Abstract
Background
Scleral buckling surgery and pars plana vitrectomy are competing methods in the treatment of retinal detachment. The recent development of spectral-domain optical coherence tomography (SD-OCT) has dramatically improved the visualization of the photoreceptor layer relative to conventional OCT, and offers new opportunities to investigate the discordances between anatomic and functional outcomes after retinal detachment surgery. Hence, the study aim was to use SD-OCT to compare the postoperative macular recovery between scleral buckling and vitrectomy for macular-off rhegmatogenous retinal detachment.
Methods
In this retrospective observational case series, we observed 32 patients who underwent scleral buckling surgery (group 1) and 26 patients who underwent pars plana vitrectomy (group 2) as the primary surgery for macula-off rhegmatogenous retinal detachment. OCT was used to examine microstructural changes in the macular area.
Results
The mean visual acuity improvement was 0.4 ± 0.8 logMAR in group 1 and 0.7 ± 0.9 logMAR in group 2. As detected by SD-OCT, subretinal fluid was present in 26 of the group 1 eyes (81.3%) and 5 of the group 2 eyes (19.2%) at 8 weeks postoperatively.
This difference was statistically significant (Fisher’s exact test, P < 0.05). Moreover, detection by SD-OCT revealed epiretinal membranes in 5 of the group 1 eyes (15.6%) and 11 of the group 2 eyes (42.3%), a difference that was statistically significant (Fisher’s exact test, P < 0.05).
Conclusions
Macular recovery and the mean visual acuity differed between the 2 groups of patients. With the help of SD-OCT, we observed that subretinal fluids could persist for a relatively longer period after scleral buckling. Based on our results, we conclude that primary vitrectomy surgery is a better choice for macular recovery of the macula-off rhegmatogenous retinal detachment.
Similar content being viewed by others
Background
The treatment of patients with primary rhegmatogenous retinal detachment (RRD) has undergone considerable changes in recent decades. Since pars plana vitrectomy (PPV) was established in 1971 by Machemer et al. [1], scleral buckling and PPV have competed as methods in the treatment of retinal detachment. Numerous studies have been published recommending one of the two methods [2–12]. Scleral buckling remains the method of choice in uncomplicated retinal situations, i.e., single breaks and/or a limited retinal detachment. In contrast, PPV is indicated in complicated situations, i.e., vitreous hemorrhage/opacity, proliferative vitreoretinopathy (PV), or breaks at the posterior pole [13–22].
Poor visual acuity (VA) or metamorphopsia may persist over time after a successful operation for macula-off retinal detachment. Both preoperative and postoperative factors are generally considered to contribute to the recovery of VA after surgery for this type of retinal detachment. The pre-operative factors include VA, height and duration of the macular detachment, and vitreomacular traction, while post-operative factors include cystoid macular edema [23, 24], epiretinal membranes, retinal folds, persistent subretinal fluid, retinal folds [25], and persistent foveal detachment [26, 27].
Optical coherence tomography (OCT) is a noninvasive real-time system that can be used to investigate retinal structures [28, 29]. The more recent development of spectral-domain OCT (SD-OCT) has led to a 50-fold higher data acquisition speed, which has reduced the occurrence of motion artifacts, and has dramatically improved the visualization of the photoreceptor layer by using an axial resolution of 4 to 6 μm [30]. Therefore, SD-OCT imaging offers new and interesting opportunities to better understand the discordances between anatomic and functional outcomes after retinal detachment surgery. In this study, we used SD-OCT to compare macular recovery between PPV and scleral buckling in the treatment of macula –off RRD.
Methods
This study was a retrospective observational case series. The preoperative data included age, sex, VA [converted to the logarithm of the minimal angle of resolution (logMAR)], the duration of detachment and the height of the macular detachment, lens status, and the PV grade. The height of the macular detachment was measured using the retinal thickness mode in the SD-OCT software and was defined as the distance between the inner surface of the retinal pigment epithelium and the outer surface of the neurosensory retina at the fovea.
