Abstract
Background
Nonspecific back pain is common, disabling, and costly. Therefore, we assessed effectiveness of osteopathic manipulative treatment (OMT) in the management of nonspecific low back pain (LBP) regarding pain and functional status.
Methods
A systematic literature search unrestricted by language was performed in October 2013 in electronic and ongoing trials databases. Searches of reference lists and personal communications identified additional studies. Only randomized clinical trials were included; specific back pain or single treatment techniques studies were excluded. Outcomes were pain and functional status. Studies were independently reviewed using a standardized form. The mean difference (MD) or standard mean difference (SMD) with 95% confidence intervals (CIs) and overall effect size were calculated at 3 months posttreatment. GRADE was used to assess quality of evidence.
Results
We identified 307 studies. Thirty-one were evaluated and 16 excluded. Of the 15 studies reviewed, 10 investigated effectiveness of OMT for nonspecific LBP, 3 effect of OMT for LBP in pregnant women, and 2 effect of OMT for LBP in postpartum women. Twelve had a low risk of bias. Moderate-quality evidence suggested OMT had a significant effect on pain relief (MD, -12.91; 95% CI, -20.00 to -5.82) and functional status (SMD, -0.36; 95% CI, -0.58 to -0.14) in acute and chronic nonspecific LBP. In chronic nonspecific LBP, moderate-quality evidence suggested a significant difference in favour of OMT regarding pain (MD, -14.93; 95% CI, -25.18 to -4.68) and functional status (SMD, -0.32; 95% CI, -0.58 to -0.07). For nonspecific LBP in pregnancy, low-quality evidence suggested a significant difference in favour of OMT for pain (MD, -23.01; 95% CI, -44.13 to -1.88) and functional status (SMD, -0.80; 95% CI, -1.36 to -0.23), whereas moderate-quality evidence suggested a significant difference in favour of OMT for pain (MD, -41.85; 95% CI, -49.43 to -34.27) and functional status (SMD, -1.78; 95% CI, -2.21 to -1.35) in nonspecific LBP postpartum.
Conclusion
Clinically relevant effects of OMT were found for reducing pain and improving functional status in patients with acute and chronic nonspecific LBP and for LBP in pregnant and postpartum women at 3 months posttreatment. However, larger, high-quality randomized controlled trials with robust comparison groups are recommended.
Similar content being viewed by others
Background
Low back pain (LBP) is defined as pain located below the costal margin and above the inferior gluteal folds[1]. Specific causes of LBP are uncommon, accounting for less than 15% of all back pain[2]. About 85% of patients with isolated LBP cannot be given a precise pathoanatomical diagnosis[3]. Nonspecific LBP has been defined as tension, soreness, and/or stiffness in the lower back region for which it is not possible to identify a specific cause of the pain[4]. It commonly leads to a loss of function and limitations in activities and participation in social life[5]. Because LBP pain is common in Western industrial societies, the economic consequences of back pain are enormous[6], and the effect on quality of life is substantial[7].
Back pain in pregnant and postpartum women is also common. The prevalence of LBP in pregnancy ranges from 24% to 90%, although it is most commonly estimated at 40%-50%[8–10]. Prevalence increases with the duration of pregnancy and is at the highest point in the third trimester[11, 12]. The cause of pain appears to be nonspecific and may be related to changes in body posture with the development of joint, ligament, and myofascial dysfunctions[13, 14]. The prevalence of LBP in postpartum women increases in the year after delivery, with estimates from 28% after 3 months to over 50% after 5 months and 67% after 12 months[15–18].
Osteopathy is a health approach that emphases the role of the musculoskeletal system in health and promotes optimal function of the tissues of the body by using a variety of manual techniques to improve the function of the body[19]. In the United States, practitioners are known as osteopathic physicians and have full medical licence. Osteopathic manipulative treatment (OMT) typically involves an eclectic range of manual techniques, which may include soft tissue stretching, spinal manipulation, resisted isometric ‘muscle energy’ stretches, visceral technique, or exercise prescription, for example. Treatment is characterised by a holistic approach to the patient, and OMT may be applied to many regions and tissues of the body, sometimes remote from the symptomatic area and at the clinical judgement of the practitioner[19–21].
Patients with LBP visit osteopaths for treatment, although the number of patients consulting osteopaths is not clear. In the United Kingdom, osteopaths were estimated to perform 4.38 million treatments in 1998[22]. Lumbar symptoms are the most common presentation in osteopathic practice in the United Kingdom, and, in a national pilot survey[23] and a snap-shot survey[24], accounted for 36% and 46% of presenting symptoms in patients, respectively. In Australia, the osteopathic profession is relatively small, and of those patients with LBP who chose to see a practitioner, medical practitioners (22.4%) and chiropractors (19.3%) are the most popular care providers, with only 2.7% of patients seeing osteopaths[25]. Despite this, LBP is the most common patient presentation in osteopathic practices[26].
In the United States, osteopathic physicians are more likely to provide LBP care than their allopathic medical counterparts[27].
To our knowledge, only 2 systematic reviews exist for osteopathic treatment of LBP. In 2005, Licciardone et al.[28] published the first systematic review of OMT for LBP and concluded that OMT significantly reduced LBP. This review had a number of limitations and was criticized because it did not differentiate between OMT and single manual techniques[29] and because single techniques do not reflect osteopathic clinical practice. Further, it combined dichotomous and continuous outcomes, combined studies with specific and nonspecific back pain, lacked a risk of bias evaluation, and contained a unit of analysis error. Given these shortcomings, reservations remain concerning the authors’ conclusions[29].
In 2012, Orrock and Myers[30] published another systematic review of OMT for LBP. This review only included studies of chronic nonspecific LBP and was limited to those published in English[30]. Only 2 studies met their specific search criteria, so no meta-analysis or robust conclusions were possible.
