Abstract
Background
Based on the site of breakpoint in t(9;22) (q34;q11), bcr-abl fusion in leukemia patients is associated with different types of transcript proteins. In this study we have seen the association of HLA genes with different types of bcr-abl transcripts. The association could predict the bcr-abl peptide presentation by particular HLA molecules.
Methods
The study included a total of 189 patients of mixed ethnicity with chronic myelogenous leukemia and acute lymphocytic leukemia who were being considered for bone marrow transplantation. Typing of bcr-abl transcripts was done by reverse transcriptase PCR method. HLA typing was performed by molecular methods. The bcr-abl and HLA association was studied by calculating the relative risks and chi-square test.
Results
Significant negative associations (p < 0.05) were observed with HLA-A*02 (b2a2, e1a2), -A*68 (b2a2, b3a2, e1a2), -B*14 (b2a2, b3a2, e1a2), -B*15 (b2a2, b3a2), -B*40 (b2a2), -DQB1*0303 (b2a2, b3a2), -DQB1*0603 (b2a2), -DRB1*0401 (e1a2), -DRB1*0701 (b3a2), and -DRB1*1101 (b2a2).
Conclusions
The negative associations of a particular bcr-abl transcript with specific HLA alleles suggests that these alleles play a critical role in presenting peptides derived from the chimeric proteins and eliciting a successful T-cell cytotoxic response. Knowledge of differential associations between HLA phenotypes and bcr-abl fusion transcript types would help in developing better strategies for immunization with the bcr-abl peptides against t(9;22) (q34;q11)-positive leukemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The t(9;22) (q34;q11) translocation seen in 90% of patients with chronic myelogenous leukemia (CML) and about 10% patients with acute lymphocytic leukemia (ALL) results in juxtaposition of the 3' segment of the c-abl proto-oncogene on chromosome 9 with the 5' segment on the bcr gene on chromosome 22 [1–6]. Breaks in c-abl gene generally involve exon 2, also known as a2. Breaks in the bcr occur in one of the three following regions: the major breakpoint cluster region (M-bcr), the minor breakpoint cluster region (m-bcr) or the micro breakpoint cluster region (μ-bcr) [7]. Breakpoints occurring in m-bcr involve introns 13 and 14 and join exon 13 or 14 with abl, resulting in the fusion transcripts e13a2 (also known as b2a2) and e14a2 (also known as b3a2), respectively. These transcripts lead to production of a 8.5-kb transcript coding for a 210-kD chimeric protein (p210) [8, 9]. Breakpoints in m-bcr involve the first intron of bcr, exon 1 joins with abl, resulting in a smaller fusion transcript, e1a2, that codes for a 190-kD protein (p190) [10]. Breakpoints in the μ-bcr involve intron 19, the joining of exon 19 with abl results in a fusion transcript e19a2, that codes for a 230-kD protein (p230) [11]. Although tyrosine kinase is activated in all bcr-abl fusion transcripts, the p190 form has been shown to have more transforming potential than p210 in vitro and in vivo [12–14]. Fusion transcripts b3a2 and b2a2, which are translated into p210, account for the majority of CML cases, while the fusion transcript e1a2, which is translated into p190, is seen primarily in t(9;22)-positive ALL and the blastic phase of CML [10, 15]. The rare fusion transcript e19a2, resulting in p230, is associated primarily with the entity known as chronic neutrophilic leukemia [16].
Several reports indicate an association between t(9;22) (q34;q11) and different human leukocyte antigen (HLA) alleles. This association suggests a possible role for T-cell cytotoxicity in the pathogenesis of diseases linked to bcr-abl fusion proteins resulting from t(9;22) (q34;q11). Different HLA alleles have different predilections for the sequence of peptides they can present to T cells. In order to elicit a T-cell response, a peptide must bind to the HLA molecule prior to its presentation to the T cell. Since a given HLA allele can bind and present only peptides with certain sequence constraints, the ability of an individual to elicit a successful T-cell cytotoxic response to cells carrying foreign or newly mutated proteins depends on the set of HLA alleles that individual has inherited. Thus, individuals carrying certain HLA alleles capable of binding peptides derived from bcr-abl fusion transcripts can in principle be considered to have a biological advantage in fighting the disease over individuals lacking these particular HLA alleles.
