Abstract
Background
Several studies have determined that dietary intake of B vitamins may be associated with breast cancer risk as a result of interactions between 5,10-methylenetetrahydrofolate reductase (MTHFR) and methionine synthase (MTR) in the one-carbon metabolism pathway. However, the association between B vitamin intake and breast cancer risk in Brazilian women in particular has not yet been investigated.
Methods
A case-control study was conducted in São Paulo, Brazil, with 458 age-matched pairs of Brazilian women. Energy-adjusted intakes of folate, vitamin B6, and vitamin B12 were derived from a validated Food Frequency Questionnaire (FFQ). Genotyping was completed for MTHFR A1298C and C677T, and MTR A2756G polymorphisms. A logistical regression model was used to calculate odds ratios (ORs) and 95% confidence intervals (95% CIs).
Results
Neither dietary intake of folate, vitamin B6, or vitamin B12 nor MTHFR polymorphisms were independently associated with breast cancer risk. Analysis stratified by menopausal status showed a significant association between placement in the highest tertile of folate intake and risk of breast cancer in premenopausal women (OR = 2.17, 95% CI: 1.23–3.83; P trend = 0.010). The MTR 2756GG genotype was associated with a higher risk of breast cancer than the 2756AA genotype (OR = 1.99, 95% CI = 1.01–3.92; P trend = 0.801), and statistically significant interactions with regard to risk were observed between the MTHFR A1298C polymorphism and folate (P = 0.024) or vitamin B6 (P = 0.043), and between the MTHFR C677T polymorphism and folate (P = 0.043) or vitamin B12 (P = 0.022).
Conclusion
MTHFR polymorphisms and dietary intake of folate, vitamin B6, and vitamin B12 had no overall association with breast cancer risk. However, increased risk was observed in total women with the MTR 2756GG genotype and in premenopausal women with high folate intake. These findings, as well as significant interactions between MTHFR polymorphisms and B vitamins, warrant further investigation.
Similar content being viewed by others
Background
Folate and other methyl-related B vitamins are essential nutrients which play important roles in DNA synthesis (genetics), repair, and methylation (epigenetics). These roles in turn indicate a potential association for these vitamins with the development of several types of cancer [1–3]. For example, in one folate metabolism pathway, the enzyme 5,10-methylenetetrahydrofolate reductase (MTHFR) irreversibly catalyzes the conversion of 5,10-methylenetetrahydrofolate (5,10-methylene THF) to 5-methyltetrahydrofolate (5-methyl THF), the methyl donor in DNA methylation. In another, folate leads to purine synthesis in DNA repair [2–4]. Activity of the MTHFR gene is attenuated by two common genetic polymorphisms, the MTHFR C677T and A1298C polymorphisms [2, 5]. Methionine synthase (MTR), which catalyzes the remethylation of homocysteine to methionine, has the common genetic polymorphism MTR A2756G [5, 6].
Several studies have suggested an inverse association between folate intake and breast cancer risk in all women [7–13], pre- [7, 8], and postmenopausal women [7–9, 12, 14, 15]. However, recent meta-analysis has shown no clear overall association between folate intake or folate levels in the blood and breast cancer risk [2, 16]. A number of studies have examined MTHFR and MTR polymorphisms [4–6, 17–25] and found that variant genotypes of MTHFR C677T are associated with an increased [4, 17, 22–25] or decreased [5, 20] risk of breast cancer, while those of MTHFR A1298C are associated with a decreased risk [24] and those of MTR A2756G with a decreased risk [6]. Several studies have further reported on the interaction between these MTHFR genotypes and folate intake in affecting risk [4, 19]. In addition to the influence of genotype, DNA methylation and synthesis are also subject to the effects of other vitamins relevant to the one-carbon metabolism pathway, including vitamin B6 (pyridoxine) as a cofactor of MTHFR and vitamin B12 as a cofactor of MTR [4, 6, 19, 26]. Although a role for genotype in modifying the association between dietary intake and disease is biologically plausible [2, 4], research into the protective effects of increasing dietary intake of these B vitamins against breast cancer risk remains inconclusive [2, 27].
In our similar previous case-control study conducted in a Japanese population, we found no significant association between dietary folate intake, MTHFR and MTR genotype, and breast cancer risk [28]. Although the incidence of breast cancer is higher in Brazilian than Japanese women [29], the association between B vitamin intake in the diet, relevant genotypes, and breast cancer risk in Brazilian populations has not been investigated. Here, we conducted a hospital-based case-control study in São Paulo, Brazil, to investigate the role of MTHFR and MTR polymorphisms in modifying the association of folate and other B vitamin intake with breast cancer risk in Brazilian women.