The objective of the current review was to examine the effectiveness of OMT for improving pain and functional status in LBP patients as compared to control treatments (no treatment, sham, and all other treatments) for adults in randomized clinical trials. Although 2 systematic reviews have been published on this topic, we were aware of recent, non-English studies that were not included in the previous reviews. Further, we intended to search the non-published ‘grey’ literature for studies which have not been published in journals or books, as recommended by the Cochrane Collaboration[31] for preparing and updating high-quality systematic reviews. We expected that using rigorous methodology and an extensive search without language restriction would provide a more comprehensive insight into the effectiveness of this intervention.
Methods
Criteria for considering studies for the current review
Types of studies
Only randomized controlled studies (RCTs) were included in the current review. Potential studies could be published or unpublished (grey literature) in any language.
Types of participants
We included studies with adults (older than 18 years) with nonspecific LBP (i.e., pain between the lumbo-pelvic region and the 12th rib) and without any limitation of the duration of the pain period (acute, subacute, or chronic back pain). We excluded studies which included participants with specific LBP (back pain with a specific cause, e.g., compression fracture, a tumour or metastasis, ankylosing spondylitis, infection).
There is a high prevalence of LBP associated with pregnancy and the postpartum period. Pregnancy and postpartum can be considered risk factors for nonspecific LBP, but they are not considered specific pathologies (e.g., infection, tumour, osteoporosis, ankylosing spondylitis, fracture, inflammatory conditions). Therefore, these groups can have specific or nonspecific LBP. For this reason we included studies that examined nonspecific LBP in pregnant and postpartum women, but presented these results as separate comparisons, even though other systematic reviews have excluded this subgroup without clear justification[32, 33].
Types of interventions
Treatment was required to be an ‘authentic’ OMT intervention where the practitioners were identified as osteopaths or osteopathic physicians and had a choice of manual techniques and judgment was required for the treatment selection, without any technique restrictions or standardised treatment protocols. The techniques chosen were based on the treating examiner’s opinion of what techniques would be most appropriate for a given patient. This eclectic, pragmatic approach best represents ‘real-world’ osteopathic practice[34–36], as opposed to treatment following an established study protocol that applies an isolated manual technique or set of techniques.
Therefore, our inclusion criteria were RCTs of OMT for nonspecific LBP where the treating practitioner was an osteopath or osteopathic physician who used clinical judgment to determine the treatment performed. Only studies where an effect size could be assigned to the OMT intervention were considered. If co-interventions were used, they also had to be performed in the control group. Studies were excluded that used an intervention of a single manual technique, such as high-velocity manipulation.
Types of comparisons
Studies with any type of comparison intervention (e.g., manual therapy, usual care, sham treatment, untreated) were included.
Types of outcome measures
Only patient-reported outcome measures were evaluated.
Primary outcomes
The primary outcomes were pain and functional status. Pain was measured by visual analogue scale (VAS), number rating scale (NRS), or the McGill Pain Questionnaire. Studies measured functional status using the Roland-Morris Disability Questionnaire, Oswestry-Disability Index, or another valid instrument. For the meta-analysis, the outcome measure (pain or functional status) closest to the 3 month interval was used, even if studies used various time point measurements, because this interval was common for most of the included studies.
Secondary outcome
These outcomes included any kind of adverse event.
Data sources and searches
A systematic literature search was performed in October 2013 in the following electronic databases: Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, Embase, CINAHL, PEDro, OSTMED.DR, and Osteopathic Web Research. The following search terms were used: low back pain, back pain, lumbopelvic pain, dorsalgia, osteopathic manipulative treatment, OMT, and osteopathic medicine. In addition to the listed databases, an ongoing trial database was also screened (metaRegister of Controlled Trialshttp://controlled-trials.com/mrct/). Our search was supplemented by citation tracking of the identified trials and a manual search in the reference lists for all relevant papers that were not listed in the electronic databases. Table 1 shows an example of the applied search strategy in MEDLINE.
Data collection and analysis
Study selection
All authors independently screened titles and abstracts of the results identified by our search strategy. Potentially eligible studies were read in full text and independently evaluated for inclusion in the current review.
Data extraction and quality assessment
The authors independently extracted data from identified studies using a standardized data extraction form.
Dealing with missing data
If the article did not contain sufficient information, the authors were contacted for additional information. When standard deviations (SDs) were not reported, we estimated these from the confidence intervals (CIs) or other measures of variance, where possible. When the results were reported in median and interquartile range (IQR), we expected that the relation of median to mean was 1:1[37] and IQR to SD was 1.35:1[31]. If the normal distribution was skewed, we calculated the missing SD from the SDs of included studies that had similar results for outcome, comparison, and duration of pain[31].
Assessment of heterogeneity
Heterogeneity refers to the variation in study outcomes between studies and is useful for the interpretation of meta-analysis results. Assessment of heterogeneity was based on the calculation of I2. The Cochrane Collaboration[31] provides the following interpretation of I2: 0% to 30%, might not be important; 30% to 60%, may represent moderate heterogeneity; 50% to 90%, may represent substantial heterogeneity; and 75% to 100%, considerable heterogeneity.
Unit of analysis issues
In cases where 3 or more interventions were evaluated in a single study, we included each pair-wise comparison separately. In these instances, the total number of participants in the OMT intervention group was divided approximately evenly among the comparison groups.
Assessment of risk of bias in included studies
The methodological quality of the studies was assessed using the Risk of Bias tool of the Cochrane Back Review Group[38]. Discussion and consensus between the researchers were used to resolve disagreements about the methodological quality of the RCTs included in the current review. Every Risk of Bias criterion was scored as ‘low risk’, ‘high risk’, or ‘unclear’ and included assessment of randomization, blinding, baseline comparability between groups, patient compliance, and dropping out. In line with recommendations from the Cochrane Back Review Group, studies were rated as having ‘low risk’ when at least 6 criteria were met and the study had no serious flaws (e.g., large drop-out rate). A dropout rate of greater than 50% was defined as a serious flaw and the comparison was excluded from quantitative analysis. When information was missing from the published studies and the authors could not be contacted or when the information was no longer available, the criteria were scored as ‘unclear’.
