Abstract
Background
Effective management of menopause is an important way to improve the quality of life of the increasing number of older women. The study sought to find out if Nigerian Gynaecologists offer effective treatment for severe menopausal symptoms.
Methods
126 Nigerian Gynaecologists representing the six health zones of Nigeria were interviewed to determine the menopausal symptoms they had ever encountered in their practices, frequency of the symptoms, treatments ever offered for severe symptoms including their attitude to, and practice of hormone replacement therapy.
Results
A Nigerian Gynaecologist encountered an average of one patient with menopausal symptoms every three months (range: 0-3 patients per month). The commoner symptoms they encountered were hot flushes (88%), insomnia (75.4%), depression (58.0%), irritability (56.3%), night sweats (55.6%) and muscle pains (54.8%) while urinary symptoms (16.7%) and fracture (1.6%) were less common. Treatments ever offered for severe symptoms were reassurance (90.5%), anxiolytics (68.3%), analgesics (14.3), HRT (7.9%), Vitamins (4%), Beta-blockers (3.2%) and Danazol (2.4%). These treatments were offered as a matter of institutional traditions rather than being based on any evidence of their efficacy.
Conclusion
The result revealed that most Nigerian Gynaecologists prefer reassurance and anxiolytics for managing severe menopausal symptoms instead of evidence-based effective therapies. A policy of mandatory continuing medical education for Nigerian physicians is recommended to ensure evidence-based management of gynaecological problems, including menopause.
Similar content being viewed by others
Background
Effective management of menopause is necessary to improve the quality of life of the growing population of menopausal women. The increasing life expectancy in most societies means that more than ever before, women are now attaining menopause and spending more years in a state of ovarian failure. The age of menopause has remained constant at about 51 ± 3 years [1–3]. With an average life expectancy of 82 years in Britain for instance, an average woman now spends about a third of her life-time in the menopausal state. Ovarian failure is associated with profound changes which have both short term and long term consequences for the woman's quality of life [4]. Relatively simple hormone treatments are effective for this condition [4–6]. Non-hormonal treatments have also been employed for many years with varying degrees of reported successes [4, 7–10]. However, only hormone replacement therapy (HRT) is believed to address the root cause of the symptoms, and has proved effective for symptomatic relief as well as for prevention of the long term sequellae of menopause [4, 11, 12]. HRT remains the reference standard for assessing the effectiveness of non-hormonal interventions. The results of the Women's Health Initiative Survey [13] and subsequent studies [14, 15], have revealed evidences of increased risks of breast cancer, stroke and pulmonary embolism in association with long term use of hormone replacement therapy. HRT is however still considered justifiable and indeed recommended for symptomatic relief of severe menopausal symptoms although it is no longer recommended for long-term prophylaxis [5, 14–16]. Physicians who care for women are expected to be familiar with evidence-based effective and safe management of menopause.
In Nigeria, there is dearth of information on the subject menopause. Because few women presented to hospital with menopausal symptoms, it was assumed in the past that most Nigerian women did not develop menopausal symptoms or that the symptoms were so mild that the women could cope without medical treatment. Hence, the average Nigeria-trained physician did not consider menopausal symptoms as important health problems. Recent community-based studies [17, 18] have revealed that most menopausal symptoms are indeed prevalent amongst Nigerian women. Because of cultural practices that engender positive attitude to menopause in some Nigerian communities [17], women with mild menopausal symptoms are able to cope with the symptoms without seeking for treatment. However, women with moderate and severe menopausal symptoms consider them important health concerns and seek treatment for these symptoms. According to Agwu et.al [18] women who consulted physicians for menopausal symptoms were not offered effective treatments of their symptoms whereas those who consulted the herbal medicine practitioners were offered more effective herbal therapies most of which consisted of phytoestrogen preparations. As a result, the botanical preparations are very popular among the menopausal women while hospital consultations for menopausal symptoms are unpopular. Could the paucity of hospital consultations for menopausal symptoms in Nigeria be the result of ineffective hospital-based treatment of these symptoms? The overall objective of this study was to determine whether or not Nigerian Gynaecologists offer effective and evidence-based treatment of severe menopausal symptoms. The specific objectives were to determine the menopausal symptoms ever encountered by Nigerian Gynaecologists in their practices, the relative frequencies of the symptoms, the types of treatment they had ever offered for severe menopausal symptoms and their attitude to, and practice of hormone replacement therapy. The results of the study are expected to be particularly useful to the Society of Gynaecology and Obstetrics of Nigeria (SOGON) and the Postgraduate Medical Colleges in their respective functions of regulating gynaecology practice and training of Gynaecologists in Nigeria.