Methods
Subjects
Eligible cases were a consecutive series of female patients aged 20–74 years with newly diagnosed and histologically confirmed invasive breast cancer. Cases were recruited between 2001 and 2006 at eight hospitals in São Paulo which historically treat a relatively large number of Japanese-Brazilian patients. Eligible controls confirmed not to have any cancer were selected from the same hospitals, with one control matched to each case by age (within 5 years) and ethnicity (Caucasian, African, Asian, or mixed) during the study period. Primary reasons for study patients visiting a hospital included health check-up (52%), treatment for gynecological (13%; 64% of which were uterine myoma), urological (8%), and dermatological conditions (6%), clinical examination (8%), and others. Of the eligible cases, 472 patients (389 non-Japanese Brazilian [99%] and 83 Japanese-Brazilian [91%]) gave written informed consent, while among potential controls, 22 patients refused, resulting in a total of 472 matched pairs ultimately enrolled. The study was approved by the Comissão Nacional de Ética em Pesquisa (CONEP), Brasília, Brazil, and by the Institute Review Board of the National Cancer Center, Tokyo, Japan, in 2000.
Data Collection and Dietary Assessment
In-person interviews were conducted by trained interviewers using a structured questionnaire which included questions on demographic characteristics, medical history, family history of cancer, anthropometric factors, smoking habits, physical activities, menstrual and reproductive factors, as well as a self-quantitative FFQ with 118 food terms.
The FFQ used here, developed specifically for this study to estimate dietary intake among participants, inquired about how often participants consumed individual food items (frequency of consumption), as well as about representative relative sizes compared with standard portions in the preceding year (control patients) or one year before their breast cancer diagnosis (cancer patients). Daily food intake was calculated by multiplying frequency by standard portion size and relative size for each food item in the FFQ. Daily intake of nutrients was calculated using the United States Department of Agriculture (USDA) food composition tables [30] and the Fifth Revised and Enlarged Edition of the Standard Tables of Food Composition in Japan [31] for intake regarding Japanese-specific foods. The regression-residual model was used to adjust intake of folate, vitamin B6, and vitamin B12 [32]. Our FFQ included questions on supplement use, but nutrient intake data from supplements were not included in analyses, as no comprehensive data for supplements were available.
The validity of nutrient intake estimated from the FFQ was evaluated in a subsample of the control group. Fifty-five women completed a 4-day dietary record (DR) in two seasons. Spearman's correlation coefficient between energy-adjusted nutrient intakes estimated from the FFQ and DR was 0.30 for folate, 0.38 for vitamin B6, and 0.33 for vitamin B12.
Genotype of Polymorphisms
Peripheral blood samples were obtained from each subject and stored at -80°C until analysis. Genomic DNA samples were extracted from the blood using QIAGEN FlexiGene® DNA kits in accordance with the manufacturer's protocol. Genotyping of the three single-nucleotide polymorphisms (SNPs) in the MTHFR and MTR genes was performed by a commercial laboratory (Genetic Lab., Inc., Sapporo, Japan) using TaqMan® SNP Genotyping Assays developed by Applied Biosystems (Framingham, MA, USA). Cases and matched controls were analyzed in the same well by laboratory personnel blinded to case-control status. To assess quality control, we conducted laboratory genotyping of six SNPs of four genes (N-acetyltransferase 2 [NAT2], cytochrome P450c17α [CYP17], aromatase [CYP19], and cytochrome P450 2E1 [CYP2E1]) using approximately 25% of samples from the present study, although SNPs used in the present study were not included. The concordance rates between Genetic Lab. and our laboratory varied between 97.5% and 99.2% for the six SNPs.
Data Analysis
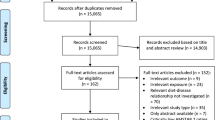
Study subjects with markedly low or high total energy intake (<500 or ≥4000 kcal) or without DNA samples were excluded from the study, leaving 458 pairs of Brazilian women for analysis (379 non-Japanese Brazilian and 79 Japanese-Brazilian pairs). ORs and 95% CIs for associations between dietary intake, polymorphisms, and risk of breast cancer were calculated by the conditional logistical model, and statistical significance was examined by the Wald chi-square test. Baseline characteristics between cases and controls were compared by the Cochran-Mantel-Haenszel test using matched-pair strata. Deviation from the Hardy-Weinberg equilibrium in genotype frequencies was assessed with the chi-square test.
In the primary analysis of all subjects, risk factors identified by univariate analysis as independently related to disease risk, including smoking habit, alcohol consumption, number of live births, and a moderate level of physical activity in the preceding 5 years, were adjusted in multivariable analyses. Other potential confounders such as age at menarche, age at first live birth, breast feeding, number of pregnancies, and breast cancer in first-degree relatives were not independently associated with breast cancer risk, nor did they substantially modify the effects when tested in the multivariable model (less than 10% change in strength), and were thus not retained. Nutrient intakes of folate, vitamin B6, and vitamin B12 were categorized into tertiles for total study subjects based on the distribution among controls, with the lowest tertiles considered as the reference categories.