Measures of treatment effect
Data for the meta-analysis was analysed using Review Manager (RevMan, Version 5.2., Nordic Cochrane Centre,http://ims.cochrane.org/revman). For measurement of pain, the NRS or VAS scores from the included studies were converted to a 100-point scale and the mean difference (MD) with 95% CIs was calculated in a random effects model. For functional status, the standard mean difference (SMD) was also used in a random effects model. Because only 1 study was included that examined acute LBP[39] and 3 other studies examined patients with both acute and chronic LBP[40–42], we grouped the studies into 4 groups for meta-analyses: acute and chronic LBP, chronic LBP (pain for a duration of greater than 3 months), LBP in pregnant women, and LBP in postpartum women.
Assessment of clinical relevance
Assessment of clinical relevance was made using the recommendations of the Cochrane Back Review Group. Therefore, we defined a small effect as MD less than 10% of the scale (e.g., 10 mm on a 100 mm VAS) and SMD or ‘d’ scores less than 0.5. A medium effect was defined as MD 10% to 20% of the scale and SMD or ‘d’ scores from 0.5 to 0.8. A large effect was defined as MD greater than 20% of the scale and SMD or ‘d’ scores greater than 0.8[38].
Data synthesis
The overall quality of the evidence for each outcome in the included studies was assessed using the GRADE approach[43, 44], as recommended by the updated Cochrane Back Review Group method guidelines[38]. The GRADE approach specifies 4 levels of quality, the highest rating being for RCT evidence. Authors of systematic reviews can downgrade this evidence to moderate, low, or even very low quality evidence, depending on the evaluation of quality of the evidence for each outcome against 5 key domains, which are (1) limitations in design (downgraded when more than 25% of the participants were from studies with a high Risk of Bias), (2) inconsistency of results (downgraded in the presence of significant statistical heterogeneity and inconsistent findings), (3) indirectness (i.e., generalisability of the findings, downgraded when more than 50% of the participants were outside the target group), (4) imprecision (downgraded when the total number of participants was less than 400 for each continuous outcome), and (5) other (such as publication bias)[33].
For the current review, the following definitions for quality of the evidence definitions were followed. For high quality, further research was very unlikely to change our confidence in the estimate of effect. There were also consistent findings among at least 75% of RCTs with no limitations of the study design and no known or suspected reporting biases. For moderate quality, further research was likely to have an important impact on confidence in the estimate of effect and may have changed the estimate; one of the domains was not met. For low quality, further research was very likely to have an important impact on confidence in the estimate of effect and was likely to change the estimate; 2 of the domains were not met. For very low quality, there was great uncertainty about the estimate; 3 of the domains were not met. For no evidence, no RCTs were identified that addressed the outcome. The research methods and reporting of this study adhered to the PRISMA guidelines[45].
Results
Included studies
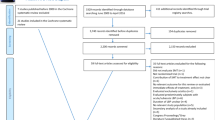
The search strategy of the current review identified 307 studies (Figure 1). Fifteen trials[39–42, 46–56] with 18 comparison groups and 1502 participants were included in the qualitative and quantitative analysis. Tables 2 and3 summarize the important characteristics of the included studies. Of the 15 included studies, 6 were retrieved from the grey literature[42, 46, 48, 53–55]. Six studies came from Germany[42, 46, 48, 53–55], 5 from the United States[39, 40, 49–51], 2 from the United Kingdom[41, 47], and 2 from Italy[52, 56]. Ten studies investigated the effectiveness of OMT for back pain[39–42, 46, 47, 50–52, 56], 3 investigated the effect of OMT for LBP in pregnant women[48, 49, 53], and 2 investigated the effect of OMT for LBP in postpartum women[54, 55]. All included studies reported on pain and back pain-specific functional status, except for 1 study[41] that only reported pain.
Excluded studies
Sixteen of the 31 identified studies were excluded from our review (Figure 1). In 3 studies, the treatment involved only a single technique[57–59], and in 1 study the treatment was based on local fascial manipulations[60]. Seven studies did not use RCT methodology[61–63] (Conrady A, Döring R: Does osteopathic treatment influence immune parameters in patients with chronic low back pain? A pre-post pilot trial, unpublished D.O. thesis, Akademie für Osteopathie, 2010; Kofler G: Osteopathy for back and pelvic pain in pregnancy, unpublished D.O. thesis, Wiener Schule für Osteopathie, 2006; Lutzelberger N: Does osteopathic treatment influence thoracolumbar junction back pain positively? unpublished D.O. thesis, Akademie für Osteopathie, 2009; Müller P: Nonspecific, pseudoradicular low back pain after lumbar nucleotomy, unpublished D.O. thesis, Akademie für Osteopathie, 2006), and 1 study focused on specific LBP[5]. In another study, we could not differentiate the back pain results from the neck pain results[64]. One study used a non-validated disability index and did not report pain scores[65]. Another study focused on outcomes other than pain and functional status[66]. One pilot study was excluded because it focused only on feasibility[67].
Risk of bias
Thirteen of the included studies in the meta-analysis had high internal validity (low risk of bias) (Table 4). The study by Licciardone et al.[51] from 2003 and Gibson[41] were found to have a high risk of bias, with both studies having only 5 criteria each assessed as low risk. Additionally, the second comparison group (OMT/group exercise) in the study by Chown et al.[47] was rated as having a high risk of bias because only 40% of the participants in the exercise group completed all therapy sessions. This comparison was excluded. In the 2009 study by Licciardone et al.[49], 83 of 144 participants withdrew before the last treatment. Although we determined this study had a high risk of bias, we included it in our analysis because the reasons for the dropouts were described and an intention-to-treat-analysis (last observation carried forward) was performed.
Effect of interventions
Results are presented in the forest plots (Figures 2,3,4,5,6,7,8, and9) and in the summary of findings tables (Tables 5,6,7, and8). All results are based on measures which were closest to 3 months posttreatment.