In studying the association between the distribution of HLA alleles in patients with different types of bcr-abl transcripts, a positive association suggests that a particular HLA allele does not effectively bind and present peptides derived from a given bcr-abl transcript. Likewise, a negative association suggests that the binding and presentation of a peptide is effective and elicits a successful T-cell cytotoxic response with destruction of leukemia cells.
The aim of this study was to analyze the disease association between HLA alleles and bcr-abl fusion transcripts in greater detail than has so far been studied. First, we assessed the HLA association with a particular bcr-abl transcript, i.e., b2a2 or b3a2 or e1a2, and not with CML in general. Second, unlike earlier studies that were limited to low-resolution allele typing, this study used high-resolution typing for HLA class II genes.
Methods
A total of 189 patients comprising of 163 with CML and 26 with ALL, all with t(9;22) (q34;q11) and known HLA types, were included in this study. Of these patients, 28 expressed b2a2 and b3a2 transcripts, while 68 expressed the b2a2 transcript, 76 the b3a2 transcript, and 17 the e1a2 transcript. The comparisons were made with healthy, potential bone marrow donors that were HLA typed at our laboratory. 376 donors were typed for HLA class I and 267 donors for HLA class II. The donor population is a multiracial group of both related and unrelated prospective bone-marrow donors with no significant clinical history. The gene frequencies are not at odds with reported gene frequencies in general populations for prevailing races. We decided to use our internal gene frequencies from this donor population for three reason: First, it is a multiracial group in which no racial bias was made, more representative of the population the reported patients came from than any specific racial group typically used to determine HLA gene frequencies. Second, it is a group for which high-resolution high-quality typing is readily available making it possible to evaluate allelic gene frequency differences, rather than differences at the serologic low-resolution level. Third, it is a group for which not only the HLA phenotype is available, but also the genotype, that is, the haplotypes were determined in each case, particularly in regard to class II genes.
Typing of bcr-ablfusion transcripts by reverse-transcriptase PCR
Leukocytes prepared by erythrocyte lysis of bone marrow aspirate (1–2 ml) and peripheral blood (10 ml) samples collected in ethylene diamine tetraacetic acid were used for RNA isolation. Total RNA was isolated by using Trizol reagent (Invitrogen Lifetechnologies, USA) according to the manufacturer's instruction. The integrity of RNA was determined by gel electrophoresis prior to reverse transcription (RT). Total RNA (1–5 μg) from samples with intact 28 s and 18 s RNA was converted to cDNA by using random hexamers and Superscript II reverse transcriptase (Invitrogen Lifetechnologies) according to the recommendations of the manufacturer.
Each sample was amplified in duplicate for bcr-abl in a multiplex RT-PCR using an abl primer in combination with bcr b2- and e1-specific primers [17]. The t(9;22)-positive cell lines KBM7, K562, and B15, which carry b2a2, b3a2, and e1a2 fusion genes, respectively, served as positive controls. [18, 19] The HL60 cell line was used as negative control.
HLA typing
HLA typing was performed by molecular methods. For class I, HLA typing was done at the intermediate-resolution level by using enzyme linked probe hybridization assay with sequence-specific oligonucleotide probe (ELPHA-SSOP) (Biotest, Germany). The sequence-specific oligonucleotide probes were used to identify polymorphic sequence motifs. The hybridization between probe and target DNA from the series of amplified PCR products was detected by a method adapted from the protein enzyme linked immunosorbent assay (ELISA) technique. For class II, HLA typing was done at the high-resolution level by using the sequence specific primers (SSP) (Genovision, USA or Pel-freez, USA). The technique uses a battery of known sequence specific primers to amplify specific alleles or group of alleles. This typing method is based on the fact that a completely matched primer will be used more efficiently in the PCR reaction than a partially mismatched primer. The electrophoresis bands generated were compared with the kit standards.
