Abstract
Background
A growing body of evidence suggests that variations in the levels of folate may contribute to the development of cancer. A functional polymorphic variant (C→T substitution at nucleotide 677) in the 5,10-methylenetetrahydrofolate reductase (MTHFR) gene results in the conversion of an alanine to a valine and may modify the risk of breast and other cancers.
Method
We have investigated the possible influence of this MTHFR variant on breast cancer risk in a case-control study of 233 healthy women and 335 women who had breast cancer that occurred under the age of 40 years, bilateral breast cancer or a family history of breast cancer.
Results
A significant excess of the valine genotypes was observed among the cases (odds ratio 1.43, 95% confidence interval 1.02–2.00). The effect was more pronounced among the cases with a breast cancer diagnosis under the age of 40 years, with an odds ratio of 1.66 (95% confidence interval 1.12–2.41). A nonsignificant excess of the valine genotypes was observed among the cases with a family history of breast cancer or bilateral breast cancer.
Conclusions
The low activity C677T (valine) genotype of MTHFR may increase the risk of early onset breast cancer.
Similar content being viewed by others
Introduction
The enzyme 5,10-methylenetetrahydrofolate reductase (MTHFR) catalyses the reduction of 5,10-methylenetetrahydrofolate to 5-methyltetrahydrofolate, which is the carbon donor for de novo methionine synthesis and DNA methylation. Approximately 10% of Caucasian populations are homozygous for a common C→T substitution at nucleotide 677 of the MTHFR gene. This mutation converts an alanine to a valine at codon 225 and is associated with reduced enzyme activity and increased thermolability [1]. The potential influence of MTHFR activity on DNA methylation and on the availability of uridylates and thymidylates for DNA synthesis and repair makes MTHFR an attractive candidate for a cancer predisposing gene [2, 3].
Deficiencies in thymidylate have been shown to increase the rate of misincorporation of uridylate into DNA and may in turn lead to an increased rate of DNA strand breaks and other chromosomal damage [4]. Consequently, reduced MTHFR activity, which leads to increased levels of cytosolic 5,10-methylenetetrahydrofolate available for thymidylate synthesis, may protect cells from DNA damage induced by uridylate misincorporation. Consistent with this model, several independent studies have shown that the mutant (valine) allele of MTHFR may confer a twofold reduction in risk of colon cancer [2, 5] and a fourfold reduction in risk of acute lymphocytic leukemia [6]. Mutant MTHFR has also been associated with a 2.8-fold increase in risk of endometrial cancer [7] and a 2.9-fold increase in risk of cervical intraepithelial neoplasia [8]. In the latter situation the increased cancer risk associated with mutant MTHFR might be explained by impairment of DNA methylation due to a reduction in the availability of 5-methyltetrahydrofolate. This is a plausible model because DNA methylation plays a critical role in regulation of gene expression and maintenance of genomic stability [9, 10] and aberrations in normal methylation patterns have been associated with the development of cancer [10, 11]. More recently, Stern et al.[12] demonstrated that individuals who are homozygous for the mutant C677T MTHFR polymorphism show a higher degree of genomic DNA hypomethylation than do homozygotes for the wild-type MTHFR.
The role of folate in breast cancer has been investigated in several dietary studies and most have shown folate consumption to be inversely related to breast cancer risk [13–16]. By contrast, few studies have investigated the influence of the MTHFR C677T polymorphism on breast cancer risk. In one study the frequency of the low MTHFR activity valine allele was reported to occur significantly more frequently in Jewish women diagnosed with bilateral breast cancer or combined breast and ovarian cancer [17]. Another study of unselected breast cancer cases among a Scottish population did not detect any association with the C677T polymorphism and breast cancer risk [18], although the study involved only 62 cases and 66 controls and lacked statistical power.
Given the plausible role of variations in MTHFR activity in breast cancer susceptibility we undertook an analysis of the C677T polymorphism in a case-control study of 335 women with breast cancer and 233 controls.