OMT versus other interventions for acute and chronic nonspecific low back pain
Ten studies with 12 comparison groups and 1141 participants were analysed for the effect of OMT for pain in acute and chronic LBP. Six studies reported a significant effect on pain in favour of OMT[39, 42, 46, 50, 52, 56], 3 studies reported a non-significant effect in favour of OMT[40, 41, 51], and 3 studies reported a non-significant effect in favour of the control treatment[41, 47, 51]. For pain, there was moderate-quality evidence (downgraded due to inconsistency) that OMT had a significant effect on pain relief (MD, -12.91; 95% CI, -20.00 to -5.82) (Figure 2 and Table 5).
For functional status, which was based on 9 studies with 10 comparisons and 1046 participants, there was moderate-quality evidence (downgraded due to inconsistency) of a significant difference in favour of OMT (SMD, -0.36; 95% CI, -0.58 to -0.14). Four studies reported a significant effect in favour of OMT[42, 46, 52, 56], 3 studies reported a non-significant effect in favour of OMT[39, 40, 47], and 1 study reported a non-significant effect in favour of the control group[51]. For 1 study[50], we estimated the effect size with a confidence interval which was very near to 0 (SMD, -0.19; 95% CI, -0.38 to -0.01) and significant (P = .04), whereas the authors reported that the results were not significant (P = .07, based on median and interquartile range) (Figure 3 and Table 5).
OMT versus other interventions for chronic nonspecific low back pain
For the outcome of pain and based upon 6 studies[46, 47, 50–52, 56] with 7 comparisons and 769 participants, there was moderate-quality evidence (downgraded due to inconsistency) of a significant difference in favour of OMT (MD, -14.93; 95% CI, -25.18 to -4.68) (Figure 4 and Table 6).
For functional status, 3 studies reported a significant improvement for OMT[46, 52, 56], 1 reported a non-significant effect for OMT[47], and 1 reported an effect for the control group[51] (Figure 5). There was moderate-quality evidence (downgraded due to inconsistency) for a significant difference in favour of OMT (SMD, -0.32; 95% CI, -0.58 to -0.07) (Figure 5 and Table 6).
OMT versus usual obstetric care, sham ultrasound, and untreated for nonspecific low back pain in pregnant women
Three studies with 4 comparisons and 242 participants were included for the analysis of OMT for LBP in pregnant women. Two of these studies showed a significant improvement[48, 53] following OMT, and 1 study[49] showed a non-significant improvement. There was low-quality evidence (downgraded due to inconsistency and imprecision) for a significant difference in favour of OMT for pain (MD, -23.01; 95% CI, -44.13 to -1.88) and functional status (SMD, -0.80; 95% CI, -1.36 to -0.23) (Figures 6 and7, Table 7).
OMT versus untreated for nonspecific low back pain in postpartum women
Two studies examining OMT for LBP in postpartum women were found, both reporting significant improvement following OMT[54, 55]. There was moderate-quality evidence (downgraded due to imprecision) for a significant difference in favour of OMT for pain (MD, -41.85; 95% CI, -49.43 to -34.27) and functional status (SMD, -1.78; 95% CI, -2.21 to -1.35) (Figures 8 and9, Table 8).
Adverse events
Of the 15 included studies, only 4 studies reported on adverse events. Two studies reported minor adverse events such as stiffness and tiredness[42, 46]. In the 2013 study, Licciardone et al.[50] reported that 6% of patients had adverse events, but none of the serious events appeared to be related to the treatment intervention, and there were no significant differences between the treatment groups in the frequency of adverse events or serious adverse events. In a personal communication, the authors of another study[48] reported that no adverse events occurred.
Discussion
To our knowledge, the current review is the first systematic review with meta-analyses examining the effect of osteopathic management for acute and chronic nonspecific LBP based only on studies that used an authentic osteopathic approach. This approach required clinical judgment to individualise the treatment to each patient, rather than applying a single technique or predetermined set of techniques. Because our review had no language or publication restrictions, it is likely the most comprehensive review to date. When included studies were grouped and analysed using meta-analyses, a significant effect for OMT was found for LBP (acute and chronic), chronic LBP, LBP in pregnant women, and LBP in postpartum women. The significant effects were also found to be clinically relevant according to the criteria recommended by the Cochrane Collaboration[38].
The risk of bias in the studies was generally low, with all but 3 of the 15 included studies found to have low risk. None of the studies had a high risk of bias in the randomisation and allocation procedure, but every study had problems with the 3 blinding criteria in the risk of bias assessment. For studies of manual therapy, blinding will usually be an issue because patients tend to be aware of the manual treatment and practitioners cannot be easily blinded from the treatment intervention they deliver. When using methodology assessment tools such as the Risk of Bias instrument, the difficulty of blinding creates a disadvantage for manual therapy studies compared to studies using other interventions like pharmaceuticals which can easily be blinded.
The 2013 study by Licciardone et al.[50] was the largest RCT included in the current review, assessing 455 patients with chronic LBP. The data in the study was not normally distributed and the authors reported medians and interquartile ranges, which were not easily used for meta-analyses. We contacted the authors of this study[50] several times for additional data that could be used in the current analysis, but unfortunately this data was not made available. Subsequently, we needed to transform these data to determine means and standard deviations. We used simulation calculations recommended by Hozo et al.[37], where the median was the best estimator for the mean for sample sizes greater than 60. For the estimation of standard deviations, we calculated average standard deviations based on 3 studies[46, 51, 52], which were similar in outcome, comparison and duration of pain. For the estimation of standard deviations for functional status, we based calculations on two studies[46, 51]. For the margin of error for every estimation, it was possible that a greater difference between our estimation and the real data (i.e., the data was more in favour of the control group) could change our results regarding functional status in chronic and acute and chronic back pain. However, our results for the comparisons were almost identical regardless of whether the transformed data from Licciardone et al.[50] were included or not.