Statistical analysis
HLA gene frequencies (not phenotype frequency) were calculated in two different populations: (1) Healthy individuals typed as potential candidates for donating bone marrow; and (2) Patients diagnosed as having CML or ALL in whom bcr-abl transcripts were identified.
The sizes of the gene pools of these populations for HLA typing are shown in Table 1. In order to obtain more accurate gene frequencies, the largest population of typed donors was used. This resulted in a larger population for class I genes (376 individuals) than for class II genes (268 individuals). The frequencies of the HLA-A, -B, -DRB1 and -DQB1 alleles for the three groups of CML patients with different bcr-abl transcripts were compared with their gene frequencies in the healthy donor group. The frequencies of HLA alleles in patients were evaluated in 192 chromosomes of patients with b2a2 transcirpts (96 individuals, 68 with only b2a2 and 28 with both b2a2 and b3a2); 208 chromosomes of patients with b3a2 (104 individuals, 76 with only b3a2 and 28 with both b2a2 and b3a2); and 34 chromosomes of patients with e1a2 (17 individuals). The comparisons were made by calculating the relative risks. Chi-squares were also calculated to assess the statistical significance of the differences. With (ν) = (r-1)(c-1) = 1 degree of freedom and a significance level of α = 0.05 needed to reject the null hypothesis, the χ2 statistic must be > 3.84. Since ours is an international referral center with a patient population of diverse racial backgrounds, it was not possible to compare the patient data with the standard HLA frequencies based on ethnicity. We therefore used the healthy bone marrow donor population for comparison.
The binding scores were calculated on the basis of the amino acid sequence of the peptide and the HLA molecule as described elsewhere [20–22]. The sequences of e1a2, b3a2, and b2a2 junctional peptides are EGAFHGDAEALQRPVAS [10, 15], ATGFKQSSKALQRPVAS [23], and IPLTINKEEALQRPVAS [24].
Results and discussion
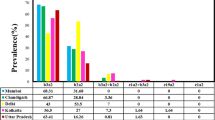
Our findings are summarized in Tables 2,3,4, which include only statistically significant observations with χ2 > 3.84, corresponding to a significance level of p < 0.05. Relative risk > 1 indicates that a particular HLA allele is more frequent in a patient population with a particular transcript than within the corresponding healthy population. Relative risk < 1 indicates a negative association, with a gene frequency significantly smaller than in the corresponding general population. Significant negative associations with b2a2 were seen with HLA-A*02, -A*68, -B*14, -B*15, -B*40, -DQB1*0303, -DQB1*0603, and -DRB1*1101. Significant positive association was seen with HLA-A*01, -A*23, -A*66, -B*37, -B*38, -B*42, -B*45, -B*49, -B*53, -B*56, -B*62, -DQB1*0201, -DQB1*0402, -DQB1*0609, -DRB1*0301, -DRB1*0302, -DRB1*0901, -DRB1*1001, -DRB1*1201, -DRB1*1202, and -DRB1*1503 (Table 2).
Significant negative associations with b3a2 were seen with HLA-A*68, -B*14, -B*15, -DQB1*0303, and DRB1*0701. Significant positive association were seen with HLA-A*25, -B*37, -B*49, -B*51, -B*53, -B*56, -B*60, -B*62, -DQB1*0609, -DRB1*0405, -DRB1*0802, -DRB1*0901, -DRB1*1001, and -DRB1*1503 (Table 3).
Significant negative associations with e1a2 were seen with HLA-A*02, -A*68, -B*14, and -DRB1*0401. Significant positive association were seen with HLA-A*01, -A*11, -A*26, -B*08, -B*49, -B*53, -B*62, -DQB1*0201, -DQB1*0502, -DRB1*0301, -DRB1*0802, and DRB1*1601 (Table 4).
The relative maximum binding scores of various peptides with the HLA types are also shown in the corresponding tables. The scores are particularly high for HLA-A*02, -A*68, -B*14, and -B*53 (all with b2a2), HLA-A*68, -B*14, and -B*62 (all with b3a2) and HLA-A*01, -A*02, -B*08, and -B*14 (all with e1a2).