Materials and methods
Subjects
Women with breast cancer were selected on the basis of an age at onset of less than 40 years, or a family history of breast cancer (defined as two or more cases of breast cancer in a first- or second-degree female relative) irrespective of age at onset, or bilateral breast cancer irrespective of family history or age at onset. All breast cancer cohort cases were systematically ascertained through breast clinics in the Wessex region of southern England as described previously [19]. Briefly, women were invited to take part in a research study, the primary goal of which was to ascertain and verify family histories for segregation analysis. The breast cancer cases diagnosed before 40 years of age were consecutively ascertained without regard to family history. The group of women with bilateral breast cancer were ascertained in the same clinics but the selection criterion was the presence of bilateral breast cancer diagnosed after 40 years of age. The familial breast cancer cases consisted of women presenting to the same clinics with a strong family history of breast or ovarian cancer or both. Family histories were verified as far as possible using medical records and death certificates. Blood was taken from all recruits who consented to molecular analysis for breast cancer predisposition genes. The age range of the women included in the breast cancer cohort was 19–79 with a mean age of 38 years. The controls represent the population from which the cases arose and consisted of 233 Caucasian female volunteers who were either staff at the Princess Anne Hospital, Southampton, UK or patients attending for non-neoplastic disease conditions. The age of the controls ranged from 18 to 84 with a mean age of 39 years. For all groups normal genomic DNA was prepared from blood lymphocytes. Epidemiological data such as reproductive factors, oral contraceptive use, smoking habits and obesity were not obtained for either the cases or controls. Both control and cancer groups were drawn from the same geographical area, which has predominantly an Anglo-Saxon population.
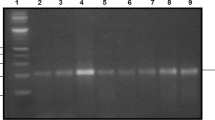
MTHFR genotyping
Genomic DNA from cases and controls was assessed for the presence of the C677T mutation by PCR amplification using an exonic primer (5'-tgaaggagaaggtgtctgcggga-3') and an intronic primer (5'-aggacggtgcggtgagagtg-3') as described previously [1]. PCRs were performed in a reaction volume of 10 μl containing 50 ng of genomic DNA, primers (25 ng of each), 1 × reaction buffer (Genepak, New Milton, UK), 200 nM of dATP, dTTP, dGTP, dCTP (Promega, Annandale, Australia) and 0.2 units of Taq DNA polymerase (Taq Express, Genepak, UK). PCR conditions consisted of an initial denaturation at 94°C for 5 minutes followed by 35 cycles of 94°C for 30 s, 55°C for 30 s, 72°C for 60 s followed by one cycle of 72°C for 5 min. The PCR products were digested with HinfI in a volume of 20 μl and the fragments were separated on 2.0% agarose gels and visualized by ethidium bromide staining. The C→T (valine) variant creates a HinfI restriction enzyme site and produces fragments of 178 basepairs (bp) and 23 bp.
Statistical analysis
Frequency comparisons were analysed using Fisher's exact test. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using the relevant 2 × 2 contingency tables. All statistical calculations were two-sided and performed using InStat version 3.01 (GraphPad Software Inc., San Diego, CA, USA). All statistical tests were based on two-tailed probability.
Results
Table 1 shows the distribution of the C677T polymorphism among the 335 women in the breast cancer cohort and 233 controls. The distribution of the alleles among the controls is consistent with that for previously reported control populations [6, 20]. We did not observe a departure from Hardy–Weinberg equilibrium in the breast cancer or the control groups (P = 0.62 and P = 0.37, respectively).
The frequency of the valine allele among the breast cancer cohort was 0.34, which was higher than that of the controls (0.30), but this was not statistically significant (P = 0.30). The combined number of valine/valine homozygotes and alanine/valine heterozygotes was significantly higher among the breast cancer cases as a whole than among the controls (OR 1.43, 95% CI 1.02–2.00). The significant excess of valine genotypes was only observed among the breast cancer cases diagnosed under the age of 40 years (OR 1.64, 95% CI 1.12–2.41). Interestingly, the valine heterozygotes had a significantly increased OR (OR 1.7, 95% CI 1.2–2.6) while the homozygotes did not (OR 1.4, 95% CI 0.7–2.7). This may be due to the effect of the small number of valine homozygotes.
Discussion
The potential influence of MTHFR activity on DNA methylation and on the availability of uridylates and thymidylates for DNA synthesis and repair makes MTHFR an attractive candidate cancer-predisposing gene. Reduced MTHFR activity leads to increased levels of cytosolic 5,10-methylenetetrahydrofolate, which may protect cells from DNA damage induced by uridylate misincorporation. Indeed, several independent studies have shown that the mutant valine allele of MTHFR may reduce the risk of colon cancer [2, 5, 20] and acute lymphocytic leukemia [6]. Conversely, mutant MTHFR has also been associated with an increase in risk of endometrial cancer [7] and cervical intraepithelial neoplasia [8]. An increased cancer risk conferred by the valine allele may be explained by impairment of DNA methylation due to a reduction in the availability of 5-methyltetrahydrofolate.