To increase statistical power, respective genotypes of less-frequent polymorphisms were also combined into two groups. Genotypes of MTHFR 677CC and 1298AA, and MTR 2756AA were considered as the referent group. With regard to evaluation of the interactive effects of SNPs and dietary intakes on breast cancer risk, the combined effects of SNPs and dietary intakes were assessed by adding the multiplicative interaction product (genotype × dietary intake) to the final model as indicator variables.
In a secondary analysis, we stratified patients by menopause status, alcohol consumption, and vitamin supplement use using an unconditional logistic model which adjusted for identified risk factors as well as age and ethnicity. Further, trend testing was conducted by treating each categorized variable as a continuous term and entering the variable into the logistic regression models. All p values reported were two-sided, and the significance level was set at p < 0.05. All analyses were conducted with SAS 9.02 (SAS Institute Inc., Cary, NC, USA).
Results
Characteristics of case and control subjects at baseline are shown in Table 1. The breast cancer case group tended to include more smokers and have higher energy intake, but lower alcohol consumption, less moderate physical activity, fewer live births, and lower vitamin supplement use than the control group.
B Vitamins and Breast Cancer Risk
Using the lowest tertile intake of folate, vitamin B6, and vitamin B12 as reference, no statistically significant association was observed between vitamin intake and breast cancer risk in all women (Table 2). Similar null results were found in Japanese and non-Japanese women, as well as in individuals who refrained from alcohol consumption or vitamin supplement use (data not shown). An increased risk was seen in premenopausal women in the highest tertile of folate intake (P for trend = 0.010) and in postmenopausal women in the highest tertile of vitamin B6 intake (P for trend = 0.047). Similarly, a statistically significant increase in risk was seen for high folate intake in premenopausal women of non-Japanese Brazilian ethnicity (in the highest tertile of folate intake, OR = 1.89, 95% CI = 1.06–3.38; P for trend = 0.037), but not in those of Japanese-Brazilian ethnicity.
Polymorphisms of MTHFR and MTRGenes and Breast Cancer Risk
Associations between polymorphisms of the MTHFR or MTR genes and breast cancer risk are shown in Table 3. No deviation from the Hardy-Weinberg equilibrium was observed in the controls. Compared to the reference group, women with the MTR 2756GG genotype had a significantly increased risk of breast cancer (OR = 1.99, 95% CI = 1.01–3.92; P for trend = 0.801), but no other statistically significant associations were observed for all, pre-, or postmenopausal women. Similar null results were found in both non-Japanese and Japanese-Brazilian women (data not shown), although distribution of the MTHFR C677T polymorphism (CC, CT, and TT genotype) in control subjects differed significantly between the non-Japanese Brazilian (51%, 39%, and 10%, respectively) and Japanese-Brazilian women (35%, 52%, and 13%, respectively) (P = 0.038).
We also examined the effects of combined genotypes of MTHFR A1298C and C677T, MTHFR A1298C and MTR A2756G, and MTHFR C677T and MTR A2756G, none of which was statistically significantly associated with the risk of breast cancer compared to their wild genotypes.
Gene-environment Interactions in Breast Cancer
The joint effects of MTHFR and MTR polymorphisms and dietary intake on breast cancer risk are shown in Table 4, in which the genotypes MTHFR 1298AA and 677CC and MTR 2756AA with the lowest tertiles of dietary intake were used as references, with variant allele combinations. Statistically significant positive associations between folate intake and breast cancer risk were observed among women with the MTHFR 1298AA (P for trend = 0.003), 677CT and TT (P for trend = 0.011), and MTR 2756AA genotypes (P for trend = 0.049). An increased risk of breast cancer was seen in those women with the lowest folate intake who had the MTHFR 1298AC and CC genotype (OR = 1.95, 95% CI = 1.18–3.22). In contrast, a decreased risk was seen in those women with the lowest folate intake who had the MTHFR 677CT and TT genotype (OR = 0.60, 95% CI = 0.37–0.97). Statistically significant interactions were detected for folate intake with MTHFR A1298C (P for interaction = 0.024) and C677T polymorphisms (P for interaction = 0.043).
A marginally positive association was observed between the highest tertile of vitamin B6 intake and breast cancer risk among women with the MTHFR 1298AA genotype (P for trend = 0.061), whereas an inverse association was observed between the highest tertile of vitamin B12 intake and breast cancer risk among those with the MTHFR 677CC genotype (P for trend = 0.073). A statistically significant interaction was detected between the MTHFR A1298C polymorphism and vitamin B6 intake (P for interaction = 0.043) and between the MTHFR C677T polymorphism and vitamin B12 intake (P for interaction = 0.022).
Discussion
In this study, we found no overall association between folate, vitamin B6, and vitamin B12 intake and the risk of breast cancer. These findings are consistent with previous studies on folate [4, 14, 16, 20, 28, 33–40], vitamin B6 [4, 12, 28, 35, 39, 40], and vitamin B12 [8, 15, 28, 39, 40].