Interestingly, 1.6% of patients with t(9;22) (q34;q11) lacked HLA-DRB3, -DRB4, and -DRB5 alleles. This contrasts with the healthy group of which only 0.13% lacked these alleles. The 2 × 2 contingency table analysis yielded a likelihood ratio of 25 and a χ2 of 42.8, indicating a statistical significance of p < 0.001.
The presence of bcr-abl transcripts in patients with leukemia appears to be associated with both HLA class I and II alleles. In general, exogenous antigens are processed to peptides in the endocytic compartment and are presented by HLA class II to CD4+ T cells. On the other hand, endogenous peptides resulting from cleavage of proteins are transferred by the transport-associated proteins to the endocytoplasmic reticulum. In the endocytoplasmic reticulum, these peptides bind to newly synthesized HLA class I molecules, and the resulting complexes are transported to the cell surface to be recognized by CD8+ T cells. It has been shown however, that endogenous antigens can be processed by both class I and class II HLA molecules [25–27]. The bcr-abl transcripts in leukemia cells would be endogenous peptides and would normally be presented by HLA class I molecules. In our study and other studies cited in Table 5, negative associations with both HLA class I and II alleles have been seen. A possible explanation is that the bcr-abl transcripts are presented by both HLA class I and class II.
There are published reports of both negative and positive associations of bcr-abl transcripts with HLA class I and class II alleles (Table 5). By a positive association it is meant that individuals having a particular bcr-abl transcript are more likely to be endowed with a particular HLA phenotype. By a negative association it is meant that individuals showing a particular bcr-abl transcript are less likely to have a given HLA phenotype. Most of these studies were done with low-resolution HLA typing data. Posthuma et al claimed that HLA-A3 and -B8 are associated with a diminished risk of development of CML [28]. On the basis of a large multi-center data from the European bone marrow transplant program (n = 1462), they also claimed that HLA-DR4 is associated with diminished risk of CML. They compared patient data with data from unaffected individuals from the registry of bone marrow donors worldwide (n = 500596). The patients and controls were matched by country. The odds ratio for HLA-DR3 was 0.86 (95% confidence interval CI 0.75–0.98) and for -DR4 combined with -B8, was 0.84 (95% CI 0.72–0.98) [29]. A limitation of this study was that no high-resolution class II typing was done. It was also assumed that all the CML patients expressed the p210 protein, which is present in a majority but not all cases of CML. Pawelec and Wagner have questioned their claim on the basis of its reliance on low-resolution typing and have stressed the need for high-resolution HLA typing [30]. Our present study not only used high-resolution HLA class II typing but also included all three types of bcr-abl transcripts (b2a2, b3a2, and e1a2). Significant negative associations with p < 0.05 was seen with HLA-A*02 (b2a2, e1a2), -A*68 (b2a2, b3a2, e1a2), -B*14 (b2a2, b3a2, e1a2), -B*15 (b2a2, b3a2), -B*40 (b2a2), -DQB1*0303 (b2a2, b3a2), -DQB1*0603 (b2a2), -DRB1*0401 (e1a2), -DRB1*0701 (b3a2), and -DRB1*1101 (b2a2). In a similar study using high-resolution HLA-DRB1 typing, Yasukawa et al reported positive association with HLA-DRB1*1201 (b2a2), and -DRB1*0403, -DRB1*0802, -DRB1*1403, DRB1*1405 (all with b3a2), and a negative association with -DRB1*0405, -DRB1*08032, -DRB1*1502 (all with b2a2) and -DRB1*08032, and -DRB1*1501 (both with b3a2) in a Japanese population (Table 5) [36]. However, the study included only 50 cases and included no patients with the e1a2 transcript. Furthermore, association with HLA-DQB1 typing was not assessed. Our study had a larger population (n = 189) though of mixed ethnicity. The common findings of the two studies include positive association with HLA-DRB1*1201 (b2a2) and -DRB1*0802 (b3a2). There were no common HLA alleles with a negative association.
Tabe 6 shows HLA class II haplotypes with increased frequency in patients with the various types of bcr-abl transcripts.