Fifty-eight consecutive patients (58 eyes) with macula-off RRD underwent surgical repair at department of Retina and Vitreous, the Second People's Hospital of Jinan, Shandong province, China, between February 2011 and February 2012 were reviewed. All the patients met the inclusion/exclusion criteria. All eyes had primary retinal detachment without age-related macular degeneration, cataract, vitreous hemorrhage, macular hole, trauma, macular edema, intraocular inflammation, glaucoma, or retinal vascular occlusive diseases. Patients with systemic diseases, such as diabetes or hypertension, were excluded. We divided the patients based on retinal tears. If the tears were more than 2 disk diameter, the retinal detachment range was big (more than half of the retina) and obvious traction existed, we choose PPV; If retinal tears were small and gathered, the retinal detachment range was small and no obvious traction existed, we choose SB. PV grade showed no significant difference in the two groups, being less than grade B in all the patients. In our study, 32 eyes (group 1) and 26 eyes (group 2) successfully underwent scleral buckling and PPV respectively. Informed consent was obtained from all patients included in the study and the study was approved by the ethical committee of the Second People's Hospital of Jinan, Shandong province, China.
In ppv group, perfluoropropane (C3F8) tamponade was used in the patients who had tears located in the upper retina. Four patients (4 eyes) underwent phacoemulsification to deal with peripheral retinal holes and retina degeneration or dry hole areas. These four eyes underwent oil implantation 3 months later. Both silicone oil and perfluoropropane (C3F8) filled eyes did not develop cataract at final follow-up. Meanwhile, no gas remained in the vitreous cavity 2 months after the operation for group 2 eyes in which gas tamponade was used.
All patients underwent pre- and postoperative best-corrected logMAR VA testing, slit-lamp biomicroscopy, and dilated fundus examination. High-resolution, three-dimensional SD-OCT (Cirrus HD-OCT 4000 Zeiss, Germany) examinations were performed for each eye. The SD-OCT measurements were made after pupil dilation (0.5% tropicamide), with the patient in the sitting position and the head placed on a chin rest. SD-OCT measurements were also obtained 2 weeks, 1 month, and 2 months after the operation.
Values are given as the frequency and percentage for qualitative parameters, while the mean and standard deviation are provided for quantitative parameters. The best-corrected VA (BCVA) was evaluated before the operation and at the final follow-up using a paired t-test. The incidence of epiretinal membranes, subretinal fluid, discontinued external limiting membrane (ELM), and disruptions of the inner segment/outer segment junction and ELM were evaluated with Fisher’s exact test. The results were considered statistically significant at P < 0.05. Statistical analyses were performed using SPSS 11.0 software (SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics are shown in Table 1. The mean age of groups 1 (scleral buckling) and 2 (vitrectomy) were 36.38 ± 13.32 years (range, 17–59 years) and 44.69 ± 14.37 years (range, 19–67 years), respectively. The age, sex, duration of macular detachment (group 1: 12 ± 4.5 days; group 2: 15 ± 6.5 days), and the height of the macular detachment (group 1: 375 ± 107 μm; group 2: 470 ± 125 μm) showed no significant differences between the 2 groups.
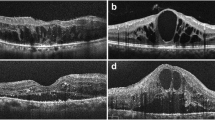
The improvement in the mean VA was significantly greater in PPV group compared to that in SB group (0.7 ± 0.9 logMAR vs. 0.4 ± 0.8 logMAR, P < 0.05). Meanwhile, as detected by SD-OCT, subretinal fluid was present in 26 of the group 1 eyes (81.3%) and 5 of the group 2 eyes (19.2%) at the final follow-up (2 months postoperation), a difference that was statistically significant (P < 0.05) (Figure 1). Further, epiretinal membranes were observed in 5 of the group 1 eyes (15.6%) and 5 of the group 2 eyes (42.3%). This difference was not statistically significant (P = 1.0). No significant differences were observed between groups in terms of the frequency of discontinued ELM and disruptions of ELM or the inner segment/outer segment (IS/OS) junction (Table 2).
Optical coherence tomographic images of preoperative and postoperative retinas. A-C: Shows a patient from the SB group. The patient was a 34 year old female, with Poor visual acuity (VA) and metamorphopsia for 15 days before operation. A. The best-corrected visual acuity (BCVA) among the preoperative retinas was 2.0. B. Typical residual retinal detachment can be seen 1 week after sclera bucking; the BCVA was 1.3. C, Typical residual retinal detachment can be seen 2 months after sclera bucking; the BCVA was 1.0. D-E: Shows a patient from the PPV group. The patient was a 42 years old female, with Poor visual acuity (VA) and metamorphopsia for 21 days before operation. D. Optical coherence tomographic images of a preoperative retina; the BCVA was 1.3. E. One month after primary vitrectomy operation, macular reattachment was successful in this patient, and no subretinal fluid was present; the BCVA was 0.3.
