Abstract
Background
The discovery of a "serrated neoplasia pathway" has highlighted the role of hyperplastic lesions of the colon as the significant precursor of colorectal adenocarcinoma. In mice, hyperplasia of the colonic mucosa is a regular phenomenon after a challenge with colonic carcinogens indicating that mucosal hyperproliferation and thickening, even without cytological dysplasia, represents an early pre-malignant change. Cyclophilin C-associated protein (CyCAP) has been described to down-modulate endotoxin signaling in colorectal murine mucosa and is a murine orthologue of the tumor-associated antigen 90 K (TAA90K)/mac-2-binding protein.
Methods
Female Balb/c wild-type (WT) and CyCAP knock-out (KO) mice (6–8 weeks old) were administered 2 or 6 weekly subcutaneous injections of azoxymethane. The animals were evaluated post-injection at six weeks for aberrant crypt foci (ACF) study and at five months for colon tumor measurement. The thickness of the colon crypts was measured in microns and the number of colonocytes per crypt was also determined in well-oriented crypts. Morphometric analyses of the colon mucosa were also performed in untreated 6–8 weeks old KO and WT animals. Formalin-fixed/paraffin-embedded colon sections were also studied by immunohistochemistry to determine the Ki-67 proliferation fraction of the colon mucosa, β-catenin cellular localization, cyclin D1, c-myc, and lysozyme in Paneth cells.
Results
Cyclophilin C-associated protein (CyCAP)-/- mice, spontaneously developed colonic mucosal hyperplasia early in life compared to wild-type mice (WT) (p < 0.0001, T-test) and crypts of colonic mucosa of the (CyCAP)-/- mice show higher proliferation rate (p = 0.039, Mann-Whitney Test) and larger number of cyclin D1-positive cells (p < 0.0001, Mann-Whitney Test). Proliferation fraction and cyclin D1 expression showed positive linear association (p = 0.019, Linear-by-Linear Association). The hyperplasia was even more pronounced in CyCAP-/- mice than in WT after challenge with azoxymethane (p = 0.005, T-test). The length of the crypts (r = 0.723, p = 0.018, Spearman Correlation) and the number of colonocytes per crypt (r = 0.863, p = 0.001, Spearman Correlation) in non-tumorous areas were positively associated with azoxymethane-induced number of tumors. CyCAP-/- developed larger numbers of tumors than WT animals (p = 0.003, T-Test) as well as overall larger tumor mass (p = 0.016, T-Test). Membranous β-catenin was focally overexpressed in KO mice including proliferative zone of the crypts.
Conclusion
CyCAP-/- represent the first described model of spontaneous colonic mucosal hyperplasia. We conclude that CyCAP-deficient mice spontaneously and after challenge with carcinogen develop significantly more colorectal mucosal hyperplasia, an early stage in murine colonic carcinogenesis.
Similar content being viewed by others
Background
Colorectal cancer remains a significant cause of morbidity in Western countries [1]. Colorectal carcinoma evolves through multiple pathways (recently reviewed by Jass J. R.)[2]. For many years clinical practice has been focused on early detection and removal of adenomatous polyps by screening colonoscopy is an important strategy for reducing the risk of developing colon cancer [3]. Colorectal adenoma is considered to be a precursor of about 70% colorectal carcinomas, those that are characterized by chromosomal instability and are microsatellite stable. It appears that as many as 20% of colorectal carcinomas may originate by serrated neoplasia pathway [2]. It has become apparent that clinical management of lesions traditionally diagnosed as "hyperplastic polyps" and generally considered as benign lesions with no malignant potential, may need to change because of the malignant potential associated with some types of serrated polyps including so-called "traditional serrated adenoma" and "sessile serrated adenoma" [1, 4–6].
Hyperplasia of the human colon is found in several forms including focal mucosal hyperplasia in hyperplastic polyp, the thickening of the mucosa surrounding colon carcinoma or adenoma, which is termed "transitional mucosa", and regenerative hyperplasia, which may occur in a variety of inflammatory conditions. All of these lesions are considered to be benign, harmless lesions, with no proven premalignant potential [7–9]. Sessile serrated polyp is a newly described type of serrated polyp, now recognized as a main actor in a so-called "serrated pathway" of colon carcinogenesis and it shares many features with the common hyperplastic polyp [5, 10, 11]. Therefore in humans, two types of colonic serrated mucosal hyperplasia can be distinguished; non-preneoplastic and preneoplastic. Most forms of mucosal thickening of the colon are due to reactive epithelial hyperplasia and do not lead to malignancy, which is in contrast to mice in which mucosal hyperplasia develops as the first change and also in parallel with colonic epithelial tumors after the treatment with carcinogens [12].
The above observations in humans are in agreement with the notion that not all hyperplastic agents have tumor-promoting activity [13]. For instance, TGF- alpha is a potent in vivo epithelial mitogen which promotes dramatic hyperplasia in the colon, but does not lead to any alteration in colonic tissue architecture or colonic tumors [14]. TGF- alpha was also found to be absent in ACF in rats and there was reduced amounts of TGF- alpha expression in the upper part of the aberrant crypts compared with the surrounding normal crypts [15]. Although the absence of TGF-alpha was unexpected, it was in accordance with observations from recent in vitro studies which demonstrated that the presence of TGF-alpha in the top of the colonic crypt serves to inhibit growth of differentiated colonic epithelial cells [16, 17]. In humans, lower levels of TGF-alpha are present in the distal part of the colon, which is the most common site of tumor formation [18]. Additionally, non-preneoplastic secondary mucosal hyperplasia as a reaction to a colonic tumor, so-called "transitional mucosa", possibly develops due to tumoral secretion of IL-15 [19].
Despite these findings, it has been established that thickened and serrated colonic mucosa at least in the form of sessile serrated adenoma (synonymously referred to as "atypical hyperplasia"), represents a morphologic entity of the serrated neoplasia pathway [2, 20]. The discovery of different subtypes of serrated polyps enabled morphologic separation of the harmless hyperplastic lesions from those that are likely to be precancerous [4, 6]. It is possible that precancerous serrated polyps of the colon represent a human homologue of the murine pre-neoplastic hyperplasia induced by carcinogens since these represent the only form of "hyperplasia" of human colonic mucosa that has been biologically linked to colorectal carcinoma [2].
