Abstract
Background
Colorectal surgery is associated with postoperative infectious complications in up to 40% of cases, but the diagnosis of these complications is frequently misleading, delaying its resolution. Several biomarkers have been shown to be useful in infection diagnosis.
Methods
We conducted a single-centre, prospective, observational study segregating patients submitted to elective colorectal surgery with primary anastomosis, CRP and PCT were measured daily. We compared infected and non-infected patients.
Results
From October 2009 to June 2011, a total of 50 patients were included. Twenty-one patients developed infection. PCT and CRP before surgery were equally low in patients with or without postoperative infectious complications. After surgery, both PCT and CRP increased markedly. CRP time-course from the day of surgery onwards was significantly different in infected and non-infected patients (P = 0.001) whereas, PCT time-course was almost parallel in both groups (P = 0.866). Multiple comparisons between infected and non-infected patients from 5th to 9th postoperative days (POD) were performed and CRP concentration was significantly different (P < 0.01, Bonferroni correction), on the 6th, 7th and 8th POD. A CRP concentration > 5.0 mg/dl at the D6 was predictive of infection with a sensitivity of 85% and a specificity of 62% (positive likelihood ratio 2.2, negative likelihood ratio 0.2).
Conclusions
After a major elective surgical insult both CRP and PCT serum levels increased independently of the presence of infection. Besides serum CRP time-course showed to be useful in the early detection of an infectious complication whereas PCT was unhelpful.
Similar content being viewed by others
Background
Elective colorectal surgery is associated with postoperative infectious complications in up to 40% of the cases [1, 2]. Despite recent advances in both surgical technique and perioperative care, infectious complications remain a major clinical problem in colorectal surgery, contributing to significant postoperative morbidity, increased mortality, prolonged hospital stay and additional costs [3–6]. As a result, early diagnosis of the infectious complications is a crucial step in order to initiate treatment as soon as possible [7].
Nonetheless, the diagnosis of infectious complications after elective colorectal surgery is frequently misleading, delaying its resolution. Consequently the availability of an early sensitive and specific marker of postoperative infectious complications would be of great interest [8].
Several biomarkers of infection, namely C-reactive protein (CRP) and procalcitonin (PCT), have been shown to be useful in the diagnosis of infection in different clinical settings as well as in the assessment of its response to antibiotic therapy [9–11].
C-reactive protein has been studied by several authors as an early predictor of abdominal septic complications after esophageal, pancreatic and rectal resection with sensitivities and specificities between 65 and 80% [12–15]. Reith et al. used PCT to identify patients with postoperative complications after elective surgery of the colon and the aorta [16]. In this study, on the first postoperative day (POD) serum PCT was higher in patients with complications (6.9 versus 1.12 ng/mL) [16]. However, the preoperatively PCT levels were already higher in the group with complication.
C-reactive protein (CRP) is one of these biomarkers and probably the most widely used. In different infections and clinical settings, the course of relative CRP variations and the CRP ratio, can discriminates, early in the clinical course, survivors from non-survivors [17, 18][19]. The identification of the individual pattern of CRP ratio response to antibiotic therapy appears to be a reflection of the clinical course of infection independently of other possible confounders [20].
Recently Oberhofer and colleagues [21] demonstrated in a prospective study in patients submitted to elective colorectal surgery that CRP concentrations were not inferior to PCT levels in identifying patients with infectious postoperative complications. In this study ROC curve analysis showed that CRP concentrations on POD 3 and PCT concentrations on POD 2 had similar predictive values for the development of infectious complications (AUC 0.746 and 0.750, respectively).
To the best of our knowledge, this is the only study that compared the diagnostic accuracy of CRP and PCT for early detection of postoperative complications in patients undergoing colorectal surgery.
The present study was designed to assess the value of serum CRP and PCT time course in the postoperative setting of elective colorectal surgery with primary anastomosis and its potential in detecting infectious postoperative complications.