Discussion
Vitrectomy has a short operation time, is a standard procedure, and its success rate is approximately the same as scleral buckling for deep retinal tears and multiple retinal tears at different depths [31]. Furthermore, a better success rate for macular reattachment and earlier recovery of VA has been reported for vitrectomy relative to scleral buckling [32–36]. Based on our preliminary results, the mean VA improvement was greater in PPV group compared to that in SB group. The postoperative visual outcome of macular-off RRD was significantly associated with the integrity of the ELM and the IS/OS junction. In addition, the persistent subretinal fluid (SRF) was directly related to metamorphopsia and poor VA. SD-OCT was introduced for advanced imaging, thus reducing acquisition time and allowing high resolution imaging of macular microstructures [28–30]. SD-OCT allows improved visualization of retinal structures, especially photoreceptor cell layers. With the advent of SD-OCT, the subtle changes of the macula including the integrity of the ELM, the IS/OS junction, the SRF could be well defined. In our present study, both of the two groups showed discontinued ELM, disruptions of IS/OS junction and the existence of the SRF. These findings helped us compare the changes in the macula between the SB group and PPV group. The SD-OCT findings showed the SRF was statistically different in the group 1(81.3%) and group 2 (19.2%).
Persistent SRF could be viewed in the patients who had undergone SB surgery. Several reasons result in the persistent SRF in SB surgery. The mean macular microcirculation blood flows were lower in SB surgery than in PPV surgery. Also, choroidal blood flow has been reported to be less reduced in vitrectomy relative to that in scleral buckling [37]. Further, during PPV surgery, the SRF was exchanged by gas as possible. However, in the SB surgery, the SRF was limited drained out. The silicone oil or perfluoropropane (C3F8) can help the retina reattachment. The hemodynamic change may affect the polarity of the RPE, leading to fluid leakage. Furthermore, inflammation induced by condensation of the scleral buckling may accelerate subretinal fluid accumulation [31]. As such, the presence of persistent subretinal fluid after successful scleral buckling surgery for macular-off RRD may influence the final BCVA or anatomic attachment.
The present study focusses on the macular reattachment and the mean VA improvement of macular-off RRD undergone SB and PPV surgery. It showed that PPV group showed a better mean VA than the scleral buckling group at the final follow-up. The SD-OCT findings demonstrated that a better macular reattachment in the PPV group than the SB group for macular-off RRD.
However, other studies showed that SRF gradually disappeared in most cases within 1 year after surgery [26, 27]. The long-term follow-up is necessary in our further study.
The limitations of our study were the short follow-up time, the small sample size, and the subjective nature of the interpretations of the images. In the present study, no attempt was made to determine the long-term complications, such as cataracts and redetachment of the retina. Hence, further follow-up is needed to observe the changes of postoperative VA and SRF.
Conclusions
SD-OCT contributed to the observation of subtle changes of macula structure of macula-off RRD. SRF that persisted in the SB surgery could influence the VA. We conclude that primary vitrectomy surgery showed advantages in treating macula-off rhegmatogenous retinal detachment. For the macular-off rhegmatogenous retinal detachment patients, PPV surgery helps in the anatomic reduction of the macular and there is no obvious subretinal fluid, thus better visual ability can be achieved.
Abbreviations
- BCVA:
-
Best-corrected visual acuity
- ELM:
-
External limiting membrane
- logMAR:
-
Logarithm of the minimal angle of resolution
- OCT:
-
Optical coherence tomography
- SD-OCT:
-
Spectral-domain optical coherence tomography
- PPV:
-
Pars plana vitrectomy
- RRD:
-
Rhegmatogenous retinal detachment
- VA:
-
Visual acuity
- SRF:
-
Subretinal fluid.
References
Machemer R, Buettner H, Norton EW, Parel JM: Vitrectomy: a pars plana approach. Trans Am Acad Ophthalmol Otolaryngol. 1971, 75: 813-820.
Afrashi F, Erakgun T, Akkin C, Kaskaloglu M, Mentes J: Conventional buckling surgery or primary vitrectomy with silicone oil tamponade in rhegmatogenous retinal detachment with multiple breaks. Graefes Arch Clin Exp Ophthalmol. 2004, 242: 295-300. 10.1007/s00417-003-0842-2.
