Abstract
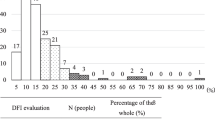
Sperm DNA integrity is a prerequisite for normal spermatozoal function. The aim of the study was to evaluate the role of sperm chromatin damage, its cut-off level and its effect on sperm parameters in men with idiopathic infertility by analyzing 100 idiopathic infertile men and 50 fertile controls. Semen samples were analyzed as per WHO 1999 guidelines and sperm chromatin structure assay (SCSA) was applied to measure DNA fragmentation index (DFI) in sperm. The mean DFI of infertile men (35.75) was significantly (P < .0001) higher as compared to controls (26.22). The threshold level of 30.28% was obtained as cut-off value to discriminate infertile men from fertile controls. Sperm count, forward motility, and normal morphology found to be negatively associated with DFI in overall study subjects. Infertile men with severe oligozoospermia had higher mean DFI (40.01 ± 11.31) than infertile men with oligozoospermia (35.11 ± 10.05) and normal sperm count (33.99 ± 9.96). Moreover 64% of infertile men have DFI > 30 against 6% of fertile controls (P < .0001). Higher sperm DNA fragmentation may be the underlying cause for poor semen quality in idiopathic infertile men and the threshold value of 30.28% is a clear discriminator to distinguish infertile men from fertile men of Indian population. Thus, DFI is a good prognostic marker as cases with higher sperm DFI may have poor success rate even after assisted conception and may experience recurrent pregnancy loss (RPL) and should be counseled accordingly.
Similar content being viewed by others
References
Dowsing AT, Yong EL, Clark M, McLachlan RI, de Kretser DM, Trounson AO. Linkage between male infertility and trinucleotide repeat expansion in the androgen-receptor gene. Lancet. 21, 1999;354(9179):640–643.
Derijck AA, van der Heijden GW, Ramos L, Giele M, Kremer JA, de Boer P. Motile human normozoospermic and oligozoospermic semen samples show a difference in double-strand DNA break incidence. Hum Reprod. 2007;22(9):2368–2376
Borini A, Tarozzi N, Bizzaro D, et al. Sperm DNA fragmentation: paternal effect on early post-implantation embryo development in ART. Hum Reprod. 2006;21(11):2876–2881
Varghese AC, Bragais FM, Mukhopadhyay D, et al. Human sperm DNA integrity in normal and abnormal semen samples and its correlation with sperm characteristics. Andrologia. 2009;41(4):207–215
Ward WS, Coffey DS. DNA packaging and organization in mammalian spermatozoa: comparison with somatic cells. Biol Reprod. 1991;44(4):569–574
Giwercman A, Richthoff J, Hjollund H, et al. Correlation between sperm motility and sperm chromatin structure assay parameters. Fertil Steril. 2003;80(6):1404–1412
Moskovtsev SI, Willis J, Azad A, Mullen JB. Sperm DNA integrity: correlation with sperm plasma membrane integrity in semen evaluated for male infertility. Arch Androl. 2005;51(1):33–40
Miller D, Brinkworth M, Iles D. Paternal DNA packaging in spermatozoa: more than the sum of its parts? DNA, histones, protamines and epigenetics. Reproduction. 2010;139(2):287–301
Fuentes-Mascorro G, Serrano H, Rosado A. Sperm chromatin. Arch Androl. 2000;45(3):215–225
Torregrosa N, Dominguez-Fandos D, Camejo MI, et al. Protamine 2 precursors, protamine 1/protamine 2 ratio, DNA integrity and other sperm parameters in infertile patients. Hum Reprod. 2006;21(8):2084–2089
Braun RE. Packaging paternal chromosomes with protamine. Nat Genet. 2001;28(1):10–12
Irvine DS, Twigg JP, Gordon EL, Fulton N, Milne PA, Aitken RJ. DNA integrity in human spermatozoa: relationships with semen quality. J Androl. 2000;21(1):33–44
Smith R, Kaune H, Parodi D, et al. Increased sperm DNA damage in patients with varicocele: relationship with seminal oxidative stress. Hum Reprod. 2006;21(4):986–993
Venkatesh S, Riyaz AM, Shamsi MB, et al. Clinical significance of reactive oxygen species in semen of infertile Indian men. Andrologia. 2009;41(4):251–256
Evenson DP, Darzynkiewicz Z, Melamed MR. Relation of mammalian sperm chromatin heterogeneity to fertility. Science. 5 1980;210(4474):1131–1133.