Methods
The present study was a prospective, single centre, observational study conducted during a 21 months period, between October 2009 and June 2011, in the General Surgery Department of São Francisco Xavier Hospital. Our hospital is a central and university hospital of Lisbon that belongs to a Hospital of 900 beds. Fifty patients with elective colon resections with primary anastomosis were prospectively included in the present study. Inclusion criteria were age >18 and elective colon resections. Patients were excluded if they were on systemic antibiotics at the time of surgery, if it was not able to obtain an informed consent and if they were in other clinical trial. The West Lisbon Hospital Centre Ethics Committee previously approved the study. Informed consent was obtained from all patients or legal representative before surgery.
Data collection and definitions
Data on patient demographics, surgical procedures, postoperative mortality and morbidity were prospectively collected from medical records. The baseline characteristics of the patients enrolled in the study are detailed in Table 1.
Postoperative infectious complications were defined as follows: anastomotic leakage (AL), abscess, surgical site infection, pneumonia, urinary tract infections and central line infections.
Patients underwent further postoperative diagnostic test or treatment only in case of symptoms or signs of an infectious complication. An AL was verified either by radiography enema performed with computed tomography scan, x-ray or by endoscopy. Abscesses were verified by purulent drainage or during re-laparotomy. Surgical site infection was diagnosed by the presence of clear signs of inflammation at the wound margin or purulent drainage from the wound [22]. Diagnosis of central line infection required positive blood cultures and cultures from the catheter tip with the same microorganism [23]. Pneumonia was diagnosed by the presence of new pulmonary infiltration chest radiography or in chest CT scan accompanied by clinical symptoms of the lower respiratory tract or on physical or laboratory exam [24]. Urinary tract infection was defined by positive urine sediment analysis combined with fever and/or leukocytosis [25].
Pneumonia and UTI were treated with antibiotics; central line infections were treated with antibiotics and removal of the catheter; surgical site infections were treated with drainage and antibiotics; AL and abdominal abscess were treated with re-laparotomy and antibiotics.
Serum CRP, PCT, white cell count (WCC), platelets and higher body temperature were recorded routinely before surgery, and on POD 1 to 12 or before if the patient was discharge earlier.
Biomarkers measurements
Measurement of CRP was performed by an immunoturbidimetric method (Tina-quant CRP; Roche Diagnostics, Mannheim, Germany). The precision of the assay measured by the intra- and inter-assay coefficient of variation was < 7%, the sensitivity of the method was 0.1 mg/dL and the detection limit was 0.3 mg/dL.
Procalcitonin was quantified by sensitive time-resolved amplified cryptate emission assay (Kryptor PCT, B.R.A.H.M.S AG, Hennigsdorf, Germany). The precision of the assay measured by the intra- and inter-assay coefficient of variation was between 2 and 3%, the sensitivity of the method was 0.01 ng.mL−1 and the detection limit was 0.06 ng.mL−1.
Comparison between infected and non-infected patients after elective colorectal surgery with primary anastomosis was performed.
Statistics
Results are expressed as the mean ± standard deviation unless stated otherwise. To assess differences between the two main groups, infected and non-infected patients, the Student's t test and the Mann–Whitney U test were used for continuous variables and the χ2 test was used for categorical variables. Time dependent analysis of different variables was performed with a general linear model, univariate, repeated-measures analysis using a split-plot design approach.
Median values with interquartile range were used for graphical visualization. Logistic regression models were used to determine if each biomarker from the POD5 to POD9 was associated with complications. Bonferroni correction was used to counteract the problem of multiple comparisons [26].
The diagnostic accuracy was evaluated with area under the curve (AUC), using the ROC methodology [27]. The AUCs were computed using the non parametric trapezoidal method and their 95% confidence limits were computed according to method established by DeLong [28].
Results were reported as the odds ratio with a 95% confidence interval. Significance was accepted for P < 0.05 unless otherwise stated. Data were analyzed using PASW Statistics v.18.0 (SPSS, Chicago, IL).
Results
Baseline and outcomes
From October 2009 to June 2011, a total of 50 patients were prospectively included.
Infectious complications were diagnosed in 21 patients (42%): sixteen surgical site infections, one AL, one intra-abdominal abscess and three extra-abdominal infections. The median day of diagnosis of complications was POD7 (interquartile range (IQR) 5–12). Infection was less frequent in men (28% vs. 72%, P = 0.042).
Diagnosis, comorbidities and surgical procedures were similar in patients with and without infectious complications.