Two previous systematic reviews examined the effect of OMT on LBP. In a 2005 review by Licciardone et al.[28], studies were included if they were performed by an osteopath or osteopathic physician, but the authors also included interventions based on single manual techniques. In the current review, we wanted to examine the effect of studies that used an authentic osteopathic intervention where the clinician was free to use clinical judgment for each patient, as occurs in clinical practice. Consequently, we excluded 2 studies[58, 59] that were included in the 2005 Liccardone et al. review[28] because they involved single techniques. Further, we did not include studies with specific causes of LBP[68]. Although our review did include studies of LBP associated with pregnant and postpartum women, these studies were pooled and analysed separately. Despite these differences, the results and conclusions of our study and of the Licciardone et al.[28] study are similar: both suggested that OMT may be an effective treatment for LBP.
The findings of the current review differ from the results of a recent review by Orrock and Myers[30], largely due to different inclusion criteria. The Orrock and Myers review[30] was restricted to chronic nonspecific LBP and consequently fewer studies met their inclusion criteria. The current review was not restricted to the English language or the published literature, and we located 6 unpublished studies in German[42, 46, 48, 53–55] and 1 study in Italian[52]. Searching the unpublished grey literature for relevant studies is recommended by the Cochrane Collaboration for a more comprehensive search and to avoid publication bias[31]. In addition, the limited number of studies retrieved by Orrock and Myers prevented statistical analysis, whereas we were able to conduct meta-analyses to determine the effect of OMT interventions on LBP. In another systematic review, Posadzki and Ernst[69] examined the effect of osteopathy for musculoskeletal pain. However, Posadzki and Ernst[69] did not specifically address LBP, had only 5 studies that focused on LBP, and had no quantitative analysis, so this study is not comparable to the current review.
OMT appeared to have a larger effect on pain than functional status. Given that our analyses used results from the included studies recorded 3 months after the initial intervention, the subjective experience of pain may be quicker to respond to treatment than function.
It is difficult to assess the relative effectiveness of OMT compared to other specific interventions commonly offered to people with LBP using the available studies. The comparison interventions of the studies included in this review were varied, including sham treatment, usual medical care, physiotherapy, and no treatment; and it was not possible to group and analyse these studies according to the comparison intervention. Rubinstein et al.[32] found that there was high-quality evidence that spinal manipulation, a technique used by osteopaths and other manual therapists, had a small short-term effect on pain, but the effect was not clinically significant. The current review suggested that the effect of OMT was clinically relevant, and it may be that an individualised approach with different techniques contributed to greater effectiveness. However, Rubinstein et al.[32] had access to a greater number of studies with a total of 6070 participants, and the authors were able to examine different time periods for longevity of effectiveness. Walker et al.[70] reviewed studies of chiropractic management of LBP when combined with other interventions, as represents typical practice for many chiropractors, rather than spinal manipulation alone. Chiropractic interventions were found to improve pain in the short and medium term, but not in the long term, compared to other interventions. For functional status, there were short-term improvements, but not in the medium and long term. This review included 12 studies involving 2887 participants, substantially more than the current review on OMT, but only 3 studies had low risk of bias. Given the differing comparison groups in the studies of both reviews, it is not possible to directly compare the effects of OMT and chiropractic management.
Two important limitations of the current review were the sample sizes and comparison groups of the included studies. When studies include few participants and have wide confidence intervals in the analysis, or have small confidence intervals with effects in different directions, heterogeneity is evident and the rating of the quality of evidence should be downgraded according to the GRADE approach recommended by the Cochrane Handbook[31]. Although the majority of the included studies had relatively small sample sizes[39, 42, 46, 48, 51–56], each comparison for chronic and acute pain and for chronic pain contained over 400 participants. However, the comparisons for the conditions of LBP in pregnant and postpartum women contained fewer than 400 participants, which indicated likely imprecision of results and a resultant downgrading of the level of evidence[31]. Future studies with larger samples sizes may change our estimates of effect size for all these comparisons, particularly for LBP in pregnant and postpartum women. There were also a number of different comparison groups in the included studies, including placebo control, usual medical care, and untreated patients.
Considerable heterogeneity was evident in many of the forest plots, which indicated variability and poor overlap in the confidence intervals of the studies. This heterogeneity may be related to the small sample sizes of the studies, as well as the different comparison interventions, which may have had differing effects on pain and functional status. The small sample sizes of many of the studies, the different comparison interventions, and the heterogeneity are limitations of the current review and cause for caution concerning the conclusions. Although we performed meta-analyses on patient groups with different chronicity of symptoms, this did not appear to be a major source of heterogeneity. All patient groups together had a substantial heterogeneity of I2 = 85%, but the heterogeneity of only the mixed acute and chronic groups (I2 = 81%) and only the chronic groups (I2 = 89%) were similar.
It should be noted that the broad widths of the 95% CIs in the forest plots indicate imprecision of the results. This is often the case with systematic reviews of RCTs with small sample sizes. We have interpreted clinical relevance based on the scores of the MD and SMD, but it is necessary to consider lower and higher bounds of the CI and that the true value may lie in this range. The true value could be higher or lower than our point estimator from which we have calculated the clinical relevance, and future studies, using larger samples and robust methodology, may clarify the true point estimate and the clinical effectiveness of OMT for LBP.
The delivery of OMT, which can include a range of manual techniques, is not standardized between practitioners and requires individual clinical judgment for each patient. Most of the included studies provided an indication of the range of manual techniques used for OMT, but the exact interventions performed for each patient were generally unknown. For instance, OMT interventions in the included studies may emphasize different manual treatment approaches. Unfortunately, this lack of specific information from the included studies does not enable us to identify whether responder and non-responder patient groups received different treatments or to understand what the most effective components of OMT interventions are for LBP.
The pain and functional status outcomes analysed in the current review were measured in each study close to 3 months after the initial treatment. Therefore, the longevity of the effect of OMT for LBP cannot be determined, and most of the included studies did not have a longer follow-up period for assessment of pain and functional status. Details about the treatment approach used and clearly reported adverse events should also be included in studies. Future studies should examine the long-term effects of OMT, clearly describe the treatment approach, and report adverse events. Because of the small sample sizes in the majority of the included studies and the heterogeneity in our analyses, these future studies should also have larger sample sizes. Larger RCT studies are expensive to conduct and most of the reviewed studies were unfunded. In order to produce large RCTs examining the effect of OMT on LBP, there must be willingness from osteopathic professional organizations and national funding bodies to support such research.
