Abstract
Purpose
This study aimed to measure the prevalence of menopausal symptoms in patients attending a multidisciplinary model of care clinic at their initial clinic visit and their subsequent follow-up consultation using a validated patient-reported outcome measure to assess whether menopausal symptoms after cancer had improved.
Methods
A retrospective review was conducted of patients attending the clinic in a 12-month period in 2017 (n = 189). Recorded variables included patient demographics, details of index cancer, previous treatments, and menopausal symptom management strategies. Severity of menopausal symptoms was evaluated using the Greene Climacteric Scale. The extent to which patients were bothered by symptoms was combined into two categories and dichotomized (present/absent). Differences in symptom prevalence between the initial consultation and first follow-up visit were examined using McNemar’s test.
Results
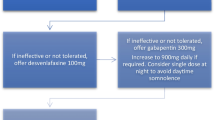
The majority of patients attending the clinic had a history of breast cancer (72%). Fifty-five percent of patients were prescribed a non-hormonal therapy at their initial visit, most commonly gabapentin. Significantly fewer patients reported being bothered by hot flushes, fatigue, sleep difficulties, and loss of interest in sex, anxiety, or troubles concentrating at the first follow-up visit compared to their initial consultation (p < 0.01).
Conclusion
In this study, there was an improvement in self-reported menopausal symptoms in a significant proportion of cancer survivors attending a multidisciplinary menopause clinic between their initial and first subsequent follow-up consultations.
Similar content being viewed by others
Availability of data and material
Available on request.
Code availability
NA.
References
Nelson HD (2008) Menopause. Lancet 371(9614):760–770
Guthrie JR, Dennerstein L, Taffe JR, Donnelly V (2003) Health care-seeking for menopausal problems. Climacteric 6(2):112–117
Whiteley J, DiBonaventura M, Wagner JS, Alvir J, Shah S (2013) The impact of menopausal symptoms on quality of life, productivity, and economic outcomes. J Womens Health (Larchmt) 22(11):983–990
Marino JL, Saunders CM, Emery LI, Green H, Doherty DA, Hickey M (2014) Nature and severity of menopausal symptoms and their impact on quality of life and sexual function in cancer survivors compared with women without a cancer history. Menopause 21(3):267–274
Hickey M, Emery LI, Gregson J, Doherty DA, Saunders CM (2010) The multidisciplinary management of menopausal symptoms after breast cancer: a unique model of care. Menopause 17(4):727–733
Kligman L, Younus J (2010) Management of hot flashes in women with breast cancer. Curr Oncol 17(1):81–86
Gupta P, Sturdee DW, Palin SL et al (2006) Menopausal symptoms in women treated for breast cancer: the prevalence and severity of symptoms and their perceived effects on quality of life. Climacteric 9(1):49–58
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021.
Breast cancer in Australia statistics. Australian Government. https://www.canceraustralia.gov.au/affected-cancer/cancer-types/breast-cancer/breast-cancer-australia-statistics. Accessed 12 December 2020
Holmberg L, Iversen OE, Rudenstam CM et al (2008) Increased risk of recurrence after hormone replacement therapy in breast cancer survivors. J Natl Cancer Inst 100(7):475–482
Cohen PA, Brennan A, Marino JL, Saunders CM, Hickey M (2017) Managing menopausal symptoms after breast cancer - A multidisciplinary approach. Maturitas 105:4–7
Cancer Australia. Management of menopausal symptoms in women with a history of breast cancer. URL: https://canceraustralia.gov.au/clinical-best-practice/breast-cancer/management-menopausal-symptoms-women-history-breast-cancer-%E2%80%93-clinical-practice-guideline Accessed March 3 2017. 2016.
Sinno AK, Pinkerton J, Febbraro T et al (2020) Hormone therapy (HT) in women with gynecologic cancers and in women at high risk for developing a gynecologic cancer: A Society of Gynecologic Oncology (SGO) clinical practice statement: This practice statement has been endorsed by The North American Menopause Society. Gynecol Oncol 157(2):303–306
Fleissig A, Jenkins V, Catt S, Fallowfield L (2006) Multidisciplinary teams in cancer care: are they effective in the UK? Lancet Oncol 7(11):935–943
Greene JG (1998) Constructing a standard climacteric scale. Maturitas 29(1):25–31
Peate M, Saunders C, Cohen P, Hickey M. Who is managing menopausal symptoms, sexual problems, mood and sleep disturbance after breast cancer and is it working? Findings from a large community-based survey of breast cancer survivors. Breast Cancer Research and Treatment 2021.
Dorjgochoo T, Gu K, Kallianpur A et al (2009) Menopausal symptoms among breast cancer patients 6 months after diagnosis: a report from the Shanghai Breast Cancer Survival Study. Menopause 16(6):1205–1212
Shams T, Firwana B, Habib F et al (2014) SSRIs for hot flashes: a systematic review and meta-analysis of randomized trials. J Gen Intern Med 29(1):204–213
Guthrie KA, LaCroix AZ, Ensrud KE et al (2015) Pooled Analysis of Six Pharmacologic and Nonpharmacologic Interventions for Vasomotor Symptoms. Obstet Gynecol 126(2):413–422
Tran S, Hickey M, Saunders C, Ramage L, Cohen PA. Nonpharmacological therapies for the management of menopausal vasomotor symptoms in breast cancer survivors. Supportive Care in Cancer 2020.
Yoon SH, Lee JY, Lee C, Lee H, Kim SN (2020) Gabapentin for the treatment of hot flushes in menopause: a meta-analysis. Menopause 27(4):485–493
Shan D, Zou L, Liu X, Shen Y, Cai Y, Zhang J (2020) Efficacy and safety of gabapentin and pregabalin in patients with vasomotor symptoms: a systematic review and meta-analysis. Am J Obstet Gynecol 222(6):564–79.e12
Pandya KJ, Morrow GR, Roscoe JA et al (2005) Gabapentin for hot flashes in 420 women with breast cancer: a randomised double-blind placebo-controlled trial. Lancet 366(9488):818–824
Christakis MK, Strobino DM, Shen W (2019) A critical appraisal of vasomotor symptom assessment tools used in clinical trials evaluating hormone therapy compared to placebo. Menopause 26(11):1334–1341
Author information
Authors and Affiliations
Contributions
Jade Hollingworth: substantial contribution to the conception and design, acquisition of data, drafted the work, and approved the version to be published.
Lucy Walsh, Stephanie Tran: substantial contribution to the acquisition of data, revised the work critically, and approved the version to be published.
Lesley Ramage, Manju Ambekar, Jane Weeks, Lucy Williams: substantial contribution to the conception of the work, revised the work critically, and approved the version to be published.
Shavita Patel-Brown: substantial contribution to the acquisition of data, revised the work critically, and approved the version to be published.
Paul Cohen: substantial contribution to the conception and design, interpretation of data, revised the work critically, and approved the version to be published.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval for the study was granted by the Womens and Newborns Health Service Ethics Committee (Reference 27240, approved 6 June 2019).
Consent to participate
The study was deemed low risk to participants and a waiver of consent was granted in accordance with the Australian National Health and Medical Research Council National Statement on Ethical Conduct in Human Research (https://www.nhmrc.gov.au/about-us/publications/national-statement-ethical-conduct-human-research-2007-updated-2018; accessed 19 October 2020).
Consent for publication
Yes.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hollingworth, J., Walsh, L., Tran, S. et al. Does a multidisciplinary menopausal symptoms after cancer clinic reduce symptoms?. Support Care Cancer 30, 2245–2252 (2022). https://doi.org/10.1007/s00520-021-06637-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06637-4