The patients in our study had HLA class II typing that included HLA-DRB1*, -DRB3*, -DRB4*, -DRB5*, -DQB1* and -DPB1*. We included in our results the statistical data on HLA-DRB1* and -DQB1*. Our study is unique among published reports by incorporating HLA-DQB1 data. Unlike HLA-DRB1 and -DQB1, HLA-DRB3, -DRB4, and -DRB5 are not expressed by all individuals; expression depends on the haplotype. An interesting observation was the fact that the frequencies of absence of HLA-DRB3, -DRB4 and -DRB5 phenotype were higher in the patient pool then in the healthy donors. This could imply that HLA-DRB3, -DRB4, and -DRB5 alleles are associated with bcr-abl transcript presentation.
The bcr-abl transcripts can generate a T-cell response [31–34]. Successful allogeneic, autologous, and HLA-identical sibling dendritic cell immunization strategies against CML with b3a2-p210 peptide have also been tried, with generation of T-cell response [35–39]. There are reports of successful in vitro generation of HLA-DRB1*1501-restricted p190 minor bcr-abl (e1a2)-specific CD4+ T lymphocytes in ALL [40, 41]. The restriction was confirmed by loss of the cytotoxic effect in the presence of anti-HLA-DR and preservation of the effect when anti-HLA class I was used.
Conclusions
It seems that bcr-abl peptides are presented by many different HLA types. The negative association could occur because the early leukemogenic events are contained by a T-cell cytotoxic response and this prevents disease proliferation. A positive association could mean that the HLA molecules do not present the bcr-abl transcripts. We hold the theoretical assumption that HLA-restricted T-cell cytotoxicity performs an immunosurveillance role in the pathogenesis of bcr-abl-transcript leukemias. Should this assumption hold, knowledge of the HLA association with different bcr-abl transcripts would have diagnostic and prognostic implications. It would also help in improving strategies of immunization with the bcr-abl peptides against t(9;22) (q34;q11) leukemia.
References
Nowell PC, Hungerford DA: A minute chromosome in human chronic granulocytic leukemia. Science. 1960, 132: 1197-1200.
Catovsky D: Ph1-positive acute leukaemia and chronic granulocytic leukaemia: one or two diseases?. Br J of Haematol. 1979, 42: 493-498.
Rowley JD: A new consistent chromosomal abnormality in chronic myelogenous leukemia identified by quinacrine fluorescence and Giemsa staining. Nature. 1973, 243: 290-293.
de Kleinn A, Van Kessel AG, Grosveld D, Bartram CR, Hagemeijer A, Bootsma D, Spurr NK, Heisterkamp N, Groffen J, Stephenson JR: A cellular oncogene is translocated to the Philadelphia chromosome in chronic myelocytic leukemia. Nature. 1982, 300: 765-767.
Groffen J, Stephenson JR, Heisterkamp N, de Klein A, Bartram CR, Grosveld G: Philadelphia chromosomal breakpoints are clustered within a limited region, bcr, on chromosome 22. Cell. 1984, 36 (1): 93-99. 10.1016/0092-8674(84)90077-1.
Kantarjian HM, Deisseroth A, Kuzrock R, Estrov Z, Talpaz M: Chronic myelogenous leukemia: A concise update. Blood. 1993, 82: 691-703.
Melo JV: The diversity of BCR-ABL fusion proteins and their relationship to leukemia phenotype. Blood. 1996, 88: 2375-2384.
Shtivelman E, Lifshitz B, Gale RP, Canaani E: Fused transcript of abl and bcr genes in chronic myelogenous leukemia. Nature. 1985, 315: 550-554.
Ben-Nariah Y, Daley GQ, Mes-Masson AM, Witte ON, Baltimore D: The chronic myelogenous leukemia-specific p210 protein is the product of the bcr-abl hybrid gene. Science. 1986, 233: 212-214.
Hermans A, Heisterkamp N, von Linden M, van Baal S, Meijer D, vander Plas D, Wiedermann LM, Groffen J, Bootsma D, Grosveld G: Unique fusion of bcr and c-abl genes in Philadelphia chromosome-positive acute lymphoblastic leukemia. Cell. 1987, 51: 33-40. 10.1016/0092-8674(87)90007-9.