Conclusion
To our knowledge, the current systematic review used the most comprehensive search for studies of OMT for nonspecific LBP. The studies we reviewed generally had a low risk of bias, but most had relatively small sample sizes of patients. Our results suggest that OMT improves pain and functional status in acute and chronic nonspecific LBP, in chronic nonspecific LBP, and in pregnant and postpartum women with LBP. Given the small sample sizes, different comparison groups in different studies, heterogeneity, and lack of long-term measurement, larger, high-quality RCTs with robust comparison groups are needed to provide firm conclusions regarding the effectiveness of OMT for LBP.
References
van Tulder M, Becker A, Bekkering T, Breen A, del Real MT, Hutchinson A, Koes B, Laerum E, Malmivaara A, Care CBWGoGftMoALBPiP: Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J. 2006, 15 (Suppl 2): S169-S191.
Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, Mannion AF, Reis S, Staal JB, Ursin H, Zanoli G: Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006, 15 (Suppl 2): S192-S300.
Deyo RA, Weinstein JN: Low back pain. N Engl J Med. 2001, 344: 363-370. 10.1056/NEJM200102013440508.
National Collaborating Centre for Primary Care: Low Back Pain: Early Management of Persistent Non-specific Low Back Pain. NICE Clinical Guideline 88. 2009, London: National Institute for Health and Clinical Excellence,http://www.nice.org.uk/nicemedia/pdf/CG88NICEGuideline.pdf,
Burton AK, Balague F, Cardon G, Eriksen HR, Henrotin Y, Lahad A, Leclerc A, Muller G, van der Beek AJ: Chapter 2. European guidelines for prevention in low back pain. Eur Spine J. 2006, 15 (Suppl 2): S136-S168.
Dagenais S, Caro J, Haldeman S: A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008, 8: 8-20. 10.1016/j.spinee.2007.10.005.
Croft P, Papageorgiou A: Low back pain in the community and in hospitals. A report to the Clinical Standards Advisory Group of the Department of Health, Arthritis and Rheumatism Council. 1994, Manchester: Epidemiology Research Unit University of Manchester
Vermani E, Mittal R, Weeks A: Pelvic girdle pain and low back pain in pregnancy: a review. Pain Pract. 2010, 10: 60-71. 10.1111/j.1533-2500.2009.00327.x.
Vleeming A, Albert HB, Ostgaard HC, Sturesson B, Stuge B: European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J. 2008, 17: 794-819. 10.1007/s00586-008-0602-4.
Gutke A, Ostgaard HC, Oberg B: Predicting persistent pregnancy-related low back pain. Spine. 2008, 33: E386-E393. 10.1097/BRS.0b013e31817331a4.
Ostgaard HC, Zetherstrom G, Roos-Hansson E, Svanberg B: Reduction of back and posterior pelvic pain in pregnancy. Spine. 1994, 19: 894-900. 10.1097/00007632-199404150-00005.
Sabino J, Grauer JN: Pregnancy and low back pain. Curr Rev Musculoskelet Med. 2008, 1: 137-141. 10.1007/s12178-008-9021-8.
Majchrzycki M, Mrozikiewicz PM, Kocur P, Bartkowiak-Wieczorek J, Hoffmann M, Stryla W, Seremak-Mrozikiewicz A, Grzeskowiak E: Low back pain in pregnant women. Ginekol Pol. 2010, 81: 851-855.
Gutke A, Ostgaard HC, Oberg B: Association between muscle function and low back pain in relation to pregnancy. J Rehabil Med. 2008, 40: 304-311. 10.2340/16501977-0170.
Brown S, Lumley J: Maternal health after childbirth: results of an Australian population based survey. Br J Obstet Gynaecol. 1998, 105: 156-161. 10.1111/j.1471-0528.1998.tb10045.x.
MacArthur C, Lewis M, Knox EG: Health after childbirth. Br J Obstet Gynaecol. 1991, 98: 1193-1195. 10.1111/j.1471-0528.1991.tb15386.x.
Patel RR, Peters TJ, Murphy DJ: Is operative delivery associated with postnatal back pain at eight weeks and eight months? a cohort study. Acta Obstet Gynecol Scand. 2007, 86: 1322-1327. 10.1080/00016340701619530.
Saurel-Cubizolles MJ, Romito P, Lelong N, Ancel PY: Women's health after childbirth: a longitudinal study in France and Italy. BJOG. 2000, 107: 1202-1209. 10.1111/j.1471-0528.2000.tb11608.x.
DiGiovanna EL, Schiowitz S, Dowling DJ: An Osteopathic Approach to Diagnosis & Treatment. 2005, Philadelphia: Lippincott William & Wilkins, 3
Vaughan B, Morrison T, Buttigieg D, Macfarlane C, Fryer G: Approach to low back pain - osteopathy. Aust Fam Physician. 2014, 43: 197-198.
Greenman PE: Principles of Manual Medicine. 2003, Philadelphia: Lippincott William & Wilkins, 3
Maniadakis N, Gray A: The economic burden of back pain in the UK. Pain. 2000, 84: 95-103. 10.1016/S0304-3959(99)00187-6.
Fawkes CA, Leach CM, Mathias S, Moore AP: A profile of osteopathic care in private practices in the United Kingdom: a national pilot using standardised data collection. Man Ther. in press
General Osteopathic Council: Snapshot Survey. 2001, London, UK: General Osteopathic Council,http://www.osteopathy.org.uk/uploads/survey2snapshot_survery_results_2001.pdf,
Walker BF, Muller R, Grant WD: Low back pain in Australian Adults. health provider utilization and care seeking. J Manipulative Physiol Ther. 2004, 27: 327-335. 10.1016/j.jmpt.2004.04.006.