Of the 50 patients, 14 (28%) were admitted in the Intensive Care Unit and two (4%) patients died due to nosocomial infections. Clinical and demographics characteristics are expressed in Table 1.
White cell count, platelets and body temperature time course
Mean preoperative values of WCC, platelets and body temperature were similar in infected and non-infected patients (Table 1). In the POD1, WCC increased in both groups, being slightly higher in the infected group although not reaching statistical significance (Figure 1C).Platelets decreased after surgery, reaching the lower value on the POD2 and gradually increased thereafter in both groups (Figure 1D).Body temperature was significantly higher on the POD6 in patients who developed a post-operative infection complication (P = 0.003) (Figure 1E), however the absolute difference between the infected and non-infected group was only 0.3°C. These findings promote the use of biomarkers to help the discrimination between infection and non-infection promoting an earlier focus control, since clinical data are many times insufficiently.
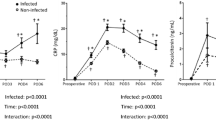
Observed means of C-reactive protein (A), procalcitonin (B), white cell count (C), platelets (D) and temperature (E) during the first 12 days after elective colo-rectal surgery for non-infected (dashed line) and infected (solid line) patients. Error bars represent point-wise 95% confidence intervals.
CRP and PCT time course
The levels of CRP and PCT before surgery were very low and similar in patients with an uneventful course as well as in those that went on to develop an infectious complication (0.1 ± 0.06 vs. 0.07 ± 0.04 ng/ml; 1.81 ± 2.83 vs. 0.72 ± 1.12 mg/dl, respectively). After surgery, in the POD1, both CRP and PCT increased : CRP increased more than 15× and peaked at 48 hrs; PCT increased around 10× the basal level and peaked at 24 to 48 hrs (Figure 1A and B).The CRP time-course from the day of surgery onwards was significantly different in infected and non-infected patients (P = 0.001). After the postoperative peak at 48 hrs, CRP decreased persistently in patients with an uneventful postoperative course (Figure 1A). In opposition, in those that will develop an infectious complications CRP decreased from during the POD2 and POD3 until reaching a concentration plateau between POD4 to POD9. After resolution of infection complication, CRP decreased again reaching at POD12 values close to those of non-infected patients. The lack of decrease in CRP levels in the post operative period is a predictor of post-operative infections in patients submitted to colorectal surgery. In opposition, the PCT time-course was almost parallel in both groups, infected and non-infected (P = 0.866) (Figure 1B).
To assess the diagnostic performance of each biomarker, we performed multiple comparisons between infected and non-infected patients from the POD5 to POD9. The CRP concentration was significantly different (P < 0.01, after Bonferroni correction), on the POD6, POD7 and POD8. The CRP levels predicted the infection in general one-day earlier, since the mean of postoperative infection occurred on POD7.
The results of the CRP ROC analysis to assess the diagnostic performance of surgical infectious complications are shown on Table 2. As early as the POD6, a CRP concentration >5.0 mg/dl was associated to with occurrence of infectious complications, with a sensitivity of 85% and a specificity of 62% (positive likelihood ratio 2.2, negative likelihood ratio 0.2).
Discussion
The early identification of patients who developed infectious complications is crucial for timely and adequate treatment. Severe sepsis is still a major cause of postoperative morbidity and mortality after major surgery, with an incidence ranging between 9 to 12% and high mortality (42% to 80%) [1, 29–32].
In our study the rate of infectious complications after elective colonic surgery was high, 42%, however the majority (36%) were surgical site infections. An AL was diagnosed in only one patient. The mortality was 4%, similar to the outcomes described in other studies [33, 34].
Septic complications after colorectal resection consist mainly of surgical site infections (up to 40%), pulmonary infections (10%) and urinary infections (5%) [2]. Anastomotic leakage and intraabdominal abcess are the most feared complications and are frequently diagnosed late in the postoperative period since the initial clinical manifestations are very subtle. About 30% of patients admitted to the ICU with intraabdominal infection died, with mortality rates even higher when peritonitis arises as a complication of a previous operative procedure [35, 36].