Barrie T, Kreissig I, Heimann H, Holz ER, Mieler WF: Repair of a primary rhegmatogenous retinal detachment. Br J Ophthalmol. 2003, 87: 782-784. 10.1136/bjo.87.6.782.
Holz ER, Mieler WF: View 3: The case for pneumatic retinopexy. Br J Ophthalmol. 2003, 87: 787-789. 10.1136/bjo.87.6.787.
Kreissig I: View 1: minimal segmental buckling without drainage. Br J Ophthalmol. 2003, 87: 782-784. 10.1136/bjo.87.6.782.
McLeod D: Is it time to call time on the scleral buckle?. Br J Ophthalmol. 2004, 88: 1357-1359.
Pournaras CJ, Kapetanios AD: Primary vitrectomy for pseudophakic retinal detachment: a prospective non-randomised study. Eur J Ophthalmol. 2003, 13: 298-306.
Schmidt JC, Rodrigues EB, Hoerle S, Meyer CH, Kroll P: Primary vitrectomy in complicated rhegmatogenous retinal detachment—a survey of 205 eyes. Ophthalmologica. 2003, 217: 387-392. 10.1159/000073067.
Schwartz SG, Kuhl DP, McPherson AR, Holz ER, Mieler WF: Twenty-year follow-up for scleral buckling. Arch Ophthalmol. 2002, 120: 325-329. 10.1001/archopht.120.3.325.
SPR Study group: View 2: the case for primary vitrectomy. Br J Ophthalmol. 2003, 87: 784-787.
Tewari HK, Kedar S, Kumar A, Garg SP, Verma LK: Comparison of scleral buckling with combined scleral buckling and pars plana vitrectomy in the management of rhegmatogenous retinal detachment with unseen retinal breaks. Clin Exp Ophthalmol. 2003, 31: 403-407. 10.1046/j.1442-9071.2003.00686.x.
Wickham L, Connor M, Aylward GW: Vitrectomy and gas for inferior break retinal detachments: are the results comparable to vitrectomy, gas, and scleral buckle?. Br J Ophthalmol. 2004, 88: 1376-1379. 10.1136/bjo.2004.043687.
Ambresin A, Wolfensberger TJ, Bovey EH: Management of giant retinal tears with vitrectomy, internal tamponade, and peripheral 360 degrees retinal photocoagulation. Retina. 2003, 23: 622-628. 10.1097/00006982-200310000-00003.
Bartz-Schmidt KU, Kirchhof B, Heimann K: Primary vitrectomy for pseudophakic retinal detachment. Br J Ophthalmol. 1996, 80: 346-349. 10.1136/bjo.80.4.346.
Duquesne N, Bonnet M, Adeleine P: Preoperative vitreous hemorrhage associated with rhegmatogenous retinal detachment: a risk factor for postoperative proliferative vitreoretinopathy?. Graefes Arch Clin Exp Ophthalmol. 1996, 234: 677-682. 10.1007/BF00292353.
el-Asrar AM: Primary vitrectomy for bullous rhegmatogenous retinal detachments due to complex breaks. Eur J Ophthalmol. 1997, 7: 322-326.
Ghartey KN, Tolentino FI, Freeman HM, McMeel JW, Schepens CL, Aiello LM: Closed vitreous surgery. XVII. Results and complications of pars plana vitrectomy. Arch Ophthalmol. 1980, 98: 1248-1252. 10.1001/archopht.1980.01020040100014.
Girard P, Karpouzas I: Pseudophakic retinal detachment: anatomic and visual results. Graefes Arch Clin Exp Ophthalmol. 1995, 233: 324-330. 10.1007/BF00200480.
Richardson EC, Verma S, Green WT, Woon H, Chignell AH: Primary vitrectomy for rhegmatogenous retinal detachment: an analysis of failure. Eur J Ophthalmol. 2000, 10: 160-166.
Spiegel D, Nasemann J, Nawrocki J, Gabel VP: Severe ocular trauma managed with primary pars plana vitrectomy and silicone oil. Retina. 1997, 17: 275-285. 10.1097/00006982-199707000-00001.
Wang JZ: Vitreo-retinal surgery for complicated retinal detachment. Chung Hua Yen Ko Tsa Chih. 1993, 29: 205-207.
Wong D, Billington BM, Chignell AH: Pars plana vitrectomy for retinal detachment with unseen retinal holes. Graefes Arch Clin Exp Ophthalmol. 1987, 225: 269-271. 10.1007/BF02150146.