Saglio G, Guerrasio A, Rosso C, Zaccaria A, Tassinari A, Serra A, Rege Cambrin G, Mazza U, Gavosto F: New type of BCR/ABL junction in Philadelphia chromosome-positive chronic myelogenous leukemia. Blood. 1990, 76: 1819-1824.
McLaughlin J, Chianese E, Witte ON: Alternative forms of the bcr-abl oncogene have quantitatively different potencies for stimulation of immature lymphoid cells. Mol Cell Biol. 1989, 9: 1866-1874.
Lugo TG, Pendergast AM, Muller AJ, Witte ON: Tyrosine kinase activity and transformation potency of bcr-abl oncogene products. Science. 1990, 247: 1079-1082.
Heisterkamp N, Jenster G, Ten Hoeve J, Zovich D, Pattengale PK, Groffen J, Bootsma D, Grosveld G: Acute leukemia in BCR/ABL transgenic mice. Nature. 1990, 344: 251-253. 10.1038/344251a0.
Fainstein E, Marcelle C, Rosner A, Canaani E, Gale RP, Dreazen O, Smith SD, Croce CM: A new fused transcript in Philadelphia chromosome-positive acute lymphocytic leukaemia. Nature. 1987, 330: 386-388. 10.1038/330386a0.
Pane F, Frigeri F, Sindona M, Luciano L, Ferrara F, Cimino R, Meloni G, Saglio G, Salvatore F, Rotoli B: Neutrophilic-chronic myeloid leukemia: a distinct disease with a specific molecular marker (BCR/ABL with C3/A2 junction). Blood. 1996, 88: 2410-2414.
Cross NC, Feng L, Chase J, Bungey J, Hughes TP, Goldman JM: Competitive polymerase chain reaction to estimate the number of BCR-ABL transcripts in chronic myeloid leukemia patients after bone marrow transplantation. Blood. 1993, 82: 1929-1936.
Lozzio CB, Lozzio BB: Human chronic myelogenous lekemia cell-line with positive Philadelphia chromosome. Blood. 1975, 45: 321-334.
Andersson BS, Collins VP, Kurzrock R, Larkin DW, Childs C, Ost A, Cork A, Trujillo JM, Freireich EJ, Siciliano MJ, Deisseroth AB: KBM-7, a human myeloid leukemia cell line with double Philadelphia chromosomes lacking normal c-ABL and BCR transcripts. Leukemia. 1995, 9: 2100-2108.
Cano P, Fan B, Stass S: A geometric study of the amino acid sequence of class I HLA molecules. Immunogenetics. 1998, 48: 324-334. 10.1007/s002510050439.
Cano P, Fan B: A geometric and algebraic view of MHC-peptide complexes and their binding properties. BMC Structural Biology. 2001, 1: 2-10.1186/1472-6807-1-2.
Cano P: The propositional calculus of peptide binding to the major histocompatibility complex. In: Immunobiology of the Human MHC: Proceedings of the 13th International Histocompatibility Workshop and Conference, Seattle, WA. 2002,
Mannering SI, McKenzie JL, Fearnley DB, Hart DNJ: HLA-DR1-restricted bcr-abl (b3a2)-specific CD4+ T lymphocytes respond to dendritic cells pulsed with b3a2 peptide and antigen presenting cells exposed to b3a2-containing cell lysates. Blood. 1997, 90: 290-297.
Grosveld G, Verwoerd T, van Agthoven T, de Klein A, Ramchandran KL, Heisterkamp N, Stam K, Groffen J: The chronic myelocytic cell line K562 contains a breakpoint in bcr and produces a chimeric bcr/c-abl transcript. Mol Cell Biol. 1986, 6 (2): 607-616.
Nuchtern JG, Biddison WE, Klausner RD: Class II MHC molecules can use the endogenous pathway of antigen presentation. Nature. 1990, 343: 74-76. 10.1038/343074a0.
Weiss S, Bogen B: MHC class II restriction presentation of intracellular antigen. Cell. 1991, 64: 767-776.
Mainati MS, Marti M, LaVaute T: Processing pathways for presentation of cytosolic antigen to MHC class II-restricted T cells. Nature. 1992, 357: 702-704. 10.1038/357702a0.