Orrock P: Profile of members of the Australian Osteopathic Association: part 2 - the patients. Int J Osteopath Med. 2009, 12: 128-139. 10.1016/j.ijosm.2009.06.001.
Licciardone JC: The epidemiology and medical management of low back pain during ambulatory medical care visits in the United States. Osteopath Med Prim Care. 2008, 2: 11-10.1186/1750-4732-2-11.
Licciardone JC, Brimhall AK, King LN: Osteopathic manipulative treatment for low back pain: a systematic review and meta-analysis of randomized controlled trials. BMC Musculoskelet Disord. 2005, 6: 43-10.1186/1471-2474-6-43.
Franke H: Why reservations remain: a critical reflection about the systematic review and meta-analysis "Osteopathic manipulative treatment for low back pain" by Licciardone et al. J Bodyw Mov Ther. 2012, 16: 411-415. 10.1016/j.jbmt.2012.05.002.
Orrock PJ, Myers SP: Osteopathic intervention in chronic non-specific low back pain: a systematic review. BMC Musculoskelet Disord. 2013, 14: 129-10.1186/1471-2474-14-129.
Higgins JPT, Green S: Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. 2011, Cochrane Collaboration,http://www.cochrane-handbook.org,
Rubinstein SM, Terwee CB, Assendelft WJ, de Boer MR, van Tulder MW: Spinal manipulative therapy for acute low back pain: an update of the cochrane review. Spine. 2013, 38: E158-E177. 10.1097/BRS.0b013e31827dd89d.
Rubinstein SM, van Middelkoop M, Assendelft WJ, de Boer MR, van Tulder MW: Spinal manipulative therapy for chronic low-back pain: an update of a Cochrane review. Spine. 2011, 36: E825-E846. 10.1097/BRS.0b013e3182197fe1.
Johnson SM, Kurtz ME: Osteopathic manipulative treatment techniques preferred by contemporary osteopathic physicians. J Am Osteopath Assoc. 2003, 103: 219-224.
Orrock P: Profile of members of the Australian Osteopathic Association: part 1 - the practitioners. Int J Osteopath Med. 2009, 12: 14-24. 10.1016/j.ijosm.2008.04.002.
Fryer G, Johnson JC, Fossum C: The use of spinal and sacroiliac joint procedures within the British osteopathic profession. part 2: treatment. Int J Osteopath Med. 2010, 13: 152-159. 10.1016/j.ijosm.2010.10.001.
Hozo SP, Djulbegovic B, Hozo I: Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005, 5: 13-10.1186/1471-2288-5-13.
Furlan AD, Pennick V, Bombardier C, van Tulder M: 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976). 2009, 34: 1929-1941. 10.1097/BRS.0b013e3181b1c99f.
Cruser dA, Maurer D, Hensel K, Brown S, White K, Stoll S: A randomized, controlled trial of osteopathic manipulative treatment for acute low back pain in active duty military personnel. J Man Manip Ther. 2012, 20: 5-15. 10.1179/2042618611Y.0000000016.
Andersson GB, Lucente T, Davis AM, Kappler RE, Lipton JA, Leurgans S: A comparison of osteopathic spinal manipulation with standard care for patients with low back pain. N Engl J Med. 1999, 341: 1426-1431. 10.1056/NEJM199911043411903.
Gibson T, Grahame R, Harkness J, Woo P, Blagrave P, Hills R: Controlled comparison of short-wave diathermy treatment with osteopathic treatment in non-specific low back pain. Lancet. 1985, 1: 1258-1261.
Heinze G: Unpublished D.O. Thesis. The Effectiveness of a Holistic Osteopathic Treatment in Subacute Low Back Pain. A Randomized Controlled Trial. 2006, Akademie für Osteopathie,http://www.osteopathic-research.com/index.php?option=com_jresearch&view=publication&task=show&id=13797&lang=en,
Kunz R, Djulbegovic B, Schunemann HJ, Stanulla M, Muti P, Guyatt G: Misconceptions, challenges, uncertainty, and progress in guideline recommendations. Semin Hematol. 2008, 45: 167-175. 10.1053/j.seminhematol.2008.04.005.
Guyatt GH, Oxman AD, Schunemann HJ, Tugwell P, Knottnerus A: GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011, 64: 380-382. 10.1016/j.jclinepi.2010.09.011.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D: The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009, 339: b2700-10.1136/bmj.b2700.
Adorjàn-Schaumann K, Höhrhan G, Wille H, Wolff A: Unpublished D.O. Thesis. Osteopathic Treatment of Chronic Low Back Pain. A Randomized Controlled Trial. 1999, Akademie für Osteopathie,http://www.osteopathic-research.com/index.php?option=com_jresearch&view=publication&task=show&id=13311&lang=en,
Chown M, Whittamore L, Rush M, Allan S, Scott D, Archer M: A prospective study of patients with chronic back pain randomised to group exercise, physiotherapy or osteopathy. Physiother. 2008, 94: 21-28. 10.1016/j.physio.2007.04.014.
Gundermann S: Unpublished D.O. Thesis. Effectiveness of Osteopathic Treatment in Pregnant Women Suffering From Low Back Pain. A Randomized Controlled Trial. 2013, Akademie für Osteopathie,http://www.osteopathic-research.com/index.php?option=com_jresearch&view=publication&task=show&id=15363&lang=en,
Licciardone JC, Buchanan S, Hensel KL, King HH, Fulda KG, Stoll ST: Osteopathic manipulative treatment of back pain and related symptoms during pregnancy: a randomized controlled trial. Am J Obstet Gynecol. 2009, 202: 43-48.
Licciardone JC, Minotti DE, Gatchel RJ, Kearns CM, Singh KP: Osteopathic manual treatment and ultrasound therapy for chronic low back pain: a randomized controlled trial. Ann Fam Med. 2013, 11: 122-129. 10.1370/afm.1468.