A method for the early identification of patients at risk for pos-operative infection would be of clinical importance, since clinical signs are usually insensitive and do not allow an early diagnosis. Several biochemical tests are used to identify persistent inflammatory activity in postoperative patients, including CRP, PCT and interleukins.
The early identification of patients at risk for post-operative infection would be of clinical importance, since clinical signs are usually insensitive and do not allow an early diagnosis. Several biochemical tests are used to identify persistent inflammatory activity in postoperative patients, including CRP, PCT and interleukins [37–39].
In our study, only CRP demonstrated to be useful in discriminating between infected and non-infected patients. The CRP levels predicted the infection in general on POD 6–7, one-day earlier, than the (median) day of post operative infection diagnosis. PCT and the other inflammatory markers were not useful in discriminating between infected and non-infected patients. Despite body temperature at POD6 was significantly higher in patients who developed a post-operative infection complication the difference between groups was only 0.3°C and no clinical significance was attributable. Recently, in a similar study Oberhofer et al. [21] demonstrated that both CRP and PCT in the early postoperative period, with a significant difference between patients with and without infectious complications.
In our study, PCT failed to discriminate between infected and non-infected patients. Meyer et al. recently reported in literature that in critically ill surgical patients an increase in PCT levels did not help to predict surgical complications [40].
It is well known that after of the presence a major elective surgical insult both CRP and PCT serum levels markedly increased independently of infection. It is demonstrated that by using a model of systemic inflammation after intravenous endotoxin administration, showed that PCT levels in healthy subjects reached a maximum by 24 h and remained above normal for >7 days. In contrast, CRP had normalized in the same subjects by 7 days [41]. Despite this data clinical studies are controversial Lindberg et al. in a series of 47 patients with major abdominal surgery and a uneventful post-operative course, mean CRP increased in the first 48 hrs and reached half its maximum value on the POD5 whereas PCT declined after 24 hrs [42]. On the other hand Meissner et al. [43] described that peak PCT levels are reached within 24 hours postoperatively and return to normal levels within the first week, depending the degree of PCT elevation on the intraoperative course and the type of the surgical procedure.
In our study the peak of PCT was reached between 24 and 48 hrs, after this period PCT could not discriminate between infected and non-infected patients. In our study after the postoperative peak at 48 hrs, CRP decreased persistently in patients with an uneventful postoperative course and at POD11 CRP was <50% the basal level.
CRP kinetics has been recently described by several authors as a predictive of infectious postoperative complications [15, 44]. CRP has been studied in detecting AL after rectal resection. Two recent studies reported that persistently increased CRP values after POD 2–4 were associated to a later diagnosis of an AL [15–45].These authors found that prolonged elevation and/or a absence of decline in CRP levels were associated with more infectious complications and poor outcome [15, 44].
More recently Warschkow et al. [46] demonstrated that CRP values exceeding 123 mg/l on POD 4 where associated a higher risk of infectious complications. These authors found that CRP level above 143 mg/L had a good diagnostic accuracy to detect infectious complications with an AUC ROC 0.76 [46]. We found similar results and CRP time course showed to be useful in the early detection of an infectious complication after elective colorectal surgery. The highest diagnostic accuracy was observed for CRP measured on POD 8, with an AUC of 0.75. However, already by POD6, that is to say 1 day before the median day of infectious diagnosis, the CRP AUC was 0.74.
Some authors advocate the use of PCT as an early biomarker of infection. Takakura et al. recently reported in 18 patients with surgical site infections (SSI) in patients undergoing elective colorectal resection that PCT was significantly higher than CRP levels [47]. Nevertheless higher PCT levels were found on POD1 that could be due to the surgical insult. Reith et al. found, in a prospective study involving 70 patients, 35 with intra-abdominal colorectal elective surgery, that PCT levels were closely related to postoperative complications (severe pneumonia, ischemia, and AL) [16]. PCT was measured preoperatively and postoperatively from day 1 to 5 and on days 7 and 10. These authors could not found any differences between groups in other markers of infection such as WCC, CRP, IL-6 and body temperature. However preoperative CRP concentrations in complicated patients were already significantly higher compared to those who do not develop complications, questioning if there was underlying infection prior to surgery. Novotny et al. more recently found in 104 patients with secondary peritonitis that PCT ratio appears to be helpful in distinguishing between patients with successful eradication of the septic focus and those with a persisting infectious focus [48]. In this study CRP was not evaluated [48]. Recently Lagoutte et al. in a study that included patients undergoing elective colorectal surgery could not found differences between PCT and CRP for the detection of AL with a better AUC ROC for CRP on POD 4 [49]. Despite this data were not confirmed by the Garcia-Granero group that demonstrated a PCT superiority in the AL diagnosis [50], both studies only study the AL complication and did not performed a time dependent analysis study.