The tumor-associated antigen 90 K (TAA90K) [21, 22], also known as Mac-2-binding protein or 90 K, is a secreted 90–100 kDa glycoprotein widely expressed in human fluids [23], tumor derived cell lines including those with epithelial differentiation [24–28] and elevated in the serum of cancer patients [Iacobelli et al., 1993; Natoli et al., 1993; Iacobelli et al., 1994; Greco et al., 2004] as well as sufferers from other nonmalignant diseases such as AIDS [29, 30]. It is a member of the scavenger-receptor cysteine-rich domain superfamily implicated in development and regulation of the immune system [31]. On the other hand, its aberrant expression by epithelial neoplastic cells has also been described. Elevated expression of TAA90K has been detected in breast, gastric, lung and pancreatic cancers [32–35] and, in the cases of lung cancer and malignant mesothelioma [33, 34], protein levels correlated with metastasis and predicted survival or disease manifestation. In a recent study [36], we have also detected elevated TAA90K expression in colorectal adenocarcinoma. Although the function of aberrantly expressed TAA90K in cancer is unclear, it has been shown to mediate β1-integrin-dependent cell adhesion [37], interact with various extracellular proteins including extracellular matrix proteins and galectins [36–38], and stimulate expression of promatrilysin [39], previously implicated in colon cancer progression [40].
However, the primary and physiological role of TAA90K appears to be, according to the current knowledge, in immune regulation. This glycoprotein has been shown to be a potent immune stimulator with positive effects on the generation of cytotoxic effector cells (NK/LAK) from human peripheral blood mononuclear cells (PBMC) [41, 42]. In fact, 90 K in human milk may be protective against acute respiratory infections [43]. The protective effect seems to be related to the amount of 90 K ingested during the first few days, as milk 90 K concentrations subsequently decline rapidly in all mothers [44]. These findings suggested that 90 K initiates a defense mechanism in the infant early in life.
In recent years, cyclophilin C-associated protein (CyCAP) has been identified as the murine orthologue of TAA90K with up to 80% homology in their amino acid sequence [45, 46]. CyCAP is a widely expressed secreted glycoprotein that modulates the host response to bacterial endotoxin [47]. In response to endotoxin, CyCAP-deficient mice overproduced interleukin 12 and interferon-γ systemically and tumor necrosis factor α locally, proinflammatory molecules that also promote T helper 1 responses. Furthermore, macrophages stimulated in vitro with endotoxin in serum deficient CyCAP-null cells secreted more TNF-α, supporting the proposal that CyCAP specifically down-modulates endotoxin signaling [47].
In this report, we have examined the contribution of CyCAP to colon hyperplasia and tumorigenesis in vivo before and after injection of the colon carcinogen azoxymethane as a possible animal model suitable for elucidating the role of TAA90K in colon tumorigenesis and progression, thereby providing a level of biological understanding not readily available in clinical disease.
Methods
Animals and azoxymethane treatment
Female Balb/C mice (6–8 weeks) were obtained from the Animal Resources Center (University of Saskatchewan, Saskatoon, SK). Breeding pairs of Balb/C CyCAP knock-out mice were obtained from Dr. I. Weissman (Stanford University, San Francisco, CA) and used to set up an in-house breeding colony. Forty seven animals were tested routinely for the presence of pathogens. In particular, mice were free of Citrobacter freundii, a bacterium associated with transmissible intestinal hyperplasia [48]. All experimental procedures were carried in accordance with guidelines from the Canadian Council on Animal Care.
Forty seven female Balb/c wild-type and CyCAP knock-out mice (6–8 weeks old) were administered 6 weekly subcutaneous injections of azoxymethane (10 mg/kg) (Midwest Research Institute, MO) [49] for measurements of ACF or colon tumor incidence, respectively, using procedures described previously [50]. Six weeks (ACF measurement) or five months (colon tumor measurement) post-injection, animals were sacrificed, the intestine removed and washed in ice-cold PBS. Colons were cut longitudinally, laid flat between two pieces of 3 mm filter paper and fixed for at least two hours in formalin (10% formaldehyde in phosphate buffered saline pH 7.0). For ACF and tumor measurements, colons were stained for 5 min in a solution of 1% methylene blue in PBS and destained for 5 min in PBS. Stained colons were examined microscopically for the presence of ACF, as described by Bird et al. [51] and also for the presence of tumors. The size of tumors (length in mm × width in mm) was measured at a magnification of 40× using a gradicule (Precision Instruments, Vancouver, BC) calibrated with a slide micrometer. After the data were collected, the fixed colons of 5 untreated and 5 azoxymethane-treated wild-type and CyCAP knock-out animals were embedded in paraffin. Hematoxylin and eosin-stained five micron-thick serial sections were examined histologically.
Measurements and cell counts
All measurements and cell counts were performed on histologically non-tumorous mucosa, with no definite pathological findings. The exact absolute length of each colonic crypt was measured in μm and the exact absolute number of cells per each crypt was recorded. In addition, only areas away from the tumors and lymphoid aggregates were measured to avoid so-called traditional mucosa or reactive changes. The thickness of the crypts was measured in microns in 60 to 246 well-oriented crypts (all available well-oriented crypts were measured) using a calibrated camera (Nikon Digital Sight DS-SM, Japan) mounted on the microscope (Nikon Eclipse 80i, Japan). The presence of the full thickness of the crypt with open lumen, to avoid tangentionally-sectioned crypts, was the only positive selection criterion. The same method was used for establishing the crypt proliferation fraction as measured by the number of Ki-67+ cells divided by the total number of cells per crypt. Immunohistochemical tests for Ki-67, cyclin D1, c-myc, lysozyme, and β-catenin were done as previously described [52, 53]. In the majority of animals, a total of 60 accounted for most of the well-oriented crypts. The number of colonocytes per crypt was also determined in at least 60 well-oriented crypts per animal. B-catenin was evaluated for cellular localization and its nuclear, cytoplasmic, and membranous was recorded. The intensity of staining and its distribution was recorded in 60 well-oriented crypts using semiquantitative scale (0-negative, 1-weak membranous staining, and 2-strong membranous staining), as well as the anatomical location of the positive cells in the mucosa (crypt base, crypt body, and colonic plate).