Methods
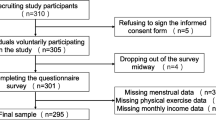
This cross sectional study was conducted amongst Nigerian Gynaecologists who were attending an annual conference. The study population was the 540 Gynaecologists in the register of the Society of Gynaecology and Obstetrics of Nigeria (SOGON) in 2006 [19]. A minimum sample size of 109, representing 20% of study population was considered an adequate representative of the study population. In order to ensure proportionate representation, the respondents were first stratified into 6 according to the 6 health zones of Nigeria. Next, 20% of the registered members of SOGON from each health zone was calculated to obtain the minimum sample size for the corresponding zone. The calculated minimum sample sizes for the 6 health zones were as follow; South-West = 35, South-South = 27, South-East = 22, North-Central = 13, North-West = 6 and North-East = 6. To increase statistical power of the study whilst maintaining the zonal proportionality of the participants, a maximum of 20% increment of the calculated minimum sample size was allowed for each zone. Hence the maximum expected sample size was 134. The expected range of participants from each zone was as follow; South-West zone = 35-42, South-South zone = 27-33, South-East = 22-27, North Central = 13-16, North-East = 6-8, North-West = 6-8. There was plan to conduct a follow-up survey in any zone that did not have its minimum sample size.
For the interview process, the purposes of the study were explained individually to consecutive attendees at the SOGON annual conference immediately following registration and they were solicited to participate in the study. Those who consented were interviewed with the aid of self-administered semi-structured questionnaire until the maximum sample size for each zone was reached. The questionnaire captured socio-demographic data, length of practice as a Gynaecologist, geographical location of practice, menopausal symptoms ever encountered by the respondents in their practices, the treatments ever offered for severe menopausal symptoms, their attitude to hormone replacement therapy, and their practice of hormone replacement therapy.
Data entry, collation and analysis were done with SPSS statistical software version 10 for descriptive statistics, Z-test and Chi-Square test as appropriate. P value of = 0.05 was considered significant (at 95% confidence interval). This study was approved by the research ethics committee of the University of Nigeria Teaching Hospital, Enugu Nigeria.
Results
Out of the 151 eligible conference attendees interviewed, 126 returned their completed questionnaires, giving a response rate of 83%. Nigeria is divided into 6 health zones. The zonal distribution of respondents was as follow: South-West = 38, South-South = 32, South-East = 27, North-Central = 14, North-East = 8 and North-West = 7. The ages of the participants ranged from 35 years to 61 years with a mean of 47.71 ± 0.84 years. They had practiced as specialist Gynaecologists for a mean of 6.83 ± 0.54 years with a range of 1 to 34 years. On the average, a Gynaecologist saw one patient with menopausal symptoms every three months (range: 0-3 patients per month). The main menopausal symptoms they had ever encountered are shown in Table 1. The commonest symptom was hot flushes while fracture and urinary symptoms were uncommonly reported. Table 2 shows the treatments ever offered by the Gynaecologists for severe menopausal symptoms. Reassurance and anxiolytics were the common treatments while HRT was infrequently used. Attitude to HRT was assessed by asking whether they considered HRT more effective than the non-hormonal therapies for the treatment of severe menopausal symptoms. 6.3% agreed that HRT is more effective than the other treatment modalities they offered while 93.7% disagreed. The reasons for non-use of HRT are shown in Table 3. Non-availability of HRT was the reason given by 59.5% of the respondents for non-use of HRT while only 10.3% of respondents gave side effects of HRT as their reason for its non-use.