Only two previous studies have examined the relationship between the MTHFR C677T polymorphism and breast cancer risk. Gershoni-Baruch et al.[17] reported that the 677T allele occurred significantly more frequently in Jewish women diagnosed with bilateral breast cancer or combined breast and ovarian cancer. Sharp et al. [18] did not observe any significant difference in the genotype distributions within a case-control study of unselected breast cancers from a Scottish population. Comparison of the number of cases that were compound homozygotes of the low-activity 677TT genotype and/or another low-activity MTHFR variant (1298 CC) revealed a significant reduction in risk (OR 0.26), suggesting that low MTHFR activity may protect against breast cancer. While this association is intriguing, the reliability of the conclusion is tempered by the fact that the study included only 62 cases and 66 controls.
Given the plausible role of variations in MTHFR activity in breast cancer susceptibility and the conflicting conclusions of previous studies we undertook an analysis of the C677T polymorphism in a more substantial number of cancers and controls. Our study revealed a significant excess of valine genotypes among the early onset breast cancers (OR 1.43). In contrast to the study by Gershoni-Baruch et al. [17], we did not observe a significant increase in the valine allele frequency among the women diagnosed with bilateral breast cancer or with a family history of breast cancer (although it was higher than in the controls). The data presented by Sharp et al. [18] suggest that low MTHFR activity is associated with a decrease rather than an increase in breast cancer risk. The reliability of their conclusions, however, is limited by the lack of statistical power. The data from our study of 335 cases suggests that, in fact, low MTHFR activity increases the risk of breast cancer. We recognise that the conflicting conclusions may be attributable to the different characteristics of the breast cancer populations studied. Our study included both familial and early onset breast cancers while those of Sharp et al. [18] were unselected cases and those of Gershoni-Baruch et al.[17] were unselected and familial cases occurring among women of Jewish ancestry.
In conclusion, we suggest that low MTHFR activity is associated with an increased risk of early onset breast cancer. It is possible, however, that chance or confounding factors such as ethnicity and the influence of known risk factors such as oral contraceptive use may have generated a false positive result. Consequently it will be important to replicate our findings in larger population-based case-control studies. In addition, it will be important for future studies to incorporate detailed dietary information, because deficiencies in MTHFR activity may be compensated for by increased folate intake and therefore may confound interpretation of the genetic data.
Abbreviations
- bp:
-
= basepairs
- CI:
-
= confidence interval
- MTHFR:
-
= 5,10-methylenetetrahydrofolate reductase
- OR:
-
= odds ratio.
References
Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG, Boers GJ, den Heijer M, Kluijtmans LA, van den Heuvel LP, Rozen RA: Candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nature Genet. 1995, 10: 111-113.
Chen J, Giovannucci EL, Hunter DJ: MTHFR polymorphism, methyl-replete diets and the risk of colorectal carcinoma and adenoma among U.S. men and women: an example of gene-environment interactions in colorectal tumorigenesis. J Nutr. 1999, 129: 560-564.
Potter JD: Colorectal cancer: molecules and populations. J Natl Cancer Inst. 1999, 91: 916-932. 10.1093/jnci/91.11.916.
Blount BC, Mack MM, Wehr CM, MacGregor JT, Hiatt RA, Wang G, Wickramasinghe SN, Everson RB, Ames BN: Folate deficiency causes uracil misincorporation into human DNA and chromosome breakage: implications for cancer and neuronal damage. Proc Natl Acad Sci USA. 1997, 94: 3290-3295. 10.1073/pnas.94.7.3290.
Slattery ML, Potter JD, Samowitz W, Schaffer D, Leppert M: Methylenetetrahydrofolate reductase, diet, and risk of colon cancer. Cancer Epidemiol Biomarkers Prev. 1999, 8: 513-518.