Generally, folate is able to prevent the development of tumors before preneoplastic lesions have been established, but conversely increases tumorigenesis once lesions have been established [39, 41, 42]. Although increased folate intake may be beneficial in populations deficient in this nutrient, increased intake in women with already-sufficient levels of folate may provide no further benefit, or actually be harmful [34]. Folate intake in Brazilian women in the present study (inter-tertile range, 446.2–602.2 μg/day) was higher than that measured in a study of Japanese women (inter-tertile range, 386–501 μg/day) [28] and in a meta-analysis of Caucasian and Asian women (inter-tertile range, 77–255 to 147–359 μg/day and 132–304 to 206–473 μg/day) [2]. In this study, we observed an increased risk of breast cancer in premenopausal women with high folate intake. Folate levels may have been already sufficient in the lower intake group, and thus an increase in intake may on this basis have contributed to tumorigenesis.
Similarly, a study on plasma folate found that concentration was associated with an increase in breast cancer risk in premenopausal but not in postmenopausal women [39]. This study also indicated that the proliferation rate of breast epithelial cells may be higher in premenopausal than postmenopausal women, leaving less time for DNA repair in premenopausal women [39]. Further, a large population-based case-control study reported that high dietary vitamin B6 intake was associated with an increased risk of breast cancer, but did not indicate the menopausal status of participants [8]. In contrast, another study found a decreased risk of breast cancer in postmenopausal women with high plasma levels of vitamin B6 [39]. Our finding of a significant increase in breast cancer risk in postmenopausal women due to vitamin B6 intake may thus be due to chance.
A Canadian study found that a high total folate intake, obtained mainly from nutritional supplements, significantly increased breast cancer risk by 32% (highest >853 μg/day versus lowest quintile ≤336 μg/day) in postmenopausal women [33]. The authors hypothesized that high folic acid concentrations may contribute to epigenetic changes in gene-regulatory mechanisms, which may result in gene silencing and enhanced cancer development, or may promote the growth of tumors expressing folate receptors [33, 41]. However, the mechanism of this effect remains unclear [41]. In our study, however, overall vitamin supplement users (defined as more than once-weekly use for at least one year) accounted for 11.8% of controls, and the distribution of supplement users was similar in the highest and lowest intake groups (data not shown). Because folate and other B vitamin intake in our population was thus obtained primarily from unfortified diets, the increased risk of breast cancer in premenopausal women with high folate intake was unlikely due to supplement use.
A recent meta-analysis indicated no overall significant association between the MTHFR C677T polymorphism and breast cancer risk in Caucasians and East Asians, or between the MTHFR A1298C polymorphism and risk in Caucasians [27]. Our study supports the lack of association found in this meta-analysis as well as in others studies in Caucasian and Asian women [1, 5, 43]. In contrast to another finding of the meta-analysis [27], however, which found an increased risk of breast cancer in premenopausal women with the MTHFR 677CT and TT genotype compared to those with the CC genotype, we did not observe any increase in risk in these groups. Further, contrary to the findings in a previous study conducted in Americans [1], we did not find an increased risk of breast cancer to be related to the genotype combination of MTHFR A1298C and C677T. This lack of concordance in findings may be due to the low proportion of the MTHFR 677T genotype in our study population or to compensation by the folate-replete status of patients for the effects of the variant alleles of the MTHFR A1298C and C677T genotypes [2]. Nevertheless, few studies have achieved conclusive results regarding whether functional polymorphisms in one-carbon metabolizing genes affect breast cancer risk associated with dietary intake of folate and other related B vitamins, the biological plausibility of this scenario notwithstanding [2].
The MTR gene contributes to alterations in the plasma levels of homocysteine and folate; specifically, subjects with the 2756AG and GG genotypes have lower levels of plasma homocysteine or higher levels of serum folate than those with the 2756AA genotype [44, 45]. When methionine levels are adequate, these variant polymorphisms with lower enzyme activity may also result in elevated homocysteine levels and DNA hypomethylation [46]. A Polish study reported the possible association between the hetero- and homozygote variants of the MTR A2756G and a decreased risk of breast cancer [6]. In the present study, however, we observed an increased risk of breast cancer in total subjects who had the MTR 2756GG genotype, a finding similar to that reported in a recent study conducted in Taiwan [46]. This observed increase may be due to the linkage between the MTR A2756G polymorphism and other genetic polymorphisms, or to the interaction between the MTR A2756G polymorphism and other genetic polymorphisms related to folate metabolism, such as that for methionine synthase reductase (MTRR G66A) [25, 45], cytosolic serine hydroxymethyltransferase (cSHMT C1420T) [21], or MTHFR C677T [47]. However, we observed no statistically significant associations between the combined genotypes of MTR A2756G and either MTHFR A1298C or C667T and breast cancer risk, nor could we test the joint effects of MTR with MTRR or cSHMT genes since MTRR and cSHMT genes were not available in the present study. Given the low frequency of the MTR 2756GG genotype in our study population, the significant finding of our present study may be the result of chance.