Licciardone JC, Stoll ST, Fulda KG, Russo DP, Siu J, Winn W, Swift J: Osteopathic manipulative treatment for chronic low back pain: a randomized controlled trial. Spine (Phila Pa 1976). 2003, 28: 1355-1362.
Mandara A, Fusaro A, Musicco M, Bado F: A randomised controlled trial on the effectiveness of osteopathic manipulative treatment of chronic low back pain (abstract). Int J Osteopath Med. 2008, 11: 156-
Peters R, Van Der Linde M: Unpublished D.O. Thesis. Osteopathic Treatment of Women with Low Back Pain during Pregnancy. A Randomized Controlled Trial. 2006, Akademie für Osteopathie,http://www.osteopathic-research.com/index.php?option=com_jresearch&view=publication&task=show&id=13801&lang=en,
Recknagel C, Roá J: Unpublished D.O. Thesis. Study on the Effectiveness of Osteopathic Treatment for Women with Persistent Post Partum Back Pain. A Randomized Controlled Trial. 2007, Akademie für Osteopathie,http://www.osteopathic-research.com/index.php?option=com_jresearch&view=publication&task=show&id=13395&lang=en,
Schwerla F, Rother K, Rother D, Ruetz M: Osteopathic treatment of women with persistent low back/pelvic girdle pain postpartum. Vol Proceedings of the 9th International Symposium of Osteopathy 2012. 2012, Nantes, France: Akademie für Osteopathie,http://www.osteopathic-research.com/index.php?option=com_jresearch&view=publication&task=show&id=15181&lang=en,
Vismara L, Cimolin V, Menegoni F, Zaina F, Galli M, Negrini S, Villa V, Capodaglio P: Osteopathic manipulative treatment in obese patients with chronic low back pain: a pilot study. Man Ther. 2012, 17: 451-455. 10.1016/j.math.2012.05.002.
Boesler D, Warner M, Alpers A, Finnerty EP, Kilmore MA: Efficacy of high-velocity low-amplitude manipulative technique in subjects with low-back pain during menstrual cramping. J Am Osteopath Assoc. 1993, 93: 203-204.
Cleary C, Fox JP: Menopausal symptoms: an osteopathic investigation. Complement Ther Med. 1994, 2: 181-186. 10.1016/0965-2299(94)90017-5.
Hoehler FK, Tobis JS, Buerger AA: Spinal manipulation for low back pain. JAMA. 1981, 245: 1835-1838. 10.1001/jama.1981.03310430027015.
Tozzi P, Bongiorno D, Vitturini C: Low back pain and kidney mobility: local osteopathic fascial manipulation decreases pain perception and improves renal mobility. J Bodyw Mov Ther. 2012, 16: 381-391. 10.1016/j.jbmt.2012.02.001.
Caragan C, Tang PY, Slack M, Leiber JD, Koskinen J, Zust D, Cragun T: Pilot clinical study of osteopathic manipulative treatment in pregnant patients with acute low back pain. Int J Osteopath Med. 2008, 11: 155-10.1016/j.ijosm.2008.08.010.
Hoffman KS, Hoffman LL: Effects of adding sacral base leveling to osteopathic manipulative treatment of back pain: a pilot study. J Am Osteopath Assoc. 1994, 94: 216-217.
Parker J, Heinking KP, Kappler RE: Efficacy of osteopathic manipulative treatment for low back pain in euhydrated and hypohydrated conditions: a randomized crossover trial. J Am Osteopath Assoc. 2012, 112: 276-284.
Williams NH, Wilkinson C, Russell I, Edwards RT, Hibbs R, Linck P, Muntz R: Randomized osteopathic manipulation study (ROMANS): pragmatic trial for spinal pain in primary care. Fam Pract. 2003, 20: 662-669. 10.1093/fampra/cmg607.
MacDonald RS, Bell CM: An open controlled assessment of osteopathic manipulation in nonspecific low-back pain. Spine (Phila Pa 1976). 1990, 15: 364-370. 10.1097/00007632-199005000-00005.
Williams NH, Edwards RT, Linck P, Muntz R, Hibbs R, Wilkinson C, Russell I, Russell D, Hounsome B: Cost-utility analysis of osteopathy in primary care: results from a pragmatic randomized controlled trial. Fam Pract. 2004, 21: 643-650. 10.1093/fampra/cmh612.
Kirk L, Underwood M, Chappell L, Martins-Mendez M, Thomas P: The effect of osteopathy in the treatment of chronic low back pain. a feasibility study. Int J Osteopath Med. 2005, 8: 5-11. 10.1016/j.ijosm.2004.08.001.
Burton AK, Tillotson KM, Cleary J: Single-blind randomised controlled trial of chemonucleolysis and manipulation in the treatment of symptomatic lumbar disc herniation. Eur Spine J. 2000, 9: 202-207. 10.1007/s005869900113.
Posadzki P, Ernst E: Osteopathy for musculoskeletal pain patients: a systematic review of randomized controlled trials. Clin Rheumatol. 2011, 30: 285-291. 10.1007/s10067-010-1600-6.
Walker BF, French SD, Grant W, Green S: A Cochrane review of combined chiropractic interventions for low-back pain. Spine. 2011, 36: 230-242. 10.1097/BRS.0b013e318202ac73.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2474/15/286/prepub
Acknowledgments
The authors wish to acknowledge the assistance of Deborah Goggin, MA, Scientific Writer, A.T. Still Research Institute, A.T. Still University, in the preparation of this manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests. This research received no grant from any funding agency in the public, commercial, or not-for-profit sectors. Both HF and GF are osteopaths.
Authors’ contributions
HF and GF wrote background, results, discussion, conclusion and abstract. HF, JDF and GF performed the search, study selection, data extraction and data analyses and wrote the method part. All authors read and approved the final version.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Franke, H., Franke, JD. & Fryer, G. Osteopathic manipulative treatment for nonspecific low back pain: a systematic review and meta-analysis. BMC Musculoskelet Disord 15, 286 (2014). https://doi.org/10.1186/1471-2474-15-286
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2474-15-286