Skibola CF, Smith MT, Kane E, Roman E, Rollinson S, Cartwright RA, Morgan G: Polymorphisms in the methylenetetrahydrofolate reductase gene are associated with susceptibility to acute leukemia in adults. Proc Natl Acad Sci USA. 1999, 96: 12810-12815. 10.1073/pnas.96.22.12810.
Esteller M, Garcia A, Martinez-Palones JM, Xercavins J, Reventos J: Germ line polymorphisms in cytochrome-P450 1A1 (C4887 CYP1A1) and methylenetetrahydrofolate reductase (MTHFR) genes and endometrial cancer susceptibility. Carcinogenesis. 1997, 18: 2307-2311. 10.1093/carcin/18.12.2307.
Piyathilake CJ, Macaluso M, Johanning GL, Whiteside M, Heimburger DC, Giuliano A: Methylenetetrahydrofolate reductase (MTHFR) polymorphism increases the risk of cervical intraep-ithelial neoplasia. Anticancer Res. 2000, 20: 1751-1757.
Kundu TK, Rao MR: CpG islands in chromatin organization and gene expression. J Biochem. 1999, 125: 217-222.
Lengauer C, Kinzler KW, Vogelstein B: DNA methylation and genetic instability in colorectal cancer cells. Proc Natl Acad Sci USA. 1997, 94: 2545-2550. 10.1073/pnas.94.6.2545.
Cheng P, Schmutte C, Cofer KF, Felix JC, Yu MC, Dubeau L: Alterations in DNA methylation are early, but not initial, events in ovarian tumorigenesis. Br J Cancer. 1997, 75: 396-402.
Stern LL, Mason JB, Selhub J, Choi SW: Genomic DNA hypomethylation, a characteristic of most cancers, is present in peripheral leukocytes of individuals who are homozygous for the C677T polymorphism in the methylenetetrahydrofolate reductase gene. Cancer Epidemiol Biomarkers Prev. 2000, 9: 849-853.
Rohan TE, Jain MG, Howe GR, Miller AB: Dietary folate consumption and breast cancer risk. J Natl Cancer Inst. 2000, 92: 266-269. 10.1093/jnci/92.3.266.
Zhang S, Hunter DJ, Hankinson SE, Giovannucci EL, Rosner BA, Colditz GA, Speizer FE, Willett WCA: Prospective study of folate intake and the risk of breast cancer. JAMA. 1999, 281: 1632-1637. 10.1001/jama.281.17.1632.
Goodman JE, Lavigne JA, Wu K, Helzlsouer KJ, Strickland PT, Selhub J, Yager JD: COMT genotype, micronutrients in the folate metabolic pathway and breast cancer risk. Carcinogenesis. 2001, 22: 1661-1665. 10.1093/carcin/22.10.1661.
Negri E, La Vecchia C, Franceschi S: Re: dietary folate consumption and breast cancer risk. J Natl Cancer Inst. 2000, 92: 1270-1271. 10.1093/jnci/92.15.1270-a.
Gershoni-Baruch R, Dagan E, Israeli D, Kasinetz L, Kadouri E, Friedman E: Association of the C677T polymorphism in the MTHFR gene with breast and/or ovarian cancer risk in Jewish women. Eur. Cancer. 2000, 36: 2313-2316. 10.1016/S0959-8049(00)00306-3.
Sharp L, Little J, Schofield AC, Pavlidou E, Cotton SC, Miedzybrodzka Z, Baird JO, Haites NE, Heys SD, Grubb DA: Folate and breast cancer: the role of polymorphisms in methylenete-trahydrofolate reductase (MTHFR). Cancer Lett. 2002, 181: 65-71. 10.1016/S0304-3835(02)00030-7.
Eccles DM, Englefield P, Soulby MA, Campbell IG: BRCA1 mutations in southern England. Br J Cancer. 1998, 77: 2199-2203.
Ma J, Stampfer MJ, Giovannucci E, Artigas C, Hunter DJ, Fuchs C, Willett WC, Selhub J, Hennekens CH, Rozen R: Methylenete-trahydrofolate reductase polymorphism, dietary interactions, and risk of colorectal cancer. Cancer Res. 1997, 57: 1098-1102.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Campbell, I.G., Baxter, S.W., Eccles, D.M. et al. Methylenetetrahydrofolate reductase polymorphism and susceptibility to breast cancer. Breast Cancer Res 4, R14 (2002). https://doi.org/10.1186/bcr457
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/bcr457