Previous authors have speculated that interactions between folate and MTHFR polymorphism may be elicited to show that (a) the lower activity of variant genotypes may increase the risk of breast cancer at low levels of dietary folate since less 5-methyl THF is made available for DNA methylation, and (b) variant genotypes might provide advantages over the wild genotype in folate-replete conditions since 5,10-methyl THF would be available for nucleotide synthesis [2, 4]. Supporting notion (a), we found an increased risk of breast cancer among women with the lowest folate intake who had the MTHFR 1298AC and CC genotype. Contrary to (a), however, we also saw a decrease in breast cancer risk among women with the lowest folate intake who had the MTHFR 677CT and TT genotype. Similar findings of decreased breast cancer risk in variant MTHFR C677T genotypes have been reported in previous studies in German [5], Japanese-American [20], and Chinese patients [10]. The reduced activity of the MTHFR C677T polymorphism was speculated to increase the pool of intracellular 5,10-methylene THF, which protects against potential defects in DNA synthesis, although circulating folate levels (5-methyl THF) tended to be lower [10]. Nevertheless, the inconsistencies in results between this and previous studies may be due to differences in ethnicity [10, 19], background dietary status [19, 37], or possibly chance. Given the above discussion regarding folate intake level, the increased risk of breast cancer observed here in patients with the MTHFR 1298AA and MTR 2756AA genotype in a higher tertile of folate intake may be due to the harmful effects brought about by excessive intake of folate. Notion (b) suggests that the lower activity of variant alleles of MTHFR A1298C provides advantages over the MTHFR 1298AA genotype, but with the compensation of sufficient folate intake, the lower enzyme activity was attenuated to result in the lack of significant association seen with the variant MTHFR A1298C genotypes in the higher category of folate intake. In addition, the observed trend to a decline in breast cancer risk with increased vitamin B12 intake (P for trend = 0.073) and significant interaction between vitamin B12 and MTHFR C677T polymorphism might be due to the function of vitamin B12 as a cofactor in folate metabolisms [12, 19].
Several limitations of this study warrant mention. First, dietary intake of folate, vitamin B6, and vitamin B12 was assessed after breast cancer diagnosis and was therefore sensitive to recall bias. Case subjects may have been more motivated to recall diet than controls, and their recall may also have been inaccurate, depending on the belief of an association between diet and their disease. Second, although substantially high participation rates among both eligible case and control subjects minimized potential selection bias, the use of cancer-free patients as controls, whose dietary habits may have differed from the general population due to health consciousness or disease concerns, might have lead to selection bias. Third, as our subjects were recruited from eight hospitals in São Paulo, Brazil, they may not necessarily be representative of the general Brazilian population, and thus any extrapolation of results to the general population should be done cautiously. Fourth, our validation study found relatively low correlation coefficients between FFQ and DR-based nutrient intake estimates. Further, the validation study indicated that measurement errors in assessing nutrient intake by FFQ were unavoidable, although such random errors tend to result in null associations [48]. Fifth, although our quality control assessment of the genotyping showed high concordance rates between Genetic Lab. and our laboratory, we did not genotype the duplicate blinded samples of SNPs used in the present study and therefore cannot rule out the possibility of misclassification in genotyping status, although its effect on the results might be minimal. Sixth, stratified analyses were performed based on a relatively small number of cases, possibly limiting the interpretability of our results.
Conclusion
In this case-control study conducted in Brazilian women, we found no overall significant associations between dietary intake of folate, vitamin B6, and vitamin B12, MTHFR genotype, and breast cancer risk. However, we did identify an increased risk of breast cancer in total women with the MTR 2756GG genotype, increased risk associated with higher folate intake in premenopausal women, and gene-nutrient interactions. Further studies into these factors will help to elucidate the etiology of breast cancer.
Abbreviations
- CI:
-
confidence interval
- FFQ:
-
food frequency questionnaire
- MTHFR:
-
5,10-methylenetetrahydrofolate reductase
- MTR:
-
methionine synthase
- OR:
-
odds ratio
- SNPs:
-
single-nucleotide polymorphisms.
References
Stevens VL, McCullough ML, Pavluck AL, Talbot JT, Feigelson HS, Thun MJ, Calle EE: Association of polymorphisms in one-carbon metabolism genes and postmenopausal breast cancer incidence. Cancer Epidemiol Biomarkers Prev. 2007, 16: 1140-7. 10.1158/1055-9965.EPI-06-1037.
Lewis SJ, Harbord RM, Harris R, Smith GD: Meta-analyses of observational and genetic association studies of folate intakes or levels and breast cancer risk. J Natl Cancer Inst. 2006, 98: 1607-22.
Choi SW, Mason JB: Folate and carcinogenesis: an integrated scheme. J Nutr. 2000, 130: 129-132.