Posthuma EFM, Falkenburg JHF, Apperley JF, Roosnek E, Oudshoorn M, Schipper RF, Schreuder GMT, D'Amaro J, van Biezen JH, Hermans J, Willemze R, Niederwieser D: HLA-B8 and HLA-A3 coexpressed with HLA-B8 are associated with a reduced risk of the development of chronic myeloid leukemia. Blood. 1999, 93: 3863-3865.
Posthuma EFM, Falkenburg JHF, Apperley JF, Hertenstein B, Schipper RF, Oudshoorn M, v Biezen JH, Hermans J, Willemze R, Roosnek E, Niederwieser D: HLA-DR4 is associated with a diminished risk of the development of chronic myeloid leukemia (CML). Leukemia. 2000, 14: 859-862. 10.1038/sj.leu.2401774.
Pawelec G, Wagner W: Is HLA-DR4 or the HLA-DRB1*0402 allele association with decreased risk for CML?. Leukemia. 2001, 15 (5): 192-193. 10.1038/sj.leu.2401946.
ten Bosch GJ, Joosten AM, Kessler JH, Melief CJ, Leeksma OC: Recognition of BCR-ABL positive leukemic blasts by human CD4+ T cells elicited by primary in vitro immunization with a BCR-ABL breakpoint peptide. Blood. 1996, 88: 3522-3527.
ten Bosch GJ, Toornvliet AC, Friede T, Melief CJM, Leeksma OC: Recognition of peptides corresponding to the joining region of p210 bcr-abl protein by human T cells. Leukemia. 1995, 9: 1344-1348.
Yasukawa M, Ohminami H, Kojima K, Hato T, Hasegawa A, Takahashi T, Hirai H, Fujita S: HLA class II-restricted antigen presentation of endogenous bcr-abl fusion protein by chronic myelogenous leukemia-derived dendritic cells to CD4+ T lymphocytes. Blood. 2001, 98: 1498-1505. 10.1182/blood.V98.5.1498.
Yasukawa M, Ohminami H, Kaneko S, Yakushijin Y, Nishimura Y, Inokuchi K, Miyakuni T, Nakao S, Kishi K, Kubonishi I, Dan K, Fujita S: CD4+ cytotoxic T-cell clones specific for bcr-abl b3a2 fusion peptide augment colony formation by chronic myelogenous leukemia cells in a b3a2-specific and HLA-DR-restricted manner. Blood. 1998, 92: 3355-3361.
Osman Y, Takahashi M, Zheng Z, Koike T, Toba K, Liu A, Furukawa T, Aoki S, Aizawa Y: Generation of bcr-abl-specific cytotoxic T-lymphocytes by using dendritic cells pulsed with bcr-abl (b3a2) peptide: its applicability for donor leukocyte transfusions in marrow-grafted CML patients. Leukemia. 1999, 13: 166-174. 10.1038/sj/leu/2401311.
Westermann J, Kopp J, Korner I, Richter G, Qin Z, Blankenstein T, Dorken B, Pezzutto A: Bcr/abl+ autologous dendritic cells for vaccination in chronic myeloid leukemia. Bone Marrow Transplant. 2000, 25 (Suppl 2): S46-49.
Cullis JO, Barett AJ, Goldman JM, Lechler RI: Binding of BCR/ABL junctional peptides to major histocompatibility complex (MHC) class I molecules: studies in antigen processing defective cell lines. Leukemia. 1994, 8: 165-170.
Pinilla-Ibarz J, Cathcart K, Korontsvit T, Soignet S, Bocchia M, Caggiano J, Lai L, Jimenez J, Kolitz J, Scheinberg DA: Vaccination of patients with chronic myelogenous leukemia with bcr-abl oncogene breakpoint fusion peptides generates specific immune responses. Blood. 2000, 95: 1781-1787.
Baxevanis CN, Voutsas IF, Tsitsilonis QE, Gritzapis AD, Sotiriadou R, Papamichail M: Tumor-specific CD4+ T lymphocytes from cancer patients are required for optimal induction of cytotoxic T cells against the autologous tumor. J Immunol. 2000, 164: 3902-3912.