Our data found that PCT time course could not differentiate between patients who developed complications with lower AUC ROC than those found in CRP.
Few studies have investigated the use of PCT in the diagnosis of intra-abdominal infections. While PCT showed promise as a marker to exclude perforation and ischaemia in obstructive bowel syndrome, the utility in acute appendicitis and pancreatitis was limited [51–54].
In 1993, Assicot et al. showed in children that PCT levels were high in severe bacterial infections in contrast with those who had absent, localized or viral infections [55]. Some authors advocate that patients who have a localised infection without a general systemic response do not appear to have high levels of serum PCT. An extrapolation as been made to patients who do not develop a marked systemic inflammatory response syndrome such as the elderly or the malnourished patient, although this has not been tested [56].
In the present study, most of the infected patients had surgical site infections that could be considered a localised infection and as a result could justify the lack of sensitivity for PCT.
Similar to previous published studies, measurements of WCC contribute little to the early detection of infectious surgical complications [46].
Our pilot study has some limitations. It is a single-centre study and the number of clinical events (21 patients with infection complications) is small which limits the statistical power of our analysis. However, as far as we are aware, this is the first prospective study in elective colorectal surgery that evaluate two biomarkers simultaneously, CRP and PCT, with measurements before the surgery and a 12 days follow-up.
Recently other biomarkers like lipopolysaccharide-binding protein (LBP) have been study as screening tools for AL and increased concentrations of LBP in drain fluid were associated to a higher chance of AL. However, future studies are needed to validate this biomarkers [57].
Despite these limitations our study provides support to use serial measurements of CRP after elective colorectal surgery for early identification of patients at risk of developing infections, that is to say even before infection diagnosis, having CRP a lower cost of CRP compared to the PCT.
Conclusions
Our study suggested that serial CRP measurements after elective colorectal surgery could be used as a diagnostic biomarker in the early prediction of postoperative infectious complications. A prolonged elevation of CRP levels with no subsequent decrease precedes the detection of infection by one day on average. In the present study serial PCT measurements after elective colorectal surgery were unhelpful in prediction of postoperative infectious complications.
References
Nakamura T, Mitomi H, Ihara A, Onozato W, Sato T, Ozawa H, Hatade K, Watanabe M: Risk factors for wound infection after surgery for colorectal cancer. World J Surg. 2008, 32 (6): 1138-1141.
Rovera F, Dionigi G, Boni L, Piscopo C, Masciocchi P, Alberio MG, Carcano G, Diurni M, Dionigi R: Infectious complications in colorectal surgery. Surg Oncol. 2007, 16 (Suppl 1): S121-S124.
Alves A, Panis Y, Trancart D, Regimbeau JM, Pocard M, Valleur P: Factors associated with clinically significant anastomotic leakage after large bowel resection: multivariate analysis of 707 patients. World J Surg. 2002, 26 (4): 499-502.
Buchs NC, Gervaz P, Secic M, Bucher P, Mugnier-Konrad B, Morel P: Incidence, consequences, and risk factors for anastomotic dehiscence after colorectal surgery: a prospective monocentric study. Int J Colorectal Dis. 2008, 23 (3): 265-270.
Makela JT, Kiviniemi H, Laitinen S: Risk factors for anastomotic leakage after left-sided colorectal resection with rectal anastomosis. Dis Colon Rectum. 2003, 46 (5): 653-660.
Veyrie N, Ata T, Muscari F, Couchard AC, Msika S, Hay JM, Fingerhut A, Dziri C: Anastomotic leakage after elective right versus left colectomy for cancer: prevalence and independent risk factors. J Am Coll Surg. 2007, 205 (6): 785-793.
Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L, Gurka D, Kumar A, Cheang M: Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006, 34 (6): 1589-1596.
MacKay GJ, Molloy RG, O'Dwyer PJ: C-reactive protein as a predictor of postoperative infective complications following elective colorectal resection. Colorectal Dis. 13 (5): 583-587.
Fujii T, Tabe Y, Yajima R, Tsutsumi S, Asao T, Kuwano H: Relationship between C-reactive protein levels and wound infections in elective colorectal surgery: C-reactive protein as a predictor for incisional SSI. Hepatogastroenterology. 2011, 58 (107–108): 752-755.
Korner H, Nielsen HJ, Soreide JA, Nedrebo BS, Soreide K, Knapp JC: Diagnostic accuracy of C-reactive protein for intraabdominal infections after colorectal resections. J Gastrointest Surg. 2009, 13 (9): 1599-1606.
Simon L, Gauvin F, Amre DK, Saint-Louis P, Lacroix J: Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: a systematic review and meta-analysis. Clin Infect Dis. 2004, 39 (2): 206-217.
Matthiessen P, Henriksson M, Hallbook O, Grunditz E, Noren B, Arbman G: Increase of serum C-reactive protein is an early indicator of subsequent symptomatic anastomotic leakage after anterior resection. Colorectal Dis. 2008, 10 (1): 75-80.
Deitmar S, Anthoni C, Palmes D, Haier J, Senninger N, Bruwer M: [Are leukocytes and CRP early indicators for anastomotic leakage after esophageal resection?]. Zentralbl Chir. 2009, 134 (1): 83-89.
Welsch T, Frommhold K, Hinz U, Weigand MA, Kleeff J, Friess H, Buchler MW, Schmidt J: Persisting elevation of C-reactive protein after pancreatic resections can indicate developing inflammatory complications. Surgery. 2008, 143 (1): 20-28.
Welsch T, Muller SA, Ulrich A, Kischlat A, Hinz U, Kienle P, Buchler MW, Schmidt J, Schmied BM: C-reactive protein as early predictor for infectious postoperative complications in rectal surgery. Int J Colorectal Dis. 2007, 22 (12): 1499-1507.
Reith HB, Mittelkotter U, Debus ES, Kussner C, Thiede A: Procalcitonin in early detection of postoperative complications. Dig Surg. 1998, 15 (3): 260-265.
Pierrakos C, Vincent JL: Sepsis biomarkers: a review. Crit Care. 2010, 14 (1): R15-
Povoa P: C-reactive protein: a valuable marker of sepsis. Intensive Care Med. 2002, 28 (3): 235-243.
Ranzani OT, Prada LF, Zampieri FG, Battaini LC, Pinaffi JV, Setogute YC, Salluh JI, Povoa P, Forte DN, Azevedo LC, Park M: Failure to reduce C-reactive protein levels more than 25% in the last 24 hours before intensive care unit discharge predicts higher in-hospital mortality: a cohort study. J Crit Care. 2013, 27 (5): 525-e529-515
Povoa P, Coelho L, Almeida E, Fernandes A, Mealha R, Moreira P, Sabino H: C-reactive protein as a marker of ventilator-associated pneumonia resolution: a pilot study. Eur Respir J. 2005, 25 (5): 804-812.
Oberhofer D, Juras J, Pavicic AM, Rancic Zuric I, Rumenjak V: Comparison of C-reactive protein and procalcitonin as predictors of postoperative infectious complications after elective colorectal surgery. Croat Med J. 2012, 53 (6): 612-619.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR: Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999, 27 (2): 97-132. quiz 133–134; discussion 196
O'Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, Lipsett PA, Masur H, Mermel LA, Pearson ML, Raad II, Randolph AG, Rupp ME, Saint S, Healthcare Infection Control Practices Advisory Committee (HICPAC) (Appendix 1): Summary of recommendations: Guidelines for the Prevention of Intravascular Catheter-related Infections. Clin Infect Dis. 2011, 52 (9): 1087-1099.
Niederman MS, Craven DE: Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005, 171 (4): 388-416.
Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA: Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010, 31 (4): 319-326.
Perneger TV: What's wrong with Bonferroni adjustments. BMJ. 1998, 316 (7139): 1236-1238.