Statistical analysis
Descriptive statistics were used to summarize data. Initial descriptive analyses were done to determine whether to use parametric t-test or non-parametric Mann-Whitney test for mean comparisons and whether to assume equal variance or unequal variance. A Student's t-test was used to examine the differences for continuous variable under assuming either equal or unequal variance. Association between variables were determined using Spearman correlation coefficient analysis. Linear regression model were also used after checking assumption of linearity, normality and constant variance of independent error. A p-value of less than 0.05 was considered statistically significant. The analysis was performed using the SPSS – 15 software.
Results
Correlation between the number of cells per crypt and the length of the crypt was significant (p < 0.0001, Spearman Correlation). The coefficient of correlation was 0.86. This result indicated that the increased length of the crypts was due to hyperplasia, rather than hypertrophy or other phenomena like edema or various artifacts.
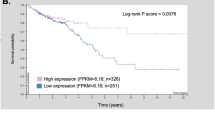
All available well-oriented crypts were evaluated for the number of cells per crypt as well as for the absolute length of the crypt. The number of observations (N) per animal varied from 60 to 246 per animal depending on the number of available well-oriented crypts. The results are summarized in Tables 1 and 2 and Figure 1, 2, 3, 4, 5, 6, and 7. The length of the crypts in CyCAP null mice and WT mice (r = 0.723, p = 0.018, Spearman Correlation) as well as the number of colonocytes per crypt (r = 0.863, p = 0.001, Spearman Correlation) in non-tumorous areas of the colon were positively associated with total number of tumors induced by azoxymethane (Figure 1 and 2). Also, the length of the crypts (r = 0.782, p = 0.008, Spearman Correlation) and the number of colonocytes per crypt (r = 0.927, p < 0.0001, Spearman Correlation) in non-tumorous areas of the colon of CyCAP null mice and WT mice correlated with the total size of the tumors. In addition, untreated 8-week old CyCAP null mice had significantly thicker mucosa and significantly larger numbers of colonocytes per crypt (hyperplasia) (p < 0.0001, T-test), as well as higher proliferation fraction as measured by Ki-67 immunohistochemical test (p = 0.032, Mann-Whitney Test) even before azoxymethane treatment was initiated (Figure 1, 2A, and 3) indicating spontaneous development of mucosal hyperplasia. The difference in diffuse mucosal thickness was even more pronounced after the treatment with carcinogen (p < 0.0001, T-test, Figure 2A, 3, 4, and 5). Similarly, the null mice had larger numbers of cells per crypt both before (p = 0.032, Linear Regression; plots not shown) and after treatment with carcinogen (p = 0.012, Linear Regression; plots not shown) compared with WT animals.
The differences in the measured crypt length were significant before and after treatment by azoxymethane. CyCAP-/- animals spontaneously developed increased crypt length and also developed much more exuberant response to azoxymethane treatment (A), which resulted in more hyperplasia (A) larger number of adenomas (p = 0.003, Linear Regression) (B) and increased cumulative size of adenomas (p = 0.016, Linear Regression) (C). The CyCAP-/- untreated animals also spontaneously developed higher crypt proliferation ratio (p = 0.039, Mann-Whitney Test) (D).
The CyCAP -/- mice spontaneously develop colonic mucosal hyperplasia early in life at 6–8 wk. The difference between this hyperplastic mucosa and normal mucosa of the WT mice is inconspicuous by superficial observation, but statistically, the difference is significant (p < 0.0001, T-test) (20 × magnification, H&E).
The differences in the crypt length and crypt cell content are more obvious between WT and KO animals after the treatment by azoxymethane. After the treatment by azoxymethane, the CyCAP-/- mice develop more extensive mucosal hyperplasia of the colon than WT animals (p < 0.0001, T-test). The mononuclear inflammatory content in the lamina propria is not increased compared to WT animals (20 × magnification, H&E).
In many early adenomas after azoxymethane treatment, hyperplastic-like changes were also present. Adenomatous changes without (A) and with (B) evidence of cytologic dysplasia and cystically dilated crypts and hyperplastic changes in close proximity to muscularis mucosae were found in tumors after azoxymethane treatment (20 × magnification, H&E).
Spectrum of histologic changes in KO mice treated by azoxymethane. Early dysplastic changes were noted in many areas, some of which corresponded to ACF (A). More extensive moderate dysplasia was noted in areas of thickened mucosa (B) and in tumors/adenomas (C). Focal severe dysplasia/carcinoma in situ changes were also note (D).
B-catenin cellular localization in WT and CyCAP KO mice. In WT mice, β-catenin expression is higher in the colonic plate than in the crypts of the colon mucosa (A). However, CyCAP KO mice show overall increased membranous expression of β-catenin with irregular distribution, which focally significantly extended into crypts (B). No definite nuclear localization of β-catenin was detected either in WT or KO mice.
CyCAP null mice had significantly larger numbers of ACF and tumors per animal than control WT animals (p = 0.016, T-Test, Figure 2B). The mean tumor size was larger in CyCAP null mice (p = 0.031, T-Test) as well as cumulative tumor size per animal (p = 0.003, T-Test, Figure 2C). Spectrum of histologic changes is shown in Figure 6.