Chen J, Gammon MD, Chan W, Palomeque C, Wetmur JG, Kabat GC, Teitelbaum SL, Britton JA, Terry MB, Neugut AI, Santella RM: One-carbon metabolism, MTHFR polymorphisms, and risk of breast cancer. Cancer Res. 2005, 65: 1606-14. 10.1158/0008-5472.CAN-04-2630.
Justenhoven C, Hamann U, Pierl CB, Rabstein S, Pesch B, Harth V, Baisch C, Vollmert C, Illig T, Brüning T, Ko Y, Brauch H: One-carbon metabolism and breast cancer risk: no association of MTHFR, MTR, and TYMS polymorphisms in the GENICA study from Germany. Cancer Epidemiol Biomarkers Prev. 2005, 14: 3015-8. 10.1158/1055-9965.EPI-05-0592.
Lissowska J, Gaudet MM, Brinton LA, Chanock SJ, Peplonska B, Welch R, Zatonski W, Szeszenia-Dabrowska N, Park S, Sherman M, Garcia-Closas M: Genetic polymorphisms in the one-carbon metabolism pathway and breast cancer risk: a population-based case-control study and meta-analyses. Int J Cancer. 2007, 120: 2696-703. 10.1002/ijc.22604.
Negri E, La Vecchia C, Franceschi S: Re: dietary folate consumption and breast cancer risk. J Natl Cancer Inst. 2000, 92: 1270-1. 10.1093/jnci/92.15.1270-a.
Shrubsole MJ, Jin F, Dai Q, Shu XO, Potter JD, Hebert JR, Gao YT, Zheng W: Dietary folate intake and breast cancer risk: results from the Shanghai Breast Cancer Study. Cancer Res. 2001, 61: 7136-41.
Levi F, Pasche C, Lucchini F, La Vecchia C: Dietary intake of selected micronutrients and breast-cancer risk. Int J Cancer. 2001, 91: 260-3. 10.1002/1097-0215(200002)9999:9999<::AID-IJC1041>3.3.CO;2-R. [http://www3.interscience.wiley.com/journal/76502470/abstract]
Chou YC, Wu MH, Yu JC, Lee MS, Yang T, Shih HL, Wu TY, Sun CA: Genetic polymorphisms of the methylenetetrahydrofolate reductase gene, plasma folate levels and breast cancer susceptibility: a case-control study in Taiwan. Carcinogenesis. 2006, 27: 2295-300. 10.1093/carcin/bgl108.
Adzersen KH, Jess P, Freivogel KW, Gerhard I, Bastert G: Raw and cooked vegetables, fruits, selected micronutrients, and breast cancer risk: a case-control study in Germany. Nutr Cancer. 2003, 46: 131-7. 10.1207/S15327914NC4602_05.
Lajous M, Lazcano-Ponce E, Hernandez-Avila M, Willett W, Romieu I: Folate, vitamin B(6), and vitamin B(12) intake and the risk of breast cancer among Mexican women. Cancer Epidemiol Biomarkers Prev. 2006, 15: 443-8. 10.1158/1055-9965.EPI-05-0532.
Zhang SM, Willett WC, Selhub J, Hunter DJ, Giovannucci EL, Holmes MD, Colditz GA, Hankinson SE: Plasma folate, vitamin B6, vitamin B12, homocysteine, and risk of breast cancer. J Natl Cancer Inst. 2003, 95: 373-80.
Zhang S, Hunter DJ, Hankinson SE, Giovannucci EL, Rosner BA, Colditz GA, Speizer FE, Willett WC: A prospective study of folate intake and the risk of breast cancer. JAMA. 1999, 281: 1632-7. 10.1001/jama.281.17.1632.
Lajous M, Romieu I, Sabia S, Boutron-Ruault MC, Clavel-Chapelon F: Folate, vitamin B12 and postmenopausal breast cancer in a prospective study of French women. Cancer Causes Control. 2006, 17: 1209-13. 10.1007/s10552-006-0053-3.
Larsson SC, Giovannucci E, Wolk A: Folate and risk of breast cancer: a meta-analysis. J Natl Cancer Inst. 2007, 99: 64-76.
Campbell IG, Baxter SW, Eccles DM, Choong DY: Methylenetetrahydrofolate reductase polymorphism and susceptibility to breast cancer. Breast Cancer Res. 2002, 4: R14-10.1186/bcr457.
Shrubsole MJ, Gao YT, Cai QY, Shu XO, Dai Q, Jin F, Zheng W: MTR and MTRR Polymorphisms, Dietary Intake, and Breast Cancer Risk. Caner Epidemiol Biomarkers Prev. 2006, 15: 586-8. 10.1158/1055-9965.EPI-05-0576.
Shrubsole MJ, Gao YT, Cai Q, Shu XO, Dai Q, Hébert JR, Jin F, Zheng W: MTHFR polymorphisms, dietary folate intake, and breast cancer risk: results from the Shanghai Breast Cancer Study. Cancer Epidemiol Biomarkers Prev. 2004, 13: 190-6. 10.1158/1055-9965.EPI-03-0273.