Discussion
The zonal distribution of participants in this study, especially the North-South disparity, is consistent with the national distribution of Gynaecologists in Nigerian [19, 20] and each health zone was represented by at least 20% of its registered Gynaecologists. The study revealed that although most reported menopausal symptoms [17, 18] are prevalent amongst Nigerian women, the average Nigerian Gynaecologist sees only a small number of such cases each year. Whereas hot flushes and psychosomatic symptoms are commonly reported, uro-genital symptoms are less commonly reported while fracture is rarely reported. The widespread social inhibition and secrecy about female sexual and genital matters in most Nigerian communities may be responsible for the low reporting of sexual and genital symptoms such as vaginal dryness, dyspareunia, reduced libido and urinary symptoms. Women are much less embarrassed about reporting the non-genital and non-sexual complaints such as hot flushes, crawling sensation, insomnia, irritability and depression, hence the apparent higher prevalence of these non-genital and non-sexual symptoms. Information from focused group discussions however, revealed that Nigerian menopausal women experience the urinary and genital symptoms. These symptoms are usually presented to the clergy, spiritualists and traditional medicine men rather than to the hospitals [18]. Nkwo et.al [17] recorded only one case of fracture while Agwu et.al [18] reported no case of fracture in their studies. The black woman is blessed with a large bone mass which may explain the protection of Nigerian women from menopausal fracture. On the other hand, women with menopause-induced osteoporotic fracture are more likely to be found in orthopaedic wards and homes and not in the Gynaecology clinic and church service (as in the study of Nkwo et.al) or in a village square meeting (as in the study of Agwu et.al) and so may have been unintentionally excluded by the study designs!
The common use of reassurance and anxiolytics for treating menopausal symptoms was probably influenced by the high prevalence of psychosomatic symptoms. It is however more likely that such treatments resulted from a common but wrong opinion held by many Nigerian doctors in the past that the typical Nigerian women do not manifest severe menopausal symptoms, hence reassurance evolved as the first line management of menopausal symptoms. Women who did not respond to reassurance were given analgesics and anxiolytics as well. By practice tradition, generations of Nigerian doctors learnt to treat menopausal symptoms, including severe symptoms, with reassurance, anxiolytics and analgesics. Although some societal privileges enjoyed by menopausal women in some Nigerian communities tend to modulate the expression of menopausal symptoms; they do not eliminate them [17]. Indeed, some Nigerian women are known to have presented with quite severe menopausal symptoms that are not mitigated by reassurance, anxiolytics or analgesics but by hormonal or effective non-hormonal therapies.
It is worrisome that most of the respondents (93.7% of them) did not consider HRT more effective than reassurance, anxiolytics and analgesics for severe menopausal symptoms. This revealed an important knowledge gap amongst the respondents, leading to suboptimal treatment of these symptoms. The superiority of HRT over placebos for severe menopausal symptoms is established [5, 7, 14, 16]. Moreover, reassurance, analgesics, anxiolytics, and multivitamins are not among the documented effective non-hormonal therapies for severe menopausal symptoms [10]; their widespread use by Nigerian Gynaecologists is not based on any documented evidence. Caution in the use of HRT resulted from its potential cardiovascular and oncogenic side effects following prolonged usage [12, 15]. Incidentally, only 10.3% of the respondents withheld the use of HRT for fear of its side effects.
Patient satisfaction is an important determinant of health seeking behaviour. Dissatisfaction with treatments offered by the physicians might be the major reason why only few women present to them with menopausal symptoms. Instead, the women seek treatment from alternative sources including botanical preparations some of which are quite popular among the women possibly as the result of their effectiveness in relieving the menopausal symptoms. There is an urgent need for Nigerian Gynecologists to regain the confidence of the Nigerian menopausal women by offering them effective management of their menopausal symptoms. The Society of Gynaecology and Obstetrics of Nigeria (SOGON) and the Post Graduate Medical Colleges are encouraged to take particular note of studies on practice patterns and institute mandatory continuing medical education programmes to bridge observed gaps and so encourage evidence-based best practices rather medical practice based on existing traditions.
Conclusion
Most Nigerian Gynaecologists offered suboptimal and ineffective treatments for severe menopausal symptoms. This resulted from medical practice that is still strongly influenced by tradition rather than evidence. Continuing medical education of physicians is recommended to encourage evidence-based best practice of medicine in Nigeria.
Author's contributions
PN conceived the study, prepared the questionnaire, supervised the data collection, collation and analysis and wrote the manuscript.
References
Frere G: Mean age of menopause and menarche in South Africa. South African Journal of Medical Sciences. 1971, 36: 21-4.
Mekinlay SM, Feffreys K, Thompson B: An I nvestigation of the age of menopause. Journal of Biosocial Sciences. 1972, 4: 161-3.
Whitehead MI: Menopause. Dewhurst's Textbook of Obstetrics and Gynaecology for Postgraduate Students. Edited by: Edmonds DK. 1999, Edinburgh. Blackwell Science, 441-6
Brincat M, Savvas M, Studd J: The menopause. Clinical Gynaecology. Edited by: Varma TR. 1990, London. Edward Arnold, 742.