Beta-catenin was not detected in the nuclei of the colonocytes either in WT or KO mice. Membranous β-catenin was overall less expressed in WT mice than in KO mice (p < 0.0001, Mann-Whitney Test). In WT mice, β-catenin was very weakly expressed in the colonic crypts with more notable expression in the colonic plate/luminal surface of the mucosa (Figure 7A). Membranous β-catenin in CyCAP KO mice is not only overall stronger, but also there is strong expression not only in the colonic plate, but focally also in an irregular fashion including the base of the crypts (Figure 7B). The difference between WT and KO mice in the distribution of β-catenin expression was also highly significant (p < 0.0001, Mann-Whitney Test). This overexpression of the membranous β-catenin is highly variable from one crypt to another. No definite difference in c-myc expression between WT and KO mice was noted. Cyclin D1 expression was significantly higher in KO mice (p < 0.0001, Mann-Whitney Test) and also positively correlated with Ki-67 expression (p = 0.019, Linear-by-Linear Association).
Discussion
Historically, it has been claimed that the transition from hyperplasia to neoplasia is frequent [54, 55]. Human studies and experimental data from animals suggest that high rates of colonic epithelial cell replication enhance the development of colon cancer [56–58]. Exaggerated mucosal proliferative activity is in some way associated with the development of large-bowel neoplasia. Individuals with inflammatory and proliferative diseases of the bowel such as Crohn's disease, ulcerative colitis, and familial polyposis suffer an unusually high risk and early onset of colorectal cancer. However, as mentioned above, this has never been shown in a very common form of colonic mucosal hyperplasia, i.e. hyperplastic polyps [59] and no evidence of diffuse hyperplasia was ever detected in patients with colorectal carcinoma despite demonstrable abnormalities in cell kinetics in histologically normal mucosa in some patients with adenocarcinoma [60] adenomatous polyps [61], familial polyposis [62], and ulcerative colitis [63].
The hyperplasia-neoplasia model has also been challenged at least by one experiment in rodents [64] in which experimentally produced megacolon was associated with reactive mucosal hyperplasia, but showed less malignant tumors than rats without megacolon, both treated by dimethylhydrazine for 20 weeks. One possible interpretation of these results would suggest that experimentally induced reactive hyperplasia is not a premalignant condition and may even be protective of neoplastic transformation. This is in contrast with our findings of increased number of tumors developing in animals with more pronounced mucosal hyperplasia suggesting that colorectal hyperplasia in our model is a preneoplastic change.
In mice, colonic mucosal hyperplasia can be caused by infection. Transmissible murine colonic hyperplasia is the only naturally occurring hyperplastic disease of the colon in mice [65]. This severe but transient mucosal hyperplasia of the distal colon is caused by Citrobacter freundii [48] and was shown to have an expansion of the proliferative zone, an increased labeling index, a prolongation of the cell cycle time, an increase in variation of DNA synthesis times resulting in prolongation of the S phase, and an accelerated migration rate [66]. Interestingly, these findings parallel the "atypical" kinetics found in human and murine preneoplastic and neoplastic disorders of the colon, and also abnormal proliferative kinetics which occur in the flat mucosa of humans between existing tumors or polyps and in the preneoplastic mucosa of rodents treated with carcinogens [60, 62]. Hyperplasia, analogous to tumor promoters which induce proliferation [12], has been shown to reduce the lag period for the appearance of carcinogen-induced neoplastic lesions and to allow their induction with single, subthreshold doses of carcinogen. Our data indicate that the CyCAP null mice spontaneously develop thicker and more proliferative mucosa of the colon, which allowed for marked induction of both additional mucosal hyperplasia and mucosal tumors after the treatment with carcinogen and is in agreement with previous studies, which have indicated that mucosal hyperplasia has a profound effect upon early carcinogenesis [67, 68].
Intraluminal factors including western-style diet/food were found to produce colonic mucosal hyperplasia in experimental animals [69, 70]. However, Delvaux et al. [71] detected an increase in colonic cell proliferation within an excluded colostomy segment. It was also recently demonstrated that serum insulin levels directly correlate with the presence of adenoma and hyperplastic polyps in the proximal colon of humans [72]. The history of tobacco smoking was also associated with higher incidence of hyperplastic polyps [59]. The latter studies suggested that extraluminal factors may also play an important role in the regulation of colonic mucosal growth. Immune regulation and host defense may represent one additional extraluminal factor in regulation of colonic mucosal growth. Suzuki et al. [73] developed an experimental hyperplasia in nu/nu mice by transfer of lymphocytes from the C57BL/6 mice infected by murine leukemia virus (LP-BM5). Lymphocyte transfer to nu/nu mice induced colitis and hyperplasia of intestinal epithelial cells. In contrast to CyCAP null mice in our study, which did not show any mucosal inflammation in addition to the hyperplasia, these mice developed marked mononuclear infiltrates rich in CD4+/CD45RBlow T-cells. Suzuki et al. [73] work shows that in such model, hyperplasia of the colon may be due to defects in immunoregulatory mechanisms. TAA90K belongs to an ancient protein superfamily which is defined by a scavenger receptor cysteine-rich (SRCR) domain [41]. It is particularly noteworthy that all the previously characterized SRCR domains occur in proteins involved in or thought to participate in critical functions of the cellular host defense system, and thus they resemble the immunoglobulin superfamily of the cysteine-containing protein domains (reviewed in ref. 31). Histochemically, Mac-2 has been located intracellularly in many members of the macrophage lineage, including tissue macrophages, certain dendritic cells, alveolar and Kupffer cells [74, 75]. Importantly, Jallal et al. [23] showed that engineered enhancement of 90 K expression results in significant (> 80%) tumor growth inhibition, not by direct action on the tumor cells, but by stimulation of the residual cell-mediated immune defense of the nude mouse.
Recently, Rigby at al. [76] showed a role of suppressor of cytokine signaling-3 (SOCS3) in colonic mucosal epithelial proliferation. Mice with disrupted SOCS3 gene responded with increased proliferation and increased crypt depth after acute dextran sodium sulfate(DSS)-induced mucosal injury or after azoxymethane and chronic DSS. However, the authors did not report spontaneously developing mucosal hyperproliferation and mucosal hyperplasia as it was the case in CyCAP deficient mice in our study. Similarly, Jones et al. [77] reported that conditional deletion of beta-1 integrins in the intestinal epithelium causes a loss of Hedgehog expression and intestinal hyperplasia. However, images illustrated in their publication reveal architectural abnormalities and cytologic atypia, both of which are indicating development of ectopic crypts and adenomas rather than simple lengthening of the crypts, which would indicate hyperplasia only.