Le Marchand L, Haiman CA, Wilkens LR, Kolonel LN, Henderson BE: MTHFR polymorphisms, diet, HRT, and breast cancer risk: the multiethnic cohort study. Cancer Epidemiol Biomarkers Prev. 2004, 13: 2071-7.
Cheng CW, Yu JC, Huang CS, Shieh JC, Fu YP, Wang HW, Wu PE, Shen CY: Polymorphism of cytosolic serine hydroxymethyltransferase, estrogen and breast cancer risk among Chinese women in Taiwan. Breast Cancer Res Treat. 2008, 111: 145-55. 10.1007/s10549-007-9754-x.
Langsenlehner T, Renner W, Yazdani-Biuki B, Langsenlehner U: Methylenetetrahydrofolate reductase (MTHFR) and breast cancer risk: a nested-case-control study and a pooled meta-analysis. Breast Cancer Res Treat. 2008, 107: 459-60. 10.1007/s10549-007-9564-1.
Macis D, Maisonneuve P, Johansson H, Bonanni B, Botteri E, Iodice S, Santillo B, Penco S, Gucciardo G, D'Aiuto G, Rosselli Del Turco M, Amadori M, Costa A, Decensi A: Methylenetetrahydrofolate reductase (MTHFR) and breast cancer risk: a nested-case-control study and a pooled meta-analysis. Breast Cancer Res Treat. 2007, 106: 263-71. 10.1007/s10549-006-9491-6.
Jakubowska A, Gronwald J, Menkiszak J, Górski B, Huzarski T, Byrski T, Edler L, Lubiñski J, Scott RJ, Hamann U: Methylenetetrahydrofolate reductase polymorphisms modify BRCA1-associated breast and ovarian cancer risks. Breast Cancer Res Treat. 2007, 104: 299-308. 10.1007/s10549-006-9417-3.
Suzuki T, Matsuo K, Hirose K, Hiraki A, Kawase T, Watanabe M, Yamashita T, Iwata H, Tajima K: One-carbon metabolism-related gene polymorphisms and risk of breast cancer. Carcinogenesis. 2008, 29: 356-62. 10.1093/carcin/bgm295.
Mason JB: Biomarkers of nutrient exposure and status in one-carbon (methyl) metabolism. J Nutr. 2003, 133 (Suppl 3): 941S-947S.
Zintzaras E: Methylenetetrahydrofolate reductase gene and susceptibility to breast cancer: a meta-analysis. Clin Genet. 2006, 69: 327-36. 10.1111/j.1399-0004.2006.00605.x.
Ma E, Iwasaki M, Kobayashi M, Kasuga Y, Yokoyama S, Onuma H, Nishimura H, Kusama R, Tsugane S: Dietary Intake of Folate, Vitamin B2, Vitamin B6, and Vitamin B12, Genetic Polymorphism of Related Enzymes, and Risk of Breast Cancer: a Case-control Study in Japan. Nutr Cancer.
Tsugane S, de Souza JM, Costa ML, Mirra AP, Gotlieb SL, Laurenti R, Watanabe S: Cancer incidence rates among Japanese immigrants in the city of São Paulo, Brazil, 1969–78. Cancer Causes Control. 1990, 1: 189-93. 10.1007/BF00053172.
U.S. Department of Agriculture, Agricultural Research Service: USDA National Nutrient Database for Standard Reference, Release 18. Nutrient Data Laboratory Home Page. 2006, [http://www.ars.usda.gov/ba/bhnrc/ndl]
Council for Science and Technology; Ministry of Education C, Sports, Science and Technology; the Government of Japan: Standard Tables of Food Composition in Japan, the fifth revised and enlarged edition. 2005, Tokyo: Printing Bureau, Ministry of Finance
Willett W, Stampfer MJ: Total energy intake: implications for epidemiologic analyses. Am J Epidemiol. 1986, 124: 17-27.
Stolzenberg-Solomon RZ, Chang SC, Leitzmann MF, Johnson KA, Johnson C, Buys SS, Hoover RN, Ziegler RG: Folate intake, alcohol use, and postmenopausal breast cancer risk in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial. Am J Clin Nutr. 2006, 83: 895-904.
Ulrich CM: Folate and cancer prevention: a closer look at a complex picture. Am J Clin Nutr. 2007, 86: 271-3.
Wu K, Helzlsouer KJ, Comstock GW, Hoffman SC, Nadeau MR, Selhub J: A prospective study on folate, B12, and pyridoxal 5'-phosphate (B6) and breast cancer. Cancer Epidemiol Biomarkers Prev. 1999, 8: 209-17.
Zhu K, Davidson NE, Hunter S, Yang X, Payne-Wilks K, Roland CL, Phillips D, Bentley C, Dai M, Williams SM: Methyl-group dietary intake and risk of breast cancer among African-American women: a case-control study by methylation status of the estrogen receptor alpha genes. Cancer Causes Control. 2003, 14: 827-36. 10.1023/B:CACO.0000003823.97506.be.