Tanaka Y, Takahashi T, Nieda M, Masuda S, Kashiwase K, Ogawa S, Chiba S, Juji T, Hirai H: Generation of HLA-DRB1*1501-restricted p190 minor bcr-abl (e1a2)-specific CD4+ T lymphocytes. Br J of Haematol. 2000, 109: 435-437. 10.1046/j.1365-2141.2000.02018.x.
Tanaka Y, Takahashi T, Nieda M, Masuda S, Kashiwase K, Takahashi T, Ogawa S, Chiba S, Juji T, Hirai H: Generation of FAS-independent CD4 + cytotoxic T cell clone specific for p190 minor bcr-abl fusion peptide. Leuk Res. 2002, 26: 317-321. 10.1016/S0145-2126(01)00119-9.
Yasukawa M, Ohminami H, Kojima K, Inokuchi K, Nishimura Y, Fujita S: Analysis of HLA-DRB1 alleles in Japanese patients with chronic myelogenous leukemia. Am J Hematol. 2000, 63 (2): 99-101. 10.1002/(SICI)1096-8652(200002)63:2<99::AID-AJH8>3.0.CO;2-#.
Yotunda P, Firat H, Garcia-Pons F, Garcia Z, Gourru G, Vernant J, Lemonnier FA, Leblond V, Langlade-Demoyen P: Cytotoxic T-cell response against the chimeric p210 BCR-ABL protein in patients with chronic myelogenous leukemia. J Clin Invest. 1998, 101: 2290-2296.
Bocchia M, Korontsvit T, Xu Q, Mackinnon S, Yang SY, Sette A, Scheinberg DA: Specific human cellular immunity to bcr-abl oncogene-derived peptides. Blood. 1996, 87: 3587-3592.
Greco G, Fruci D, Accapezzato D, Barnaba V, Nisini R, Alimena G, Montefusco E, Vigneti E, Butler R, Tanigaki N, Tosi R: Two bcr-abl junctional peptides bind HLA-A3 molecules and allow specific induction of human cytotoxic T lymphocytes. Leukemia. 1996, 10: 693-699.
ten Bosch GJ, Kessler JH, Joosten AM, Bres-Vloemans AA, Geluk A, Godthelp BC, van Bergen J, Melief CJ, Leeksma OC: A BCR-ABL oncoprotein p210 b2a2 fusion region sequence is recognized by HLA-DR2a-restricted cytotoxic T lymphocytes and presented by HLA-DR-matched cells transfected with an L-Ii (b2a2) construct. Blood. 1999, 94 (3): 1038-1045.
Norbury LC, Clark RE, Christmas SE: b3a2 BCR-ABL fusion peptides as targets for cytotoxic T cells in chronic myeloid leukemia. Br J of Haematol. 2000, 109 (3): 616-621. 10.1046/j.1365-2141.2000.02090.x.
Clark RE, Dodi IA, Hill SC, Lill JR, Aubert G, Macintyre AR, Rojas J, Bourdon A, Bonner PL, Wang L, Christmas SE, Travers PJ, Creaser CS, Rees RC, Madrigal JA: Direct evidence that leukemic cells present HLA-associated immunogenic peptides derived from the BCR-ABL b3a2 fusion protein. Blood. 2001, 98 (10): 2887-2893. 10.1182/blood.V98.10.2887.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/4/25/prepub
Acknowledgements
We wish to acknowledge the editorial assistance by Ms. Kathryn Hale, Department of Scientific Publications, M. D. Anderson Cancer Center.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Authors' contributions
SM carried out the data collection and analysis and writing the manuscript. The bcr-abl typing was done in the lab of RL. HLA typing was done in the lab supervised by PC. RL and PC did the study design and analysis of the data. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Mundhada, S., Luthra, R. & Cano, P. Association of HLA Class I and Class II genes with bcr-abl transcripts in leukemia patients with t(9;22) (q34;q11). BMC Cancer 4, 25 (2004). https://doi.org/10.1186/1471-2407-4-25
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-4-25