Wnt/β-catenin signalling is critically important for colon organogenesis and also for colon carcinogenesis. Wnt protein binding to Frizzled (Fzd) and low-density lipoprotein receptor-related proteins (LRP) causes inactivation of glycogen synthase kinase (GSK) 3β and Axin, respectively. The inactivation of these proteins stabilizes β-catenin, which subsequently accumulates in the cell nucleus and activates the transduction of target genes that are crucial in the G1-S-phase transition and therefore, nuclear β-catenin co-localize with markers of proliferation including c-myc and cyclin D1, and Ki-67 [78, 79]. This pathway also has a critical role in Paneth cell differentiation [80]. We have not observed any morphological or immunohistochemical evidence of increase or aberrant localization of Paneth cells in the colon specimens of the CyCAP knockout mice. Also, no abnormalities of Paneth cells were identified in the small intestine of the CyCAP KO mice. While β-catenin was not detected in the nuclei of the colonocytes in either WT or KO mice and there were no definite difference in expression of the c-myc and cyclin D1, KO mice had increased membranous β-catenin expression compared to their matched WT control and strong expression of β-catenin was also detected in all segments of the colonic crypts including the base indicating that proliferative zone shows β-catenin phenotype that is seen only on the colonic plate of normal mice. Since one way by which cytoplasmic β-catenin is prevented from returning to the nucleus is by being locked by the emerging E-cadherin into adherens junctions which link the cell to proliferatively shut-down functioning cells moving up and out of the crypt, the finding of overexpressed membranous β-catenin in proliferative compartment of the hyperplastic mucosa may represent a significant abnormality; however, it needs to be further evaluated in future studies.
Conclusion
CyCAP knockout mice develop mucosal hyperproliferation and mucosal hyperplasia early in life without exposure to carcinogen and as such they represent the first known model of spontaneous colonic hyperplasia. When challenged by a carcinogen, CyCAP knockout mice also develop significantly more hyperplasia and more tumors than wild-type mice, indicating that their mucosa is more proliferative than in WT animals. Therefore, our results link an early premalignant change in murine colorectal mucosa to deficiency of a glycoprotein with a role in modulation of endotoxin signalling. Further studies are necessary to elucidate if this multifunctional glycoprotein may also have a role in human preneoplastic hyperplasia, the pathogenesis of which is largely unknown.
References
Weir HK, Thun MJ, Hankey BF, Ries LA, Howe HL, Wingo PA, et al: Annual report to the nation on the status of cancer, 1975–2000 featuring the uses of surveillance data for cancer prevention and control. J Natl Cancer Inst. 2003, 95: 1276-99.
Jass JR: Classification of colorectal cancer based on correlation of clinical, morphological and molecular features. Histopathology. 2007, 50: 113-30. 10.1111/j.1365-2559.2006.02549.x.
Levine JS, Ahnen DJ: Adenomatous polyps of the colon. N Engl J Med. 2006, 355: 2551-57. 10.1056/NEJMcp063038.
Longacre TA, Fenoglio-Preiser CM: Mixed hyperplastic adenomatous polyps/serrated adenomas. A distinct form of colorectal neoplasia. Am J Surg Pathol. 1990, 14: 524-37.
Torlakovic E, Skovlund E, Snover CD, Torlakovic G, Nesland JM: Morphologic reappraisal of serrated colorectal polyps. Am J Surg Pathol. 2003, 27: 65-81. 10.1097/00000478-200301000-00008.
Torlakovic E, Snover DC: Sessile serrated adenoma: a brief history and current status. Crit Rev Oncog. 2006, 12: 27-39.
Estrada RG, Spjut HJ: Hyperplastic polyps of the large bowel. Am J Surg Pathol. 1980, 4: 127-33. 10.1097/00000478-198004000-00004.
Shamsuddin AK, Weiss L, Phelps PC, Trump BF: Colon epithelium. IV. Human colon carcinogenesis. Changes in human colon mucosa adjacent to and remote from carcinomas of the colon. J Natl Cancer Inst. 1981, 66: 413-9.
Surawicz CM, Haggitt RC, Husseman M, McFarland LV: Mucosal biopsy diagnosis of colitis: acute self-limited colitis and idiopathic inflammatory bowel disease. Gastroenterology. 1994, 107: 755-63.
Torlakovic E, Snover DC: Serrated adenomatous polyposis in humans. Gastroenterology. 1996, 110: 748-55. 10.1053/gast.1996.v110.pm8608884.
Higuchi T, Sugihara K, Jass JR: Demographic and pathological characteristics of serrated polyps of colorectum. Histopathology. 2005, 47: 32-40. 10.1111/j.1365-2559.2005.02180.x.
Weinstein IB, Troll W: National cancer workshop on tumor promotion and carcinogenesis. Cancer Res. 1977, 37: 3461-63.
Miller EC, Miller JA: Mechanisms of chemical carcinogenesis. Cancer. 1981, 47 (Suppl 5): 1055-64. 10.1002/1097-0142(19810301)47:5+<1055::AID-CNCR2820471302>3.0.CO;2-3.
Sandgren EP, Luetteke NC, Palmiter RD, Brinster RL, Lee DC: Overexpression of TGF alpha in transgenic mice: induction of epithelial hyperplasia, pancreatic metaplasia, and carcinoma of the breast. Cell. 1990, 61: 1121-35. 10.1016/0092-8674(90)90075-P.
Thorup I: Histomorphological and immunohistochemical characterization of colonic aberrant crypt foci in rats: relationship to growth factor expression. Carcinogenesis. 1997, 18: 465-72. 10.1093/carcin/18.3.465.
Huang F, Sauma S, Yan Z, Friedman E: Colon absorptive epithelial cells lose proliferative response to TGF alpha as they differentiate. Exp Cell Res. 1995, 219: 8-14. 10.1006/excr.1995.1198.