Sharp L, Little J, Schofield AC, Pavlidou E, Cotton SC, Miedzybrodzka Z, Baird JO, Haites NE, Heys SD, Grubb DA: Folate and breast cancer: the role of polymorphisms in methylenetetrahydrofolate reductase (MTHFR). Cancer Lett. 2002, 181: 65-71. 10.1016/S0304-3835(02)00030-7.
Baglietto L, English DR, Gertig DM, Hopper JL, Giles GG: Does dietary folate intake modify effect of alcohol consumption on breast cancer risk? Prospective cohort study. BMJ. 2005, 331: 807-10.1136/bmj.38551.446470.06.
Lin J, Lee IM, Cook NR, Selhub J, Manson JE, Buring JE, Zhang SM: Plasma folate, vitamin B-6, vitamin B-12, and risk of breast cancer in women. Am J Clin Nutr. 2008, 87: 734-43.
Cho E, Holmes M, Hankinson SE, Willett WC: Nutrients involved in one-carbon metabolism and risk of breast cancer among premenopausal women. Cancer Epidemiol Biomarkers Prev. 2007, 16: 2787-90. 10.1158/1055-9965.EPI-07-0683.
Kim YI: Does a high folate intake increase the risk of breast cancer?. Nutr Rev. 2006, 64: 468-75. 10.1111/j.1753-4887.2006.tb00178.x.
Xu X, Gammon MD, Wetmur JG, Bradshaw PT, Teitelbaum SL, Neugut AI, Santella RM, Chen J: B-vitamin intake, one-carbon metabolism, and survival in a population-based study of women with breast cancer. Cancer Epidemiol Biomarkers Prev. 2008, 17: 2109-16. 10.1158/1055-9965.EPI-07-2900.
Lee SA, Kang D, Nishio H, Lee MJ, Kim DH, Han W, Yoo KY, Ahn SH, Choe KJ, Hirvonen A, Noh DY: Methylenetetrahydrofolate reductase polymorphism, diet, and breast cancer in Korean women. Exp Mol Med. 2004, 36: 116-21.
Zhang Z, Shi Q, Liu Z, Sturgis EM, Spitz MR, Wei Q: Polymorphisms of methionine synthase and methionine synthase reductase and risk of squamous cell carcinoma of the head and neck: a case-control analysis. Cancer Epidemiol Biomarkers Prev. 2005, 14: 1188-93. 10.1158/1055-9965.EPI-04-0501.
Silaste ML, Rantala M, Sämpi M, Alfthan G, Aro A, Kesäniemi YA: Polymorphisms of Key Enzymes in Homocysteine Metabolism Affect Diet Responsiveness of Plasma Homocysteine in Healthy Women. J Nutr. 2001, 131: 2643-7.
Yu CP, Wu MH, Chou YC, Yang T, You SL, Chen CJ, Sun CA: Breast cancer risk associated with multigenotypic polymorphisms in folate-metabolizing genes: a nested case-control study in Taiwan. Anticancer Res. 2007, 27: 1727-32.
Le Marchand L, Donlon T, Hankin JH, Kolonel LN, Wilkens LR, Seifried A: B-vitamin intake, metabolic genes, and colorectal cancer risk (United States). Cancer Causes Control. 2002, 13: 239-48. 10.1023/A:1015057614870.
Ishihara J, Otani T, Inoue M, Iwasaki M, Sasazuki S, Tsugane S, Japan Public Health Center-based Prospective Study Group: Low intake of vitamin B-6 is associated with increased risk of colorectal cancer in Japanese men. J Nutr. 2007, 137: 1808-14.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/9/122/prepub
Acknowledgements
This study was supported by a Grant-in-Aid for Research on Risk of Chemical Substances from the Ministry of Health, Labour and Welfare of Japan, and Grants-in-Aid for Scientific Research on Priority Areas (17015049) and for Young Scientists (B) (17790378 and 19790415) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan and Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
EM performed the data analysis and drafted the manuscript. MI participated in the study design, coordinated the study and helped with data integrity, analysis, interpretation, and preparation of the manuscript. JI participated in data analysis and interpretation of data. GH involved the study design, supervised the study, contributed to data acquisition and interpretation. IN involved the study design, and contributed to data acquisition and interpretation. SC contributed to data acquisition and interpretation. JM contributed to data acquisition and interpretation. FL contributed to data acquisition and interpretation. ST designed, supervised and coordinated the study and helped with data interpretation and preparation of the manuscript. All authors have read and approved the final manuscript.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Ma, E., Iwasaki, M., Junko, I. et al. Dietary intake of folate, vitamin B6, and vitamin B12, genetic polymorphism of related enzymes, and risk of breast cancer: a case-control study in Brazilian women. BMC Cancer 9, 122 (2009). https://doi.org/10.1186/1471-2407-9-122
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-9-122