Evenson DP, Larson KL, Jost LK. Sperm chromatin structure assay: its clinical use for detecting sperm DNA fragmentation in male infertility and comparisons with other techniques. J Androl. 2002;23(1):25–43
Evenson DP, Kasperson K, Wixon RL. Analysis of sperm DNA fragmentation using flow cytometry and other techniques. Soc Reprod Fertil Suppl. 2007;65:93–113
Bungum M, Bungum L, Giwercman A. Sperm chromatin structure assay (SCSA): a tool in diagnosis and treatment of infertility. Asian J Androl. 2010;13(1):69–75
WHO, ed. WHO laboratory Manual for the Examination of Human Semen and Sperm-Cervical Mucus Interaction. 4 ed.; 1999. Cambridge UCUP.
Evenson DP, Jost LK, Marshall D, et al. Utility of the sperm chromatin structure assay as a diagnostic and prognostic tool in the human fertility clinic. Hum Reprod. 1999;14(4):1039–1049
Ward WS. Function of sperm chromatin structural elements in fertilization and development. Mol Hum Reprod. 2010;16(1):30–36
Shamsi MB, Venkatesh S, Pathak P, Deka D, Dada R. Sperm DNA damage and oxidative stress: Role in Recurrent spontaneous abortions. Indian J Med Res. 2011.
Lin MH, Kuo-Kuang Lee R, Li SH, Lu CH, Sun FJ, Hwu YM. Sperm chromatin structure assay parameters are not related to fertilization rates, embryo quality, and pregnancy rates in in vitro fertilization and intracytoplasmic sperm injection, but might be related to spontaneous abortion rates. Fertil Steril. 2008;90(2):352–359
Spano M, Bonde JP, Hjollund HI, Kolstad HA, Cordelli E, Leter G. Sperm chromatin damage impairs human fertility. The Danish First Pregnancy Planner Study Team. Fertil Steril. 2000;73(1):43–50
Duran EH, Morshedi M, Taylor S, Oehninger S. Sperm DNA quality predicts intrauterine insemination outcome: a prospective cohort study. Hum Reprod. 2002;17(12):3122–3128
Saleh RA, Agarwal A, Nada EA, et al. Negative effects of increased sperm DNA damage in relation to seminal oxidative stress in men with idiopathic and male factor infertility. Fertil Steril. 2003;79(suppl 3):1597–1605
Sun JG, Jurisicova A, Casper RF. Detection of deoxyribonucleic acid fragmentation in human sperm: correlation with fertilization in vitro. Biol Reprod. 1997;56(3):602–607
Benchaib M, Braun V, Lornage J, et al. Sperm DNA fragmentation decreases the pregnancy rate in an assisted reproductive technique. Hum Reprod. 2003;18(5):1023–1028
Dada R, Mahfouz RZ, Humar R, et al. A comprehensive work up for an asthenozoospermic man with repeated intracytoplasmic sperm injection (ICSI) failure. Andrologia. 2011.
Bungum M, Humaidan P, Spano M, Jepson K, Bungum L, Giwercman A. The predictive value of sperm chromatin structure assay (SCSA) parameters for the outcome of intrauterine insemination, IVF and ICSI. Hum Reprod. 2004;19(6):1401–1408
Larson-Cook KL, Brannian JD, Hansen KA, Kasperson KM, Aamold ET, Evenson DP. Relationship between the outcomes of assisted reproductive techniques and sperm DNA fragmentation as measured by the sperm chromatin structure assay. Fertil Steril. 2003;80(4):895–902
Micinski P, Pawlicki K, Wielgus E, Bochenek M, Tworkowska I. The sperm chromatin structure assay (SCSA) as prognostic factor in IVF/ICSI program. Reprod Biol. 2009;9(1):65–70
Dada, R, ed. Recurrent pregnancy loss: Male factor. New Delhi, IN: Federation of obstetrics and gynecological society of India publication. Jaypee brothers; 2010. Deka D, Malhotra N, eds. An introduciton to genetics and fetal medicine.
Venkatesh S, Shamsi MB, Dada R. Re: Attenuation of oxidative stress after varicocelectomy in subfertile patients with varicocele: S.-S. Chen, W. J. Huang, L. S. Chang and Y.-H. Wei J Urol 2008;179:639–642. J Urol. 2009;181(4):1964–1965; author reply 1965–1966
Smit M, Romijn JC, Wildhagen MF, Weber RF, Dohle GR. Sperm chromatin structure is associated with the quality of spermatogenesis in infertile patients. Fertil Steril. October;94(5):1748–1752.