Sauma S, Huang F, Winawer S, Friedman E: Colon goblet cells lose proliferative response to TGF alpha as they differentiate. Int J Cancer. 1995, 61: 848-53. 10.1002/ijc.2910610617.
Cartlidge SA, Elder JB: Transforming growth factor alpha and epidermal growth factor levels in normal human gastrointestinal mucosa. Br J Cancer. 1989, 60: 657-60.
Kuniyasu H, Ohmori H, Sasaki T, Sasahira T, Yoshida K, Kitadai Y, Fidler IJ: Production of interleukin 15 by human colon cancer cells is associated with induction of mucosal hyperplasia, angiogenesis, and metastasis. Clin Cancer Res. 2003, 9: 4802-10.
Spring KJ, Zhao ZZ, Karamatic R, Walsh MD, Whitehall VL, Pike T, Simms LA, Young J, James M, Montgomery GW, Appleyard M, Hewett D, Togashi K, Jass JR, Leggett BA: High prevalence of sessile serrated adenomas with BRAF mutations: a prospective study of patients undergoing colonoscopy. Gastroenterology. 2006, 131: 1400-7. 10.1053/j.gastro.2006.08.038.
Iacobelli S, Arno , D'Orazio A, Coletti G: Detection of antigens recognized by a novel monoclonal antibody in tissue and serum from patients with breast cancer. Cancer Res. 1986, 46: 3005-10.
Linsley PS, Horn D, Marquardt H, Brown JP, Hellstrom I, Hellstrom KE, Ochs V, Tolentino E: Identification of a novel serum protein secreted by lung carcinoma cells. Biochem. 1986, 25: 2978-86. 10.1021/bi00358a037.
Koths K, Taylor E, Halenbeck R, Casipit C, Wang A: Cloning and characterization of a human Mac-2-binding protein, a new member of the superfamily defined by the macrophage scavenger receptor cysteine-rich domain. J Biol Chem. 1993, 268: 14245-49.
Jallal B, Powell J, Zachwieja J, Brakebusch C, Germain L, Jacobs J, Iacobelli S, Ullrich A: Suppression of tumor growth in vivo by local and systemic 90 K level increase. Cancer Res. 1995, 55: 3223-27.
Iacobelli S, Bucci I, D'Egidio M, Guiliani C, Natoli C, Tinari N, Rubinstein M, Schlessinger J: Purification and characterization of a 90 kDa protein released from human tumors and tumor cell lines. FEBS. 1993, 319: 59-65. 10.1016/0014-5793(93)80037-U.
Natoli C, Garufi C, Tinari N, D'Egidio M, Lesti G, Gaspari LA, Visini R, Iacobelli S: Dynamic test with recombinant interferon-alpha-2b: effect on 90 K and other tumour-associated antigens in cancer patients without evidence of disease. Br J Cancer. 1993, 67: 564-67.
Iacobelli S, Sismondi M, Giai M, D'Egidio N, Tinari C, Amatetti P, Di Stefano P, Natoli C: Prognostic value of a novel circulating serum 90 K antigen in breast cancer. Br J Cancer. 1994, 69: 172-176.
Greco C, Vona R, Cosimelli M, Matarrese P, Straface E, Scordati P, Giannarelli D, Casale V, Assisi D, Mottolese M, Moles A, Malorni W: Cell surface overexpression of galectin-3 and the presence of its ligand 90 K in the blood plasma as determinants in colon neoplastic lesions. Glycobiology. 2004, 14: 783-92. 10.1093/glycob/cwh092.
Iacobelli S, Ullrich A, Tinari N, Ortona L, Tamburrini E, D'Egidio M, Ghinelli F, Sighinolfi L, Piazza M, Chirianni A, Guerra L, Natoli C: The 90 K tumor-associated antigen and clinical progression in human immunodeficiency virus infection. J of Acq Imm Defic Syn and Hum Retrovir. 1995, 10: 450-56. 10.1097/00042560-199512000-00008.
Natoli C, lacobelli S, Ghinelli F: Unusually high level of a tumor associated antigen in the serum of human immunodeficiency virus seropositive individuals. J Infect Dis. 1991, 164: 616-17.
Resnick D, Pearson A, Krieger M: The SRCR superfamily: a family reminiscent of the Ig superfamily. Trends Biochem Sci. 1994, 19: 5-8. 10.1016/0968-0004(94)90165-1.
Künzli BM, Berberat PO, Zhu ZW, Martignoni M, Kleef J, Tempia-Caliera A, Fukuda M, Zimmermann A, Friess H, Buchler MW: Influences of the lysosomal associated membrane proteins (Lamp-1, Lamp-2) and mac-2 binding protein (Mac-2-BP) on the prognosis of pancreatic carcinoma. Cancer. 2002, 94: 228-39. 10.1002/cncr.10162.
Marchetti A, Tinari N, Buttitta F, Chella A, Angeletti CA, Sacco R, Mucilli F, Ullrich A, Iacobelli S: Expression of 90 K (Mac-2 BP) correlates with distant metastasis and predicts survival in stage I non-small cell lung cancer patients. Cancer Res. 2002, 62: 2535-9.
Ozaki Y, Kontani K, Hanaoka J, Chano T, Teramoto K, Tezuka N, Sawai S, Fujino S, Yoshiki T, Okabe H, Ohkubo I: Expression and immunogenicity of a tumor-associated antigen, 90 K/Mac-2 binding protein, in lung carcinoma. Cancer. 2002, 95: 1954-62. 10.1002/cncr.10899.
Park YP, Choi SC, Kim JH, Song EY, Kim JW, Yoon DY, Yeom YI, Lim JS, Kim JW, Park SG, Lee HG: Up-regulation of Mac-2 binding protein by hTERT in gastric cancer. Int J Cancer. 2007, 120: 813-20. 10.1002/ijc.22369.
Ulmer T, Keeler V, Loh L, Chibbar R, Torlakovic E, André S, Gabius HJ, Laferté S: Tumor-associated antigen 90 K/Mac-2 binding protein: possible role in colon cancer. J Cellular Biochem. 2006, 98: 1351-66. 10.1002/jcb.20784.