Hanley JA, McNeil BJ: The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982, 143 (1): 29-36.
DeLong ER, DeLong DM, Clarke-Pearson DL: Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988, 44 (3): 837-845.
Novotny A, Emmanuel K, Bartels H, Siewert JR, Holzmann B: [Indicators for early prediction of outcome in sepsis]. Chirurg. 2005, 76 (9): 837-844.
Reinhart K, Bayer O, Brunkhorst F, Meisner M: Markers of endothelial damage in organ dysfunction and sepsis. Crit Care Med. 2002, 30 (5 Suppl): S302-S312.
Branagan G, Finnis D: Prognosis after anastomotic leakage in colorectal surgery. Dis Colon Rectum. 2005, 48 (5): 1021-1026.
Velasco E, Thuler LC, Martins CA, Dias LM, Conalves VM: Risk factors for infectious complications after abdominal surgery for malignant disease. Am J Infect Control. 1996, 24 (1): 1-6.
Karanicolas PJ, Dubois L, Colquhoun PH, Swallow CJ, Walter SD, Guyatt GH: The more the better?: the impact of surgeon and hospital volume on in-hospital mortality following colorectal resection. Ann Surg. 2009, 249 (6): 954-959.
Richards CH, Leitch FE, Horgan PG, McMillan DC: A systematic review of POSSUM and its related models as predictors of post-operative mortality and morbidity in patients undergoing surgery for colorectal cancer. J Gastrointest Surg. 2010, 14 (10): 1511-1520.
Bohnen J, Boulanger M, Meakins JL, McLean AP: Prognosis in generalized peritonitis. Relation to cause and risk factors. Arch Surg. 1983, 118 (3): 285-290.
Evans HL, Raymond DP, Pelletier SJ, Crabtree TD, Pruett TL, Sawyer RG: Diagnosis of intra-abdominal infection in the critically ill patient. Curr Opin Crit Care. 2001, 7 (2): 117-121.
Chung YC, Chang YF: Serum C-reactive protein correlates with survival in colorectal cancer patients but is not an independent prognostic indicator. Eur J Gastroenterol Hepatol. 2003, 15 (4): 369-373.
Kragsbjerg P, Holmberg H, Vikerfors T: Serum concentrations of interleukin-6, tumour necrosis factor-alpha, and C-reactive protein in patients undergoing major operations. Eur J Surg. 1995, 161 (1): 17-22.
Castelli GP, Pognani C, Cita M, Stuani A, Sgarbi L, Paladini R: Procalcitonin, C-reactive protein, white blood cells and SOFA score in ICU: diagnosis and monitoring of sepsis. Minerva Anestesiol. 2006, 72 (1–2): 69-80.
Meyer ZC, Schreinemakers JM, Mulder PG, Schrauwen L, de Waal RA, Ermens AA, van der Laan L: Procalcitonin in the recognition of complications in critically ill surgical patients. J Surg Res. 2014, 187 (2): 553-558.
Preas HL, Nylen ES, Snider RH, Becker KL, White JC, Agosti JM, Suffredini AF: Effects of anti-inflammatory agents on serum levels of calcitonin precursors during human experimental endotoxemia. J Infect Dis. 2001, 184 (3): 373-376.
Lindberg M, Hole A, Johnsen H, Asberg A, Rydning A, Myrvold HE, Bjerve KS: Reference intervals for procalcitonin and C-reactive protein after major abdominal surgery. Scand J Clin Lab Invest. 2002, 62 (3): 189-194.
Meisner M, Tschaikowsky K, Hutzler A, Schick C, Schuttler J: Postoperative plasma concentrations of procalcitonin after different types of surgery. Intensive Care Med. 1998, 24 (7): 680-684.
Woeste G, Muller C, Bechstein WO, Wullstein C: Increased serum levels of C-reactive protein precede anastomotic leakage in colorectal surgery. World J Surg. 2010, 34 (1): 140-146.
Cruickshank AM, Hansell DT, Burns HJ, Shenkin A: Effect of nutritional status on acute phase protein response to elective surgery. Br J Surg. 1989, 76 (2): 165-168.