Erenpreiss J, Elzanaty S, Giwercman A. Sperm DNA damage in men from infertile couples. Asian J Androl. 2008;10(5):786–790
Bungum M, Humaidan P, Axmon A, et al. Sperm DNA integrity assessment in prediction of assisted reproduction technology outcome. Hum Reprod. 2007;22(1):174–179
Boe-Hansen GB, Fedder J, Ersboll AK, Christensen P. The sperm chromatin structure assay as a diagnostic tool in the human fertility clinic. Hum Reprod. 2006;21(6):1576–1582
Giwercman A, Lindstedt L, Larsson M, et al. Sperm chromatin structure assay as an independent predictor of fertility in vivo: a case-control study. Int J Androl. February;33(1):e221–e227.
Sakkas D, Moffatt O, Manicardi GC, Mariethoz E, Tarozzi N, Bizzaro D. Nature of DNA damage in ejaculated human spermatozoa and the possible involvement of apoptosis. Biol Reprod. 2002;66(4):1061–1067
Balhorn R, Reed S, Tanphaichitr N. Aberrant protamine 1/protamine 2 ratios in sperm of infertile human males. Experientia. 15 1988;44(1):52–55.
Bennetts LE, De Iuliis GN, Nixon B, et al. Impact of estrogenic compounds on DNA integrity in human spermatozoa: evidence for cross-linking and redox cycling activities. Mutat Res. 2008;641(1–2):1–11
Badouard C, Menezo Y, Panteix G, et al. Determination of new types of DNA lesions in human sperm. Zygote. 2008;16(1):9–13
Tunc O, Tremellen K. Oxidative DNA damage impairs global sperm DNA methylation in infertile men. J Assist Reprod Genet. 2009;26(9–10):537–544
Rubes J, Selevan SG, Evenson DP, et al. Episodic air pollution is associated with increased DNA fragmentation in human sperm without other changes in semen quality. Hum Reprod. 2005;20(10):2776–2783
Schmid TE, Eskenazi B, Baumgartner A, et al. The effects of male age on sperm DNA damage in healthy non-smokers. Hum Reprod. 2007;22(1):180–187
Potts RJ, Newbury CJ, Smith G, Notarianni LJ, Jefferies TM. Sperm chromatin damage associated with male smoking. Mutat Res. 25 1999;423(1–2):103–111.
Lewis SE, Aitken RJ. DNA damage to spermatozoa has impacts on fertilization and pregnancy. Cell Tissue Res. 2005;322(1):33–41
Zini A, Blumenfeld A, Libman J, Willis J. Beneficial effect of microsurgical varicocelectomy on human sperm DNA integrity. Hum Reprod. 2005;20(4):1018–1021
Werthman P, Wixon R, Kasperson K, Evenson DP. Significant decreases in sperm deoxyribonucleic acid fragmentation after varicocelectomy. Fertil Steril. 2008;90(5):1880–1884
Zampieri N, Zamboni C, Ottolenghi A, Camoglio FS. The role of lifestyle changing to improve the semen quality in patients with varicocele. Minerva Urol Nefrol. 2008;60(4):199–204
Hughes CM, Lewis SE, McKelvey-Martin VJ, Thompson W. A comparison of baseline and induced DNA damage in human spermatozoa from fertile and infertile men, using a modified comet assay. Mol Hum Reprod. 1996;2(8):613–619
Henkel R, Kierspel E, Hajimohammad M, et al. DNA fragmentation of spermatozoa and assisted reproduction technology. Reprod Biomed Online. 2003;7(4):477–484
Bakos HW, Thompson JG, Feil D, Lane M. Sperm DNA damage is associated with assisted reproductive technology pregnancy. Int J Androl. 2008;31(5):518–526
Barroso G, Valdespin C, Vega E, et al. Developmental sperm contributions: fertilization and beyond. Fertil Steril. 2009;92(3):835–848
Miller D, Ostermeier GC. Towards a better understanding of RNA carriage by ejaculate spermatozoa. Hum Reprod Update. 2006;12(6):757–767
Carrell DT, Liu L, Peterson CM, et al. Sperm DNA fragmentation is increased in couples with unexplained recurrent pregnancy loss. Arch Androl. 2003;49(1):49–55
Zini A, San Gabriel M, Baazeem A. Antioxidants and sperm DNA damage: a clinical perspective. J Assist Reprod Genet. 2009;26(8):427–432
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Venkatesh, S., Singh, A., Shamsi, M.B. et al. Clinical Significance of Sperm DNA Damage Threshold Value in the Assessment of Male Infertility. Reprod. Sci. 18, 1005–1013 (2011). https://doi.org/10.1177/1933719111401662
Published:
Issue Date:
DOI: https://doi.org/10.1177/1933719111401662