Sasaki T, Brakebusch C, Engel J, Timpl R: Mac-2 binding protein is a cell-adhesive protein of the extracellular matrix which self-assembles into ring-like structures and binds beta1-integrins, collagens and fibronectin. EMBO J. 1998, 17: 1606-13. 10.1093/emboj/17.6.1606.
Muller SA, Sasaki T, Bork P, Wolpensinger B, Schulthess T, Timpl R, Engel A, Engel J: Domain organization of Mac-2 binding protein and its oligomerization to linear and ring-like structures. J Mol Biol. 1999, 291: 801-13. 10.1006/jmbi.1999.2996.
Bair E, Nagle R, Ulmer TA, Laferté S, Bowden TG: 90 K/Mac-2 binding protein is expressed in prostate cancer and induces promatrilysin espression. Prostate. 2005, 66: 283-293. 10.1002/pros.20343.
Zucker S, Vacirca J: Role of matrix metalloproteinases (MMPs) in colorectal cancer. Cancer Metastasis Rev. 2004, 23: 101-17. 10.1023/A:1025867130437.
Ullrich A, Sures I, D'Egidio M, Jallal B, Powell TJ, Herbst R, Dreps A, Azam M, Rubinstein M, Natoli C, Shawver L, Schlessinger J, Iacobelli S: The secreted tumor-associated antigen 90 K is a potent immune stimulator. J Biol Chem. 1994, 269: 18401-7.
Powell TJ, Schreck R, McCall M, Hui R, Rice A, App H, Azam M, Ullrich A, Shawver LK: A tumor-derived protein which provides T-cell costimulation through accessory cell activation. J Immunotherapy. 1995, 17: 209-221.
Fornarini B, Iacobelli S, Tinari N, Natoli C, De Martino M, Sabatino G: Human milk 90 K (Mac-2 BP): possible protective effects against acute respiratory infections. Clin Exp Immunol. 1999, 115: 91-4. 10.1046/j.1365-2249.1999.00782.x.
D'Ostilio N, Sabatino G, Natoli C, Ullrich A, Iacobelli S: 90 K (Mac-2 BP) in human milk. Clin Exp Immunol. 1996, 104: 543-46. 10.1046/j.1365-2249.1996.40745.x.
Friedman J, Trahey M, Weissman I: Cloning and characterization of cyclophilin C-associated protein: a candidate natural cellular ligand for cyclophilin C. Proc Natl Acad Sci USA. 1993, 90: 6815-19. 10.1073/pnas.90.14.6815.
Chicheportiche Y, Vassalli P: Cloning and expression of a mouse macrophage cDNA coding for a membrane glycoprotein of the scavenger receptor cysteine-rich domain family. J Biol Chem. 1994, 269: 5512-17.
Trahey M, Weissman IL: Cyclophilin C-associated protein: a normal secreted glycoprotein that down-modulates endotoxin and proinflammatory responses in vivo. Proc Natl Acad Sci USA. 1999, 96: 3006-11. 10.1073/pnas.96.6.3006.
Barthold SW, Coleman GL, Bhatt PN, Osbaldiston GW, Jonas AM: The etiology of transmissible murine colonic hyperplasia. Lab Anim Sci. 1976, 26: 889-94.
Fiala ES: Investigations into the metabolism and mode of action of the colon carcinogens 1,2-dimethylhydrazine and azoxymethane. Cancer. 1977, 40 (5 Suppl): 2436-45. 10.1002/1097-0142(197711)40:5+<2436::AID-CNCR2820400908>3.0.CO;2-U.
Laferté S, Prokopishyn NL, Moyana T, Bird RP: Monoclonal antibody recognizing a determinant on type 2 chain blood group A and B oligosaccharides detects oncodevelopmental changes in azoxymethane-induced rat colon tumors and human colon cancer cell lines. J Cellular Biochem. 1995, 57: 101-119. 10.1002/jcb.240570111.
Bird RP, Good CK: The significance of aberrant crypt foci in understanding the pathogenesis of colon cancer. Toxicol Lett. 2000, 112–113: 395-402. 10.1016/S0378-4274(99)00261-1.
Torlakovic EE, Gomez JD, Driman DK, Parfitt JR, Wang C, Benerjee T, Snover DC: Sessile serrated adenoma (SSA) vs. traditional serrated adenoma (TSA). Am J Surg Pathol. 2008, 32 (1): 21-9. 10.1097/PAS.0b013e318157f002.
Bassarova AV, Torlakovic E, Sedloev T, Hristova SL, Trifonov DV, Nesland JM: Simultaneous bilateral breast carcinoma: Histopathological characteristics and CD44/catenin-cadherin profile. Histol Histopathol. 2005, 20: 791-9.
Willis RA: Pathology of Tumours. 1960, Butterworth, London, UK, 122-126.
Pitot HC, Dragan YP: Facts and theories concerning the mechanisms of carcinogenesis. FASEB J. 1991, 5: 2280-86.
Lipkin M: Phase 1 and phase 2 proliferative lesions of colonic epithelial cells in diseases leading to colonic cancer. Cancer. 1974, 34 (Suppl): 878-88. 10.1002/1097-0142(197409)34:3+<878::AID-CNCR2820340715>3.0.CO;2-R.
Farber E: The multistep nature of cancer development. Cancer Res. 1984, 44: 4217-23.
Bleiberg H, Buyse M, Galan P: Cell kinetic indicators of premalignant stages of colorectal cancer. Cancer. 1985, 56: 124-29. 10.1002/1097-0142(19850701)56:1<124::AID-CNCR2820560119>3.0.CO;2-Y.
Lieberman DA, Prindiville S, Weiss DG, Willett W, VA Cooperative Study Group 380: Risk factors for advanced colonic neoplasia and hyperplastic polyps in asymptomatic individuals. JAMA. 2003, 290: 2959-67. 10.1001/jama.290.22.2959.
Bleiberg H, Galand P: In vitro autoradiographic determination of cell kinetic parameters in adenocarcinomas and adjacent healthy mucosa of the human colon and rectum. Cancer Res. 1976, 36: 325-8.
