 1797: 197-203. 10.1016/j.bbabio.2009.10.003.
Srere PA: Citrate synthase. Methods in Enzymology. 1969, 13: 3-11. full_text.
Driessen-Kletter MF, Bar PR, Scholte HR, Hoogenraad TU, Luyt-Houwen IEM: A striking correlation between muscle damage after exercise and mitochondrial dysfunction in patients with chronic external ophthalmoplegia. Journal of Inherited Metabolic Disease. 1987, 10 (suppl 2): 252-255. 10.1007/BF01811418.
Paul L, Wood L, Behan WMH, Maclaren WM: Demonstration of delayed recovery from fatiguing exercise in chronic fatigue syndrome. European Journal of Neurology. 1999, 6: 63-69. 10.1046/j.1468-1331.1999.610063.x.
Kaiser J: Biomedicine. Genes and chronic fatigue: how strong is the evidence?. Science. 2006, 312: 669-671. 10.1126/science.312.5774.669.
Witkowski JA: The postgenomic era and complex disease. Pharmacogenomics. 2006, 7: 341-343. 10.2217/14622416.7.3.341.
Carmel L, Efroni S, White PD, Aslakson E, Vollmer-Conna U, Rajeevan MS: Gene expression profile of empirically delineated classes of unexplained chronic fatigue. Pharmacogenomics. 2006, 7: 375-386. 10.2217/14622416.7.3.375.
Fang H, Xie Q, Boneva R, Fostel J, Perkins R, Tong W: Gene expression profile exploration of a large dataset on chronic fatigue syndrome. Pharmacogenomics. 2006, 7: 429-440. 10.2217/14622416.7.3.429.
Fostel J, Boneva R, Lloyd A: Exploration of the gene expression correlates of chronic unexplained fatigue using factor analyis. Pharmacogenomics. 2006, 7: 441-454. 10.2217/14622416.7.3.441.
Goertzel BN, Pennachin C, de Souza Coelho L, Gurbaxani B, Maloney EM, Jones JF: Combinations of single nucleotide polymorphisms in neuroendocrine effector and receptor genes predict chronic fatigue syndrome. Pharmacogenomics. 2006, 7: 475-483. 10.2217/14622416.7.3.475.
Demitrack MA: Clinical methodology and its implications for the study of therapeutic interventions for chronic fatigue syndrome: A commentary. Pharmacogenomics. 2006, 7: 521-528. 10.2217/14622416.7.3.521.
Kaushik N, Fear D, Richards SCM, McDermott CR, Nuwaysir EF, Kellam P, Harrison TJ, Wilkinson RJ, Tyrrell DAJ, Holgate ST, Kerr JR: Gene expression in peripheral blood mononuclear cells from patients with chronic fatigue syndrome. Journal of Clinical Pathology. 2005, 58: 826-832. 10.1136/jcp.2005.025718.
Gow JW, Hagan S, Herzyk P, Cannon C, Behan PO, Chaudhuri A: A gene signature for post-Infectious chronic fatigue syndrome. BMC Medical Genomics. 2009, 2-
van Raam BJ, Sluiter W, de Wit LEA, Roos D, Verhoeven AJ, Kuijpers TW: Mitochondrial membrane potential in human neutrophils is maintained by complex III activity in the absence of supercomplex organisation. PLoS ONE. 2008, 3: e2013-10.1371/journal.pone.0002013.
Maianski NA, Geissler J, Srinivasula SM, Alnemri ES, Roos D, Kuijpers TW: Functional characterization of mitochondria in neutrophils: A role restricted to apoptosis. Cell Death and Differentiation. 2004, 11: 143-153. 10.1038/sj.cdd.4401320.
Mathew SJ, Mao X, Keegan KA, Levine SM, Smith ELP, Heier LA, Otcheretko V, Coplan JD, Shungu DC: Ventricular cerebrospinal fluid lactate is increased in chronic fatigue syndrome compared with generalized anxiety disorder: An in vivo 3.0 T 1H MRS imaging study. NMR in Biomedicine. 2009, 22: 251-258. 10.1002/nbm.1315.
McCully KK, Natelson BH: Impaired oxygen delivery to muscle in chronic fatigue syndrome. Clinical Science. 1999, 97: 603-608. 10.1042/CS19980372.
Neary JP, Roberts ADW, Leavins N, Harrison MF, Croll JC, Sexsmith JR: Prefrontal cortex oxygenation during incremental exercise in chronic fatigue syndrome. Clinical Physiology and Functional Imaging. 2008, 28: 364-372. 10.1111/j.1475-097X.2008.00822.x.
Streeten DHP, Bell DS: Circulating blood volume in chronic fatigue syndrome. Journal of Chronic Fatigue Syndrome. 1998, 4: 3-11. 10.1300/J092v04n01_02.
Hurwitz BE, Coryell VT, Parker M, Martin P, Laperriere A, Klimas NG, Sfakianakis GN, Bilsker MS: Chronic fatigue syndrome: Illness severity, sedentary lifestyle, blood volume and evidence of diminished cardiac function. Clinical Science. 2010, 118: 125-135. 10.1042/CS20090055.
Acknowledgements
This study was supported by the William Dircken grant from the "ME/CVS-Stichting Nederland". We thank Elly de Wit for expert biochemical assistance, Prof dr J Lindemans for the CK test and Otto Bauermann for fruitful discussions and support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
All authors were involved in the set up of the experiments. The clinicians (RCWV, RMK, FCV) performed the clinical experiments. The blood separation and the biochemical assays were done by WS. The first drafts of the paper were written by RCWV and HRS. The final manuscript was read and approved by all authors.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Vermeulen, R.C., Kurk, R.M., Visser, F.C. et al. Patients with chronic fatigue syndrome performed worse than controls in a controlled repeated exercise study despite a normal oxidative phosphorylation capacity. J Transl Med 8, 93 (2010). https://doi.org/10.1186/1479-5876-8-93
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1479-5876-8-93