Warschkow R, Tarantino I, Torzewski M, Naf F, Lange J, Steffen T: Diagnostic accuracy of C-reactive protein and white blood cell counts in the early detection of inflammatory complications after open resection of colorectal cancer: a retrospective study of 1,187 patients. Int J Colorectal Dis. 2011, 26 (11): 1405-1413.
Takakura Y, Hinoi T, Egi H, Shimomura M, Adachi T, Saito Y, Tanimine N, Miguchi M, Ohdan H: Procalcitonin as a predictive marker for surgical site infection in elective colorectal cancer surgery. Langenbecks Arch Surg. 2013, 398 (6): 833-839.
Novotny AR, Emmanuel K, Hueser N, Knebel C, Kriner M, Ulm K, Bartels H, Siewert JR, Holzmann B: Procalcitonin ratio indicates successful surgical treatment of abdominal sepsis. Surgery. 2009, 145 (1): 20-26.
Lagoutte N, Facy O, Ravoire A, Chalumeau C, Jonval L, Rat P, Ortega-Deballon P: C-reactive protein and procalcitonin for the early detection of anastomotic leakage after elective colorectal surgery: pilot study in 100 patients. J Visc Surg. 2012, 149 (5): e345-e349.
Garcia-Granero A, Frasson M, Flor-Lorente B, Blanco F, Puga R, Carratala A, Garcia-Granero E: Procalcitonin and C-reactive protein as early predictors of anastomotic leak in colorectal surgery: a prospective observational study. Dis Colon Rectum. 2013, 56 (4): 475-483.
Anielski R, Kusnierz-Cabala B, Szafraniec K: An evaluation of the utility of additional tests in the preoperative diagnostics of acute appendicitis. Langenbecks Arch Surg. 2010, 395 (8): 1061-1068.
Markogiannakis H, Memos N, Messaris E, Dardamanis D, Larentzakis A, Papanikolaou D, Zografos GC, Manouras A: Predictive value of procalcitonin for bowel ischemia and necrosis in bowel obstruction. Surgery. 2011, 149 (3): 394-403.
Gurda-Duda A, Kusnierz-Cabala B, Nowak W, Naskalski JW, Kulig J: Assessment of the prognostic value of certain acute-phase proteins and procalcitonin in the prognosis of acute pancreatitis. Pancreas. 2008, 37 (4): 449-453.
Mofidi R, Suttie SA, Patil PV, Ogston S, Parks RW: The value of procalcitonin at predicting the severity of acute pancreatitis and development of infected pancreatic necrosis: systematic review. Surgery. 2009, 146 (1): 72-81.
Assicot M, Gendrel D, Carsin H, Raymond J, Guilbaud J, Bohuon C: High serum procalcitonin concentrations in patients with sepsis and infection. Lancet. 1993, 341 (8844): 515-518.
O'Connor E, Venkatesh B, Lipman J, Mashongonyika C, Hall J: Procalcitonin in critical illness. Crit Care Resusc. 2001, 3 (4): 236-243.
Komen N, Slieker J, Willemsen P, Mannaerts G, Pattyn P, Karsten T, de Wilt H, van der Harst E, de Rijke YB, Murawska M, Jeekel J, Lange JF, The APPEAL Study Group: Acute phase proteins in drain fluid: a new screening tool for colorectal anastomotic leakage? The APPEAL study: analysis of parameters predictive for evident anastomotic leakage. Am J Surg. 2014, 208 (3): 317-323.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2334/14/444/prepub
Acknowledgements
The authors would like to thank to Dr. Jorge Salluh, from D'or Institute for Research and Education, Rio de Janeiro, Brazil for reading and revising the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they do not have competing interests in this study.
Authors’ contributions
JS participated in the design of the study, performed the statistical analysis and wrote the manuscript. JR and PP conceived of the study, and participated in its design and coordination and helped to draft the manuscript. CL helped in the database and to draft the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Silvestre, J., Rebanda, J., Lourenço, C. et al. Diagnostic accuracy of C-reactive protein and procalcitonin in the early detection of infection after elective colorectal surgery – a pilot study. BMC Infect Dis 14, 444 (2014). https://doi.org/10.1186/1471-2334-14-444
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2334-14-444