Maclennan AH, Broadbent JL, Lester S, Moore V: Oral estrogen and combined estrogen/progestogen therapy versus placebo for hot flushes. Cochrane Data Base Syst Rev. 2004, 18 (4): C.D002978.
Bhavnani BR, Strickler RC: Menopausal hormone therapy. J Obstet Gynecol Can. 2005, 27 (2): 137-62.
Clayden JR, Bell JW, Pollard P: Menopausal flushing: double blind trial of a non-hormonal preparation. British Medical Journal. 1994, 1 (5905): 409-12. 10.1136/bmj.1.5905.409.
Alcoff JM, Cambell D, Tribble D, Oldfield B, Cruess D: Double blind placebo controlled, cross-over trial of propranolol as treatment for menopausal vaso-motor symptoms. Clinical therapeutics. 1981, 3: 356-64.
Harrison RF: Ethamsylate in the treatment of climacteric flushing. Maturitas. 1981, 3: 31-7. 10.1016/0378-5122(81)90017-7.
Deepti Cheema, Arri Coomarasamy, Tarek El-Toukhy: Non-hormonal therapy of post-menopausal vasomotor symptoms: a structured evidence-based review. Arch Gynecol Obstet. 2007, 276: 463-469. 10.1007/s00404-007-0390-9.
Belchetz PE: Hormonal treatment of post menopausal women. New Enland Journal of Medicine. 1994, 330 (15): 1062-71. 10.1056/NEJM199404143301508.
Lobo RA: Benefits and risks of estrogen replacement therapy. American Journal of Obstetrics and Gynecology. 1995, 173 (3 pt 2): 982-9. 10.1016/0002-9378(95)90247-3.
Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J: Writing Group for the Women's Health Initiative Investigators. Risk and benefits of estrogen plus progestin in healthy post menopausal women. Principal result of the Women's Health Initiatives Randomized Investigation. JAMA. 2002, 288 (3): 321-333. 10.1001/jama.288.3.321.
Nelson HD, Humphrey LL, Nygren P, Teusch MS, Allan JD: Post menopausal hormone replacement therapy scientific review (both benefits and harms). JAMA. 2002, 288 (7): 872-81. 10.1001/jama.288.7.872.
Canderelli R, Leccesse LA, Miller NL, Unruh Davidson J: Benefits of hormone replacement therapy in postmenopausal women. J Am Acad Nurse Pract. 2007, 19 (12): 635-41. 10.1111/j.1745-7599.2007.00269.x.
March 2007 Position Statement of the North American Menopause Society: Estrogen and Progestogen in Peri and Postmenopausal women. Menopause. 2007, 14 (2): 168-182. 10.1097/gme.0b013e31803167ab.
Peter Nkwo, Hyacith Onah: Positve attitude to menopause and improved quality of life among Igbo women in Nigeria. International Journal of Gynecology and Obstetrics. 2008, 103 (1): 71-72. 10.1016/j.ijgo.2008.05.006.
Agwu UM, Umeora OUJ, Ejkeme BN: Patterns of menopausal symptoms and adaptive ability in a rural population in south-east Nigeria. Journal of Obstetrics and Gynaecology. 2008, 28 (2): 217-221. 10.1080/01443610801915637.
Society of Gynaecology and Obstetrics of Nigeria (SOGON): 2005 Membership Directory. 2006, Nigeria; SOGON
National Population Commission (NPC), Federal Republic of Nigeria, and ORC Macro International: Nigeria Demographic and Health Survey 2003. 2004, Calverton, MD, USA: NPC and ORC Macro International
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6874/9/30/prepub
Acknowledgements
The contributions of the following persons are hereby gratefully acknowledged: Dr. Azubike Onyebuchi, Dr. Mike Nwafor, Dr. George Ugwu and Dr. Ogbuefi who helped to administer the questionnaire, Mr. Douglas Ibe who collated and analyzed the data and Dr HE Onah who reviewed the article in-house.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author declares that they have no competing interests.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Nkwo, P.O. Suboptimal management of severe menopausal symptoms by Nigerian Gynaecologists: a call for mandatory continuing medical education for physicians. BMC Women's Health 9, 30 (2009). https://doi.org/10.1186/1472-6874-9-30
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6874-9-30