Sabates NR, Sabates FN, Sabates R, Lee KY, Ziemianski MC: Macular changes after retinal detachment surgery. Am J Ophthalmol. 1989, 108: 22-29.
Heimann H: KB Primary vitrectomy in rhegmatogenous retinal detachment. Retina. Edited by: Ryan S, Hinton D, Schachat A. 2006, Philadelphia: Elsevier Mosby, 2085-2094. 4
Tani P, Robertson DM, Langworthy A: Prognosis for central vision and anatomic reattachment in rhegmatogenous retinal detachment with macula detached. Am J Ophthalmol. 1981, 92: 611-620.
Hagimura N, Iida T, Suto K: Persistent foveal retinal detachment after successful rhegmatogenous retinal detachment surgery. Am J Ophthalmol. 2002, 133: 516-520. 10.1016/S0002-9394(01)01427-1.
Wolfensberger TJ, Gonvers M: Optical coherence tomography in the evaluation of incomplete visual acuity recovery after macula-off retinal detachments. Graefes Arch Clin Exp Ophthalmol. 2002, 240: 85-89. 10.1007/s00417-001-0410-6.
Fercher AF, Hitzenberger CK, Drexler W, Kamp G, Sattmann H: In vivo optical coherence tomography. Am J Ophthalmol. 1993, 116: 113-114.
Swanson EA, Izatt JA, Hee MR, Huang D, Lin CP, Schuman JS, Puliafito CA, Fujimoto JG: In vivo retinal imaging by optical coherence tomography. Opt Lett. 1993, 18: 1864-1866. 10.1364/OL.18.001864.
Landa G, Rosen RB, Garcia PM, Seiple WH: Combined three-dimensional spectral OCT/SLO topography and microperimetry: steps toward achieving functional spectral OCT/SLO. Ophthalmic Res. 2010, 43: 92-98. 10.1159/000247593.
Eshita T, Shinoda K, Kimura I, Kitamura S, Ishida S, Inoue M, Mashima Y, Katsura H, Oguchi Y: Retinal blood flow in the macular area before and after scleral buckling procedures for rhegmatogenous retinal detachment without macular involvement. Jpn J Ophthalmol. 2004, 48: 358-363.
Escoffery RF, Olk RJ, Grand MG, Boniuk I: Vitrectomy without sclera buckling for primary rhegmatogenous retinal detachment. Am J Ophthalmol. 1985, 99: 275-281.
Ogino N: Transvitreous surgery for rhegmatogenous retinal detachment (in Japanese with English abstract). Nihon Ganka Kiyo (Folia Ophthalmol Jpn). 1985, 36: 2453-2460.
Ogino N: Transvitreal approach for rhegmatogenous retinal detachment (in Japanese with English abstract). Rinsho Ganka (Jpn J Clin Ophthalmol). 1987, 41: 1095-1097.
Uemura A, Nakao K: A comparison between scleral buckling procedure and vitrectomy for the management of uncomplicated retinal detachment caused by posterior retinal break (in Japanese with English abstract). Nippon Ganka Gakkai Zasshi (J Jpn Ophthalmol Soc). 1995, 99: 1170-1174.
Heimann H, Zou X, Jandeck C, Kellner U, Bechrakis NE, Kreusel KM, Helbig H, Krause L, Schüler A, Bornfeld N, Foerster MH: Primary vitrectomy for rhegmatogenous retinal detachment: an analysis of 512 cases. Graefes Arch Clin Exp Ophthalmol. 2006, 244: 69-78. 10.1007/s00417-005-0026-3.
Vetrugno M, Gigante G, Cardia L: The choroidal circulation after retinal detachment surgery. Clin Hemorheol Microcirc. 1999, 21: 349-352.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2415/13/12/prepub
Acknowledgements
The authors thank Dr. Jian Liu and Dr. Ning Wei for help in OCT examination and acquisition of data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
CH, TZ, and TF participated in the design of the study and performed the statistical analysis. CH participated in the sequence alignment and drafted the manuscript. XW and QJ conceived the study, and participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Huang, C., Fu, T., Zhang, T. et al. Scleral buckling versus vitrectomy for macula-off rhegmatogenous retinal detachment as accessed with spectral-domain optical coherence tomography: a retrospective observational case series. BMC Ophthalmol 13, 12 (2013). https://doi.org/10.1186/1471-2415-13-12
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2415-13-12