Deschner EE, Lipkin M: Study of human rectal epithelial cells in vitro. III. RNA, protein, and DNA synthesis in polyps and adjacent mucosa. J Natl Cancer Inst. 1970, 44: 175-85.
Bleiberg H, Mainguet P, andGaland P: Cell Renewalin Familial Polyposis: Comparison between Polyps and Adjacent Healthy Mucosa. Gastroenterology. 1972, 63: 240-245.
Bleibeng H, Mainguet P, Galand P, Chretien J, Dupont-Mairesse N: Cell Renewal in the Human Rectum. "In vitro" Autoradiognaphic Study on Active Ulcerative Colitis. Gastroenterology. 1970, 58: 851-855.
Garcia SB, Oliveira JS, Pinto LZ, Muccillo G, Zucoloto S: The relationship between megacolon and carcinoma of the colon: an experimental approach. Carcinogenesis. 1996, 17: 1777-79. 10.1093/carcin/17.8.1777.
Barthold SW, Coleman GL, Jacoby RO, Livestone EM, Jonas AM: Transmissible murine colonic hyperplasia. Vet Pathol. 1978, 15: 223-36.
Barthold SW: Autoradiographic cytokinetics of colonic mucosal hyperplasia in mice. Cancer Res. 1979, 39: 24-29.
Barthold SW, Jonas AM: Morphogenesis of early 1, 2-dimethylhydrazine-induced lesions and latent period reduction of colon carcinogenesis in mice by a variant of Citrobacter freundii. Cancer Res. 1977, 37: 4352-60.
Barthold SW, Beck D: Modification of early dimethylhydrazine carcinogenesis by colonic mucosal hyperplasia. Cancer Res. 1980, 40: 4451-55.
Bird RP, Schneider R, Stamp D, Bruce WR: Effect of dietary calcium and cholic acid on the proliferative indices of murine colonic epithelium. Carcinogenesis. 1986, 7: 1657-61. 10.1093/carcin/7.10.1657.
Jacobs R: Role of dietary factors in cell replication and colon cancer. Am J Clin Nutr. 1988, 48 (Suppl): 775-79.
Delvaux G, Caes F, Willems G: Refeeding of fasting rats stimulates epithelial cell proliferation in the excluded colon. Gastroenterology. 1984, 86: 802-7.
Yoshida I, Suzuki A, Vallee M, Matano Y, Masunaga T, Zenda T, Shinozaki K, Okada T: Serum insulin levels and the prevalence of adenomatous and hyperplastic polyps in the proximal colon. Clin Gastroenterol Hepatol. 2006, 4: 1225-31. 10.1016/j.cgh.2006.07.002.
Suzuki K, Narita T, Yui R, Ohtsuka K, Inada S, Kimura T, Okada Y, Makino M, Mizuochi T, Asakura H, Fujiwara M: Induction of intestinal lesions in nu/nu mice induced by transfer of lymphocytes from syngeneic mice infected with murine retrovirus. Gut. 1997, 41: 221-28.
Flotte TJ, Springer TA, Thorbecke GJ: Dendritic cell and macrophage staining by monoclonal antibodies in tissue sections and epidermal sheets. Am J Pathol. 1983, 111: 112-24.
Nabarra B, Papiernik M: Phenotype of thymic stromal cells. An immunoelectron microscopic study with anti-IA, anti-MAC-1, and anti-MAC-2 antibodies. Lab Invest. 1988, 58: 524-31.
Rigby RJ, Simmons JG, Greenhalgh CJ, Alexander WS, Lund PK: Suppressor of cytokine signaling 3 (SOCS3) limits damage-induced crypt hyper-proliferation and inflammation-associated tumorigenesis in the colon. Oncogene. 2007, 26: 4833-41. 10.1038/sj.onc.1210286.
Jones RG, Li X, Gray PD, Kuang J, Clayton F, Samowitz WS, Madison BB, Gumucio DL, Kuwada SK: Conditional deletion of beta1 integrins in the intestinal epithelium causes a loss of Hedgehog expression, intestinal hyperplasia, and early postnatal lethality. J Cell Biol. 2006, 175: 505-14. 10.1083/jcb.200602160.
Kim BM, Mao J, Taketo MM, Shivdasani RA: Phases of canonical Wnt signaling during the development of mouse intestinal epithelium. Gastroenterology. 2007, 133: 529-38. 10.1053/j.gastro.2007.04.072.
Andreu P, Peignon G, Slomianny C, Taketo MM, Colnot S, Robine S, Lamarque D, Laurent-Puig P, Perret C, Romagnolo B: A genetic study of the role of the Wnt/beta-catenin signalling in Paneth cell differentiation. Dev Biol. 2008, 5;324: 288-96. 10.1016/j.ydbio.2008.09.027.
Willert K, Nusse R: Beta-catenin: a key mediator of Wnt signaling. Curr Opin Genet Dev. 1998, 8: 95-102. 10.1016/S0959-437X(98)80068-3.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/9/251/prepub
Acknowledgements
Supported by grants from the Cancer Research Society Inc., Canadian Institutes of Health Research (FRN 11185) and an RUH Foundation Grant (G00005255)
This project was performed in part using azoxymethane provided by the National Cancer Institute's Chemical Carcinogen Reference Standards Repository operated under contract by Midwest Research Institute, NO, N02-CB-07008.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
EET participated in the design of the study, carried out morphometric and immunoassays, participated in statistical analysis, and drafted the manuscript. VK helped with animal experiments. CW participated in the histological analyses. HJL participated in the design of the study and the statistical analysis. LAL evaluated and quantitated Ki-67 proliferation fraction. SL conceived of the study, performed experiments with laboratory animals, participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Torlakovic, E.E., Keeler, V., Wang, C. et al. Cyclophilin C-associated protein (CyCAP) knock-out mice spontaneously develop colonic mucosal hyperplasia and exaggerated tumorigenesis after treatment with carcinogen azoxymethane1 . BMC Cancer 9, 251 (2009). https://doi.org/10.1186/1471-2407-9-251
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-9-251